Renal excretion mechanisms US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Renal excretion mechanisms. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
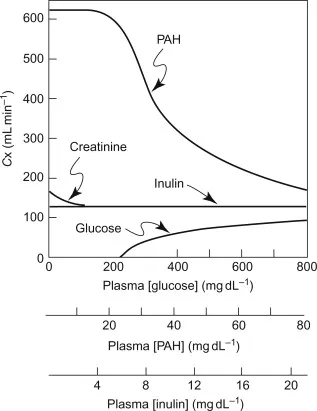
Renal excretion mechanisms US Medical PG Question 1: A patient is receiving daily administrations of Compound X. Compound X is freely filtered in the glomeruli and undergoes net secretion in the renal tubules. The majority of this tubular secretion occurs in the proximal tubule. Additional information regarding this patient's renal function and the renal processing of Compound X is included below:
Inulin clearance: 120 mL/min
Plasma concentration of Inulin: 1 mg/mL
PAH clearance: 600 mL/min
Plasma concentration of PAH: 0.2 mg/mL
Total Tubular Secretion of Compound X: 60 mg/min
Net Renal Excretion of Compound X: 300 mg/min
Which of the following is the best estimate of the plasma concentration of Compound X in this patient?
- A. 2 mg/mL (Correct Answer)
- B. 3 mg/mL
- C. There is insufficient information available to estimate the plasma concentration of Compound X
- D. 1 mg/mL
- E. 0.5 mg/mL
Renal excretion mechanisms Explanation: ***2 mg/mL***
* The **net renal excretion of Compound X (300 mg/min)** is the sum of the filtered load and the net tubular secretion.
* Given that Compound X is **freely filtered** and undergoes **net secretion (60 mg/min)**, we can calculate the filtered load and subsequently its plasma concentration.
* **Net excretion = Filtered load + Net tubular secretion**
* **300 mg/min = Filtered load + 60 mg/min**
* **Filtered load = 300 mg/min - 60 mg/min = 240 mg/min**
* Since **Filtered load = Glomerular Filtration Rate (GFR) * Plasma concentration (P_X)**, and GFR is estimated by **inulin clearance (120 mL/min)**:
* **240 mg/min = 120 mL/min * P_X**
* **P_X = 240 mg/min / 120 mL/min = 2 mg/mL**.
*3 mg/mL*
* This value would imply a significantly higher filtered load or a different contribution from tubular secretion.
* Calculations using this plasma concentration would not align with the provided excretion and secretion rates.
*There is insufficient information available to estimate the plasma concentration of Compound X*
* The problem provides all necessary values: **Inulin clearance (GFR)**, **net tubular secretion of Compound X**, and **net renal excretion of Compound X**.
* These parameters are sufficient to determine the filtered load and thus the plasma concentration of Compound X.
*1 mg/mL*
* A plasma concentration of 1 mg/mL would result in a lower filtered load than calculated and would not account for the observed net renal excretion.
* **Filtered load = 120 mL/min * 1 mg/mL = 120 mg/min**. Total excretion would then be 120 mg/min + 60 mg/min = 180 mg/min, which contradicts the given 300 mg/min.
*0.5 mg/mL*
* This plasma concentration would lead to an even lower filtered load, making it impossible to achieve the *net renal excretion of Compound X* given the tubular secretion.
* **Filtered load = 120 mL/min * 0.5 mg/mL = 60 mg/min**. Total excretion would be 60 mg/min + 60 mg/min = 120 mg/min, which is much lower than the given 300 mg/min.
