Metabolic acidosis mechanisms and compensation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Metabolic acidosis mechanisms and compensation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Metabolic acidosis mechanisms and compensation US Medical PG Question 1: A 65-year-old man is brought to the emergency department from his home. He is unresponsive. His son requested a wellness check because he had not heard from his father in 2 weeks. He reports that his father was sounding depressed during a telephone call. The paramedics found a suicide note and a half-empty bottle of antifreeze near the patient. The medical history includes hypertension and hyperlipidemia. The vital signs include: blood pressure 120/80 mm Hg, respiratory rate 25/min, heart rate 95/min, and temperature 37.0°C (98.5°F). He is admitted to the hospital. What do you expect the blood gas analysis to show?
- A. Non-anion gap metabolic acidosis
- B. Metabolic alkalosis
- C. Respiratory acidosis
- D. Anion gap metabolic acidosis (Correct Answer)
- E. Mixed acid-base disorder
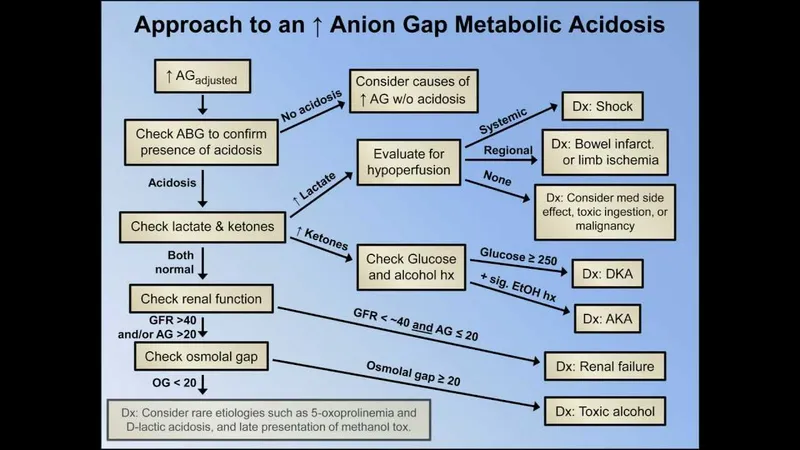
Metabolic acidosis mechanisms and compensation Explanation: ***Anion gap metabolic acidosis***
- The patient's history of **antifreeze ingestion** indicates likely exposure to **ethylene glycol**, which is metabolized into toxic acids (glycolic and oxalic acid).
- These accumulating acids lead to an **increased anion gap metabolic acidosis**.
*Non-anion gap metabolic acidosis*
- This type of acidosis typically results from **bicarbonate loss** (e.g., severe diarrhea) or **excessive chloride intake**, which is not indicated by the antifreeze ingestion.
- It involves a normal anion gap because other unmeasured anions do not accumulate.
*Metabolic alkalosis*
- This imbalance is characterized by an **increase in bicarbonate** or a significant loss of acid, often due to vomiting or diuretic use.
- Antifreeze poisoning directly leads to acid accumulation, precisely the opposite of metabolic alkalosis.
*Respiratory acidosis*
- This occurs due to **hypoventilation** and subsequent buildup of CO2, leading to increased carbonic acid.
- While respiratory rate is elevated, the primary problem here is metabolic due to toxin ingestion, not respiratory CO2 retention.
*Mixed acid-base disorder*
- While a mixed disorder is possible in complex cases, the presentation with antifreeze poisoning is classically dominated by a **severe anion gap metabolic acidosis**.
- There is no clear indication of a separate primary respiratory or alkalotic disorder at onset to warrant a "mixed" label as the primary anticipated finding.
Metabolic acidosis mechanisms and compensation US Medical PG Question 2: A 72-year-old female is brought to the emergency department after being found unresponsive in her garage with an open bottle of unmarked fluid. She is confused and is unable to answer questions on arrival. Her medical history is significant for Alzheimer disease, but her family says she has no medical comorbidities. Serum analysis of this patient's blood shows a pH of 7.28 with a high anion gap. The electrolyte that is most likely significantly decreased in this patient follows which of the following concentration curves across the proximal tubule of the kidney?
- A. Curve C
- B. Curve E
- C. Curve B
- D. Curve A
- E. Curve D (Correct Answer)
Metabolic acidosis mechanisms and compensation Explanation: ***Curve D***
- The patient presents with **high anion gap metabolic acidosis**, which, in the context of an unknown fluid ingestion, is highly suggestive of **methanol** or **ethylene glycol poisoning**. These toxins are metabolized into toxic acids (**formic acid** from methanol; **glycolic acid, oxalic acid** from ethylene glycol).
