Respiratory alkalosis mechanisms and compensation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Respiratory alkalosis mechanisms and compensation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Respiratory alkalosis mechanisms and compensation US Medical PG Question 1: A 24-year-old woman presents to the emergency department after she was found agitated and screaming for help in the middle of the street. She says she also has dizziness and tingling in the lips and hands. Her past medical history is relevant for general anxiety disorder, managed medically with paroxetine. At admission, her pulse is 125/min, respiratory rate is 25/min, and body temperature is 36.5°C (97.7°F). Physical examination is unremarkable. An arterial blood gas sample is taken. Which of the following results would you most likely expect to see in this patient?
- A. pH: increased, HCO3-: increased, Pco2: increased
- B. pH: decreased, HCO3-: decreased, Pco2: decreased
- C. pH: decreased, HCO3-: increased, Pco2: increased
- D. pH: increased, HCO3-: decreased, Pco2: decreased (Correct Answer)
- E. pH: normal, HCO3-: increased, Pco2: increased
Respiratory alkalosis mechanisms and compensation Explanation: ***pH: increased, HCO3-: decreased, Pco2: decreased***
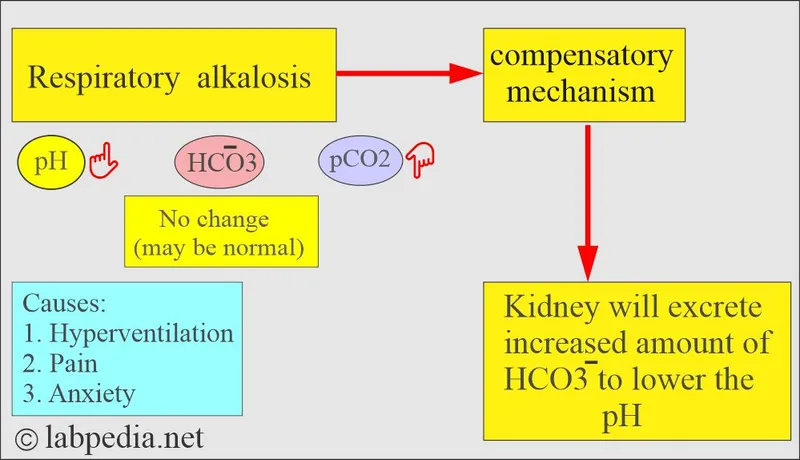
- The patient's presentation with **agitation**, **dizziness**, **paresthesias** (tingling in lips and hands), and **tachypnea** (respiratory rate 25/min) is highly suggestive of **hyperventilation** due to an anxiety attack.
- **Hyperventilation** leads to excessive **CO2 expulsion**, causing a decrease in Pco2, which results in respiratory alkalosis (increased pH) and a compensatory decrease in HCO3-.
*pH: increased, HCO3-: increased, Pco2: increased*
- An **increased pH** coupled with **increased HCO3-** and **increased Pco2** would suggest a **metabolic alkalosis with respiratory compensation**, which is not consistent with the patient's acute hyperventilation.
- While pH is increased, the other values contradict the primary respiratory cause suggested by the symptoms.
*pH: decreased, HCO3-: decreased, Pco2: decreased*
- This profile describes **metabolic acidosis with respiratory compensation**, which would typically present with **Kussmaul breathing** and other signs of acidosis, not acute hyperventilation and agitation.
- Symptoms such as dizziness and tingling are associated with alkalosis, not acidosis.
*pH: decreased, HCO3-: increased, Pco2: increased*
- This pattern is characteristic of **respiratory acidosis with metabolic compensation**, often seen in conditions like **COPD exacerbation** or **opioid overdose** with hypoventilation.
- The patient's rapid breathing and clinical picture are not consistent with respiratory acidosis.
*pH: normal, HCO3-: increased, Pco2: increased*
- A **normal pH** with **increased HCO3-** and **increased Pco2** would indicate a **compensated metabolic alkalosis**.
- Her acute symptoms point to an uncompensated or acutely compensated respiratory disorder, not a compensated metabolic issue.