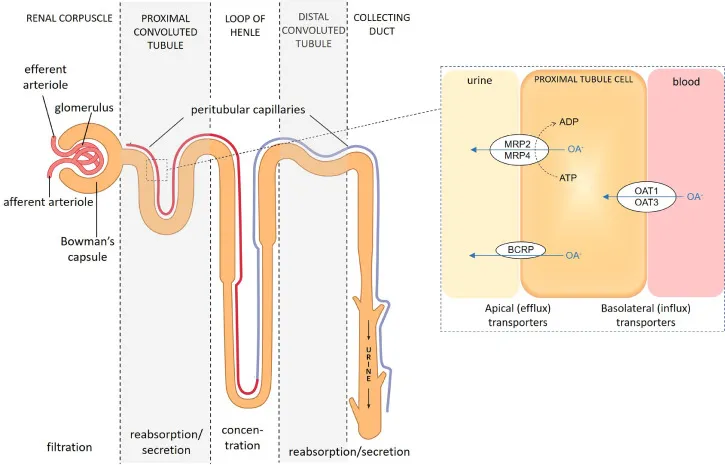
Renal excretion mechanisms US Medical PG Question 2: On cardiology service rounds, your team sees a patient admitted with an acute congestive heart failure exacerbation. In congestive heart failure, decreased cardiac function leads to decreased renal perfusion, which eventually leads to excess volume retention. To test your knowledge of physiology, your attending asks you which segment of the nephron is responsible for the majority of water absorption. Which of the following is a correct pairing of the segment of the nephron that reabsorbs the majority of all filtered water with the means by which that segment absorbs water?
- A. Distal convoluted tubule via passive diffusion following ion reabsorption
- B. Distal convoluted tubule via aquaporin channels
- C. Thick ascending loop of Henle via passive diffusion following ion reabsorption
- D. Proximal convoluted tubule via passive diffusion following ion reabsorption (Correct Answer)
- E. Collecting duct via aquaporin channels
Renal excretion mechanisms Explanation: ***Proximal convoluted tubule via passive diffusion following ion reabsorption***
- The **proximal convoluted tubule (PCT)** is responsible for reabsorbing approximately **65-70% of filtered water**, making it the primary site of water reabsorption in the nephron.
- This water reabsorption primarily occurs **passively**, following the active reabsorption of solutes (especially **sodium ions**), which creates an osmotic gradient.
*Distal convoluted tubule via passive diffusion following ion reabsorption*
- The **distal convoluted tubule (DCT)** reabsorbs a much smaller percentage of filtered water (around 5-10%) and its water reabsorption is largely **regulated by ADH**, not primarily simple passive diffusion following bulk ion reabsorption.
- While some passive water movement occurs, it is not the main mechanism or location for the majority of water reabsorption.
*Distal convoluted tubule via aquaporin channels*
- While aquaporin channels do play a role in water reabsorption in the DCT, particularly under the influence of **ADH**, the DCT is not the segment responsible for the **majority of all filtered water absorption**.
- The bulk of water reabsorption occurs earlier in the nephron, independently of ADH for the most part.
*Thick ascending loop of Henle via passive diffusion following ion reabsorption*
- The **thick ascending loop of Henle** is primarily involved in reabsorbing ions like Na+, K+, and Cl- but is largely **impermeable to water**.
- Its impermeability to water is crucial for creating the **osmotic gradient** in the renal medulla, which is necessary for later water reabsorption.
*Collecting duct via aquaporin channels*
- The **collecting duct** is critically important for **regulated water reabsorption** via **aquaporin-2 channels** under the influence of **ADH**, allowing for fine-tuning of urine concentration.
- However, it reabsorbs only a variable portion (typically 5-19%) of the remaining filtered water, not the **majority of all filtered water**.
Renal excretion mechanisms US Medical PG Question 3: A new drug has been shown to block epithelial sodium channels in the cortical collecting duct. Which of the following is most likely to be decreased upon drug administration?
- A. Urea reabsorption in the collecting tubules
- B. Hydrogen ion secretion in the collecting tubules
- C. Potassium secretion in the collecting tubules (Correct Answer)
- D. Sodium secretion in the collecting tubules
- E. Sodium chloride reabsorption in the distal tubule
Renal excretion mechanisms Explanation: ***Potassium secretion in the collecting tubules***
- Blocking **epithelial sodium channels (ENaC)** in the cortical collecting duct reduces sodium reabsorption, which in turn diminishes the electrochemical gradient driving **potassium secretion** into the lumen.