- These toxic acid anions displace **bicarbonate** (HCO3-) in the blood to maintain electroneutrality, leading to a **decreased bicarbonate level**. Curve D represents bicarbonate, which is largely reabsorbed in the proximal tubule but significantly reduced in this scenario.
*Curve C*
- This curve likely represents a substance like **phosphate** or **urea**, which is partially reabsorbed and partially excreted.
- While phosphate levels can be affected in various metabolic derangements, it's not the primary electrolyte significantly decreased in **high anion gap metabolic acidosis** from toxic alcohol ingestion.
*Curve E*
- This curve typically represents a substance that is **filtered and then minimally reabsorbed** or even secreted, such as **creatinine** or **potassium** when excess is being excreted.
- **Potassium** levels can be variable in acidosis but are not typically the most significantly decreased electrolyte in this poisoning scenario.
*Curve B*
- This curve would normally represent an electrolyte that is **highly reabsorbed** in the proximal tubule, with very little remaining.
- This might represent substances like **glucose** (under normal conditions) or **amino acids**, which are not the primary electrolyte affected in this case.
*Curve A*
- This curve represents a substance that is **freely filtered** and then **neither reabsorbed nor secreted** significantly in the proximal tubule, such as **inulin**.
- This pattern does not correspond to an electrolyte whose level would be significantly decreased due to high anion gap metabolic acidosis.
Metabolic acidosis mechanisms and compensation US Medical PG Question 3: A 37-year-old G1P0 woman presents to her primary care physician for a routine checkup. She has a history of diabetes and hypertension but has otherwise been healthy with no change in her health status since the last visit. She is expecting her first child 8 weeks from now. She also enrolled in a study about pregnancy where serial metabolic panels and arterial blood gases are obtained. Partial results from these studies are shown below:
Serum:
Na+: 141 mEq/L
Cl-: 108 mEq/L
pH: 7.47
pCO2: 30 mmHg
HCO3-: 21 mEq/L
Which of the following disease processes would most likely present with a similar panel of metabolic results?
- A. Diarrheal disease
- B. Loop diuretic abuse
- C. Living at high altitude (Correct Answer)
- D. Ingestion of metformin
- E. Anxiety attack
Metabolic acidosis mechanisms and compensation Explanation: ***Living at high altitude***
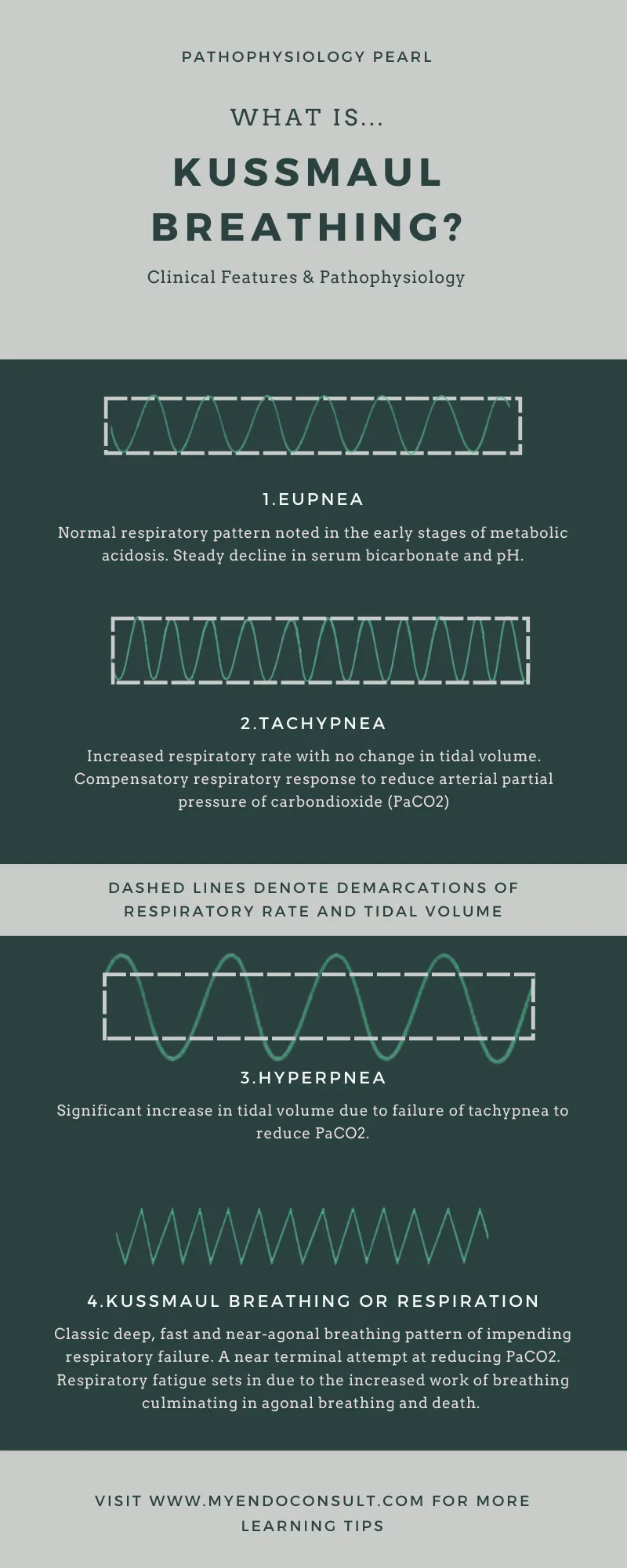
- Chronic exposure to **high altitude** leads to sustained **hypoxia**, which stimulates **hyperventilation** as a compensatory mechanism.