Respiratory alkalosis mechanisms and compensation US Medical PG Question 2: A 66-year-old man is brought to the emergency department by his daughter because of 3 days of fever, chills, cough, and shortness of breath. The cough is productive of yellow sputum. His symptoms have not improved with rest and guaifenesin. His past medical history is significant for hypertension, for which he takes hydrochlorothiazide. He has a 30-pack-year history of smoking. His temperature is 38.9 C (102.0 F), blood pressure 88/56 mm Hg, and heart rate 105/min. Following resuscitation with normal saline, his blood pressure improves to 110/70 mm Hg. His arterial blood gas is as follows:
Blood pH 7.52, PaO2 74 mm Hg, PaCO2 28 mm Hg, and HCO3- 21 mEq/L.
Which of the following acid-base disturbances best characterizes this patient's condition?
- A. Metabolic acidosis
- B. Respiratory acidosis
- C. Respiratory alkalosis (Correct Answer)
- D. Normal acid-base status
- E. Metabolic alkalosis
Respiratory alkalosis mechanisms and compensation Explanation: ***Respiratory alkalosis***
- The patient's pH of **7.52** indicates alkalemia. A **PaCO2 of 28 mm Hg** (normal range 35-45 mm Hg) is low, indicating a respiratory component.
- The **primary disturbance is respiratory alkalosis** due to hyperventilation from pneumonia/sepsis causing tachypnea and increased CO2 elimination.
- The HCO3- of 21 mEq/L (normal range 22-26 mEq/L) is at the lower limit of normal. In acute respiratory alkalosis, bicarbonate remains near normal since **metabolic compensation takes 2-3 days** to develop significantly.
- With a 3-day history, minimal renal compensation is expected, consistent with the near-normal bicarbonate.
*Metabolic acidosis*
- Metabolic acidosis would present with a **low pH** and a **low HCO3-**, which is not seen here.
- The patient's pH is **alkaline (7.52)**, not acidic, ruling out this diagnosis.
*Respiratory acidosis*
- Respiratory acidosis would be characterized by a **low pH** and a **high PaCO2**, indicating hypoventilation.
- The patient's **PaCO2 is low (28 mm Hg)** and the **pH is high**, directly contradicting respiratory acidosis.
*Normal acid-base status*
- A normal acid-base status would have a **pH between 7.35 and 7.45** and PaCO2 between 35-45 mm Hg.
- The patient's **pH of 7.52** and **PaCO2 of 28 mm Hg** are both abnormal, specifically indicating alkalemia and hypocapnia.
*Metabolic alkalosis*
- Metabolic alkalosis would feature a **high pH** and a **high HCO3-** (typically >26 mEq/L), often resulting from conditions like vomiting or diuretic use.
- While the patient is on hydrochlorothiazide, his **HCO3- is 21 mEq/L** (low-normal, not elevated), indicating this is not a primary metabolic alkalosis.
Respiratory alkalosis mechanisms and compensation US Medical PG Question 3: A 24-year-old male is brought in by ambulance to the emergency department after he was found unresponsive at home for an unknown length of time. Upon arrival, he is found to be severely altered and unable to answer questions about his medical history. Based on clinical suspicion, a panel of basic blood tests are obtained including an arterial blood gas, which shows a pH of 7.32, a pCO2 of 70, and a bicarbonate level of 30 mEq/L. Which of the following is most likely the primary disturbance leading to the values found in the ABG?
- A. Respiratory acidosis (Correct Answer)
- B. Metabolic alkalosis
- C. Respiratory alkalosis
- D. Metabolic acidosis
- E. Mixed alkalosis
Respiratory alkalosis mechanisms and compensation Explanation: ***Respiratory acidosis***
- The **pH (7.32)** is acidic (normal 7.35-7.45), and the **pCO2 (70 mmHg)** is significantly elevated (normal 35-45 mmHg), indicating **primary respiratory acidosis** due to hypoventilation.
- The **bicarbonate (30 mEq/L)** is elevated above normal (22-26 mEq/L), indicating **partial metabolic compensation** by the kidneys retaining bicarbonate to buffer the acidosis.
- This pattern suggests **chronic respiratory acidosis** (e.g., from COPD, CNS depression, neuromuscular disease) with renal compensation.
*Metabolic alkalosis*
- This would present with **elevated pH** (>7.45) and **elevated bicarbonate** as the primary disturbance, often with compensatory elevation in pCO2.
