Respiratory regulation of acid-base US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Respiratory regulation of acid-base. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Respiratory regulation of acid-base US Medical PG Question 1: A 60-year-old woman is brought to the emergency department by her husband because of worsening shortness of breath over the past 2 days. Last week, she had a sore throat and a low-grade fever. She has coughed up white sputum each morning for the past 2 years. She has hypertension and type 2 diabetes mellitus. She has smoked 2 packs of cigarettes daily for 35 years. Current medications include metformin and lisinopril. On examination, she occasionally has to catch her breath between sentences. Her temperature is 38.1°C (100.6°F), pulse is 85/min, respirations are 16/min, and blood pressure is 140/70 mm Hg. Expiratory wheezes with a prolonged expiratory phase are heard over both lung fields. Arterial blood gas analysis on room air shows:
pH 7.33
PCO2 53 mm Hg
PO2 68 mm Hg
An x-ray of the chest shows hyperinflation of bilateral lung fields and flattening of the diaphragm. Which of the following additional findings is most likely in this patient?
- A. Decreased urinary bicarbonate excretion (Correct Answer)
- B. Decreased urinary chloride concentration
- C. Increased serum anion gap
- D. Increased urine osmolar gap
- E. Increased urinary pH
Respiratory regulation of acid-base Explanation: ***Decreased urinary bicarbonate excretion***
- The patient's ABG results (pH 7.33, PCO2 53 mmHg) indicate **chronic respiratory acidosis**, consistent with a **COPD exacerbation** on a background of chronic disease.
- In chronic respiratory acidosis, the kidneys compensate by **retaining bicarbonate** (increasing reabsorption) and **excreting hydrogen ions** to normalize pH.
- Therefore, urinary bicarbonate excretion is **decreased** as the kidneys conserve bicarbonate to buffer the chronic acidosis.
*Decreased urinary chloride concentration*
- This is typically seen in states of **metabolic alkalosis** (with volume contraction) or profound **volume depletion**, neither of which is the primary condition here.
- The patient has respiratory acidosis, not metabolic alkalosis.
*Increased serum anion gap*
- An increased anion gap indicates **metabolic acidosis** due to accumulation of unmeasured anions (e.g., lactate, ketones, toxins).
- The patient has **respiratory acidosis**, not metabolic acidosis with an anion gap.
- The anion gap is not directly affected by primary respiratory disorders.
*Increased urine osmolar gap*
- An increased urine osmolar gap suggests the presence of **unmeasured osmolytes** in the urine (e.g., from methanol or ethylene glycol ingestion).
- There is nothing in the patient's presentation to suggest toxic ingestion.
*Increased urinary pH*
- Increased urinary pH would occur if the kidneys were **excreting bicarbonate**, which happens in metabolic alkalosis or renal tubular acidosis.
- In chronic respiratory acidosis, the kidneys compensate by **excreting acid** (lowering urinary pH) and **retaining bicarbonate**.
- Therefore, urinary pH would be **decreased**, not increased.
Respiratory regulation of acid-base US Medical PG Question 2: A 39-year-old woman is brought to the emergency room by her husband because of severe dyspnea and dizziness. Her symptoms started suddenly 30 minutes ago. She appears distressed. Arterial blood gas shows a pH of 7.51, pO2 of 100 mm Hg, and a pCO2 of 30 mm Hg. Which of the following is the most likely cause?
- A. Myasthenia gravis
- B. Opioid toxicity
- C. Panic attack (Correct Answer)
- D. Epiglottitis
- E. Pulmonary fibrosis
Respiratory regulation of acid-base Explanation: ***Panic attack***
- The sudden onset of **severe dyspnea** and **dizziness** in a distressed patient, along with ABG results indicating **respiratory alkalosis** (pH 7.51, pCO2 30 mm Hg), is highly characteristic of a panic attack with hyperventilation.
- **Hyperventilation** leads to excessive CO2 exhalation, causing the pCO2 to drop and the pH to rise, resulting in symptoms like lightheadedness and dyspnea.
*Myasthenia gravis*
- This is a **neuromuscular disorder** causing muscle weakness, which can lead to respiratory compromise over time, but typically does not present with such acute, sudden dyspnea and dizziness without prior symptoms.
- The ABG findings of respiratory alkalosis are not typical for a primary myasthenic crisis, which would likely show respiratory acidosis if respiratory failure were imminent.
