Phase II metabolism (conjugation reactions) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Phase II metabolism (conjugation reactions). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Phase II metabolism (conjugation reactions) US Medical PG Question 1: A 72-year-old man presents to the emergency department with a 1 hour history of bruising and bleeding. He says that he fell and scraped his knee on the ground. Since then, he has been unable to stop the bleeding and has developed extensive bruising around the area. He has a history of gastroesophageal reflux disease, hypertension, and atrial fibrillation for which he is taking an oral medication. He says that he recently started taking omeprazole for reflux. Which of the following processes is most likely inhibited in this patient?
- A. Sulfation
- B. Oxidation (Correct Answer)
- C. Filtration
- D. Acetylation
- E. Glucuronidation
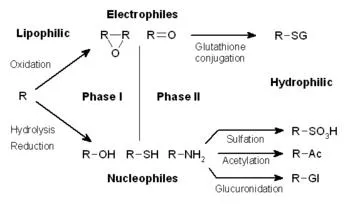
Phase II metabolism (conjugation reactions) Explanation: ***Oxidation***
- The patient is taking **omeprazole**, a proton pump inhibitor, which is a known **CYP450 inhibitor**.
- Since the patient is also on an **oral anticoagulant** for atrial fibrillation, inhibition of CYP450 enzymes can reduce the metabolism of the anticoagulant, leading to **increased anticoagulant effect** and subsequent bleeding and bruising.
*Sulfation*
- **Sulfation** is a phase II metabolic reaction that converts compounds into more polar and excretable forms, but omeprazole primarily affects phase I metabolism involving CYP450 enzymes.
- While sulfation can be important for the metabolism of some drugs, it is not the primary process inhibited by omeprazole to cause increased bleeding with oral anticoagulants.
*Filtration*
- **Filtration** is a renal process and not a metabolic enzyme pathway affected by omeprazole.
- Omeprazole's interaction with anticoagulants mainly occurs through hepatic metabolism, not renal filtration.
*Acetylation*
- **Acetylation** is a phase II metabolic reaction, primarily carried out by **N-acetyltransferases**.
- Omeprazole is primarily known to interact with **CYP450 enzymes** (phase I metabolism) rather than N-acetyltransferases.
*Glucuronidation*
- **Glucuronidation** is a phase II metabolic reaction involving **UGT enzymes** that typically inactivates and increases the excretion of drugs.
- While important for drug metabolism, omeprazole's primary drug interactions leading to increased anticoagulant effects are via **CYP450 inhibition** (phase I metabolism), not directly through glucuronidation.
Phase II metabolism (conjugation reactions) US Medical PG Question 2: You are seeing a patient in clinic who recently started treatment for active tuberculosis. The patient is currently being treated with rifampin, isoniazid, pyrazinamide, and ethambutol. The patient is not used to taking medicines and is very concerned about side effects. Specifically regarding the carbohydrate polymerization inhibiting medication, which of the following is a known side effect?