- The patient's **pH is acidic (7.32)**, not alkalotic, ruling out metabolic alkalosis as the primary process.
*Respiratory alkalosis*
- This would present with **elevated pH** (>7.45) and **decreased pCO2** (<35 mmHg) due to hyperventilation.
- The patient has the opposite: **acidic pH and elevated pCO2**, ruling out respiratory alkalosis.
*Metabolic acidosis*
- This would present with **decreased pH** and **decreased bicarbonate** (<22 mEq/L) as the primary disturbance.
- While the pH is low, the **bicarbonate is elevated (30 mEq/L)**, not decreased, ruling out metabolic acidosis as the primary disorder.
*Mixed alkalosis*
- A mixed alkalosis would involve simultaneous respiratory and metabolic processes causing **elevated pH**.
- The patient's **pH is acidic (7.32)**, making any form of alkalosis impossible as the primary disturbance.
Respiratory alkalosis mechanisms and compensation US Medical PG Question 4: A 52-year-old man with a history of Type 1 diabetes mellitus presents to the emergency room with increasing fatigue. Two days ago, he ran out of insulin and has not had time to obtain a new prescription. He denies fevers or chills. His temperature is 37.2 degrees Celsius, blood pressure 84/56 mmHg, heart rate 100/min, respiratory rate 20/min, and SpO2 97% on room air. His physical exam is otherwise within normal limits. An arterial blood gas analysis shows the following:
pH 7.25, PCO2 29, PO2 95, HCO3- 15.
Which of the following acid-base disorders is present?
- A. Respiratory alkalosis with appropriate metabolic compensation
- B. Respiratory acidosis with appropriate metabolic compensation
- C. Mixed metabolic and respiratory acidosis
- D. Metabolic acidosis with appropriate respiratory compensation (Correct Answer)
- E. Metabolic alkalosis with appropriate respiratory compensation
Respiratory alkalosis mechanisms and compensation Explanation: ***Metabolic acidosis with appropriate respiratory compensation***
- The patient's pH of 7.25 and HCO3- of 15 indicate **metabolic acidosis**, while the PCO2 of 29 indicates **respiratory compensation**.
- The compensation is **appropriate** as suggested by Winter's formula [Expected PCO2 = (1.5 x HCO3-) + 8 +/- 2; (1.5 x 15) + 8 = 30.5, which is close to 29].
*Respiratory alkalosis with appropriate metabolic compensation*
- This would involve a **pH > 7.45** and **low PCO2** with a secondary drop in HCO3-, which is not seen here.
- The patient's primary problem is a metabolic disturbance due to insulin deficiency.
*Respiratory acidosis with appropriate metabolic compensation*
- This disorder is characterized by a **low pH** and a **high PCO2**, with a secondary rise in HCO3-.
- The patient's PCO2 is low, indicating a compensatory response rather than a primary respiratory acidosis.
*Mixed metabolic and respiratory acidosis*
- A mixed disorder would show a **low pH** due to both **low HCO3-** and **high PCO2**.
- The patient's PCO2 is low, indicating a compensatory response to metabolic acidosis, not an additional respiratory acidosis.
*Metabolic alkalosis with appropriate respiratory compensation*
- This would present with a **high pH (>7.45)** and **high HCO3-**, with compensatory **elevated PCO2**.
- The patient's pH and HCO3- are low, indicating acidosis, not alkalosis.
Respiratory alkalosis mechanisms and compensation US Medical PG Question 5: What is the primary mechanism for maintaining acid-base balance during prolonged vomiting?
