Renal bicarbonate handling US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Renal bicarbonate handling. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Renal bicarbonate handling US Medical PG Question 1: An investigator is studying patients with acute decompensated congestive heart failure. He takes measurements of a hormone released from atrial myocytes, as well as serial measurements of left atrial and left ventricular pressures. The investigator observes a positive correlation between left atrial pressures and the serum level of this hormone. Which of the following is most likely the mechanism of action of this hormone?
- A. Increases potassium excretion at the collecting ducts
- B. Constricts afferent renal arteriole
- C. Decreases sodium reabsorption at the collecting tubules (Correct Answer)
- D. Decreases reabsorption of bicarbonate in the proximal convoluted tubules
- E. Increases free water reabsorption from the distal tubules
Renal bicarbonate handling Explanation: ***Decreases sodium reabsorption at the collecting tubules***
- The hormone described, exhibiting a positive correlation with left atrial pressure and released from atrial myocytes, is **Atrial Natriuretic Peptide (ANP)**.
- ANP promotes **natriuresis** (sodium excretion) and **diuresis** by directly inhibiting sodium reabsorption in the collecting tubules, thereby reducing blood volume and cardiac preload.
*Increases potassium excretion at the collecting ducts*
- While ANP does promote fluid and electrolyte excretion, its primary effect is on sodium and water, not a direct increase in **potassium excretion**. **Aldosterone**, not ANP, primarily increases potassium secretion in the collecting ducts.
- This option describes a mechanism more consistent with **mineralocorticoid activity**, which is counteracted by ANP.
*Constricts afferent renal arteriole*
- ANP generally causes **vasodilation** of the afferent arteriole and constriction of the efferent arteriole, increasing glomerular filtration rate (GFR).
- **Angiotensin II** is a primary constrictor of the afferent and efferent renal arterioles, which is the opposite effect of ANP.
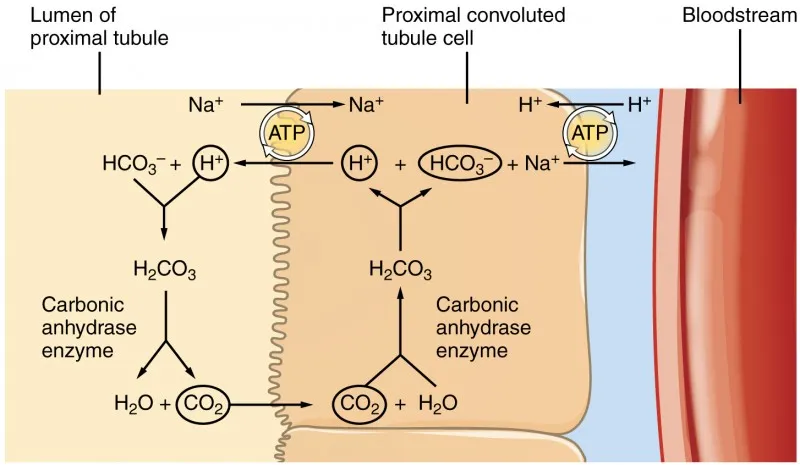
*Decreases reabsorption of bicarbonate in the proximal convoluted tubules*
- This mechanism is primarily involved in **acid-base balance** and is influenced by factors like parathyroid hormone or respiratory/metabolic acidosis/alkalosis.
- ANP's main action is on **sodium and water balance**, not directly on bicarbonate reabsorption.
*Increases free water reabsorption from the distal tubules*
- **Vasopressin (Antidiuretic Hormone, ADH)** is responsible for increasing free water reabsorption in the distal tubules and collecting ducts.
- ANP's action is to *increase* water excretion, working in opposition to ADH to reduce circulating fluid volume.
Renal bicarbonate handling US Medical PG Question 2: A researcher is studying the effects of a new antihypertensive medication on urine osmolality. She first measures urine osmolality in different parts of the nephron of a healthy human control. The findings are shown below:
Portion of nephron Urine osmolality (mOsmol/kg)
Proximal convoluted tubule 300
Loop of Henle, descending limb 1200
Loop of Henle, ascending limb 200
Distal convoluted tubule 100
Collecting duct 600
Which of the following is the most likely explanation for the urine osmolality in the ascending limb of the loop of Henle?