- This persistent hyperventilation causes a **respiratory alkalosis** (high pH, low pCO2) and a compensatory **metabolic acidosis** (low HCO3-) to normalize pH, mimicking the presented metabolic panel.
*Diarrheal disease*
- Severe **diarrhea** leads to the loss of bicarbonate from the gastrointestinal tract, causing a **non-anion gap metabolic acidosis**.
- This would present with a **low pH**, **low HCO3-**, and a **compensatory drop in pCO2**, not a respiratory alkalosis with a high pH.
*Loop diuretic abuse*
- Chronic abuse of **loop diuretics** can cause **metabolic alkalosis** due to increased renal excretion of hydrogen ions and potassium, leading to volume contraction.
- This would typically present with a **high pH**, high HCO3-, and a compensatory rise in pCO2, which is different from the given values.
*Ingestion of metformin*
- **Metformin** can cause **lactic acidosis** (a type of high anion gap metabolic acidosis), especially in patients with renal impairment.
- This would manifest as a **low pH**, **low HCO3-**, and a **compensatory decrease in pCO2**, along with an elevated anion gap, not the respiratory alkalosis seen here.
*Anxiety attack*
- An **anxiety attack** causes acute **hyperventilation**, leading to **acute respiratory alkalosis** (high pH, low pCO2).
- However, in an acute setting, there is insufficient time for significant renal compensation, so the HCO3- would remain near normal, unlike the compensated state shown in the panel.
Metabolic acidosis mechanisms and compensation US Medical PG Question 4: A 72-year-old man being treated for benign prostatic hyperplasia (BPH) is admitted to the emergency department for 1 week of dysuria, nocturia, urge incontinence, and difficulty initiating micturition. His medical history is relevant for hypertension, active tobacco use, chronic obstructive pulmonary disease, and BPH with multiple urinary tract infections. Upon admission, he is found with a heart rate of 130/min, respiratory rate of 19/min, body temperature of 39.0°C (102.2°F), and blood pressure of 80/50 mm Hg. Additional findings during the physical examination include decreased breath sounds, wheezes, crackles at the lung bases, and intense right flank pain. A complete blood count shows leukocytosis and neutrophilia with a left shift. A sample for arterial blood gas analysis (ABG) was taken, which is shown below.
Laboratory test
Serum Na+ 140 mEq/L
Serum Cl- 102 mEq/L
Serum K+ 4.8 mEq/L
Serum creatinine (SCr) 2.3 mg/dL
Arterial blood gas
pH 7.12
Po2 82 mm Hg
Pco2 60 mm Hg
SO2% 92%
HCO3- 12.0 mEq/L
Which of the following best explains the patient’s condition?
- A. Metabolic acidosis complicated by respiratory alkalosis
- B. Non-anion gap metabolic acidosis
- C. Respiratory alkalosis complicated by metabolic acidosis
- D. Respiratory acidosis complicated by metabolic alkalosis
- E. Metabolic acidosis complicated by respiratory acidosis (Correct Answer)
Metabolic acidosis mechanisms and compensation Explanation: ***Metabolic acidosis complicated by respiratory acidosis***
- The patient's pH is significantly low (7.12), indicating **acidemia**. The **HCO3- is markedly low (12 mEq/L)**, and PCO2 is elevated (60 mm Hg), suggesting both a metabolic and a respiratory component to the acidosis.
- The severe infection (fever, elevated heart rate, hypotension, flank pain, leukocytosis, elevated creatinine) and the signs of hypoperfusion contribute to **lactic acidosis (metabolic acidosis)**, while his history of COPD and lung findings (decreased breath sounds, wheezes, crackles) explain the impaired ventilation leading to **respiratory acidosis**.