- A. Increased chloride reabsorption
- B. Increased potassium excretion
- C. Increased bicarbonate excretion (Correct Answer)
- D. Decreased hydrogen secretion
Respiratory alkalosis mechanisms and compensation Explanation: ***Increased bicarbonate excretion***
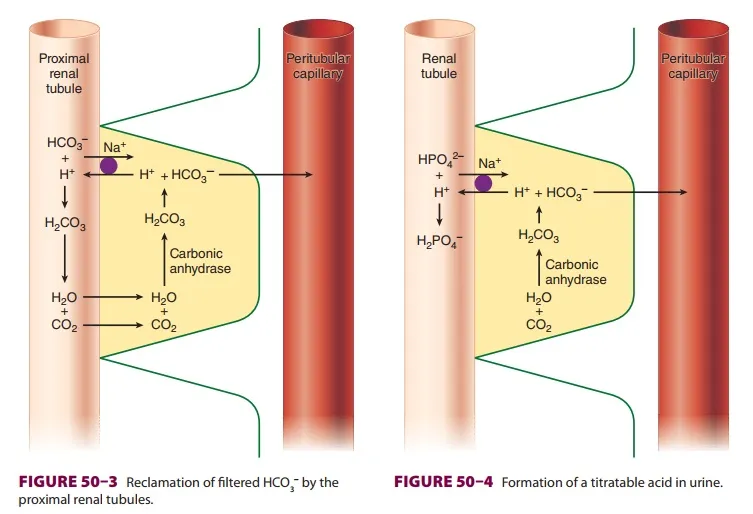
- Prolonged vomiting leads to the loss of **gastric acid (HCl)**, causing **metabolic alkalosis**. The kidneys compensate by increasing the excretion of **bicarbonate (HCO3-)** to restore acid-base balance.
- This renal compensation is the primary mechanism to eliminate the excess alkali from the body.
*Increased chloride reabsorption*
- In **metabolic alkalosis** due to vomiting, the body tends to reabsorb less chloride, not more, in an attempt to excrete bicarbonate.
- **Chloride depletion** can actually hinder bicarbonate excretion by promoting sodium reabsorption with bicarbonate.
*Increased potassium excretion*
- **Hypokalemia** can occur with prolonged vomiting due to increased aldosterone activity and direct renal loss associated with metabolic alkalosis.
- However, increased potassium excretion itself is not the primary mechanism for correcting the acid-base disorder; rather, it is a consequence or a contributing factor to the imbalance.
*Decreased hydrogen secretion*
- In response to alkalosis, the kidneys would typically decrease, not increase, **hydrogen ion (H+) secretion** in an effort to retain H+ and normalize pH.
- Decreased H+ secretion is a compensatory mechanism, but the direct excretion of bicarbonate is more crucial for correcting the metabolic alkalosis.
Respiratory alkalosis mechanisms and compensation US Medical PG Question 6: A 22-year-old female college student presents to the emergency department due to severe pain in her stomach after an evening of heavy drinking with her friends. The pain is located in the upper half of the abdomen, is severe in intensity, and has an acute onset. She claims to have consumed a dozen alcoholic drinks. Her past medical history is unremarkable. She has recently completed an extremely low-calorie diet which resulted in her losing 10 kg (22 lb) of body weight. Her pulse is 130/min, respirations are 26/min, and blood pressure is 130/86 mm Hg. Examination reveals a visibly distressed young female with periumbilical tenderness. Her BMI is 23 kg/m2. Laboratory tests show:
Arterial blood gas analysis
pH 7.54
Po2 100 mm Hg
Pco2 23 mm Hg
HCO3- 22 mEq/L
Serum
Sodium 140 mEq/L
Potassium 3.9 mEq/L
Chloride 100 mEq/L
Which of the following most likely caused her elevated pH?
- A. Renal failure-induced electrolyte imbalance
- B. Weight loss-induced electrolyte imbalance
- C. Pain-induced hypoventilation
- D. Anxiety-induced hyperventilation (Correct Answer)
- E. Alcohol-induced respiratory depression
Respiratory alkalosis mechanisms and compensation Explanation: ***Anxiety-induced hyperventilation***
- The patient's **pH of 7.54** and **low PCO2 of 23 mm Hg** indicate **respiratory alkalosis**, a condition where the body expels too much CO2.
- Hyperventilation, often triggered by **anxiety or acute pain**, leads to excessive CO2 exhalation, causing the blood to become more alkaline.
*Renal failure-induced electrolyte imbalance*
- **Renal failure** typically leads to **metabolic acidosis** due to the kidney's inability to excrete acid or reabsorb bicarbonate, which would result in a low pH, not a high one.
- The patient's basic electrolyte levels and bicarbonate are within normal limits (aside from the pH imbalance), making renal failure unlikely to be the cause of her elevated pH.