- A. Increased urea excretion
- B. Increased transcription of water channels
- C. Impermeability to water (Correct Answer)
- D. Increased bicarbonate reabsorption
- E. Impermeability to sodium
Renal bicarbonate handling Explanation: ***Impermeability to water***
- The **ascending limb of the loop of Henle** is notable for its **water impermeability** due to the absence of aquaporins.
- This impermeability, coupled with active reabsorption of solutes, leads to the production of **hypoosmotic fluid** (200 mOsmol/kg) in this segment.
*Increased urea excretion*
- While urea is a major contributor to medullary osmolality and is excreted, it is primarily reabsorbed in the **collecting duct** and secreted into the loop of Henle, not directly explaining the low osmolality in the ascending limb.
- Increased urea excretion on its own would likely lead to a higher, not lower, osmolality of the urine exiting the kidney.
*Increased transcription of water channels*
- Increased transcription of water channels (**aquaporins**) would make the tubule more permeable to water, leading to water reabsorption and an **increase in osmolality**, which contradicts the observed hypoosmotic fluid.
- The ascending limb is primarily involved in **solute reabsorption** without water, making it dilute.
*Increased bicarbonate reabsorption*
- **Bicarbonate reabsorption** primarily occurs in the **proximal tubule** and is crucial for acid-base balance, not directly impacting the dramatic osmolality changes in the ascending limb.
- While some bicarbonate is reabsorbed in the ascending limb, it does not explain the significant decrease in fluid osmolality.
*Impermeability to sodium*
- The ascending limb is **highly permeable to sodium** and actively reabsorbs it via the **Na-K-2Cl cotransporter**, which is crucial for diluting the tubular fluid.
- If it were impermeable to sodium, the reabsorption of solutes would cease, and the osmolality would not decrease as observed.
Renal bicarbonate handling US Medical PG Question 3: What is the primary mechanism for maintaining acid-base balance during prolonged vomiting?
- A. Increased chloride reabsorption
- B. Increased potassium excretion
- C. Increased bicarbonate excretion (Correct Answer)
- D. Decreased hydrogen secretion
Renal bicarbonate handling Explanation: ***Increased bicarbonate excretion***
- Prolonged vomiting leads to the loss of **gastric acid (HCl)**, causing **metabolic alkalosis**. The kidneys compensate by increasing the excretion of **bicarbonate (HCO3-)** to restore acid-base balance.
- This renal compensation is the primary mechanism to eliminate the excess alkali from the body.
*Increased chloride reabsorption*
- In **metabolic alkalosis** due to vomiting, the body tends to reabsorb less chloride, not more, in an attempt to excrete bicarbonate.
- **Chloride depletion** can actually hinder bicarbonate excretion by promoting sodium reabsorption with bicarbonate.
*Increased potassium excretion*
- **Hypokalemia** can occur with prolonged vomiting due to increased aldosterone activity and direct renal loss associated with metabolic alkalosis.
- However, increased potassium excretion itself is not the primary mechanism for correcting the acid-base disorder; rather, it is a consequence or a contributing factor to the imbalance.
*Decreased hydrogen secretion*
- In response to alkalosis, the kidneys would typically decrease, not increase, **hydrogen ion (H+) secretion** in an effort to retain H+ and normalize pH.
- Decreased H+ secretion is a compensatory mechanism, but the direct excretion of bicarbonate is more crucial for correcting the metabolic alkalosis.
Renal bicarbonate handling US Medical PG Question 4: Which mechanism primarily regulates sodium reabsorption in the collecting duct?
- A. Glomerulotubular balance
- B. Atrial natriuretic peptide
- C. Antidiuretic hormone
- D. Aldosterone (Correct Answer)
Renal bicarbonate handling Explanation: ***Aldosterone***
- **Aldosterone** is the primary hormone that stimulates **sodium reabsorption** and **potassium secretion** in the principal cells of the collecting duct.
- It acts by increasing the synthesis and activity of **ENaC channels** on the apical membrane and **Na+/K+-ATPase pumps** on the basolateral membrane.