*Metabolic acidosis complicated by respiratory alkalosis*
- While a **metabolic acidosis** is clearly present due to the low pH and HCO3-, the PCO2 is elevated, indicating **respiratory acidosis**, not alkalosis.
- Respiratory alkalosis would be characterized by a **low PCO2** due to hyperventilation.
*Non-anion gap metabolic acidosis*
- To determine the anion gap, we use the formula: **Na+ - (Cl- + HCO3-)**. In this case, 140 - (102 + 12) = 140 - 114 = **26 mEq/L**.
- An anion gap of 26 mEq/L, which is significantly elevated (normal range is typically 8-12 mEq/L), indicates an **anion gap metabolic acidosis**, not a non-anion gap one.
*Respiratory alkalosis complicated by metabolic acidosis*
- The low pH and HCO3- confirm **metabolic acidosis**, but the elevated PCO2 (60 mm Hg) indicates **respiratory acidosis**, not alkalosis, as the respiratory component is also acidotic.
- Respiratory alkalosis would result from **hyperventilation and a low PCO2**.
*Respiratory acidosis complicated by metabolic alkalosis*
- While the elevated PCO2 indicates **respiratory acidosis**, the HCO3- is significantly low (12 mEq/L), which points to a **metabolic acidosis**, not metabolic alkalosis.
- **Metabolic alkalosis** would be characterized by an **elevated HCO3-**.
Metabolic acidosis mechanisms and compensation US Medical PG Question 5: A 14-year-old male presents to the emergency department with altered mental status. His friends who accompanied him said that he complained of abdominal pain while camping. They denied his consumption of anything unusual from the wilderness, or any vomiting or diarrhea. His temperature is 100.5°F (38.1°C), blood pressure is 95/55 mmHg, pulse is 130/min, and respirations are 30/min. His pupils are equal and reactive to light bilaterally. The remainder of the physical exam is unremarkable. His basic metabolic panel is displayed below:
Serum:
Na+: 116 mEq/L
Cl-: 70 mEq/L
K+: 4.0 mEq/L
HCO3-: 2 mEq/L
BUN: 50 mg/dL
Glucose: 1010 mg/dL
Creatinine: 1.2 mg/dL
While the remainder of his labs are pending, the patient becomes bradypneic and is intubated. His ventilator is adjusted to volume control assist-control with a respiratory rate (RR) of 14/min, tidal volume (Vt) of 350 mL, positive end-expiratory pressure (PEEP) of 5 cm H2O, and fractional inspired oxygen (FiO2) of 40%. His height is 5 feet 5 inches. Intravenous fluids and additional medical therapy are administered. An arterial blood gas obtained after 30 minutes on these settings shows the following:
pH: 7.05
pCO2 :40 mmHg
pO2: 150 mmHg
SaO2: 98%
What is the best next step in management?
- A. Increase respiratory rate
- B. Increase respiratory rate and tidal volume (Correct Answer)
- C. Increase tidal volume
- D. Increase tidal volume and positive end-expiratory pressure
- E. Increase positive end-expiratory pressure
Metabolic acidosis mechanisms and compensation Explanation: ***Increase respiratory rate and tidal volume***
- The patient presents with **severe metabolic acidosis** (pH 7.05, HCO3- 2 mEq/L) due to likely **diabetic ketoacidosis** given the hyperglycemia and altered mental status.
- To compensate for metabolic acidosis, the body attempts to lower pCO2 through **hyperventilation**; therefore, increasing both the **respiratory rate** and **tidal volume** will increase minute ventilation and help "blow off" CO2, thus improving the pH.
*Increase respiratory rate*
- While increasing the respiratory rate will help decrease pCO2 and improve pH, it may not be sufficient on its own to correct the severe acidosis.
- **Tidal volume** also plays a crucial role in minute ventilation and CO2 elimination; addressing both components is more effective.
*Increase tidal volume*
- Increasing tidal volume alone will also increase minute ventilation and help reduce pCO2.
- However, combining it with an increased respiratory rate is more effective for severe acidosis, as both parameters contribute to **CO2 clearance**.
*Increase tidal volume and positive end-expiratory pressure*
- Increasing tidal volume helps reduce pCO2, but increasing PEEP primarily improves **oxygenation** by preventing alveolar collapse and increasing functional residual capacity.
- The patient's pO2 is already high (150 mmHg) with 98% SaO2, so **oxygenation is not the primary concern**; the focus should be on correcting the acidosis by reducing pCO2.
*Increase positive end-expiratory pressure*
- As mentioned, PEEP is primarily used to improve **oxygenation** and manage conditions like acute respiratory distress syndrome (ARDS), which is not the immediate problem here.