*Opioid toxicity*
- Opioid overdose causes **respiratory depression**, leading to reduced respiratory rate and shallow breathing, which would result in **respiratory acidosis** (increased pCO2 and decreased pH), not alkalosis.
- The patient's pO2 of 100 mm Hg also argues against significant respiratory depression.
*Epiglottitis*
- Epiglottitis presents with a **rapidly worsening sore throat**, difficulty swallowing, drooling, and stridor, indicating upper airway obstruction.
- While it causes severe dyspnea, the ABG would likely show signs of hypoxemia and potentially acidosis due to airway compromise, not hyperventilation-induced alkalosis.
*Pulmonary fibrosis*
- This is a **chronic interstitial lung disease** that causes progressive dyspnea, often with a dry cough.
- The onset of symptoms is typically gradual, over months to years, not sudden within 30 minutes, and ABG would likely show hypoxemia with compensated respiratory alkalosis or acidosis depending on the stage, but not acutely severe hyperventilation-induced alkalosis.
Respiratory regulation of acid-base US Medical PG Question 3: A 24-year-old woman presents to the emergency department after she was found agitated and screaming for help in the middle of the street. She says she also has dizziness and tingling in the lips and hands. Her past medical history is relevant for general anxiety disorder, managed medically with paroxetine. At admission, her pulse is 125/min, respiratory rate is 25/min, and body temperature is 36.5°C (97.7°F). Physical examination is unremarkable. An arterial blood gas sample is taken. Which of the following results would you most likely expect to see in this patient?
- A. pH: increased, HCO3-: increased, Pco2: increased
- B. pH: decreased, HCO3-: decreased, Pco2: decreased
- C. pH: decreased, HCO3-: increased, Pco2: increased
- D. pH: increased, HCO3-: decreased, Pco2: decreased (Correct Answer)
- E. pH: normal, HCO3-: increased, Pco2: increased
Respiratory regulation of acid-base Explanation: ***pH: increased, HCO3-: decreased, Pco2: decreased***
- The patient's presentation with **agitation**, **dizziness**, **paresthesias** (tingling in lips and hands), and **tachypnea** (respiratory rate 25/min) is highly suggestive of **hyperventilation** due to an anxiety attack.
- **Hyperventilation** leads to excessive **CO2 expulsion**, causing a decrease in Pco2, which results in respiratory alkalosis (increased pH) and a compensatory decrease in HCO3-.
*pH: increased, HCO3-: increased, Pco2: increased*
- An **increased pH** coupled with **increased HCO3-** and **increased Pco2** would suggest a **metabolic alkalosis with respiratory compensation**, which is not consistent with the patient's acute hyperventilation.
- While pH is increased, the other values contradict the primary respiratory cause suggested by the symptoms.
*pH: decreased, HCO3-: decreased, Pco2: decreased*
- This profile describes **metabolic acidosis with respiratory compensation**, which would typically present with **Kussmaul breathing** and other signs of acidosis, not acute hyperventilation and agitation.
- Symptoms such as dizziness and tingling are associated with alkalosis, not acidosis.
*pH: decreased, HCO3-: increased, Pco2: increased*
- This pattern is characteristic of **respiratory acidosis with metabolic compensation**, often seen in conditions like **COPD exacerbation** or **opioid overdose** with hypoventilation.
- The patient's rapid breathing and clinical picture are not consistent with respiratory acidosis.
*pH: normal, HCO3-: increased, Pco2: increased*
- A **normal pH** with **increased HCO3-** and **increased Pco2** would indicate a **compensated metabolic alkalosis**.
- Her acute symptoms point to an uncompensated or acutely compensated respiratory disorder, not a compensated metabolic issue.
Respiratory regulation of acid-base US Medical PG Question 4: A histological examination of the carotid body reveals glomus cells containing dense-core vesicles. These cells function primarily as chemoreceptors for which of the following?
