Half-life and steady state concepts US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Half-life and steady state concepts. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Half-life and steady state concepts US Medical PG Question 1: A 35-year-old woman is started on a new experimental intravenous drug X. In order to make sure that she is able to take this drug safely, the physician in charge of her care calculates the appropriate doses to give to this patient. Data on the properties of drug X from a subject with a similar body composition to the patient is provided below:
Weight: 100 kg
Dose provided: 1500 mg
Serum concentration 15 mg/dL
Bioavailability: 1
If the patient has a weight of 60 kg and the target serum concentration is 10 mg/dL, which of the following best represents the loading dose of drug X that should be given to this patient?
- A. 300 mg
- B. 450 mg
- C. 150 mg
- D. 1000 mg
- E. 600 mg (Correct Answer)
Half-life and steady state concepts Explanation: ***600 mg***
- First, calculate the **volume of distribution (Vd)** using the provided data: **Vd = Total Dose / Serum Concentration**. Converting units: 15 mg/dL = 150 mg/L. Therefore, Vd = 1500 mg / 150 mg/L = **10 L** (for the 100 kg subject).
- Since the Vd value is for a 100 kg person, Vd per kg = 10 L / 100 kg = **0.1 L/kg**. For the 60 kg patient, the Vd = 0.1 L/kg × 60 kg = **6 L**.
- The **loading dose = Target Serum Concentration × Vd / Bioavailability**. Converting target concentration: 10 mg/dL = 100 mg/L. Therefore: (100 mg/L × 6 L) / 1 = **600 mg**.
*300 mg*
- This value is obtained if an incorrect **Vd** or target concentration was used, potentially through miscalculation or incorrect unit conversion.
- For instance, if the **Vd** was inaccurately calculated at 3 L (instead of 6 L), this could lead to the incorrect answer.
*450 mg*
- This result might occur if the **Vd calculation** was flawed or if the target concentration was incorrectly interpreted.
- A potential error could involve using a Vd of 4.5 L which would result in 450 mg, or if the drug amount was simply prorated by weight without properly considering the Vd per kg.
*150 mg*
- This value suggests a significant error in the calculation of the **volume of distribution** or the target concentration.
- It might be obtained if the **Vd** was mistakenly taken as 1.5 L or if the dose was divided by the original serum concentration without accounting for the new patient's weight and desired concentration.
*1000 mg*
- This value is significantly higher than the correct answer, indicating an overestimation of the **Vd** or target concentration.
- It could result from using the original dose (1500 mg) and attempting to scale it incorrectly by weight alone (1500 mg × 60/100 = 900 mg, close to 1000), or if unit conversions were mishandled during the Vd determination.
Half-life and steady state concepts US Medical PG Question 2: A scientist is studying the excretion of a novel toxin X by the kidney in order to understand the dynamics of this new substance. He discovers that this new toxin X has a clearance that is half that of inulin in a particular patient. This patient's filtration fraction is 20% and his para-aminohippuric acid (PAH) dynamics are as follows:
Urine volume: 100 mL/min
Urine PAH concentration: 30 mg/mL
Plasma PAH concentration: 5 mg/mL
Given these findings, what is the clearance of the novel toxin X?
- A. 1,500 mL/min
- B. 600 mL/min
- C. 300 mL/min
- D. 60 mL/min (Correct Answer)
- E. 120 mL/min
Half-life and steady state concepts Explanation: ***60 ml/min***
- First, calculate the **renal plasma flow (RPF)** using PAH clearance: RPF = (Urine PAH conc. × Urine vol.) / Plasma PAH conc. = (30 mg/mL × 100 mL/min) / 5 mg/mL = 600 mL/min.
- Next, calculate the **glomerular filtration rate (GFR)**, which is the clearance of inulin. GFR = RPF × Filtration Fraction = 600 mL/min × 0.20 = 120 mL/min. Toxin X clearance is half of inulin clearance, so 120 mL/min / 2 = **60 mL/min**.
*1,500 ml/min*
- This value is likely obtained if an incorrect formula or conversion was made, possibly by misinterpreting the units or the relationship between GFR, RPF, and filtration fraction.
- It significantly overestimates the clearance for a substance that is cleared at half the rate of inulin.
*600 ml/min*
- This value represents the **renal plasma flow (RPF)**, calculated using the PAH clearance data.
- It does not account for the filtration fraction or the fact that toxin X clearance is half of inulin clearance (GFR).
*300 ml/min*
- This value would be obtained if the renal plasma flow (RPF) was incorrectly halved, or if an intermediate calculation was misinterpreted as the final answer.
- It does not align with the given filtration fraction and the relationship between toxin X and inulin clearance.
*120 ml/min*
- This value represents the **glomerular filtration rate (GFR)**, which is equal to the clearance of inulin (RPF × Filtration Fraction = 600 mL/min × 0.20 = 120 mL/min).
- The question states that the clearance of toxin X is **half** that of inulin, so this is an intermediate step, not the final answer.