- A. Vision loss (Correct Answer)
- B. Paresthesias of the hands and feet
- C. Cutaneous flushing
- D. Arthralgias
- E. Elevated liver enzymes
Phase II metabolism (conjugation reactions) Explanation: ***Vision loss***
- The "carbohydrate polymerization inhibiting medication" refers to **ethambutol**, which inhibits **arabinosyl transferase** (involved in mycobacterial cell wall arabinogalactan synthesis)
- **Ethambutol** causes **optic neuritis**, leading to **decreased visual acuity**, **red-green color blindness**, and potentially **irreversible vision loss**
- **Regular ophthalmologic monitoring** is essential during ethambutol therapy
*Paresthesias of the hands and feet*
- This describes **peripheral neuropathy** caused by **isoniazid**
- Isoniazid interferes with **pyridoxine (vitamin B6) metabolism**, leading to neurotoxicity
- Risk factors include malnutrition, diabetes, alcoholism, and pregnancy
- Prevented by **pyridoxine supplementation**
*Cutaneous flushing*
- Not a characteristic side effect of first-line anti-tuberculosis medications
- More commonly associated with niacin or certain allergic/vasodilatory reactions
*Arthralgias*
- Classic side effect of **pyrazinamide**, often affecting small joints
- Caused by **pyrazinamide-induced hyperuricemia** (inhibits renal uric acid excretion)
- May require dose adjustment or discontinuation if severe
*Elevated liver enzymes*
- **Hepatotoxicity** can occur with **rifampin**, **isoniazid**, and **pyrazinamide**
- Requires regular monitoring of liver function tests during TB treatment
- Most common serious adverse effect of combination TB therapy
Phase II metabolism (conjugation reactions) US Medical PG Question 3: A 17-year-old girl is brought to the emergency department 6 hours after she attempted suicide by consuming 16 tablets of acetaminophen (500 mg per tablet). At present, she does not have any complaints or symptoms. The patient is afebrile and vital signs are within normal limits. Physical examination is unremarkable. Laboratory findings show a serum acetaminophen level that is predictive of ‘probable hepatic toxicity’ on the Rumack-Matthew nomogram. Treatment is started with a drug, which is a precursor of glutathione and is a specific antidote for acetaminophen poisoning. Which of the following is an additional beneficial mechanism of action of this drug in this patient?
- A. Promotes glucuronidation of unmetabolized acetaminophen
- B. Promotes microcirculatory blood flow (Correct Answer)
- C. Promotes fecal excretion of unabsorbed acetaminophen
- D. Prevents gastrointestinal absorption of acetaminophen
- E. Promotes oxidation of N-acetyl-p-benzoquinoneimine (NAPQI)
Phase II metabolism (conjugation reactions) Explanation: ***Promotes microcirculatory blood flow***
- **N-acetylcysteine** (NAC), the antidote for acetaminophen poisoning, acts as a **vasodilator** and **improves microcirculatory blood flow**, which can be beneficial in preventing and treating liver injury.
- This benefit is particularly relevant in cases of severe poisoning, where compromised hepatic perfusion can exacerbate damage.
*Promotes glucuronidation of unmetabolized acetaminophen*
- NAC primarily works by replenishing **glutathione stores**, which are crucial for detoxifying the toxic metabolite **NAPQI**, not by enhancing glucuronidation.
- Glucuronidation is a separate metabolic pathway that conjugates acetaminophen for excretion and is not directly augmented by NAC.
*Promotes fecal excretion of unabsorbed acetaminophen*
- NAC is given systemically (orally or intravenously) to counteract absorbed acetaminophen and does not directly promote fecal excretion of unabsorbed drug.
- Activated charcoal is used to prevent absorption if given shortly after ingestion.
*Prevents gastrointestinal absorption of acetaminophen*
- NAC does not prevent the **Gastrointestinal absorption** of acetaminophen; it is administered after absorption has occurred and the drug is circulating in the body.
- Measures like activated charcoal or gastric lavage are used to prevent absorption if the patient presents early enough.
*Promotes oxidation of N-acetyl-p-benzoquinoneimine (NAPQI)*
- NAC works by **reducing** the toxic metabolite **NAPQI** back to acetaminophen and by replenishing **glutathione**, which then detoxifies NAPQI.
- It does not promote the *oxidation* of NAPQI; rather, it facilitates its *reduction* or conjugation to render it harmless.
Phase II metabolism (conjugation reactions) US Medical PG Question 4: A 46-year-old man comes to the physician for a follow-up examination. Two weeks ago, he underwent laparoscopic herniorrhaphy for an indirect inguinal hernia. During the procedure, a black liver was noted. He has a history of intermittent scleral icterus that resolved without treatment. Serum studies show:
Aspartate aminotransferase 30 IU/L
Alanine aminotransferase 35 IU/L
Alkaline phosphatase 47 mg/dL
Total bilirubin 1.7 mg/dL
Direct bilirubin 1.1 mg/dL
Which of the following is the most likely diagnosis?