- This is because sodium reabsorption creates a more negative luminal charge, attracting potassium ions to move from the cell into the tubule.
- This is the mechanism of **potassium-sparing diuretics** like amiloride and triamterene.
*Urea reabsorption in the collecting tubules*
- Urea **reabsorption** primarily occurs in the **medullary collecting duct** via urea transporters (UT-A1, UT-A3) and is influenced by the inner medullary osmolarity and ADH.
- Blocking ENaC would primarily affect sodium flux and potassium secretion, with minimal direct impact on urea reabsorption in the collecting duct.
*Hydrogen ion secretion in the collecting tubules*
- **Hydrogen ion (H+) secretion** occurs in the collecting tubules via intercalated cells (α-intercalated cells), which is important for acid-base balance.
- While blocking ENaC can indirectly reduce H+ secretion (by decreasing the lumen-negative potential), the primary and most significant effect is on **potassium secretion**, making this a less likely answer.
*Sodium secretion in the collecting tubules*
- The primary function of ENaC is to **reabsorb sodium** from the tubular lumen back into the blood, not to secrete it.
- Sodium is not normally secreted in the collecting tubules; blocking ENaC would decrease sodium **reabsorption**, not affect sodium secretion.
*Sodium chloride reabsorption in the distal tubule*
- **Sodium chloride reabsorption** in the distal convoluted tubule is mainly mediated by the **thiazide-sensitive Na-Cl co-transporter (NCC)**.
- ENaC are predominantly located in the cortical collecting duct (downstream from the DCT), so blocking them would not directly impact NaCl reabsorption in the distal tubule.
Renal excretion mechanisms US Medical PG Question 4: Which transport mechanism is primarily responsible for calcium reabsorption in the proximal tubule?
- A. Paracellular transport (Correct Answer)
- B. Facilitated diffusion
- C. Active transport
- D. Antiport with sodium
Renal excretion mechanisms Explanation: ***Paracellular transport***
- In the **proximal tubule**, approximately 60-70% of filtered calcium is reabsorbed primarily through the **paracellular pathway**, driven by the electrochemical gradient and solvent drag.
- This transport occurs between cells, moving through the **tight junctions**, and is passive, following the reabsorption of water.
*Facilitated diffusion*
- While a type of passive transport, **facilitated diffusion** typically involves membrane proteins and occurs across the cell membrane, not primarily between cells in the proximal tubule for calcium.
- This mechanism is prominent for calcium reabsorption in other nephron segments like the **distal convoluted tubule** via **TRPV5/6 channels**, but not the main route in the proximal tubule.
*Active transport*
- **Active transport** of calcium, mainly via **calcium ATPase** and the **Na+/Ca2+ exchanger**, occurs across the luminal and basolateral membranes, respectively, in specific nephron segments.
- However, in the **proximal tubule**, the bulk of calcium reabsorption is passive and paracellular, not ATP-dependent active transport across cell membranes.
*Antiport with sodium*
- The **Na+/Ca2+ exchanger (NCX)** is an antiport mechanism that plays a crucial role in extruding calcium from the cell into the interstitium, particularly in the basolateral membrane of the distal tubule.
- However, it is not the primary mechanism for overall tubular reabsorption of calcium in the **proximal tubule**, where paracellular movement dominates.
Renal excretion mechanisms US Medical PG Question 5: An investigator is studying the effect of antihypertensive drugs on cardiac output and renal blood flow. For comparison, a healthy volunteer is given a placebo and a continuous infusion of para-aminohippuric acid (PAH) to achieve a plasma concentration of 0.02 mg/ml. His urinary flow rate is 1.5 ml/min and the urinary concentration of PAH is measured to be 8 mg/ml. His hematocrit is 50%. Which of the following values best estimates cardiac output in this volunteer?