*Weight loss-induced electrolyte imbalance*
- Rapid or significant **weight loss** might affect electrolyte levels (e.g., potassium), but it does not directly cause **respiratory alkalosis** or a primary elevation in pH.
- Her blood gas results specifically point to a respiratory cause for the alkalosis.
*Pain-induced hypoventilation*
- **Hypoventilation** means reduced breathing, which would lead to **CO2 retention** and thus **respiratory acidosis** (a decrease in pH), not alkalosis.
- While the patient is in severe pain, her breathing rate of 26 breaths/min indicates tachypnea, not hypoventilation.
*Alcohol-induced respiratory depression*
- **Alcohol intoxication** can cause **respiratory depression**, leading to reduced breathing, which results in **CO2 retention** and thus **respiratory acidosis** (low pH).
- Her elevated pH and low PCO2 clearly rule out respiratory depression as the cause of her acid-base disturbance.
Respiratory alkalosis mechanisms and compensation US Medical PG Question 7: A 25-year-old man is in the middle of an ascent up a mountain, at an elevation of about 4,500 meters. This is the 4th day of his expedition. His friend notices that in the last few hours, he has been coughing frequently and appears to be short of breath. He has used his albuterol inhaler twice in the past 4 hours, but it does not seem to help. Within the past hour, he has coughed up some frothy, slightly pink sputum and is now complaining of nausea and headache. Other than his asthma, which has been well-controlled on a steroid inhaler, he is healthy. Which of the following is the most likely cause of this man’s symptoms?
- A. An acute asthma exacerbation
- B. Non-cardiogenic pulmonary edema (Correct Answer)
- C. Pneumothorax
- D. Pulmonary embolism
- E. Acute heart failure
Respiratory alkalosis mechanisms and compensation Explanation: ***Non-cardiogenic pulmonary edema***
- The patient's symptoms of **dyspnea**, cough, and **frothy, pink sputum** at high altitude (4,500 meters) are classic signs of **High-Altitude Pulmonary Edema (HAPE)**, a form of non-cardiogenic pulmonary edema.
- The headache and nausea are consistent with **acute mountain sickness**, which often precedes HAPE, and the ineffectiveness of albuterol points away from asthma.
*An acute asthma exacerbation*
- While the patient has a history of asthma, the **frothy, pink sputum** is atypical for asthma and strongly suggests alveolar fluid.
- The ineffectiveness of albuterol, a bronchodilator, further suggests a cause other than **bronchoconstriction** as the primary issue.
*Pneumothorax*
- A pneumothorax typically presents with **sudden onset unilateral pleuritic chest pain** and dyspnea, which can be severe.
- It would not usually cause frothy, pink sputum and is not directly linked to high altitude in the absence of trauma.
*Pulmonary embolism*
- A pulmonary embolism often causes **sudden onset dyspnea, pleuritic chest pain, and sometimes hemoptysis**, but **pink, frothy sputum** is less common.
- There are no risk factors for PE mentioned, such as prolonged immobility or recent surgery.
*Acute heart failure*
- While acute heart failure can cause **pulmonary edema with frothy, pink sputum**, the patient is a young, otherwise healthy man with no cardiac risk factors.
- The context of **high altitude** strongly points to HAPE over acute heart failure as the cause of pulmonary edema.
Respiratory alkalosis mechanisms and compensation US Medical PG Question 8: A 58-year-old man presents to the emergency department with a chief complaint of ringing in his ears that started several hours previously that has progressed to confusion. The patient denies any history of medical problems except for bilateral knee arthritis. He was recently seen by an orthopedic surgeon to evaluate his bilateral knee arthritis but has opted to not undergo knee replacement and prefers medical management. His wife noted that prior to them going on a hike today, he seemed confused and not himself. They decided to stay home, and roughly 14 hours later, he was no longer making any sense. Physical exam is notable for a confused man. The patient's vitals are being performed and his labs are being drawn. Which of the following is most likely to be seen on blood gas analysis?
