Cardiac cycle in pathologic states US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cardiac cycle in pathologic states. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cardiac cycle in pathologic states US Medical PG Question 1: A 49-year-old male presents to the emergency room with dyspnea and pulmonary edema. He reports that he has been smoking 2 packs a day for the past 25 years and has difficulty breathing during any sustained physical activity. His blood pressure is normal, and he reports a history of COPD. An echocardiogram was ordered as part of a cardiac workup. Which of the following would be the most likely finding?
- A. Right ventricular hypertrophy (Correct Answer)
- B. Left ventricular hypertrophy
- C. Mitral valve insufficiency
- D. Right atrial enlargement
- E. Tricuspid regurgitation
Cardiac cycle in pathologic states Explanation: ***Right ventricular hypertrophy***
- The patient's history of **COPD** and heavy smoking leads to **pulmonary hypertension**, which increases the afterload on the right ventricle, causing it to hypertrophy.
- While the patient has pulmonary edema, the normal blood pressure and history of COPD point toward **cor pulmonale**, where RVH is a hallmark, rather than primary left-sided heart failure.
*Left ventricular hypertrophy*
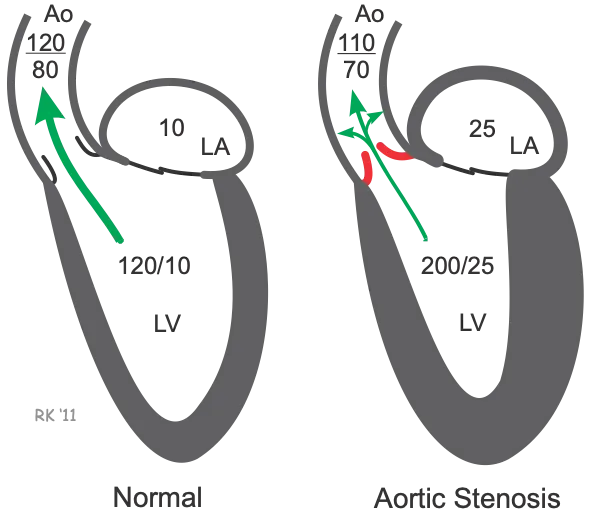
- **Left ventricular hypertrophy** is typically caused by systemic hypertension, aortic stenosis, or hypertrophic cardiomyopathy, none of which are strongly suggested here.
- The patient's **normal blood pressure** makes LVH due to chronic hypertension less likely.
*Mitral valve insufficiency*
- **Mitral valve insufficiency** would primarily cause pulmonary edema due to backflow into the left atrium and pulmonary veins, but it is not directly linked to the patient's COPD and smoking history.
- Clinical findings such as a **pansystolic murmur** and specific echocardiographic evidence of valvular dysfunction are not mentioned.
*Right atrial enlargement*
- **Right atrial enlargement** often accompanies right ventricular hypertrophy due to increased pressure and volume load, but RVH is the more direct consequence of chronic pulmonary hypertension.
- While possible, it is secondary to the elevated right ventricular pressure and usually seen with significant RV remodeling.
*Tricuspid regurgitation*
- **Tricuspid regurgitation** can develop secondary to severe pulmonary hypertension and right ventricular dilation, but it is a consequence of RV dysfunction, not the primary finding.
- The initial compensatory mechanism to increased afterload is **RV hypertrophy**, which precedes significant dilation and regurgitation.
Cardiac cycle in pathologic states US Medical PG Question 2: A 67-year-old male with a history of poorly controlled hypertension, COPD, and diabetes presents to his cardiologist for a routine appointment. He reports that he has no current complaints and has not noticed any significant changes in his health. On exam, the cardiologist hears an extra heart sound in late diastole that immediately precedes S1. This heart sound is most associated with which of the following?