- A. Partial pressure of oxygen (Correct Answer)
- B. Blood pH
- C. Temperature
- D. Blood glucose levels
Respiratory regulation of acid-base Explanation: ***Partial pressure of oxygen***
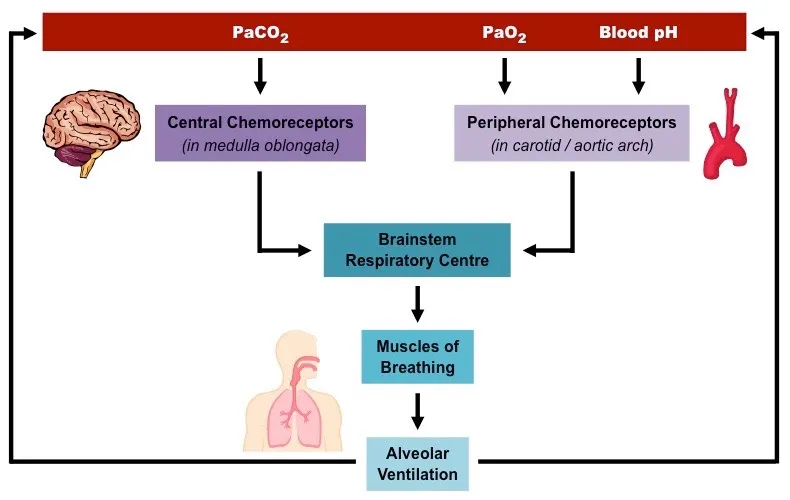
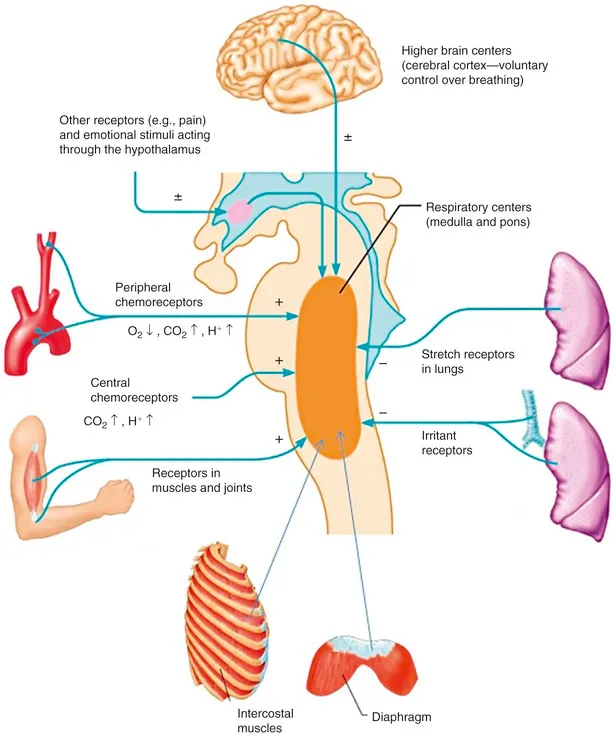
- Carotid body **glomus cells** are highly specialized **chemoreceptors** that primarily sense changes in the **partial pressure of oxygen (PO2)** in arterial blood.
- When PO2 decreases (e.g., hypoxia), these cells are activated and stimulate the respiratory and cardiovascular systems to increase oxygen uptake.
*Blood pH*
- While carotid body chemoreceptors can sense large changes in blood pH, their primary and most sensitive role is in detecting changes in **PO2**.
- Central chemoreceptors in the brainstem are more crucial for routine regulation of respiration in response to changes in **pH and PCO2**.
*Temperature*
- **Thermoreceptors** located in the skin, hypothalamus, and other internal organs are responsible for sensing body temperature, not the carotid body.
- The carotid body's main function is related to blood gas homeostasis, not temperature regulation.
*Blood glucose levels*
- Blood glucose levels are regulated by specialized cells in the **pancreas** (islets of Langerhans) that secrete hormones like insulin and glucagon.
- The carotid body is not directly involved in sensing or regulating glucose homeostasis.
Respiratory regulation of acid-base US Medical PG Question 5: A 52-year-old man with a history of Type 1 diabetes mellitus presents to the emergency room with increasing fatigue. Two days ago, he ran out of insulin and has not had time to obtain a new prescription. He denies fevers or chills. His temperature is 37.2 degrees Celsius, blood pressure 84/56 mmHg, heart rate 100/min, respiratory rate 20/min, and SpO2 97% on room air. His physical exam is otherwise within normal limits. An arterial blood gas analysis shows the following:
pH 7.25, PCO2 29, PO2 95, HCO3- 15.
Which of the following acid-base disorders is present?