- The patient's **pO2 is adequate**, and PEEP will not directly address the **severe metabolic acidosis** or aid significantly in CO2 removal.
Metabolic acidosis mechanisms and compensation US Medical PG Question 6: A 25-year-old woman with an extensive psychiatric history is suspected of having metabolic acidosis after ingesting a large amount of aspirin in a suicide attempt. Labs are drawn and the values from the ABG are found to be: PCO2: 25, and HCO3: 15, but the pH value is smeared on the print-out and illegible. The medical student is given the task of calculating the pH using the pCO2 and HCO3 concentrations. He recalls from his first-year physiology course that the pKa of relevance for the bicarbonate buffering system is approximately 6.1. Which of the following is the correct formula the student should use, using the given values from the incomplete ABG?
- A. 15/6.1 + log[10/(0.03*25)]
- B. 6.1 + log[15/(0.03*25)] (Correct Answer)
- C. 10^6.1 + 15/0.03*25
- D. 6.1 + log[0.03/15*25]
- E. 6.1 + log[25/(15*0.03)]
Metabolic acidosis mechanisms and compensation Explanation: ***6.1 + log[15/(0.03*25)]***
- This formula correctly represents the Henderson-Hasselbalch equation for the bicarbonate buffer system: **pH = pKa + log([HCO3-]/[0.03 * PCO2])**.
- Here, **pKa is 6.1**, **[HCO3-] is 15**, and **[0.03 * PCO2] is 0.03 * 25**, making this the appropriate calculation for pH.
*15/6.1 + log[10/(0.03*25)]*
- This formula incorrectly places the pKa in the denominator of the first term and introduces an arbitrary '10' in the numerator of the logarithmic term.
- The **Henderson-Hasselbalch equation** dictates that pKa is added, not divided into, another component, and the logarithmic term should reflect the ratio of bicarbonate to carbonic acid.
*10^6.1 + 15/0.03*25*
- This option incorrectly uses an exponentiation of pKa and adds it to an unrelated fractional term, which does not correspond to the Henderson-Hasselbalch equation structure.
- The formula for pH calculation is a sum of pKa and a logarithmic term, not an exponentiation and a simple fraction.
*6.1 + log[0.03/15*25]*
- This option incorrectly inverts the ratio within the logarithm, placing the carbonic acid component (0.03 * PCO2) in the numerator and bicarbonate in the denominator.
- The correct Henderson-Hasselbalch equation requires the **bicarbonate concentration in the numerator** and the carbonic acid concentration in the denominator.
*6.1 + log [25/(15*0.03)]*
- This option incorrectly places the PCO2 (25) in the numerator of the logarithmic term and the product of HCO3- and 0.03 in the denominator.
- The correct ratio for the Henderson-Hasselbalch equation is **[HCO3-] / [0.03 * PCO2]**.
Metabolic acidosis mechanisms and compensation US Medical PG Question 7: A 58-year-old man presents to the emergency department with a chief complaint of ringing in his ears that started several hours previously that has progressed to confusion. The patient denies any history of medical problems except for bilateral knee arthritis. He was recently seen by an orthopedic surgeon to evaluate his bilateral knee arthritis but has opted to not undergo knee replacement and prefers medical management. His wife noted that prior to them going on a hike today, he seemed confused and not himself. They decided to stay home, and roughly 14 hours later, he was no longer making any sense. Physical exam is notable for a confused man. The patient's vitals are being performed and his labs are being drawn. Which of the following is most likely to be seen on blood gas analysis?
- A. pH: 7.30, PaCO2: 15 mmHg, HCO3-: 16 mEq/L (Correct Answer)
- B. pH: 7.37, PaCO2: 41 mmHg, HCO3-: 12 mEq/L
- C. pH: 7.41, PaCO2: 65 mmHg, HCO3-: 34 mEq/L
- D. pH: 7.47, PaCO2: 11 mmHg, HCO3-: 24 mEq/L
- E. pH: 7.31, PaCO2: 31 mmHg, HCO3-: 15 mEq/L
Metabolic acidosis mechanisms and compensation Explanation: ***pH: 7.30, PaCO2: 15 mmHg, HCO3-: 16 mEq/L***
- This blood gas analysis shows a **low pH** (acidemia), **low PaCO2** (hypocapnia), and **low HCO3-** (bicarbonate). This pattern is consistent with a **primary metabolic acidosis** with a **compensatory respiratory alkalosis**.