*Glomerulotubular balance*
- **Glomerulotubular balance** refers to the mechanism by which the **proximal tubule** reabsorbs a constant fraction of the filtered load, regardless of changes in glomerular filtration rate (GFR).
- This mechanism maintains a relatively constant delivery of fluid and solutes to downstream segments but does not primarily regulate sodium in the collecting duct.
*Atrial natriuretic peptide*
- **Atrial natriuretic peptide (ANP)** primarily **inhibits sodium reabsorption** in the collecting duct, leading to **natriuresis** and **diuresis**, which is the opposite of sodium reabsorption.
- ANP is released in response to atrial stretch, indicating increased blood volume.
*Antidiuretic hormone*
- **Antidiuretic hormone (ADH)** primarily regulates **water reabsorption** in the collecting duct by increasing the insertion of **aquaporin-2 channels** into the apical membrane, making the collecting duct permeable to water.
- While ADH can indirectly affect sodium concentration by influencing water movement, it does not directly regulate sodium transport to the same extent as aldosterone.
Renal bicarbonate handling US Medical PG Question 5: A 17-year-old boy is brought to the physician by his father because of a 7-month history of fatigue, recurrent leg cramps, and increased urinary frequency. His pulse is 94/min and blood pressure is 118/85 mm Hg. Physical examination shows dry mucous membranes. Laboratory studies show:
Serum
Na+ 130 mEq/L
K+ 2.8 mEq/L
Cl- 92 mEq/L
Mg2+ 1.1 mEq/L
Ca2+ 10.6 mg/dL
Albumin 5.2 g/dL
Urine
Ca2+ 70 mg/24 h
Cl- 375 mEq/24h (N = 110–250)
Arterial blood gas analysis on room air shows a pH of 7.55 and an HCO3- concentration of 45 mEq/L. Impaired function of which of the following structures is the most likely cause of this patient's condition?
- A. Ascending loop of Henle
- B. Collecting duct
- C. Distal convoluted tubule (Correct Answer)
- D. Descending loop of Henle
- E. Proximal convoluted tubule
Renal bicarbonate handling Explanation: ***Distal convoluted tubule***
- The patient presents with **hypokalemia**, **metabolic alkalosis**, **hypomagnesemia**, and **hypocalciuria** (24-hour urine Ca2+ 70 mg, normal up to 250 mg), which are characteristic findings of **Gitelman syndrome**.
- **Gitelman syndrome** is caused by a loss-of-function mutation in the **thiazide-sensitive Na-Cl cotransporter (NCC)**, located in the **distal convoluted tubule**, leading to impaired reabsorption of Na+ and Cl- at this segment.
*Ascending loop of Henle*
- Impaired function of the **Na-K-2Cl cotransporter (NKCC2)** in the **thick ascending limb of the loop of Henle** causes **Bartter syndrome**.
- Bartter syndrome typically presents with **hypercalciuria**, in contrast to the hypocalciuria seen in this patient.
*Collecting duct*
- Dysfunction of the **collecting duct** can lead to various conditions, such as **renal tubular acidosis** or **diabetes insipidus**, depending on which channels or receptors are affected.
- However, the specific combination of **hypokalemia**, **metabolic alkalosis**, **hypomagnesemia**, and **hypocalciuria** points away from primary collecting duct dysfunction.
*Descending loop of Henle*
- The **descending loop of Henle** is primarily permeable to **water** and has a limited role in electrolyte reabsorption.
- Impairment here would primarily affect **urine concentration** and dilution but would not account for the specific electrolyte imbalances observed.
*Proximal convoluted tubule*
- The **proximal convoluted tubule** is responsible for reabsorbing a large fraction of filtered electrolytes, glucose, and amino acids.
- Dysfunction here (e.g., **Fanconi syndrome**) would typically present with **generalized aminoaciduria**, **glycosuria**, **phosphaturia**, and **proximal renal tubular acidosis**, which are not seen in this patient.