- A. Respiratory alkalosis with appropriate metabolic compensation
- B. Respiratory acidosis with appropriate metabolic compensation
- C. Mixed metabolic and respiratory acidosis
- D. Metabolic acidosis with appropriate respiratory compensation (Correct Answer)
- E. Metabolic alkalosis with appropriate respiratory compensation
Respiratory regulation of acid-base Explanation: ***Metabolic acidosis with appropriate respiratory compensation***
- The patient's pH of 7.25 and HCO3- of 15 indicate **metabolic acidosis**, while the PCO2 of 29 indicates **respiratory compensation**.
- The compensation is **appropriate** as suggested by Winter's formula [Expected PCO2 = (1.5 x HCO3-) + 8 +/- 2; (1.5 x 15) + 8 = 30.5, which is close to 29].
*Respiratory alkalosis with appropriate metabolic compensation*
- This would involve a **pH > 7.45** and **low PCO2** with a secondary drop in HCO3-, which is not seen here.
- The patient's primary problem is a metabolic disturbance due to insulin deficiency.
*Respiratory acidosis with appropriate metabolic compensation*
- This disorder is characterized by a **low pH** and a **high PCO2**, with a secondary rise in HCO3-.
- The patient's PCO2 is low, indicating a compensatory response rather than a primary respiratory acidosis.
*Mixed metabolic and respiratory acidosis*
- A mixed disorder would show a **low pH** due to both **low HCO3-** and **high PCO2**.
- The patient's PCO2 is low, indicating a compensatory response to metabolic acidosis, not an additional respiratory acidosis.
*Metabolic alkalosis with appropriate respiratory compensation*
- This would present with a **high pH (>7.45)** and **high HCO3-**, with compensatory **elevated PCO2**.
- The patient's pH and HCO3- are low, indicating acidosis, not alkalosis.
Respiratory regulation of acid-base US Medical PG Question 6: A 55-year-old man presents with an unremitting cough and swelling of the lower limbs for the past 2 weeks. He says he has had a chronic cough for years, however, he feels it is getting worse. He reports a 30-pack-year smoking history. Physical examination reveals mild central cyanosis and expiratory wheezes throughout the chest. Oxygen therapy is ordered immediately but, soon after administering it, his respiratory rate starts to slow down and he becomes drowsy. Dysfunction of which of the following receptors most likely led to this patient’s current condition?
- A. Pleural pain receptors
- B. Central chemoreceptors
- C. Airway stretch receptors
- D. Pulmonary stretch receptors
- E. Peripheral chemoreceptors (Correct Answer)
Respiratory regulation of acid-base Explanation: ***Peripheral chemoreceptors***
- In patients with chronic obstructive pulmonary disease (COPD) like this patient, the **central chemoreceptors** become desensitized to chronically elevated CO2 levels. Their primary respiratory drive then shifts to the **peripheral chemoreceptors** (carotid and aortic bodies), which are sensitive to **hypoxia**.
- Administering high-flow oxygen **eliminates the hypoxic stimulus** sensed by these normally functioning peripheral chemoreceptors, removing the hypoxic drive to breathe and leading to **hypoventilation, CO2 retention, respiratory acidosis**, and drowsiness (CO2 narcosis).
*Pleural pain receptors*
- These receptors are primarily involved in sensing pain associated with **pleural inflammation** or injury, contributing to the sensation of pain with breathing.
- They do not play a role in regulating the primary ventilatory drive in response to blood gas changes.
*Central chemoreceptors*
- These receptors are located in the **medulla** and are primarily sensitive to changes in **arterial PCO2** and pH (via H+ ions in CSF).
- In chronic respiratory diseases with CO2 retention, they become **desensitized** to elevated CO2, shifting the main respiratory drive to the peripheral chemoreceptors' response to hypoxia.
*Airway stretch receptors*
- These receptors, including **slowly adapting stretch receptors** and **rapidly adapting irritant receptors**, are located in the airways and respond to lung inflation and irritants.
- They are involved in the Hering-Breuer reflex and cough reflex but are not the primary drivers of ventilation in response to hypoxemia.
*Pulmonary stretch receptors*
- These receptors are located in the **bronchial smooth muscle** and respond to lung distension, contributing to the **Hering-Breuer reflex** which inhibits inspiration to prevent overinflation.
- While important for lung mechanics, they do not directly sense blood gas levels to drive ventilation in the context of hypoxia or hypercapnia.