- A. Left ventricular hypertrophy (Correct Answer)
- B. Increased filling pressures
- C. Mitral regurgitation
- D. Mitral stenosis
- E. Ventricular dilation
Cardiac cycle in pathologic states Explanation: ***Left ventricular hypertrophy***
- An **S4 heart sound** in late diastole, immediately preceding S1, is typically heard with a **stiff, non-compliant left ventricle**, which is characteristic of **left ventricular hypertrophy**.
- The patient's history of **poorly controlled hypertension and diabetes** are significant risk factors for developing left ventricular hypertrophy.
*Increased filling pressures*
- While increased filling pressures can occur in heart failure, an **S4** specifically indicates **diastolic dysfunction due to a hypertrophied ventricle**, not merely high filling pressures.
- An **S3 heart sound** is more commonly associated with increased filling pressures and **ventricular dilation in systolic dysfunction**.
*Mitral regurgitation*
- **Mitral regurgitation** is typically characterized by a **holosystolic murmur**, which is a different auscultatory finding.
- While chronic mitral regurgitation can lead to ventricular hypertrophy, the **S4 sound** itself reflects the underlying **stiffness of the ventricle**, not directly the valvular insufficiency.
*Mitral stenosis*
- **Mitral stenosis** is characterized by an **opening snap** followed by a **mid-diastolic rumble**, which is distinct from an S4 heart sound.
- It involves a narrowed mitral valve orifice, causing impedance to blood flow from the left atrium to the left ventricle.
*Ventricular dilation*
- **Ventricular dilation** is typically associated with an **S3 heart sound**, which occurs in early diastole during rapid ventricular filling.
- An **S4** signifies a **non-compliant, stiff ventricle** (often hypertrophied), rather than a dilated one.
Cardiac cycle in pathologic states US Medical PG Question 3: A 72-year-old man presents to his primary care physician for a general checkup. The patient works as a farmer and has no concerns about his health. He has a past medical history of hypertension and obesity. His current medications include lisinopril and metoprolol. His temperature is 99.5°F (37.5°C), blood pressure is 177/108 mmHg, pulse is 90/min, respirations are 17/min, and oxygen saturation is 98% on room air. Physical exam is notable for a murmur after S2 over the left sternal border. The patient demonstrates a stable gait and 5/5 strength in his upper and lower extremities. Which of the following is another possible finding in this patient?
- A. Murmur that radiates to the carotids
- B. Wedge pressure lower than expected
- C. Femoral artery murmur (Correct Answer)
- D. Rumbling heard at the cardiac apex
- E. Audible click heard at the cardiac apex
Cardiac cycle in pathologic states Explanation: ***Femoral artery murmur***
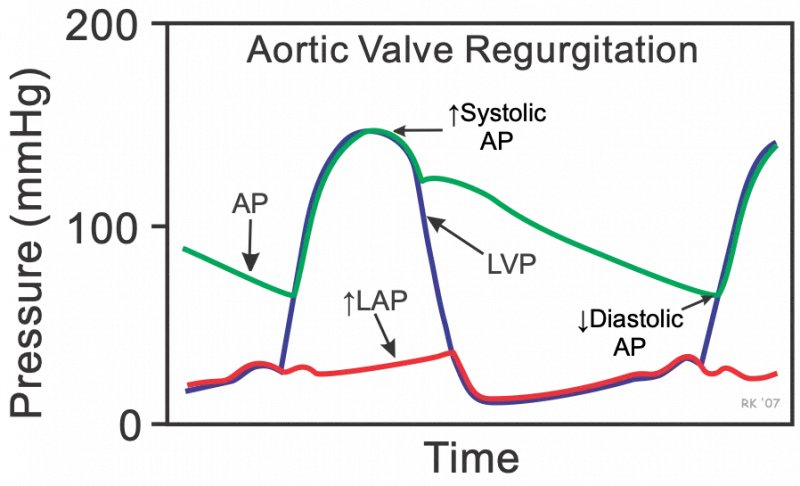
- A murmur heard after S2 over the left sternal border in an elderly patient suggests **aortic regurgitation (AR)**.