- A. 8 L/min
- B. 3 L/min
- C. 4 L/min
- D. 1.2 L/min
- E. 6 L/min (Correct Answer)
Renal excretion mechanisms Explanation: ***6 L/min***
- This value represents the estimated **cardiac output** based on the calculated renal blood flow.
- Step 1: Calculate renal plasma flow (RPF) using PAH clearance: RPF = (Urinary PAH × Urine flow rate) / Plasma PAH = (8 mg/ml × 1.5 ml/min) / 0.02 mg/ml = 600 ml/min = 0.6 L/min
- Step 2: Calculate renal blood flow (RBF): Since hematocrit is 50%, RBF = RPF / (1 - Hematocrit) = 0.6 / 0.5 = 1.2 L/min
- Step 3: Estimate cardiac output: The kidneys normally receive approximately **20-25% of cardiac output**. Using 20%: Cardiac Output = RBF / 0.20 = 1.2 / 0.20 = **6 L/min**
- This is consistent with normal resting cardiac output in a healthy adult.
*8 L/min*
- This value overestimates cardiac output based on the renal blood flow calculation.
- While some individuals may have higher cardiac output during exercise, the calculated RBF of 1.2 L/min suggests a resting cardiac output closer to 6 L/min.
*3 L/min*
- This value significantly underestimates cardiac output.
- If cardiac output were 3 L/min, the kidneys would be receiving 40% of cardiac output (1.2/3), which is physiologically implausible at rest.
*4 L/min*
- This value underestimates cardiac output based on the renal data.
- This would mean kidneys receive 30% of cardiac output (1.2/4), which is higher than the typical 20-25%.
*1.2 L/min*
- This is the calculated **renal blood flow**, not cardiac output.
- While this calculation is correct for RBF, the question specifically asks for cardiac output estimation, which requires accounting for the fact that kidneys receive only about 20-25% of total cardiac output.
Renal excretion mechanisms US Medical PG Question 6: A 50-year-old woman presents to the ED 6 hours after ingesting three bottles of baby aspirin. She complains of nausea, vomiting, dizziness, and tinnitus. Her blood pressure is 135/80 mmHg, pulse is 110/min, respirations are 32/min, temperature is 100.1 deg F (37.8 deg C), and oxygen saturation is 99% on room air. Arterial blood gas at room air shows, PCO2 11 mmHg, and PO2 129 mmHg. Blood salicylate level is 55 mg/dL. Management should involve which of the following acid-base principles?
- A. Serum neutralization, urine alkalization
- B. Serum alkalization, urine alkalization (Correct Answer)
- C. Serum neutralization, urine acidification
- D. Serum acidification, urine acidification
- E. Serum acidification, urine alkalization
Renal excretion mechanisms Explanation: ***Serum alkalization, urine alkalization***
- Managing **aspirin overdose** involves **aggressive serum alkalization** to promote the shift of salicylic acid from the cells into the bloodstream, where it remains ionized and cannot freely diffuse into the CNS. This also reduces its toxicity by increasing the proportion of the ionized form.
- Subsequently, **urine alkalization** with **sodium bicarbonate** is used to trap the ionized salicylate in the renal tubules, preventing reabsorption and enhancing its excretion.
*Serum neutralization, urine alkalization*
- This option is flawed because the goal is not to "neutralize" the serum pH to a neutral 7.0 but rather to raise it above normal towards an alkaline state (typically pH 7.45-7.55) to enhance salicylate elimination.
- While urine alkalization is correct, the idea of serum neutralization is incorrect and could lead to inadequate treatment.
*Serum neutralization, urine acidification*
- This approach is entirely incorrect for **salicylate toxicity** as **acidifying the urine** would promote the reabsorption of salicylic acid from the renal tubules, worsening toxicity.