Respiratory regulation of acid-base US Medical PG Question 7: A 25-year-old woman with an extensive psychiatric history is suspected of having metabolic acidosis after ingesting a large amount of aspirin in a suicide attempt. Labs are drawn and the values from the ABG are found to be: PCO2: 25, and HCO3: 15, but the pH value is smeared on the print-out and illegible. The medical student is given the task of calculating the pH using the pCO2 and HCO3 concentrations. He recalls from his first-year physiology course that the pKa of relevance for the bicarbonate buffering system is approximately 6.1. Which of the following is the correct formula the student should use, using the given values from the incomplete ABG?
- A. 15/6.1 + log[10/(0.03*25)]
- B. 6.1 + log[15/(0.03*25)] (Correct Answer)
- C. 10^6.1 + 15/0.03*25
- D. 6.1 + log[0.03/15*25]
- E. 6.1 + log[25/(15*0.03)]
Respiratory regulation of acid-base Explanation: ***6.1 + log[15/(0.03*25)]***
- This formula correctly represents the Henderson-Hasselbalch equation for the bicarbonate buffer system: **pH = pKa + log([HCO3-]/[0.03 * PCO2])**.
- Here, **pKa is 6.1**, **[HCO3-] is 15**, and **[0.03 * PCO2] is 0.03 * 25**, making this the appropriate calculation for pH.
*15/6.1 + log[10/(0.03*25)]*
- This formula incorrectly places the pKa in the denominator of the first term and introduces an arbitrary '10' in the numerator of the logarithmic term.
- The **Henderson-Hasselbalch equation** dictates that pKa is added, not divided into, another component, and the logarithmic term should reflect the ratio of bicarbonate to carbonic acid.
*10^6.1 + 15/0.03*25*
- This option incorrectly uses an exponentiation of pKa and adds it to an unrelated fractional term, which does not correspond to the Henderson-Hasselbalch equation structure.
- The formula for pH calculation is a sum of pKa and a logarithmic term, not an exponentiation and a simple fraction.
*6.1 + log[0.03/15*25]*
- This option incorrectly inverts the ratio within the logarithm, placing the carbonic acid component (0.03 * PCO2) in the numerator and bicarbonate in the denominator.
- The correct Henderson-Hasselbalch equation requires the **bicarbonate concentration in the numerator** and the carbonic acid concentration in the denominator.
*6.1 + log [25/(15*0.03)]*
- This option incorrectly places the PCO2 (25) in the numerator of the logarithmic term and the product of HCO3- and 0.03 in the denominator.
- The correct ratio for the Henderson-Hasselbalch equation is **[HCO3-] / [0.03 * PCO2]**.
Respiratory regulation of acid-base US Medical PG Question 8: A 58-year-old man presents to the emergency department with a chief complaint of ringing in his ears that started several hours previously that has progressed to confusion. The patient denies any history of medical problems except for bilateral knee arthritis. He was recently seen by an orthopedic surgeon to evaluate his bilateral knee arthritis but has opted to not undergo knee replacement and prefers medical management. His wife noted that prior to them going on a hike today, he seemed confused and not himself. They decided to stay home, and roughly 14 hours later, he was no longer making any sense. Physical exam is notable for a confused man. The patient's vitals are being performed and his labs are being drawn. Which of the following is most likely to be seen on blood gas analysis?
- A. pH: 7.30, PaCO2: 15 mmHg, HCO3-: 16 mEq/L (Correct Answer)
- B. pH: 7.37, PaCO2: 41 mmHg, HCO3-: 12 mEq/L
- C. pH: 7.41, PaCO2: 65 mmHg, HCO3-: 34 mEq/L
- D. pH: 7.47, PaCO2: 11 mmHg, HCO3-: 24 mEq/L
- E. pH: 7.31, PaCO2: 31 mmHg, HCO3-: 15 mEq/L
Respiratory regulation of acid-base Explanation: ***pH: 7.30, PaCO2: 15 mmHg, HCO3-: 16 mEq/L***
- This blood gas analysis shows a **low pH** (acidemia), **low PaCO2** (hypocapnia), and **low HCO3-** (bicarbonate). This pattern is consistent with a **primary metabolic acidosis** with a **compensatory respiratory alkalosis**.