- A. pH: 7.30, PaCO2: 15 mmHg, HCO3-: 16 mEq/L (Correct Answer)
- B. pH: 7.37, PaCO2: 41 mmHg, HCO3-: 12 mEq/L
- C. pH: 7.41, PaCO2: 65 mmHg, HCO3-: 34 mEq/L
- D. pH: 7.47, PaCO2: 11 mmHg, HCO3-: 24 mEq/L
- E. pH: 7.31, PaCO2: 31 mmHg, HCO3-: 15 mEq/L
Respiratory alkalosis mechanisms and compensation Explanation: ***pH: 7.30, PaCO2: 15 mmHg, HCO3-: 16 mEq/L***
- This blood gas analysis shows a **low pH** (acidemia), **low PaCO2** (hypocapnia), and **low HCO3-** (bicarbonate). This pattern is consistent with a **primary metabolic acidosis** with a **compensatory respiratory alkalosis**.
- In this clinical scenario, the patient likely has **salicylate toxicity** (aspirin poisoning). Salicylate toxicity initially causes respiratory alkalosis due to direct stimulation of the respiratory center, followed by a high anion gap metabolic acidosis as salicylates interfere with cellular metabolism. This specific ABG reflects a mixed disorder where metabolic acidosis is predominant and respiratory compensation is attempting to raise the pH. The **tinnitus** and **confusion** are classic symptoms of salicylate toxicity.
*pH: 7.37, PaCO2: 41 mmHg, HCO3-: 12 mEq/L*
- This blood gas shows a **normal pH**, **normal PaCO2**, and **low HCO3-**. This suggests a **compensated metabolic acidosis**, where the body has fully compensated to bring the pH back to normal.
- While the patient likely has metabolic acidosis from salicylate toxicity, full compensation to a normal pH is less characteristic of an acute, severe presentation with significant neurological symptoms.
*pH: 7.41, PaCO2: 65 mmHg, HCO3-: 34 mEq/L*
- This blood gas shows a **normal pH**, **high PaCO2**, and **high HCO3-**. This indicates a **compensated respiratory acidosis**, where the kidneys have compensated for chronic CO2 retention.
- This pattern is not consistent with salicylate toxicity, which typically causes **respiratory alkalosis** early on, and later **metabolic acidosis**.
*pH: 7.47, PaCO2: 11 mmHg, HCO3-: 24 mEq/L*
- This blood gas analysis shows a **high pH** (alkalemia), **very low PaCO2** (severe hypocapnia), and a **normal HCO3-**. This indicates a **primary respiratory alkalosis** with no significant metabolic compensation.
- While salicylate toxicity can cause respiratory alkalosis, severe confusion and the progression of symptoms suggest a more advanced stage, usually involving a metabolic acidosis component, making a pure, uncompensated respiratory alkalosis less likely.
*pH: 7.31, PaCO2: 31 mmHg, HCO3-: 15 mEq/L*
- This blood gas shows a **low pH**, **low PaCO2**, and **low HCO3-**. This also indicates a **metabolic acidosis** with **respiratory compensation**.
- However, compared to pH 7.30, PaCO2 15 mmHg, and HCO3- 16 mEq/L, this option shows slightly **less severe respiratory compensation** (PaCO2 is higher), which is less typical for the profound respiratory stimulation seen in severe salicylate poisoning. The chosen correct option demonstrates a more characteristic and maximal respiratory compensation for the degree of metabolic acidosis.
Respiratory alkalosis mechanisms and compensation US Medical PG Question 9: A 27-year-old man presents to the emergency department with his family because of abdominal pain, excessive urination, and drowsiness since the day before. He has had type 1 diabetes mellitus for 2 years. He ran out of insulin 2 days ago. The vital signs at admission include: temperature 36.8°C (98.2°F), blood pressure 102/69 mm Hg, and pulse 121/min. On physical examination, he is lethargic and his breathing is rapid and deep. There is a mild generalized abdominal tenderness without rebound tenderness or guarding. His serum glucose is 480 mg/dL. Arterial blood gas of this patient will most likely show which of the following?
- A. ↑ pH, ↑ bicarbonate, and normal pCO2
- B. ↓ pH, ↓ bicarbonate and ↑ anion gap (Correct Answer)
- C. ↑ pH, normal bicarbonate and ↓ pCO2
- D. ↓ pH, ↓ bicarbonate and normal anion gap
- E. ↓ pH, normal bicarbonate and ↑ pCO2
Respiratory alkalosis mechanisms and compensation Explanation: ***↓ pH, ↓ bicarbonate and ↑ anion gap***
- The patient's symptoms (abdominal pain, excessive urination, drowsiness, rapid and deep breathing, hyperglycemia) and history of Type 1 diabetes with missed insulin are highly suggestive of **diabetic ketoacidosis (DKA)**.