- In this clinical scenario, the patient likely has **salicylate toxicity** (aspirin poisoning). Salicylate toxicity initially causes respiratory alkalosis due to direct stimulation of the respiratory center, followed by a high anion gap metabolic acidosis as salicylates interfere with cellular metabolism. This specific ABG reflects a mixed disorder where metabolic acidosis is predominant and respiratory compensation is attempting to raise the pH. The **tinnitus** and **confusion** are classic symptoms of salicylate toxicity.
*pH: 7.37, PaCO2: 41 mmHg, HCO3-: 12 mEq/L*
- This blood gas shows a **normal pH**, **normal PaCO2**, and **low HCO3-**. This suggests a **compensated metabolic acidosis**, where the body has fully compensated to bring the pH back to normal.
- While the patient likely has metabolic acidosis from salicylate toxicity, full compensation to a normal pH is less characteristic of an acute, severe presentation with significant neurological symptoms.
*pH: 7.41, PaCO2: 65 mmHg, HCO3-: 34 mEq/L*
- This blood gas shows a **normal pH**, **high PaCO2**, and **high HCO3-**. This indicates a **compensated respiratory acidosis**, where the kidneys have compensated for chronic CO2 retention.
- This pattern is not consistent with salicylate toxicity, which typically causes **respiratory alkalosis** early on, and later **metabolic acidosis**.
*pH: 7.47, PaCO2: 11 mmHg, HCO3-: 24 mEq/L*
- This blood gas analysis shows a **high pH** (alkalemia), **very low PaCO2** (severe hypocapnia), and a **normal HCO3-**. This indicates a **primary respiratory alkalosis** with no significant metabolic compensation.
- While salicylate toxicity can cause respiratory alkalosis, severe confusion and the progression of symptoms suggest a more advanced stage, usually involving a metabolic acidosis component, making a pure, uncompensated respiratory alkalosis less likely.
*pH: 7.31, PaCO2: 31 mmHg, HCO3-: 15 mEq/L*
- This blood gas shows a **low pH**, **low PaCO2**, and **low HCO3-**. This also indicates a **metabolic acidosis** with **respiratory compensation**.
- However, compared to pH 7.30, PaCO2 15 mmHg, and HCO3- 16 mEq/L, this option shows slightly **less severe respiratory compensation** (PaCO2 is higher), which is less typical for the profound respiratory stimulation seen in severe salicylate poisoning. The chosen correct option demonstrates a more characteristic and maximal respiratory compensation for the degree of metabolic acidosis.
Metabolic acidosis mechanisms and compensation US Medical PG Question 8: A person is exercising strenuously on a treadmill for 1 hour. An arterial blood gas measurement is then taken. Which of the following are the most likely values?
- A. pH 7.56, PaO2 100, PCO2 44, HCO3 38
- B. pH 7.32, PaO2 42, PCO2 50, HCO3 27
- C. pH 7.57 PaO2 100, PCO2 23, HCO3 21 (Correct Answer)
- D. pH 7.38, PaO2 100, PCO2 69 HCO3 42
- E. pH 7.36, PaO2 100, PCO2 40, HCO3 23
Metabolic acidosis mechanisms and compensation Explanation: ***pH 7.57, PaO2 100, PCO2 23, HCO3 21***
- After 1 hour of strenuous exercise, this represents **respiratory alkalosis with mild metabolic compensation**, which is the expected finding in a healthy individual during sustained vigorous exercise.
- The **low PCO2 (23 mmHg)** reflects appropriate **hyperventilation** in response to increased metabolic demands and lactic acid production. During intense exercise, minute ventilation increases dramatically, often exceeding the rate of CO2 production.
- The **slightly elevated pH (7.57)** and **mildly decreased HCO3 (21 mEq/L)** indicate that respiratory compensation has slightly overshot, creating mild alkalosis, while the bicarbonate is consumed both in buffering lactate and through renal compensation.
- **Normal PaO2 (100 mmHg)** confirms adequate oxygenation maintained by increased ventilation.
*pH 7.36, PaO2 100, PCO2 40, HCO3 23*
- These are **completely normal arterial blood gas values** with no evidence of any physiological stress or compensation.
- After 1 hour of strenuous exercise, we would expect **hyperventilation with decreased PCO2**, not a normal PCO2 of 40 mmHg. This profile would be consistent with rest, not vigorous exercise.
- The absence of any respiratory or metabolic changes makes this inconsistent with the clinical scenario.
*pH 7.56, PaO2 100, PCO2 44, HCO3 38*
- This profile suggests **metabolic alkalosis** (high pH, high HCO3) with inadequate respiratory compensation (normal to slightly elevated PCO2).
- This is **not consistent with strenuous exercise**, which produces metabolic acid (lactate), not metabolic base. The elevated HCO3 suggests vomiting, diuretic use, or other causes of metabolic alkalosis.