- A. Gilbert syndrome
- B. Dubin-Johnson syndrome (Correct Answer)
- C. Type II Crigler-Najjar syndrome
- D. Type I Crigler-Najjar syndrome
- E. Rotor syndrome
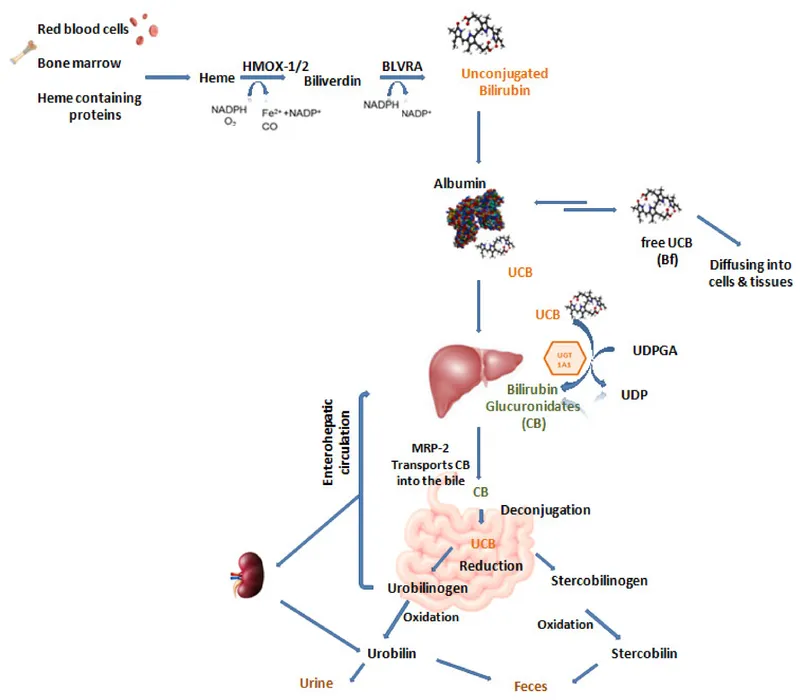
Phase II metabolism (conjugation reactions) Explanation: ***Dubin-Johnson syndrome***
- The presence of a **black liver** during surgery is pathognomonic for Dubin-Johnson syndrome, due to the accumulation of **melanin-like pigment** from impaired hepatocyte excretion.
- This syndrome is characterized by **intermittent conjugated hyperbilirubinemia** (direct bilirubin 1.1 mg/dL, total bilirubin 1.7 mg/dL) and **normal liver enzymes**, consistent with the patient's presentation of scleral icterus that resolved spontaneously.
*Gilbert syndrome*
- Gilbert syndrome is characterized by **unconjugated hyperbilirubinemia** due to reduced UDP-glucuronosyltransferase activity, while this patient has elevated direct bilirubin.
- It does **not cause a black liver**, nor does it typically present with such a significant elevation in direct bilirubin.
*Type II Crigler-Najjar syndrome*
- This syndrome involves **unconjugated hyperbilirubinemia** (due to a defect in UDP-glucuronosyltransferase) and would not present with a black liver.
- While less severe than Type I, it still primarily affects **unconjugated bilirubin metabolism**.
*Type I Crigler-Najjar syndrome*
- This is a severe form of **unconjugated hyperbilirubinemia**, often leading to **kernicterus** in infancy, and is not consistent with an adult presenting with intermittent mild icterus and normal liver enzymes.
- It is not associated with a **black liver**.
*Rotor syndrome*
- Rotor syndrome also causes **conjugated hyperbilirubinemia** with normal liver enzymes but is distinguished from Dubin-Johnson by the **absence of a black liver**.