- DKA is characterized by **metabolic acidosis** due to the accumulation of ketone bodies, leading to a **decreased pH**, consumption of bicarbonate and thus a **decreased bicarbonate level**, and an **increased anion gap**.
*↑ pH, ↑ bicarbonate, and normal pCO2*
- This pattern suggests a **metabolic alkalosis**, which is inconsistent with the patient's presentation of DKA.
- Metabolic alkalosis is typically seen in conditions like severe vomiting or diuretic use, not uncontrolled diabetes.
*↑ pH, normal bicarbonate and ↓ pCO2*
- This profile describes **respiratory alkalosis**, often caused by primary hyperventilation.
- While the patient has rapid and deep breathing (Kussmaul respiration), this is a compensatory mechanism for metabolic acidosis, not a primary respiratory alkalosis.
*↓ pH, ↓ bicarbonate and normal anion gap*
- This indicates a **normal anion gap metabolic acidosis**, also known as hyperchloremic acidosis.
- This is typically seen in conditions like renal tubular acidosis or severe diarrhea, where bicarbonate is lost or chloride is retained, which is not the case for DKA.
*↓ pH, normal bicarbonate and ↑ pCO2*
- This presentation indicates **respiratory acidosis**, which is caused by hypoventilation and retention of CO2.
- The patient's rapid and deep breathing (Kussmaul breathing) is a compensatory mechanism to blow off CO2 and would decrease pCO2, not increase it.
Respiratory alkalosis mechanisms and compensation US Medical PG Question 10: A 57-year-old woman comes to the emergency department because of dizziness, nausea, and vomiting for 4 days. Her temperature is 37.3°C (99.1°F), pulse is 100/min, respirations are 20/min, and blood pressure is 110/70 mm Hg. Physical examination shows no abnormalities. Arterial blood gas analysis on room air shows:
pH 7.58
PCO2 43 mm Hg
PO2 96 mm Hg
HCO3- 32 mEq/L
The most appropriate next step in diagnosis is measurement of which of the following?
- A. Serum anion gap
- B. Urine albumin to creatinine ratio
- C. Serum osmolal gap
- D. Urine anion gap
- E. Urine chloride (Correct Answer)
Respiratory alkalosis mechanisms and compensation Explanation: ***Urine chloride***
- The patient presents with **metabolic alkalosis** (pH 7.58, HCO3- 32 mEq/L with minimal respiratory compensation).
- **Urine chloride** is the key diagnostic test to differentiate between **saline-responsive** (urine Cl <20 mEq/L) and **saline-unresponsive** (urine Cl >20 mEq/L) metabolic alkalosis.
- Given the patient's **4-day history of vomiting**, this is likely saline-responsive alkalosis from gastric HCl loss, which would be confirmed by low urine chloride and guide appropriate treatment with saline repletion.
*Serum anion gap*
- The **serum anion gap** is primarily used to evaluate causes of **metabolic acidosis** (differentiating high AG from normal AG acidosis).
- It would not provide useful information for determining the etiology of metabolic alkalosis.
*Urine albumin to creatinine ratio*
- The **urine albumin to creatinine ratio** screens for **kidney damage** or **proteinuria**.
- There is no clinical indication (e.g., elevated creatinine, edema, hypertension) to suggest kidney disease as the cause of her acid-base imbalance.
*Serum osmolal gap*
- The **serum osmolal gap** detects **exogenous osmotically active substances** like toxic alcohols (methanol, ethylene glycol) or mannitol.
- These typically cause **high anion gap metabolic acidosis**, not metabolic alkalosis, making this test inappropriate for this patient.
*Urine anion gap*
- The **urine anion gap** differentiates causes of **normal anion gap metabolic acidosis** by assessing urinary ammonium excretion (positive in RTA, negative in GI losses).
- It is not indicated for the evaluation of metabolic alkalosis.
More Respiratory alkalosis mechanisms and compensation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.