- Serum neutralization, as mentioned, is not the correct term or goal for managing **aspirin overdose**.
*Serum acidification, urine acidification*
- This strategy would be **dangerous** in the context of **salicylate overdose** as it would significantly increase the proportion of **non-ionized salicylic acid**, allowing it to more readily cross cell membranes, including the blood-brain barrier, thereby increasing systemic and central nervous system toxicity.
- It would also drastically reduce elimination.
*Serum acidification, urine alkalization*
- **Serum acidification** is contraindicated in **salicylate poisoning** as it drives salicylate into the tissues, exacerbating its toxicity, particularly in the central nervous system.
- While urine alkalization is correct for enhancing elimination, combining it with serum acidification would counteract its benefits and worsen patient outcomes.
Renal excretion mechanisms US Medical PG Question 7: A researcher is investigating the effects of a new antihypertensive medication on renal physiology. She gives a subject a dose of the new medication, and she then collects plasma and urine samples. She finds the following: Hematocrit: 40%; Serum creatinine: 0.0125 mg/mL; Urine creatinine: 1.25 mg/mL. Urinary output is 1 mL/min. Renal blood flow is 1 L/min. Based on the above information and approximating that the creatinine clearance is equal to the GFR, what answer best approximates filtration fraction in this case?
- A. 10%
- B. 17% (Correct Answer)
- C. 33%
- D. 50%
- E. 25%
Renal excretion mechanisms Explanation: ***17%***
- First, calculate **GFR** using the creatinine clearance formula: GFR = (Urine creatinine × Urinary output) / Serum creatinine = (1.25 mg/mL × 1 mL/min) / 0.0125 mg/mL = **100 mL/min**.
- Next, calculate **Renal Plasma Flow (RPF)** from Renal Blood Flow (RBF) and Hematocrit: RPF = RBF × (1 - Hematocrit) = 1000 mL/min × (1 - 0.40) = **600 mL/min**.
- Finally, calculate **Filtration Fraction (FF)** = GFR / RPF = 100 mL/min / 600 mL/min = 0.1667 = **16.7%, which approximates to 17%**.
- This is the correct answer based on the physiological calculations and represents a normal filtration fraction.
*10%*
- This would correspond to a filtration fraction of 0.10, which would require either a GFR of 60 mL/min (lower than calculated) or an RPF of 1000 mL/min (higher than calculated).
- This value is too low given the provided parameters and doesn't match the calculation from the given data.
*25%*
- This value would suggest FF = 0.25, requiring a GFR of 150 mL/min with the calculated RPF of 600 mL/min.
- This is higher than the calculated GFR of 100 mL/min and doesn't match the given creatinine values.
*33%*
- This would imply FF = 0.33, requiring a GFR of approximately 200 mL/min with RPF of 600 mL/min.
- This is significantly higher than the calculated GFR and would represent an abnormally elevated filtration fraction.
*50%*
- A filtration fraction of 50% is unphysiologically high and would indicate severe pathology.
- This would require a GFR of 300 mL/min with the calculated RPF, which is impossible given the provided creatinine clearance data.
Renal excretion mechanisms US Medical PG Question 8: A 17-year-old woman is rushed into the emergency department by her father who found her collapsed in her bedroom 15 minutes before the ambulance's arrival. There was an empty bottle of clomipramine in her bedroom which her mother takes for her depression. Vital signs include the following: respiratory rate 8/min, pulse 130/min, and blood pressure 100/60 mm Hg. On physical examination, the patient is unresponsive to vocal and tactile stimuli. Oral mucosa and tongue are dry, and the bladder is palpable. A bedside electrocardiogram (ECG) shows widening of the QRS complexes. Which of the following would be the best course of treatment in this patient?