- It is usually less severe than Dubin-Johnson and has a slightly different pattern of urinary coproporphyrin excretion.
Phase II metabolism (conjugation reactions) US Medical PG Question 5: A 25-year-old woman presents with slightly yellow discoloration of her skin and eyes. She says she has had multiple episodes with similar symptoms before. She denies any recent history of nausea, fatigue, fever, or change in bowel/bladder habits. No significant past medical history. The patient is afebrile and vital signs are within normal limits. On physical examination, she is jaundiced, and her sclera is icteric. Laboratory findings are significant only for a mild unconjugated hyperbilirubinemia. The remainder of laboratory results is unremarkable. Which of the following is the most likely diagnosis in this patient?
- A. Crigler-Najjar syndrome type II
- B. Crigler-Najjar syndrome type I
- C. Gilbert syndrome (Correct Answer)
- D. Hemolytic anemia
- E. Physiological jaundice
Phase II metabolism (conjugation reactions) Explanation: ***Gilbert syndrome***
- This syndrome is characterized by **mild, intermittent unconjugated hyperbilirubinemia**, often triggered by stress, fasting, or illness, and typically **without other symptoms** or signs of liver disease.
- The patient's presentation with recurrent jaundice, absence of other symptoms, and normal liver function tests except for unconjugated hyperbilirubinemia are classic for **Gilbert syndrome**.
*Crigler-Najjar syndrome type II*
- While also involving unconjugated hyperbilirubinemia, **Crigler-Najjar type II** typically presents with more severe and persistent jaundice with higher bilirubin levels than seen in Gilbert syndrome.
- This condition is rare and often requires intervention with **phenobarbital** to induce UGT1A1 activity, which is not indicated by the mild presentation here.
*Crigler-Najjar syndrome type I*
- This is a very severe and rare condition characterized by a **complete absence or near-complete absence of UGT1A1 activity**, leading to extremely high levels of unconjugated bilirubin from birth.
- Patients typically develop **kernicterus** and often die in infancy or early childhood without aggressive treatment, which is inconsistent with the patient's age and mild symptoms.
*Hemolytic anemia*
- **Hemolytic anemia** causes unconjugated hyperbilirubinemia due to the breakdown of red blood cells, but it would also present with other signs such as **anemia**, **reticulocytosis**, and potentially splenomegaly, which are not mentioned.
- The patient's laboratory results are otherwise unremarkable, ruling out red blood cell destruction as the primary cause.
*Physiological jaundice*
- **Physiological jaundice** is a common and transient condition in **newborns** due to immature liver function and increased red blood cell turnover.
- It resolves within the first few weeks of life and is not applicable to a 25-year-old woman with recurrent episodes.
Phase II metabolism (conjugation reactions) US Medical PG Question 6: A 65-year-old man comes to the physician for a routine health maintenance examination. He feels well. His most recent examination 2 years ago included purified protein derivative (PPD) skin testing and showed no abnormalities. He is a retired physician and recently came back from rural China where he completed a voluntary service at a local healthcare center. A PPD skin test is performed. Three days later, an induration of 12 mm is noted. An x-ray of the chest shows no abnormalities. He is started on a drug that inhibits the synthesis of mycolic acid. This patient is at greatest risk of developing which of the following adverse effects?
- A. Cytochrome P-450 induction
- B. Hyperuricemia
- C. Liver injury (Correct Answer)
- D. Optic neuropathy
- E. Nephrotoxicity
Phase II metabolism (conjugation reactions) Explanation: ***Liver injury***
- The drug described is **isoniazid**, which inhibits **mycolic acid synthesis** and is first-line treatment for **latent tuberculosis infection**.
- **Isoniazid-induced hepatotoxicity** is the most significant adverse effect, with risk increasing dramatically in patients **>35 years old** (this patient is 65).
- Additional risk factors include alcohol use, pre-existing liver disease, and concurrent hepatotoxic medications.