- In AR, a **femoral artery murmur (Duroziez's sign)** can be heard, characterized by a systolic murmur over the femoral artery with proximal compression and a diastolic murmur with distal compression.
*Murmur that radiates to the carotids*
- A murmur radiating to the carotids is characteristic of **aortic stenosis**, which typically presents as a systolic murmur, not a diastolic one as heard in this patient.
- Aortic stenosis is also associated with a **crescendo-decrescendo murmur**, in contrast to the diastolic murmur described.
*Wedge pressure lower than expected*
- This patient likely has **aortic regurgitation**, which increases **left ventricular end-diastolic pressure** and, consequently, **pulmonary capillary wedge pressure (PCWP)**.
- A lower than expected wedge pressure would be inconsistent with the volume overload often seen in significant AR.
*Rumbling heard at the cardiac apex*
- A rumbling murmur at the cardiac apex is characteristic of **mitral stenosis**, which is typically preceded by an opening snap.
- The patient's murmur is heard after S2 (diastolic) at the left sternal border, not the apex, making mitral stenosis less likely.
*Audible click heard at the cardiac apex*
- An audible click at the cardiac apex is typically associated with **mitral valve prolapse**, often followed by a mid-systolic murmur.
- This finding is not consistent with the diastolic murmur heard after S2 at the left sternal border.
Cardiac cycle in pathologic states US Medical PG Question 4: A 65-year-old man with hypertension comes to the physician for a routine health maintenance examination. Current medications include atenolol, lisinopril, and atorvastatin. His pulse is 86/min, respirations are 18/min, and blood pressure is 145/95 mm Hg. Cardiac examination is shown. Which of the following is the most likely cause of this physical examination finding?
- A. Myxomatous degeneration of the mitral valve
- B. Inflammation of the pericardium
- C. Thickening of the mitral valve leaflets
- D. Decreased compliance of the left ventricle (Correct Answer)
- E. Dilation of the aortic root
Cardiac cycle in pathologic states Explanation: ***Decrease in compliance of the left ventricle***
- The patient's **uncontrolled hypertension** for a long time can lead to **left ventricular hypertrophy** and **stiffening** of the heart muscle, resulting in **decreased compliance**.
- A decrease in left ventricular compliance can result in a **diastolic dysfunction**, leading to **heart failure with preserved ejection fraction (HFpEF)**.
*Myxomatous degeneration of the mitral valve*
- This condition is typically associated with **mitral valve prolapse**, which causes a **mid-systolic click** and a **late systolic murmur**.
- There is no information in the question about associated findings to suggest mitral valve prolapse, such as valvular disease or specific murmurs.
*Inflammation of the pericardium*
- **Pericarditis** typically presents with **sharp chest pain** that is relieved by leaning forward and a characteristic **friction rub** on auscultation.
- While inflammation can affect cardiac function, it's not the most direct consequence of chronic hypertension in the absence of other symptoms.
*Thickening of the mitral valve leaflets*
- **Mitral valve leaflet thickening** often results from **rheumatic fever** or age-related calcification, leading to **mitral stenosis** or **regurgitation**.
- The patient's history of long-standing hypertension does not directly indicate thickening of the mitral valve leaflets.
*Dilation of the aortic root*
- Aortic root dilation is associated with conditions like **Marfan syndrome**, **Ehlers-Danlos syndrome**, or uncontrolled hypertension leading to **aortic aneurysm** or **dissection**.
- While chronic hypertension can contribute to aortic dilation, this finding isn't directly supported by the current clinical picture suggesting a primary cause for a physical finding.
Cardiac cycle in pathologic states US Medical PG Question 5: A 34-year-old male is brought to the emergency department. He has prior hospitalizations for opiate overdoses, but today presents with fever, chills, rigors and malaise. On physical exam vitals are temperature: 100.5 deg F (38.1 deg C), pulse is 105/min, blood pressure is 135/60 mmHg, and respirations are 22/min. You note the following findings on the patient's hands (Figures A and B). You note that as the patient is seated, his head bobs with each successive heart beat. Which of the following findings is most likely present in this patient?