Renal bicarbonate handling US Medical PG Question 6: Two hours after undergoing laparoscopic roux-en-Y gastric bypass surgery, a 44-year-old man complains of pain in the site of surgery and nausea. He has vomited twice in the past hour. He has hypertension, type 2 diabetes mellitus, and hypercholesterolemia. Current medications include insulin, atorvastatin, hydrochlorothiazide, acetaminophen, and prophylactic subcutaneous heparin. He drinks two to three beers daily and occasionally more on weekends. He is 177 cm (5 ft 10 in) tall and weighs 130 kg (286 lb); BMI is 41.5 kg/m2. His temperature is 37.3°C (99.1°F), pulse is 103/min, and blood pressure is 122/82 mm Hg. Examination shows five laparoscopic incisions with no erythema or discharge. The abdomen is soft and non-distended. There is slight diffuse tenderness to palpation. Bowel sounds are reduced. Laboratory studies show:
Hematocrit 45%
Serum
Na+ 136 mEq/L
K+ 3.5 mEq/L
Cl- 98 mEq/L
Urea nitrogen 31 mg/dL
Glucose 88 mg/dL
Creatinine 1.1 mg/dL
Arterial blood gas analysis on room air shows:
pH 7.28
pCO2 32 mm Hg
pO2 74 mm Hg
HCO3- 14.4 mEq/L
Which of the following is the most likely cause for the acid-base status of this patient?
- A. Hypoxia (Correct Answer)
- B. Uremia
- C. Late dumping syndrome
- D. Vomiting
- E. Early dumping syndrome
Renal bicarbonate handling Explanation: ***Hypoxia***
- The patient exhibits **metabolic acidosis** (pH 7.28, HCO3- 14.4 mEq/L) with **appropriate respiratory compensation** (pCO2 32 mm Hg using Winter's formula: expected pCO2 = 1.5 × 14.4 + 8 ± 2 = 29.6 ± 2).
- The **pO2 of 74 mm Hg is significantly low** (normal range on room air: 80-100 mm Hg), indicating **hypoxemia** that leads to **tissue hypoxia** and **anaerobic metabolism**.
- In the setting of **obesity (BMI 41.5)** and **immediate post-operative status** after laparoscopic surgery, multiple factors contribute to hypoxemia including **atelectasis, reduced functional residual capacity, pain limiting deep breathing, residual anesthetic effects, and pneumoperitoneum effects**.
- Tissue hypoxia results in **lactic acidosis** (a high anion gap metabolic acidosis), which explains the acid-base disturbance. The **elevated BUN (31 mg/dL) with relatively normal creatinine** suggests prerenal azotemia from hypoperfusion, further supporting inadequate tissue oxygenation.
- The **tachycardia (103/min)** represents a compensatory response to improve oxygen delivery to hypoxic tissues.
*Vomiting*
- Vomiting causes loss of **gastric HCl**, resulting in **hypochloremic metabolic ALKALOSIS** (elevated pH and HCO3-), not acidosis.
- While this patient is vomiting, the acid-base status shows **acidosis**, which is the opposite of what vomiting typically causes.
- The low **Cl- (98 mEq/L)** is consistent with some gastric acid loss, but the dominant acid-base disorder is metabolic acidosis from another cause.
*Uremia*
- **Uremia** causes high anion gap metabolic acidosis due to retention of organic acids and phosphates in renal failure.
- While the **BUN is elevated (31 mg/dL)**, the **creatinine (1.1 mg/dL) is essentially normal**, especially for a patient with high muscle mass (130 kg).
- The BUN elevation is more consistent with **prerenal azotemia** (dehydration/hypoperfusion) rather than intrinsic renal failure causing uremic acidosis.
*Late dumping syndrome*
- **Late dumping syndrome** occurs **1-3 hours after eating** and results from rapid carbohydrate absorption causing hyperinsulinemia and subsequent **reactive hypoglycemia**.
- This patient's **glucose is normal (88 mg/dL)**, and symptoms began only **2 hours post-surgery** in the fasting state, not after a meal.
- Late dumping does not cause metabolic acidosis.
*Early dumping syndrome*
- **Early dumping syndrome** occurs **10-30 minutes after eating** due to rapid gastric emptying of hyperosmolar contents into the small intestine, causing fluid shifts.
- Symptoms include **cramping, diarrhea, vasomotor symptoms (flushing, palpitations, dizziness)**, not metabolic acidosis.
- This patient has not yet eaten post-operatively, making dumping syndrome impossible.