- Patients should be monitored with baseline and periodic liver function tests.
*Cytochrome P-450 induction*
- **Rifampin**, not isoniazid, is a potent **CYP450 inducer** that decreases levels of many co-administered drugs.
- Isoniazid is actually a **CYP450 inhibitor** (inhibits CYP2C19, CYP3A4), which can increase levels of other drugs like phenytoin and warfarin.
*Hyperuricemia*
- **Pyrazinamide** is the anti-tuberculosis drug that causes **hyperuricemia** by inhibiting renal tubular secretion of uric acid.
- This can precipitate acute gout attacks in susceptible patients.
- Isoniazid does not affect uric acid metabolism.
*Optic neuropathy*
- **Ethambutol** causes dose-dependent **optic neuropathy**, presenting with decreased visual acuity and **red-green color blindness**.
- Patients on ethambutol require baseline and monthly visual assessments.
- Isoniazid is not associated with optic toxicity.
*Nephrotoxicity*
- **Aminoglycosides** (e.g., streptomycin) and some other antibiotics cause **nephrotoxicity** through tubular damage.
- Isoniazid is not significantly nephrotoxic and does not require renal dose adjustment.
Phase II metabolism (conjugation reactions) US Medical PG Question 7: A 35-year-old woman presents to the emergency department after ingesting approximately 50 tablets of acetaminophen 4 hours ago in a suicide attempt. Her acetaminophen level is 200 µg/mL. Which of the following best describes the mechanism of toxicity in this case?
- A. Depletion of glutathione stores (Correct Answer)
- B. Blockade of calcium channels
- C. Direct cellular necrosis
- D. Inhibition of cytochrome oxidase
Phase II metabolism (conjugation reactions) Explanation: ***Depletion of glutathione stores***
- In acetaminophen overdose, the normal metabolic pathways become saturated, leading to the accumulation of a toxic metabolite called **N-acetyl-p-benzoquinone imine (NAPQI)**.
- **NAPQI** is normally detoxified by conjugation with **glutathione**, but in overdose, glutathione stores are depleted, allowing NAPQI to bind covalently to hepatocyte macromolecules, causing damage.
*Blockade of calcium channels*
- This mechanism is characteristic of **calcium channel blocker toxicity**, leading to cardiovascular depression (bradycardia, hypotension) and is not relevant to acetaminophen overdose.
- Acetaminophen toxicity primarily affects the liver via a different pathway, not directly interfering with calcium channels.
*Direct cellular necrosis*
- While acetaminophen overdose ultimately leads to **hepatocellular necrosis**, this is the *result* of the toxicity, not the primary mechanism by which the drug initiates cellular damage.
- The necrosis is mediated by the accumulation of the toxic metabolite **NAPQI** and the subsequent oxidative stress and cellular injury, not by direct cellular destruction without prior steps.
*Inhibition of cytochrome oxidase*
- This mechanism is associated with toxins like **cyanide** and **carbon monoxide**, which impair mitochondrial respiration and cellular energy production.
- Acetaminophen toxicity does not directly involve the inhibition of cytochrome oxidase as its primary mechanism of hepatotoxicity.
Phase II metabolism (conjugation reactions) US Medical PG Question 8: A 26-year-old man comes to the emergency department because of a 1-week history of worsening fatigue, nausea, and vomiting. Six weeks ago, he was diagnosed with latent tuberculosis and appropriate low-dose pharmacotherapy was initiated. Physical examination shows right upper quadrant tenderness and scleral icterus. Laboratory studies show elevated aminotransferases. Impaired function of which of the following pharmacokinetic processes is the most likely explanation for this patient's symptoms?