- A. A holosystolic murmur at the 4th intercostal midclavicular line
- B. A water-hammer pulse when palpating the radial artery (Correct Answer)
- C. Decreased blood pressure as measured in the lower extremities compared to the upper extremities
- D. A harsh crescendo-decrescendo systolic murmur in the right second intercostal space
- E. A consistent gallop with an S4 component
Cardiac cycle in pathologic states Explanation: ***A water-hammer pulse when palpating the radial artery***
- The patient's history of **opiate overdose**, fever, chills, and the presence of **Janeway lesions** (Figures A and B) on the hands strongly suggest **infective endocarditis**. The head bobbing (Musset's sign) indicates **severe aortic regurgitation**.
- **Water-hammer pulse** (Corrigan's pulse) is a classic sign of **severe aortic regurgitation**, characterized by a rapid, forceful arterial pulse that quickly collapses due to a large stroke volume and rapid diastolic runoff.
*A holosystolic murmur at the 4th intercostal midclavicular line*
- A holosystolic murmur at the 4th intercostal midclavicular line is typically associated with **mitral regurgitation**, which is less likely given the prominent signs of aortic regurgitation.
- While endocarditis can affect the mitral valve, the specific clinical signs point towards **aortic valve involvement**.
*Decreased blood pressure as measured in the lower extremities compared to the upper extremities*
- This finding is characteristic of **coarctation of the aorta**, a congenital heart defect, which is not suggested by the patient's presentation or risk factors.
- The patient's symptoms are more consistent with an acute infectious process affecting the heart valves.
*A harsh crescendo-decrescendo systolic murmur in the right second intercostal space*
- A harsh crescendo-decrescendo systolic murmur in the right second intercostal space is typical of **aortic stenosis**.
- While aortic insufficiency is present, the murmur for uncomplicated aortic insufficiency is usually a **diastolic decrescendo murmur**, not a harsh systolic murmur.
*A consistent gallop with an S4 component*
- An S4 gallop is typically heard in conditions involving **decreased ventricular compliance** (e.g., severe hypertension, aortic stenosis, hypertrophic cardiomyopathy).
- While endocarditis can cause heart failure, an S4 gallop is not a direct or primary sign of **aortic regurgitation**. An S3 gallop is more commonly associated with **volume overload** and heart failure, which might develop in severe aortic regurgitation.
Cardiac cycle in pathologic states US Medical PG Question 6: A 54-year-old woman presents to the emergency ward with a chief complaint of chest pain. The pain is sharp and present in the anterior part of the chest. There is no radiation of the pain; however, the intensity is decreased while sitting and leaning forward. There is no associated shortness of breath. Vital signs are the following: blood pressure is 132/84 mm Hg; pulse rate is 82/min, rhythmic, and regular. Lungs are clear on auscultation and cardiovascular examination demonstrates scratchy and squeaking sounds at the left sternal border. Kussmaul sign is positive and ECG shows new widespread ST segment elevation and PR depression. The most likely cause for these findings in this patient is?
- A. Restrictive cardiomyopathy
- B. Acute pericarditis (Correct Answer)
- C. Pleurisy
- D. Right ventricular myocardial infarction
- E. Cardiac tamponade
Cardiac cycle in pathologic states Explanation: ***Acute pericarditis***
- The classic presentation includes **sharp, pleuritic chest pain** that **improves with leaning forward** and **worsens with lying down**. The presence of a **pericardial friction rub** (scratchy and squeaking sounds) and specific ECG findings like **widespread ST elevation** and **PR depression** are highly indicative.