Renal bicarbonate handling US Medical PG Question 7: A 57-year-old woman comes to the emergency department because of dizziness, nausea, and vomiting for 4 days. Her temperature is 37.3°C (99.1°F), pulse is 100/min, respirations are 20/min, and blood pressure is 110/70 mm Hg. Physical examination shows no abnormalities. Arterial blood gas analysis on room air shows:
pH 7.58
PCO2 43 mm Hg
PO2 96 mm Hg
HCO3- 32 mEq/L
The most appropriate next step in diagnosis is measurement of which of the following?
- A. Serum anion gap
- B. Urine albumin to creatinine ratio
- C. Serum osmolal gap
- D. Urine anion gap
- E. Urine chloride (Correct Answer)
Renal bicarbonate handling Explanation: ***Urine chloride***
- The patient presents with **metabolic alkalosis** (pH 7.58, HCO3- 32 mEq/L with minimal respiratory compensation).
- **Urine chloride** is the key diagnostic test to differentiate between **saline-responsive** (urine Cl <20 mEq/L) and **saline-unresponsive** (urine Cl >20 mEq/L) metabolic alkalosis.
- Given the patient's **4-day history of vomiting**, this is likely saline-responsive alkalosis from gastric HCl loss, which would be confirmed by low urine chloride and guide appropriate treatment with saline repletion.
*Serum anion gap*
- The **serum anion gap** is primarily used to evaluate causes of **metabolic acidosis** (differentiating high AG from normal AG acidosis).
- It would not provide useful information for determining the etiology of metabolic alkalosis.
*Urine albumin to creatinine ratio*
- The **urine albumin to creatinine ratio** screens for **kidney damage** or **proteinuria**.
- There is no clinical indication (e.g., elevated creatinine, edema, hypertension) to suggest kidney disease as the cause of her acid-base imbalance.
*Serum osmolal gap*
- The **serum osmolal gap** detects **exogenous osmotically active substances** like toxic alcohols (methanol, ethylene glycol) or mannitol.
- These typically cause **high anion gap metabolic acidosis**, not metabolic alkalosis, making this test inappropriate for this patient.
*Urine anion gap*
- The **urine anion gap** differentiates causes of **normal anion gap metabolic acidosis** by assessing urinary ammonium excretion (positive in RTA, negative in GI losses).
- It is not indicated for the evaluation of metabolic alkalosis.
Renal bicarbonate handling US Medical PG Question 8: A 3-month-old girl is brought to the physician because of poor feeding, irritability and vomiting for 2 weeks. She was born at 36 weeks' gestation and pregnancy was uncomplicated. She is at 5th percentile for length and at 3rd percentile for weight. Her temperature is 36.8°C (98.2°F), pulse is 112/min and respirations are 49/min. Physical and neurologic examinations show no other abnormalities. Laboratory studies show:
Serum
Na+ 138 mEq/L
K+ 3.1 mEq/L
Cl- 115 mEq/L
Ammonia 23 μmol/L (N <50 μmol/L)
Urine
pH 6.9
Blood negative
Glucose negative
Protein negative
Arterial blood gas analysis on room air shows:
pH 7.28
pO2 96 mm Hg
HCO3- 12 mEq/L
Which of the following is the most likely cause of these findings?
- A. Deficiency of ornithine transcarbamylase
- B. Impaired metabolism of branched-chain amino acids
- C. Inability of the distal tubule to secrete H+ (Correct Answer)
- D. Impaired CFTR gene function
- E. Deficiency of 21-hydroxylase
Renal bicarbonate handling Explanation: ***Inability of the distal tubule to secrete H+***
- The patient presents with **non-anion gap metabolic acidosis** (pH 7.28, HCO3- 12 mEq/L, anion gap = 138 - (115 + 12) = 11), **hypokalemia** (K+ 3.1 mEq/L), and **inappropriately alkaline urine** (pH 6.9). These findings are classic for **distal (Type 1) renal tubular acidosis (RTA)**, where the distal tubules cannot excrete H+ adequately, leading to systemic acidosis.
- The symptoms of **poor feeding, irritability, vomiting**, and **poor growth** are common manifestations of chronic acidosis in infants.