- In this clinical scenario, the patient likely has **salicylate toxicity** (aspirin poisoning). Salicylate toxicity initially causes respiratory alkalosis due to direct stimulation of the respiratory center, followed by a high anion gap metabolic acidosis as salicylates interfere with cellular metabolism. This specific ABG reflects a mixed disorder where metabolic acidosis is predominant and respiratory compensation is attempting to raise the pH. The **tinnitus** and **confusion** are classic symptoms of salicylate toxicity.
*pH: 7.37, PaCO2: 41 mmHg, HCO3-: 12 mEq/L*
- This blood gas shows a **normal pH**, **normal PaCO2**, and **low HCO3-**. This suggests a **compensated metabolic acidosis**, where the body has fully compensated to bring the pH back to normal.
- While the patient likely has metabolic acidosis from salicylate toxicity, full compensation to a normal pH is less characteristic of an acute, severe presentation with significant neurological symptoms.
*pH: 7.41, PaCO2: 65 mmHg, HCO3-: 34 mEq/L*
- This blood gas shows a **normal pH**, **high PaCO2**, and **high HCO3-**. This indicates a **compensated respiratory acidosis**, where the kidneys have compensated for chronic CO2 retention.
- This pattern is not consistent with salicylate toxicity, which typically causes **respiratory alkalosis** early on, and later **metabolic acidosis**.
*pH: 7.47, PaCO2: 11 mmHg, HCO3-: 24 mEq/L*
- This blood gas analysis shows a **high pH** (alkalemia), **very low PaCO2** (severe hypocapnia), and a **normal HCO3-**. This indicates a **primary respiratory alkalosis** with no significant metabolic compensation.
- While salicylate toxicity can cause respiratory alkalosis, severe confusion and the progression of symptoms suggest a more advanced stage, usually involving a metabolic acidosis component, making a pure, uncompensated respiratory alkalosis less likely.
*pH: 7.31, PaCO2: 31 mmHg, HCO3-: 15 mEq/L*
- This blood gas shows a **low pH**, **low PaCO2**, and **low HCO3-**. This also indicates a **metabolic acidosis** with **respiratory compensation**.
- However, compared to pH 7.30, PaCO2 15 mmHg, and HCO3- 16 mEq/L, this option shows slightly **less severe respiratory compensation** (PaCO2 is higher), which is less typical for the profound respiratory stimulation seen in severe salicylate poisoning. The chosen correct option demonstrates a more characteristic and maximal respiratory compensation for the degree of metabolic acidosis.
Respiratory regulation of acid-base US Medical PG Question 9: A 32-year-old woman is admitted to the emergency department for 36 hours of intense left-sided back pain that extends into her left groin. She reports that the pain started a day after a charitable 5 km (3.1 mi) marathon. The past medical history is relevant for multiple complaints of eye dryness and dry mouth. Physical examination is unremarkable, except for intense left-sided costovertebral pain. The results from laboratory tests are shown.
Laboratory test Result
Serum Na+ 137
Serum Cl- 110
Serum K+ 3.0
Serum creatinine (SCr) 0.82
Arterial blood gas Result
pH 7.28
pO2 98 mm Hg
pCO2 28.5 mm Hg
SaO2% 98%
HCO3- 15 mm Hg
Which of the following explains this patient’s condition?
- A. Carbonic acid accumulation
- B. Decreased bicarbonate renal absorption
- C. Decreased renal excretion of hydrogen ions (H+) (Correct Answer)
- D. Decreased synthesis of ammonia (NH3)
- E. Decreased excretion of nonvolatile acids
Respiratory regulation of acid-base Explanation: ***Decreased renal excretion of hydrogen ions (H+)***
- The patient presents with **metabolic acidosis** (pH 7.28, HCO3- 15 mEq/L) with **respiratory compensation** (pCO2 28.5 mm Hg). The anion gap is **normal** (Na+ - (Cl- + HCO3-) = 137 - (110 + 15) = **12 mEq/L**), indicating a **non-anion gap metabolic acidosis**.
- The history of **dry eyes and dry mouth** strongly suggests **Sjögren syndrome**, which is commonly associated with **Type 1 (distal) renal tubular acidosis**.
- In **Type 1 RTA**, the distal tubule alpha-intercalated cells cannot adequately secrete H+ ions, leading to metabolic acidosis with **inability to acidify urine** (urine pH > 5.5). Associated findings include **hypokalemia** (K+ 3.0), **nephrolithiasis** (calcium phosphate stones due to alkaline urine), and hypercalciuria.