*pH 7.32, PaO2 42, PCO2 50, HCO3 27*
- This indicates **respiratory acidosis** (low pH, high PCO2) with **severe hypoxemia** (PaO2 42 mmHg).
- During strenuous exercise, healthy individuals **increase ventilation** to enhance O2 delivery and remove CO2, so both hypoxemia and hypercapnia are unexpected and would suggest severe cardiopulmonary disease or hypoventilation.
*pH 7.38, PaO2 100, PCO2 69, HCO3 42*
- This demonstrates **compensated respiratory acidosis** (normal pH, markedly elevated PCO2 and HCO3).
- The **very high PCO2 (69 mmHg)** indicates severe **hypoventilation**, which is the opposite of what occurs during exercise. This profile suggests chronic respiratory failure with metabolic compensation, such as in severe COPD.
Metabolic acidosis mechanisms and compensation US Medical PG Question 9: A 32-year-old woman is admitted to the emergency department for 36 hours of intense left-sided back pain that extends into her left groin. She reports that the pain started a day after a charitable 5 km (3.1 mi) marathon. The past medical history is relevant for multiple complaints of eye dryness and dry mouth. Physical examination is unremarkable, except for intense left-sided costovertebral pain. The results from laboratory tests are shown.
Laboratory test Result
Serum Na+ 137
Serum Cl- 110
Serum K+ 3.0
Serum creatinine (SCr) 0.82
Arterial blood gas Result
pH 7.28
pO2 98 mm Hg
pCO2 28.5 mm Hg
SaO2% 98%
HCO3- 15 mm Hg
Which of the following explains this patient’s condition?
- A. Carbonic acid accumulation
- B. Decreased bicarbonate renal absorption
- C. Decreased renal excretion of hydrogen ions (H+) (Correct Answer)
- D. Decreased synthesis of ammonia (NH3)
- E. Decreased excretion of nonvolatile acids
Metabolic acidosis mechanisms and compensation Explanation: ***Decreased renal excretion of hydrogen ions (H+)***
- The patient presents with **metabolic acidosis** (pH 7.28, HCO3- 15 mEq/L) with **respiratory compensation** (pCO2 28.5 mm Hg). The anion gap is **normal** (Na+ - (Cl- + HCO3-) = 137 - (110 + 15) = **12 mEq/L**), indicating a **non-anion gap metabolic acidosis**.
- The history of **dry eyes and dry mouth** strongly suggests **Sjögren syndrome**, which is commonly associated with **Type 1 (distal) renal tubular acidosis**.
- In **Type 1 RTA**, the distal tubule alpha-intercalated cells cannot adequately secrete H+ ions, leading to metabolic acidosis with **inability to acidify urine** (urine pH > 5.5). Associated findings include **hypokalemia** (K+ 3.0), **nephrolithiasis** (calcium phosphate stones due to alkaline urine), and hypercalciuria.
- The left-sided flank pain radiating to the groin is consistent with **nephrolithiasis**, a common complication of Type 1 RTA.
*Carbonic acid accumulation*
- **Carbonic acid accumulation** indicates **respiratory acidosis** with elevated pCO2, which is not present here.
- The patient has a **low pCO2 (28.5 mm Hg)**, representing appropriate **respiratory compensation** for the primary metabolic acidosis.
*Decreased bicarbonate renal absorption*
- **Decreased bicarbonate renal absorption** characterizes **Type 2 (proximal) RTA**.
- While Type 2 RTA also causes non-anion gap metabolic acidosis, it is **not typically associated with Sjögren syndrome** and would present with different features (glycosuria, aminoaciduria, phosphaturia as part of Fanconi syndrome).
- Type 2 RTA can acidify urine to pH < 5.5 when serum HCO3- is low, unlike Type 1 RTA.
*Decreased synthesis of ammonia (NH3)*
- **Decreased ammonia synthesis** is characteristic of **Type 4 RTA** or severe chronic kidney disease.
- Type 4 RTA presents with **hyperkalemia** (due to hypoaldosteronism), not the hypokalemia seen in this patient.
- The normal serum creatinine (0.82 mg/dL) rules out significant renal failure.
*Decreased excretion of nonvolatile acids*
- **Decreased excretion of nonvolatile acids** would cause **elevated anion gap metabolic acidosis** (e.g., lactic acidosis, ketoacidosis, or advanced renal failure with accumulation of organic acids).
- This patient has a **normal anion gap (12 mEq/L)** and **normal renal function** (creatinine 0.82 mg/dL), making this mechanism unlikely.