*Deficiency of ornithine transcarbamylase*
- This urea cycle disorder would lead to **hyperammonemia** (ammonia >50 μmol/L), which is not present here (ammonia 23 μmol/L).
- While it can cause metabolic acidosis due to accumulation of organic acids in severe cases, the primary biochemical derangement is hyperammonemia, and the findings of an alkaline urine pH with metabolic acidosis are not typical.
*Impaired metabolism of branched-chain amino acids*
- This condition, known as **Maple Syrup Urine Disease**, primarily presents with a characteristic sweet odor to the urine and neurological deterioration due to the accumulation of branched-chain amino acids and their ketoacids.
- It would typically cause a significant **anion gap metabolic acidosis** and not an alkaline urine pH.
*Impaired CFTR gene function*
- This describes **Cystic Fibrosis**, which primarily affects exocrine glands, leading to symptoms like **malabsorption**, recurrent pulmonary infections, and meconium ileus in neonates.
- It does not typically cause the specific electrolyte and acid-base disturbances seen here (non-anion gap metabolic acidosis with hypokalemia and alkaline urine).
*Deficiency of 21-hydroxylase*
- This enzyme deficiency causes **Congenital Adrenal Hyperplasia (CAH)**. The most common form leads to **salt-wasting crises** with hyponatremia and hyperkalemia.
- It would not typically present with hypokalemia and non-anion gap metabolic acidosis with alkaline urine pH.
Renal bicarbonate handling US Medical PG Question 9: A 75-year-old woman is brought to a physician’s office by her son with complaints of diarrhea and vomiting for 1 day. Her stool is loose, watery, and yellow-colored, while her vomitus contains partially digested food particles. She denies having blood or mucus in her stools and vomitus. Since the onset of her symptoms, she has not had anything to eat and her son adds that she is unable to tolerate fluids. The past medical history is unremarkable and she does not take any medications regularly. The pulse is 115/min, the respiratory rate is 16/min, the blood pressure is 100/60 mm Hg, and the temperature is 37.0°C (98.6°F). The physical examination shows dry mucous membranes and slightly sunken eyes. The abdomen is soft and non-tender. Which of the following physiologic changes in glomerular filtration rate (GFR), renal plasma flow (RPF), and filtration fraction (FF) are expected?
- A. Decreased GFR, decreased RPF, decreased FF
- B. Decreased GFR, decreased RPF, no change in FF
- C. Increased GFR, increased RPF, increased FF
- D. Increased GFR, decreased RPF, increased FF
- E. Decreased GFR, decreased RPF, increased FF (Correct Answer)
Renal bicarbonate handling Explanation: ***Decreased GFR, decreased RPF, increased FF***
- Due to **dehydration** from diarrhea and vomiting, there is a decrease in blood volume leading to decreased renal blood flow and **renal plasma flow (RPF)**.
- The body responds to hypovolemia by activating the renin-angiotensin-aldosterone system (RAAS) and sympathetic nervous system, which cause **preferential efferent arteriolar constriction** (more than afferent constriction). This helps maintain glomerular hydrostatic pressure despite reduced renal perfusion.
- As a result, **GFR decreases** but proportionally **less than RPF decreases**, causing the **filtration fraction (FF = GFR/RPF) to increase**.
- In this patient with significant dehydration (tachycardia, hypotension, dry mucous membranes), both GFR and RPF are reduced, but FF is elevated due to compensatory mechanisms.
*Decreased GFR, decreased RPF, decreased FF*
- While GFR and RPF will decrease due to dehydration, the **filtration fraction is expected to increase**, not decrease.
- A decreased FF would imply GFR fell proportionally more than RPF, which contradicts the physiologic response where efferent arteriolar constriction helps preserve GFR relative to RPF.
*Decreased GFR, decreased RPF, no change in FF*
- With significant fluid loss and compensatory mechanisms (efferent arteriolar constriction via angiotensin II), a change in **filtration fraction** is expected.
- The body actively alters arteriolar tone to prioritize GFR maintenance, which directly increases FF.
*Increased GFR, increased RPF, increased FF*
- This pattern suggests **hypervolemia** or increased renal perfusion, which directly contradicts the patient's severe dehydration.