- A. Acetylation (Correct Answer)
- B. Glucuronidation
- C. Hydrolysis
- D. Sulfation
- E. Reduction
Phase II metabolism (conjugation reactions) Explanation: ***Acetylation***
- This patient is exhibiting symptoms of **hepatotoxicity** (fatigue, nausea, vomiting, RUQ tenderness, scleral icterus, elevated aminotransferases) after starting low-dose pharmacotherapy for latent tuberculosis. The most common drug used for latent TB is **isoniazid**, which is primarily metabolized by **N-acetylation**.
- Impaired acetylation, particularly in **slow acetylators**, can lead to higher plasma concentrations of isoniazid and its toxic metabolites, increasing the risk of **drug-induced liver injury**.
*Glucuronidation*
- **Glucuronidation** is a Phase II metabolic pathway that conjugates drugs with **glucuronic acid** to increase water solubility and facilitate excretion.
- While important for the metabolism of many drugs and endogenous substances (e.g., bilirubin), it is not the primary mechanism of metabolism or the main pathway implicated in the hepatotoxicity of **isoniazid**.
*Hydrolysis*
- **Hydrolysis** is a chemical reaction in which water is used to break down a compound, often involving ester or amide bonds.
- This process is not the primary metabolic pathway for **isoniazid**, nor is impaired hydrolysis a common cause of its hepatotoxicity.
*Sulfation*
- **Sulfation** is a Phase II metabolic reaction that conjugates drugs with a **sulfate group**, typically for detoxification and excretion.
- While various drugs undergo sulfation, it is not the dominant metabolic pathway for **isoniazid**, and impaired sulfation is not typically associated with isoniazid-induced hepatotoxicity.
*Reduction*
- **Reduction** reactions involve the gain of electrons or hydrogen atoms, or the loss of oxygen, and are part of drug metabolism for certain compounds.
- However, reduction is not the primary clearance mechanism for **isoniazid**, and abnormal reduction is not commonly implicated in its hepatotoxic effects.
Phase II metabolism (conjugation reactions) US Medical PG Question 9: An 18-month-old boy is brought in to the pediatrician by his mother for concerns that her child is becoming more and more yellow over the past two days. She additionally states that the boy has been getting over a stomach flu and has not been able to keep down any food. The boy does not have a history of neonatal jaundice. On exam, the patient appears slightly sluggish and jaundiced with icteric sclera. His temperature is 99.0°F (37.2°C), blood pressure is 88/56 mmHg, pulse is 110/min, and respirations are 22/min. His labs demonstrate an unconjugated hyperbilirubinemia of 16 mg/dL. It is determined that the best course of treatment for this patient is phenobarbital to increase liver enzyme synthesis. Which of the following best describes the molecular defect in this patient?
- A. Silent mutation in the UGT1A1 gene
- B. Nonsense mutation in the UGT1A1 gene
- C. Deletion in the SLCO1B1 gene
- D. Mutation in the promoter region of the UGT1A1 gene
- E. Missense mutation in the UGT1A1 gene (Correct Answer)
Phase II metabolism (conjugation reactions) Explanation: ***Missense mutation in the UGT1A1 gene***
- The presentation of **unconjugated hyperbilirubinemia** (16 mg/dL) with jaundice and sluggishness, triggered by a **stressor** (gastroenteritis, fasting) in an 18-month-old child, is characteristic of **Crigler-Najjar syndrome Type 2**.
- Crigler-Najjar Type 2 is caused by **missense mutations** in the coding region of the *UGT1A1* gene, resulting in a UGT1A1 enzyme with **reduced but present activity** (typically 10-30% of normal).
- **Phenobarbital treatment is effective** in Type 2 because it induces CYP enzyme expression and enhances the activity of the partially functional UGT1A1 enzyme, increasing bilirubin conjugation capacity.
- The severity (bilirubin 16 mg/dL with symptoms) distinguishes this from Gilbert syndrome, while the phenobarbital response distinguishes it from Type 1.
*Silent mutation in the UGT1A1 gene*
- A **silent mutation** does not alter the amino acid sequence and therefore would **not cause any functional deficit** in the UGT1A1 enzyme.