- **Kussmaul sign** (paradoxical rise in jugular venous pressure on inspiration) is unusual in uncomplicated acute pericarditis but may suggest associated pericardial effusion or early constrictive physiology. The clinical picture remains most consistent with acute pericarditis given the characteristic chest pain, friction rub, and ECG changes.
*Restrictive cardiomyopathy*
- Characterized by **diastolic dysfunction** and impaired ventricular filling, leading to symptoms like dyspnea and edema. While Kussmaul sign can be present, the chest pain characteristics, friction rub, and widespread ST elevation with PR depression are not typical.
- The ECG findings in restrictive cardiomyopathy usually involve **low voltage** and non-specific ST-T wave changes, not diffuse ST elevation and PR depression.
*Pleurisy*
- Pleurisy causes **sharp, pleuritic chest pain** that can worsen with breathing and movement, similar to pericarditis. However, it does not typically present with a pericardial friction rub or the characteristic ECG changes of widespread ST elevation and PR depression.
- Pleurisy is an inflammation of the pleura, often indicated by **pleural friction rubs** and usually associated with pulmonary conditions, which are not suggested by this patient's findings.
*Right ventricular myocardial infarction*
- While it can cause chest pain and positive Kussmaul sign due to elevated right atrial pressure, the chest pain is typically more anginal-like and not relieved by leaning forward.
- The ECG would show **ST elevation primarily in right-sided leads (V4R)** and inferior leads (II, III, aVF), but would **not typically show widespread ST elevation or PR depression** in multiple lead distributions or a pericardial friction rub.
*Cardiac tamponade*
- Characterized by the **Beck's triad** (hypotension, muffled heart sounds, and elevated jugular venous pressure) and pulsus paradoxus. Chest pain can be present, but the pain's amelioration with leaning forward and the specific ECG changes with widespread ST elevation and PR depression are not typical.
- While a pericardial friction rub might precede tamponade, **cardiac tamponade itself typically develops from a significant pericardial effusion**, leading to compression of the heart and does not directly manifest with diffuse ST elevation and PR depression.
Cardiac cycle in pathologic states US Medical PG Question 7: A 74-year-old man comes to the physician for a 6-month history of progressively worsening fatigue and shortness of breath on exertion. He immigrated to the United States 35 years ago from India. His pulse is 89/min and blood pressure is 145/60 mm Hg. Crackles are heard at the lung bases. Cardiac examination shows a grade 3/6 early diastolic murmur loudest at the third left intercostal space. Further evaluation of this patient is most likely to show which of the following?
- A. Paradoxical splitting of S2
- B. Pulsus paradoxus
- C. Pulsus parvus et tardus
- D. Fixed splitting of S2
- E. Water hammer pulse (Correct Answer)
Cardiac cycle in pathologic states Explanation: ***Water hammer pulse***
- The patient's presentation with **fatigue**, **dyspnea**, **crackles**, and a **grade 3/6 early diastolic murmur** loudest at the **third left intercostal space** is highly suggestive of **aortic regurgitation (AR)**.
- A **water hammer pulse** (also known as a **Corrigan's pulse**) is a **bounding**, **collapsing pulse** characteristic of severe AR due to the rapid runoff of blood from the aorta into the left ventricle during diastole, causing a widened pulse pressure (145/60 mmHg in this case).
*Paradoxical splitting of S2*
- **Paradoxical splitting of S2** occurs when the aortic valve closes *after* the pulmonic valve, typically due to **left bundle branch block** or **severe aortic stenosis**, which are not indicated here.
- In such cases, the split narrows or disappears during inspiration.
*Pulsus paradoxus*
- **Pulsus paradoxus** is an exaggerated drop in systolic blood pressure (>10 mmHg) during inspiration, commonly seen in **cardiac tamponade**, **severe asthma**, or **constrictive pericarditis**.
- There are no features in the patient's history or examination to suggest these conditions.
*Pulsus parvus et tardus*
- **Pulsus parvus et tardus** (small and delayed pulse) is characteristic of **severe aortic stenosis**, where the pulse is weak and slow to rise due to obstruction of left ventricular outflow.