- Both GFR and RPF are expected to decrease in volume depletion, not increase.
*Increased GFR, decreased RPF, increased FF*
- An increase in GFR is physiologically impossible given the patient's severe volume depletion and reduced renal perfusion.
- While FF does increase in dehydration, this occurs in the context of **both GFR and RPF being decreased**, not with an increased GFR.
Renal bicarbonate handling US Medical PG Question 10: A 39-year-old woman presents to the clinic with complaints of constipation for the past 2 weeks. She reports that it has been getting increasingly difficult to pass stool to the point that she would go for 2-3 days without going to the bathroom. Prior to this, she passed stool every day without difficulty. She denies weight changes, headaches, chest pain, or abdominal pain but endorses fatigue. Her past medical history is significant for 2 episodes of kidney stones within the past 3 months. A physical examination is unremarkable. Laboratory studies are done and the results are shown below:
Serum:
Na+: 138 mEq/L
Cl-: 97 mEq/L
K+: 3.9 mEq/L
HCO3-: 24 mEq/L
BUN: 10 mg/dL
Glucose: 103 mg/dL
Creatinine: 1.1 mg/dL
Thyroid-stimulating hormone: 3.1 uU/mL
Ca2+: 12.1 mg/dL
Phosphate: 1.2 mg/dL (Normal: 2.5-4.5 mg/dL)
What is the most likely explanation for this patient’s low phosphate levels?
- A. Defective G-coupled calcium-sensing receptors in multiple tissues
- B. Increased calcium reabsorption at the distal convoluted tubule due to enhanced TRPV5 channel activity
- C. Hereditary malfunction of phosphate absorption at the small brush border
- D. Chronic renal disease caused by recurrent renal stones
- E. Inhibition of sodium-phosphate cotransporter at the proximal convoluted tubule (PCT) (Correct Answer)
Renal bicarbonate handling Explanation: ***Inhibition of sodium-phosphate cotransporter at the proximal convoluted tubule (PCT)***
- The patient presents with **hypercalcemia (Ca2+ 12.1 mg/dL)** and **hypophosphatemia (Phosphate 1.2 mg/dL)**, along with a history of recurrent kidney stones and constipation, which are classic signs of **primary hyperparathyroidism**.
- In primary hyperparathyroidism, elevated **parathyroid hormone (PTH)** directly inhibits the **sodium-phosphate cotransporter** in the PCT, leading to decreased phosphate reabsorption and increased renal phosphate excretion.
*Defective G-coupled calcium-sensing receptors in multiple tissues*
- This describes **familial hypocalciuric hypercalcemia (FHH)**, where defective **calcium-sensing receptors (CaSRs)** in the parathyroid glands and kidneys cause a higher set point for calcium, leading to hypercalcemia.
- However, FHH typically presents with **normal to slightly elevated PTH levels** and **hypocalciuria**, whereas this patient's presentation with hypophosphatemia and recurrent kidney stones is more consistent with elevated PTH from primary hyperparathyroidism.
*Increased calcium reabsorption at the distal convoluted tubule due to enhanced TRPV5 channel activity*
- While **PTH** does increase calcium reabsorption, this occurs primarily in the **distal convoluted tubule (DCT)** via activation of **TRPV5 channels**.
- This mechanism explains the **hypercalcemia** but does not directly account for the observed **hypophosphatemia**, which is primarily due to PTH's action on phosphate excretion in the PCT.
*Hereditary malfunction of phosphate absorption at the small brush border*
- This describes conditions like **hereditary hypophosphatemic rickets**, which are characterized by isolated renal phosphate wasting and usually present earlier in life.
- This patient's acute onset of symptoms, hypercalcemia, and history of kidney stones point away from a primary hereditary defect in intestinal phosphate absorption.
*Chronic renal disease caused by recurrent renal stones*
- While recurrent kidney stones can lead to chronic kidney disease (CKD), CKD typically causes **hyperphosphatemia** due to reduced glomerular filtration of phosphate, especially in later stages.
- The patient's creatinine and BUN are within normal limits, indicating no significant chronic kidney disease that would explain the hypophosphatemia.
More Renal bicarbonate handling US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.