- This would not result in unconjugated hyperbilirubinemia or any clinical manifestations.
*Nonsense mutation in the UGT1A1 gene*
- A **nonsense mutation** creates a premature stop codon, resulting in a **truncated, non-functional protein** and complete or near-complete absence of UGT1A1 activity.
- This causes **Crigler-Najjar syndrome Type 1**, which presents in the **neonatal period** with severe jaundice (bilirubin often >20 mg/dL), high risk of kernicterus, and is **unresponsive to phenobarbital**.
- The patient's milder presentation, later onset, and response to phenobarbital rule out Type 1.
*Deletion in the SLCO1B1 gene*
- The **SLCO1B1 gene** encodes the **OATP1B1 transporter**, involved in hepatic uptake of conjugated bilirubin and other organic anions.
- Defects are associated with **Rotor syndrome**, which causes **conjugated hyperbilirubinemia**, not unconjugated hyperbilirubinemia.
- This does not match the patient's laboratory findings.
*Mutation in the promoter region of the UGT1A1 gene*
- **Promoter mutations** (specifically TA repeat polymorphism in the TATA box) cause **Gilbert syndrome**, resulting in mildly reduced UGT1A1 expression (~30% activity).
- Gilbert syndrome typically presents with **mild, intermittent jaundice** with bilirubin usually **1-5 mg/dL**, often asymptomatic, and does not routinely require treatment.
- The **severe hyperbilirubinemia (16 mg/dL)** with significant symptoms and need for phenobarbital treatment is inconsistent with Gilbert syndrome and indicates Crigler-Najjar Type 2 instead.
Phase II metabolism (conjugation reactions) US Medical PG Question 10: A 57-year-old man comes to the physician because of sudden-onset fever, malaise, and pain and swelling of his wrists and ankles that began a week ago. One month ago, he was started on hydralazine for adjunctive treatment of hypertension. His temperature is 37.8°C (100°F). Examination shows swelling, tenderness, warmth, and erythema of both wrists and ankles; range of motion is limited. Further evaluation is most likely to show an increased level of which of the following autoantibodies?
- A. Anti-Jo-1
- B. Anti-dsDNA
- C. Anti-β2-glycoprotein
- D. Anti-histone (Correct Answer)
- E. Anti-Smith
Phase II metabolism (conjugation reactions) Explanation: ***Anti-histone***
- The patient's presentation with **fever, malaise, polyarthritis**, and recent initiation of **hydralazine** strongly suggests **drug-induced lupus erythematosus (DILE)**.
- **Anti-histone antibodies** are the most common and characteristic autoantibody found in over 95% of cases of DILE.
*Anti-Jo-1*
- **Anti-Jo-1 antibodies** are positive in a subset of patients with **polymyositis** and **dermatomyositis**, often associated with interstitial lung disease and "mechanic's hands."
- These conditions typically involve **proximal muscle weakness** rather than predominantly joint pain and swelling as seen here.
*Anti-dsDNA*
- **Anti-dsDNA antibodies** are highly specific for **systemic lupus erythematosus (SLE)**, but are rarely positive in drug-induced lupus erythematosus (DILE).
- While DILE shares some features with SLE, the presence of these antibodies would favor a diagnosis of idiopathic SLE.
*Anti-β2-glycoprotein*
- **Anti-β2-glycoprotein antibodies** are associated with **antiphospholipid syndrome (APS)**, which presents with arterial or venous thrombosis and recurrent pregnancy loss.
- The patient's symptoms are primarily inflammatory arthritis, not thrombotic events.
*Anti-Smith*
- **Anti-Smith antibodies** are highly specific for **systemic lupus erythematosus (SLE)** and are rarely positive in drug-induced lupus erythematosus (DILE).
- Although highly specific for SLE, they are present in a minority of SLE patients (20-30%) and are not characteristic of DILE.
More Phase II metabolism (conjugation reactions) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.