- The murmur described, an **early diastolic murmur**, is indicative of **aortic regurgitation**, not stenosis.
*Fixed splitting of S2*
- **Fixed splitting of S2** is typically associated with an **atrial septal defect (ASD)**, where the split between the aortic and pulmonic components of S2 remains constant during respiration.
- There is no clinical evidence to suggest an ASD in this patient.
Cardiac cycle in pathologic states US Medical PG Question 8: An abnormal wave is noted on a routine ECG. The wave in question represents which of the following electrical events in the cardiac cycle?
- A. Period between ventricular depolarization and repolarization
- B. Atrial repolarization
- C. Ventricular repolarization (Correct Answer)
- D. Ventricular depolarization
- E. Atrial depolarization
Cardiac cycle in pathologic states Explanation: ***Ventricular repolarization***
- The **T wave** represents ventricular repolarization, which is the electrical recovery phase of the ventricles after contraction
- T wave abnormalities are among the most common ECG findings and include **T wave inversions** (myocardial ischemia, ventricular hypertrophy), **peaked T waves** (hyperkalemia), **flattened T waves** (hypokalemia, ischemia), and **biphasic T waves**
- The T wave corresponds to **phase 3** of the ventricular action potential when potassium channels open and the membrane repolarizes
*Period between ventricular depolarization and repolarization*
- This describes the **ST segment**, which represents the period when ventricles are completely depolarized before repolarization begins
- The **QT interval** encompasses both ventricular depolarization and repolarization (QRS + ST segment + T wave)
- These are intervals or segments, not waves
*Atrial repolarization*
- Atrial repolarization occurs during ventricular depolarization and is represented by the **Ta wave**
- This wave is typically **not visible** on standard ECG because it is **masked by the much larger QRS complex** and has very low amplitude
- It cannot be identified as a distinct wave on routine ECGs
*Ventricular depolarization*
- The **QRS complex** represents ventricular depolarization, the electrical activation that triggers ventricular contraction
- Normal QRS duration is **0.06-0.10 seconds** (3 small boxes or less)
- QRS abnormalities include bundle branch blocks, ventricular hypertrophy patterns, and pre-excitation
*Atrial depolarization*
- The **P wave** represents atrial depolarization, the electrical activation that triggers atrial contraction
- Normal P wave characteristics: **upright in leads I, II, aVF**; duration less than 0.12 seconds; amplitude less than 2.5 mm
- P wave abnormalities include left atrial enlargement (broad, notched P waves) and right atrial enlargement (tall, peaked P waves)
Cardiac cycle in pathologic states US Medical PG Question 9: A 27-year-old male arrives in the emergency department with a stab wound over the precordial chest wall. The patient is in distress and is cold, sweaty, and pale. Initial physical examination is significant for muffled heart sounds, distended neck veins, and a 3 cm stab wound near the left sternal border. Breath sounds are present bilaterally without evidence of tracheal deviation. Which of the following additional findings would be expected on further evaluation?
- A. Decrease in central venous pressure by 5 mmHg with inspiration
- B. 15 mmHg decrease in systolic blood pressure with inspiration (Correct Answer)
- C. Decrease in the patient's heart rate by 15 beats per minute with inspiration
- D. Steadily decreasing heart rate to 60 beats per minute
- E. Elevated blood pressure to 170/110
Cardiac cycle in pathologic states Explanation: ***15 mmHg decrease in systolic blood pressure with inspiration***
- The constellation of muffled heart sounds, distended neck veins, and hypotension (implied by cold, sweaty, and pale appearance) following a precordial stab wound points to **cardiac tamponade**, an acutely life-threatening condition.
- A significant drop in systolic blood pressure (>10 mmHg) during inspiration, known as **pulsus paradoxus**, is a classic sign of cardiac tamponade as the increased venous return to the right heart during inspiration bows the interventricular septum, impinging on left ventricular filling.