- A. Norepinephrine
- B. Sodium bicarbonate (Correct Answer)
- C. Diazepam
- D. Lidocaine
- E. Induced vomiting
Renal excretion mechanisms Explanation: ***Sodium bicarbonate***
- The patient presents with classic signs of **tricyclic antidepressant (TCA) overdose**, including coma, tachycardia, hypotension, dry oral mucosa (anticholinergic effects), urinary retention, and significantly, **widened QRS complexes** on ECG.
- **Sodium bicarbonate** is the treatment of choice for TCA overdose-induced cardiotoxicity, as it alkalinizes the blood, reducing the binding of TCAs to myocardial fast sodium channels and improving cardiac conduction.
- The primary indication is **QRS widening >100 ms**, which indicates severe sodium channel blockade and increased risk of ventricular arrhythmias.
*Norepinephrine*
- While the patient is hypotensive, **norepinephrine** (a vasopressor) primarily addresses blood pressure and not the underlying cardiotoxicity or arrhythmias caused by TCA overdose.
- Using vasopressors without addressing the membrane-stabilizing effects of TCAs on the heart may not resolve the critical cardiac issues.
- Sodium bicarbonate should be administered first to address the cardiotoxicity.
*Diazepam*
- **Diazepam** is a benzodiazepine used to treat seizures or agitation, which can sometimes occur in TCA overdose.
- However, it does not address the vital signs or the severe cardiotoxicity (widened QRS) which is the most life-threatening complication here.
*Lidocaine*
- **Lidocaine** is an antiarrhythmic drug; however, it is relatively contraindicated in TCA overdose as it blocks cardiac sodium channels, which could worsen the existing sodium channel blockade caused by TCAs.
- This could exacerbate QRS widening and increase the risk of malignant arrhythmias.
*Induced vomiting*
- **Induced vomiting** (e.g., with ipecac syrup) is contraindicated in cases of overdose, particularly with altered mental status, due to the high risk of **aspiration pneumonitis**.
- In a patient who is unresponsive, attempts at gastric decontamination via emesis are dangerous and ineffective.
Renal excretion mechanisms US Medical PG Question 9: A 59-year-old man presents with intense, sharp pain in his toe for the past hour. He reports similar symptoms in the past and this is his 2nd visit to the emergency department this year with the same complaint. The patient is afebrile and the vital signs are within normal limits. On physical examination, there is significant erythema, swelling, warmth, and moderate pain on palpation of the right 1st toe. The remainder of the examination is unremarkable. A plain radiograph of the right foot reveals no abnormalities. Joint arthrocentesis of the inflamed toe reveals urate crystals. Laboratory studies show:
Serum glucose (random) 170 mg/dL
Sodium 140 mEq/L
Potassium 4.1 mEq/L
Chloride 100 mEq/L
Uric acid 7.2 mg/dL
Serum creatinine 0.8 mg/dL
Blood urea nitrogen 9 mg/dL
Cholesterol, total 170 mg/dL
HDL-cholesterol 43 mg/dL
LDL-cholesterol 73 mg/dL
Triglycerides 135 mg/dL
HDL: high-density lipoprotein; LDL: low-density lipoprotein
Ibuprofen is prescribed for the acute treatment of this patient's symptoms. He is also put on chronic therapy to prevent the recurrence of future attacks. Which of the following drugs is 1st-line for chronic therapy of gout?
- A. Methotrexate
- B. Indomethacin
- C. Probenecid
- D. Colchicine
- E. Allopurinol (Correct Answer)
Renal excretion mechanisms Explanation: ***Allopurinol***
- Allopurinol is a **xanthine oxidase inhibitor** that reduces uric acid production, making it the **first-line therapy** for **chronic gout management**.
- It effectively **lowers serum uric acid levels** to prevent recurrent attacks and dissolution of urate crystals.
*Methotrexate*
- Methotrexate is a **disease-modifying antirheumatic drug (DMARD)** primarily used in conditions like **rheumatoid arthritis** and **psoriasis**.
- It is **not indicated for gout** as it does not target uric acid metabolism.