- The clinical context of Sjögren syndrome with dry eyes/mouth points specifically to distal RTA.
Metabolic acidosis mechanisms and compensation US Medical PG Question 10: Two hours after undergoing laparoscopic roux-en-Y gastric bypass surgery, a 44-year-old man complains of pain in the site of surgery and nausea. He has vomited twice in the past hour. He has hypertension, type 2 diabetes mellitus, and hypercholesterolemia. Current medications include insulin, atorvastatin, hydrochlorothiazide, acetaminophen, and prophylactic subcutaneous heparin. He drinks two to three beers daily and occasionally more on weekends. He is 177 cm (5 ft 10 in) tall and weighs 130 kg (286 lb); BMI is 41.5 kg/m2. His temperature is 37.3°C (99.1°F), pulse is 103/min, and blood pressure is 122/82 mm Hg. Examination shows five laparoscopic incisions with no erythema or discharge. The abdomen is soft and non-distended. There is slight diffuse tenderness to palpation. Bowel sounds are reduced. Laboratory studies show:
Hematocrit 45%
Serum
Na+ 136 mEq/L
K+ 3.5 mEq/L
Cl- 98 mEq/L
Urea nitrogen 31 mg/dL
Glucose 88 mg/dL
Creatinine 1.1 mg/dL
Arterial blood gas analysis on room air shows:
pH 7.28
pCO2 32 mm Hg
pO2 74 mm Hg
HCO3- 14.4 mEq/L
Which of the following is the most likely cause for the acid-base status of this patient?
- A. Hypoxia (Correct Answer)
- B. Uremia
- C. Late dumping syndrome
- D. Vomiting
- E. Early dumping syndrome
Metabolic acidosis mechanisms and compensation Explanation: ***Hypoxia***
- The patient exhibits **metabolic acidosis** (pH 7.28, HCO3- 14.4 mEq/L) with **appropriate respiratory compensation** (pCO2 32 mm Hg using Winter's formula: expected pCO2 = 1.5 × 14.4 + 8 ± 2 = 29.6 ± 2).
- The **pO2 of 74 mm Hg is significantly low** (normal range on room air: 80-100 mm Hg), indicating **hypoxemia** that leads to **tissue hypoxia** and **anaerobic metabolism**.
- In the setting of **obesity (BMI 41.5)** and **immediate post-operative status** after laparoscopic surgery, multiple factors contribute to hypoxemia including **atelectasis, reduced functional residual capacity, pain limiting deep breathing, residual anesthetic effects, and pneumoperitoneum effects**.
- Tissue hypoxia results in **lactic acidosis** (a high anion gap metabolic acidosis), which explains the acid-base disturbance. The **elevated BUN (31 mg/dL) with relatively normal creatinine** suggests prerenal azotemia from hypoperfusion, further supporting inadequate tissue oxygenation.
- The **tachycardia (103/min)** represents a compensatory response to improve oxygen delivery to hypoxic tissues.
*Vomiting*
- Vomiting causes loss of **gastric HCl**, resulting in **hypochloremic metabolic ALKALOSIS** (elevated pH and HCO3-), not acidosis.
- While this patient is vomiting, the acid-base status shows **acidosis**, which is the opposite of what vomiting typically causes.
- The low **Cl- (98 mEq/L)** is consistent with some gastric acid loss, but the dominant acid-base disorder is metabolic acidosis from another cause.
*Uremia*
- **Uremia** causes high anion gap metabolic acidosis due to retention of organic acids and phosphates in renal failure.
- While the **BUN is elevated (31 mg/dL)**, the **creatinine (1.1 mg/dL) is essentially normal**, especially for a patient with high muscle mass (130 kg).
- The BUN elevation is more consistent with **prerenal azotemia** (dehydration/hypoperfusion) rather than intrinsic renal failure causing uremic acidosis.
*Late dumping syndrome*
- **Late dumping syndrome** occurs **1-3 hours after eating** and results from rapid carbohydrate absorption causing hyperinsulinemia and subsequent **reactive hypoglycemia**.
- This patient's **glucose is normal (88 mg/dL)**, and symptoms began only **2 hours post-surgery** in the fasting state, not after a meal.
- Late dumping does not cause metabolic acidosis.
*Early dumping syndrome*
- **Early dumping syndrome** occurs **10-30 minutes after eating** due to rapid gastric emptying of hyperosmolar contents into the small intestine, causing fluid shifts.
- Symptoms include **cramping, diarrhea, vasomotor symptoms (flushing, palpitations, dizziness)**, not metabolic acidosis.
- This patient has not yet eaten post-operatively, making dumping syndrome impossible.
More Metabolic acidosis mechanisms and compensation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.