*Decrease in central venous pressure by 5 mmHg with inspiration*
- In cardiac tamponade, the **central venous pressure (CVP) is typically elevated** and would not decrease significantly with inspiration due to impaired right ventricular filling.
- The elevated CVP contributes to the observed **distended neck veins**.
*Decrease in the patient's heart rate by 15 beats per minute with inspiration*
- In cardiac tamponade, the body attempts to compensate for reduced cardiac output with **reflex tachycardia**, so a decrease in heart rate is unexpected.
- Heart rate usually remains elevated or variable as the heart struggles to maintain perfusion.
*Steadily decreasing heart rate to 60 beats per minute*
- A steadily decreasing heart rate to 60 bpm (bradycardia) is contrary to the expected physiological response of **tachycardia** in cardiac tamponade as the body compensates for hypoperfusion.
- Bradycardia in this context would indicate severe decompensation and imminent cardiac arrest rather than a compensatory mechanism.
*Elevated blood pressure to 170/110*
- This patient is in **obstructive shock** due to cardiac tamponade; therefore, their blood pressure would be **hypotensive**, not hypertensive.
- **Hypotension** is a key component of Beck's triad (muffled heart sounds, distended neck veins, hypotension) which strongly suggests cardiac tamponade.
Cardiac cycle in pathologic states US Medical PG Question 10: Seventy-two hours after admission for an acute myocardial infarction, a 48-year-old man develops dyspnea and a productive cough with frothy sputum. Physical examination shows coarse crackles in both lungs and a blowing, holosystolic murmur heard best at the apex. ECG shows Q waves in the anteroseptal leads. Pulmonary capillary wedge pressure is 23 mm Hg. Which of the following is the most likely cause of this patient’s current condition?
- A. Rupture of the ventricular free wall
- B. Postmyocardial infarction syndrome
- C. Aortic root dilation
- D. Rupture of the interventricular septum
- E. Rupture of the chordae tendineae (Correct Answer)
Cardiac cycle in pathologic states Explanation: ***Rupture of the chordae tendineae***
- The combination of acute dyspnea, frothy sputum (**pulmonary edema**), a new **holosystolic murmur** loudest at the apex, suggestive of **mitral regurgitation**, and high **pulmonary capillary wedge pressure** (PCWP > 18 mmHg indicating pulmonary edema) is classic for papillary muscle or chordae tendineae rupture following an **acute myocardial infarction (MI)**.
- Antero-septal Q waves suggest an infarction in an area supplied by the **left anterior descending artery**, which can also affect the **anterolateral papillary muscle** of the mitral valve.
*Rupture of the ventricular free wall*
- This typically presents as **cardiac tamponade** with hypotension, jugular venous distension, and muffled heart sounds, often leading to rapid hemodynamic collapse and death.
- While it can occur post-MI, a new holosystolic murmur and prominent pulmonary edema are not characteristic features.
*Postmyocardial infarction syndrome*
- Also known as **Dressler syndrome**, this is a **pericarditis** that develops weeks to months after an MI.
- It presents with fever, pleuritic chest pain, and pericardial friction rub and would not typically cause acute pulmonary edema or a new holosystolic murmur within 72 hours.
*Aortic root dilation*
- This condition is not directly linked to an acute MI and typically causes **aortic regurgitation**, which manifests as a **diastolic murmur** (decrescendo early diastolic murmur), not a holosystolic murmur.
- While it can cause heart failure, the acute onset post-MI with a new apical holosystolic murmur points away from this diagnosis.
*Rupture of the interventricular septum*
- This would also present with a new **holosystolic murmur**, but it would be loudest at the **left sternal border** due to a **ventricular septal defect**.
- While it can cause pulmonary edema and elevated PCWP, the murmur's location at the apex strongly points towards mitral valve pathology rather than a septal defect.
More Cardiac cycle in pathologic states US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.