*Indomethacin*
- Indomethacin is an **NSAID** commonly used for the **acute treatment of gout flares** due to its potent anti-inflammatory effects.
- It is **not suitable for chronic management** or prevention of gout due to potential long-term side effects and lack of effect on uric acid levels.
*Probenecid*
- Probenecid is a **uricosuric agent** that increases renal excretion of uric acid.
- While it lowers uric acid, it is typically considered a **second-line agent** for chronic gout, especially in patients with underexcretion of uric acid, or as an alternative to allopurinol if it cannot be tolerated.
*Colchicine*
- Colchicine is used for both **acute gout flares** and as **prophylaxis** during the initiation of uric acid-lowering therapy to prevent flares.
- It is **not a first-line drug for chronic gout management** as it does not lower uric acid levels; it primarily reduces inflammation.
Renal excretion mechanisms US Medical PG Question 10: A 55-year-old man presents to the urgent clinic complaining of pain in his right foot. He reported that the pain is intense that he had to remove his shoe and sock, and rates the pain level as 6 out of 10. He does not report trauma or recent infection. The past medical history includes hypertension. The medications include hydrochlorothiazide, enalapril, and a daily multivitamin. The family history is noncontributory. He consumes alcohol in moderation. His diet mostly consists of red meat and white rice. The blood pressure is 137/85 mm Hg, heart rate is 74/min, respiratory rate is 12/min, and the temperature is 36.9°C (98.4°F). The physical examination demonstrates swelling, redness, and tenderness to palpation in the first metatarsophalangeal joint of his right foot. There are no skin lesions. The rest of the patient’s examination is normal. An arthrocentesis procedure is scheduled. Which of the following is the most likely pharmacological treatment for the presented patient?
- A. Diclofenac alone (Correct Answer)
- B. Allopurinol alone
- C. Probenecid alone
- D. Colchicine and celecoxib
- E. Oral methylprednisolone and meloxicam
Renal excretion mechanisms Explanation: - ***Diclofenac alone***
- This patient presents with a classic picture of **acute gout**: sudden onset of severe pain, swelling, redness, and tenderness in the **first metatarsophalangeal joint** (podagra), with a history of hypertension and diuretic use (hydrochlorothiazide), and a diet rich in red meat.
- **NSAIDs like diclofenac** are first-line treatment for acute gout attacks, as they effectively reduce pain and inflammation.
- *Allopurinol alone*
- **Allopurinol** is a **xanthine oxidase inhibitor** used for the **long-term prevention** of gout attacks by lowering uric acid levels. It is not indicated for the management of acute flare-ups.
- Initiating allopurinol during an acute attack can paradoxically **worsen the flare** by mobilizing uric acid crystals.
- *Probenecid alone*
- **Probenecid** is a **uricosuric agent** that increases uric acid excretion via the kidneys and is used for **long-term management** of gout in patients who are underexcretors of uric acid.
- Like allopurinol, it is **not used for acute gout attacks** and should not be initiated during a flare.
- *Colchicine and celecoxib*
- **Colchicine** is an effective treatment for acute gout, particularly if given within the first 24-36 hours of symptom onset, but it can cause **significant gastrointestinal side effects** (nausea, vomiting, diarrhea).
- **Celecoxib** is a **COX-2 selective NSAID** which is also effective in acute gout. However, combining colchicine with another NSAID like celecoxib for initial treatment might be an **overkill** in terms of side effects and typically **only one first-line agent (NSAID or colchicine) is sufficient.**
- *Oral methylprednisolone and meloxicam*
- **Oral methylprednisolone (corticosteroids)** are highly effective for acute gout, especially in patients with **contraindications to NSAIDs** or who have polyarticular involvement.
- **Meloxicam** is an NSAID, and while appropriate for acute gout, combining it with systemic corticosteroids (methylprednisolone) is **usually reserved for more severe cases** or when monotherapy is insufficient, due to increased risk of side effects.
More Renal excretion mechanisms US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.