- The left-sided flank pain radiating to the groin is consistent with **nephrolithiasis**, a common complication of Type 1 RTA.
*Carbonic acid accumulation*
- **Carbonic acid accumulation** indicates **respiratory acidosis** with elevated pCO2, which is not present here.
- The patient has a **low pCO2 (28.5 mm Hg)**, representing appropriate **respiratory compensation** for the primary metabolic acidosis.
*Decreased bicarbonate renal absorption*
- **Decreased bicarbonate renal absorption** characterizes **Type 2 (proximal) RTA**.
- While Type 2 RTA also causes non-anion gap metabolic acidosis, it is **not typically associated with Sjögren syndrome** and would present with different features (glycosuria, aminoaciduria, phosphaturia as part of Fanconi syndrome).
- Type 2 RTA can acidify urine to pH < 5.5 when serum HCO3- is low, unlike Type 1 RTA.
*Decreased synthesis of ammonia (NH3)*
- **Decreased ammonia synthesis** is characteristic of **Type 4 RTA** or severe chronic kidney disease.
- Type 4 RTA presents with **hyperkalemia** (due to hypoaldosteronism), not the hypokalemia seen in this patient.
- The normal serum creatinine (0.82 mg/dL) rules out significant renal failure.
*Decreased excretion of nonvolatile acids*
- **Decreased excretion of nonvolatile acids** would cause **elevated anion gap metabolic acidosis** (e.g., lactic acidosis, ketoacidosis, or advanced renal failure with accumulation of organic acids).
- This patient has a **normal anion gap (12 mEq/L)** and **normal renal function** (creatinine 0.82 mg/dL), making this mechanism unlikely.
- The clinical context of Sjögren syndrome with dry eyes/mouth points specifically to distal RTA.
Respiratory regulation of acid-base US Medical PG Question 10: A 24-year-old male is brought in by ambulance to the emergency department after he was found unresponsive at home for an unknown length of time. Upon arrival, he is found to be severely altered and unable to answer questions about his medical history. Based on clinical suspicion, a panel of basic blood tests are obtained including an arterial blood gas, which shows a pH of 7.32, a pCO2 of 70, and a bicarbonate level of 30 mEq/L. Which of the following is most likely the primary disturbance leading to the values found in the ABG?
- A. Respiratory acidosis (Correct Answer)
- B. Metabolic alkalosis
- C. Respiratory alkalosis
- D. Metabolic acidosis
- E. Mixed alkalosis
Respiratory regulation of acid-base Explanation: ***Respiratory acidosis***
- The **pH (7.32)** is acidic (normal 7.35-7.45), and the **pCO2 (70 mmHg)** is significantly elevated (normal 35-45 mmHg), indicating **primary respiratory acidosis** due to hypoventilation.
- The **bicarbonate (30 mEq/L)** is elevated above normal (22-26 mEq/L), indicating **partial metabolic compensation** by the kidneys retaining bicarbonate to buffer the acidosis.
- This pattern suggests **chronic respiratory acidosis** (e.g., from COPD, CNS depression, neuromuscular disease) with renal compensation.
*Metabolic alkalosis*
- This would present with **elevated pH** (>7.45) and **elevated bicarbonate** as the primary disturbance, often with compensatory elevation in pCO2.
- The patient's **pH is acidic (7.32)**, not alkalotic, ruling out metabolic alkalosis as the primary process.
*Respiratory alkalosis*
- This would present with **elevated pH** (>7.45) and **decreased pCO2** (<35 mmHg) due to hyperventilation.
- The patient has the opposite: **acidic pH and elevated pCO2**, ruling out respiratory alkalosis.
*Metabolic acidosis*
- This would present with **decreased pH** and **decreased bicarbonate** (<22 mEq/L) as the primary disturbance.
- While the pH is low, the **bicarbonate is elevated (30 mEq/L)**, not decreased, ruling out metabolic acidosis as the primary disorder.
*Mixed alkalosis*
- A mixed alkalosis would involve simultaneous respiratory and metabolic processes causing **elevated pH**.
- The patient's **pH is acidic (7.32)**, making any form of alkalosis impossible as the primary disturbance.
More Respiratory regulation of acid-base US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.