Half-life and steady state concepts US Medical PG Question 3: An investigator is studying the effect of antihypertensive drugs on cardiac output and renal blood flow. For comparison, a healthy volunteer is given a placebo and a continuous infusion of para-aminohippuric acid (PAH) to achieve a plasma concentration of 0.02 mg/ml. His urinary flow rate is 1.5 ml/min and the urinary concentration of PAH is measured to be 8 mg/ml. His hematocrit is 50%. Which of the following values best estimates cardiac output in this volunteer?
- A. 8 L/min
- B. 3 L/min
- C. 4 L/min
- D. 1.2 L/min
- E. 6 L/min (Correct Answer)
Half-life and steady state concepts Explanation: ***6 L/min***
- This value represents the estimated **cardiac output** based on the calculated renal blood flow.
- Step 1: Calculate renal plasma flow (RPF) using PAH clearance: RPF = (Urinary PAH × Urine flow rate) / Plasma PAH = (8 mg/ml × 1.5 ml/min) / 0.02 mg/ml = 600 ml/min = 0.6 L/min
- Step 2: Calculate renal blood flow (RBF): Since hematocrit is 50%, RBF = RPF / (1 - Hematocrit) = 0.6 / 0.5 = 1.2 L/min
- Step 3: Estimate cardiac output: The kidneys normally receive approximately **20-25% of cardiac output**. Using 20%: Cardiac Output = RBF / 0.20 = 1.2 / 0.20 = **6 L/min**
- This is consistent with normal resting cardiac output in a healthy adult.
*8 L/min*
- This value overestimates cardiac output based on the renal blood flow calculation.
- While some individuals may have higher cardiac output during exercise, the calculated RBF of 1.2 L/min suggests a resting cardiac output closer to 6 L/min.
*3 L/min*
- This value significantly underestimates cardiac output.
- If cardiac output were 3 L/min, the kidneys would be receiving 40% of cardiac output (1.2/3), which is physiologically implausible at rest.
*4 L/min*
- This value underestimates cardiac output based on the renal data.
- This would mean kidneys receive 30% of cardiac output (1.2/4), which is higher than the typical 20-25%.
*1.2 L/min*
- This is the calculated **renal blood flow**, not cardiac output.
- While this calculation is correct for RBF, the question specifically asks for cardiac output estimation, which requires accounting for the fact that kidneys receive only about 20-25% of total cardiac output.
Half-life and steady state concepts US Medical PG Question 4: A 70-year-old female with chronic kidney failure secondary to diabetes asks her nephrologist to educate her about the techniques used to evaluate the degree of kidney failure progression. She learns about the concept of glomerular filtration rate (GFR) and learns that it can be estimated by measuring the levels of some substances. The clearance of which of the following substances is the most accurate estimate for GFR?
- A. Paraaminohippurate (PAH)
- B. Sodium
- C. Inulin (Correct Answer)
- D. Creatinine
- E. Glucose
Half-life and steady state concepts Explanation: ***Inulin***
- **Inulin** is freely filtered by the glomeruli and is neither reabsorbed nor secreted by the renal tubules, making its clearance the **gold standard** for accurately measuring GFR.
- Due to its ideal physiological properties, inulin clearance perfectly reflects the rate at which plasma is filtered by the kidneys.
*Paraaminohippurate (PAH)*
- **PAH** is almost completely cleared from the blood by both glomerular filtration and **tubular secretion**, making its clearance an accurate measure of **renal plasma flow (RPF)**, not GFR.
- While important for assessing renal blood flow, it does not directly reflect the filtration capacity of the glomeruli.
*Sodium*
- **Sodium** is freely filtered at the glomerulus, but a significant portion (approximately **99%**) is **reabsorbed** by the renal tubules.
- Its clearance is highly variable and depends on various physiological factors, making it unsuitable for GFR estimation.
*Creatinine*
- **Creatinine** is freely filtered by the glomeruli and is also **modestly secreted** by the renal tubules, leading to an **overestimation of GFR** at lower kidney function levels.
- Despite being the most commonly used clinical marker due to its endogenous production, its tubular secretion makes it less accurate than inulin.
*Glucose*
- **Glucose** is freely filtered by the glomeruli but is almost **completely reabsorbed** by the renal tubules under normal physiological conditions.
- Its presence in urine (glycosuria) indicates a high plasma glucose level or tubular reabsorption defects, not a measure of GFR.
Half-life and steady state concepts US Medical PG Question 5: You are currently employed as a clinical researcher working on clinical trials of a new drug to be used for the treatment of Parkinson's disease. Currently, you have already determined the safe clinical dose of the drug in a healthy patient. You are in the phase of drug development where the drug is studied in patients with the target disease to determine its efficacy. Which of the following phases is this new drug currently in?
- A. Phase 4
- B. Phase 1
- C. Phase 2 (Correct Answer)
- D. Phase 0
- E. Phase 3
Half-life and steady state concepts Explanation: ***Phase 2***
- **Phase 2 trials** involve studying the drug in patients with the target disease to assess its **efficacy** and further evaluate safety, typically involving a few hundred patients.
- The question describes a stage after safe dosing in healthy patients (Phase 1) and before large-scale efficacy confirmation (Phase 3), focusing on efficacy in the target population.
*Phase 4*
- **Phase 4 trials** occur **after a drug has been approved** and marketed, monitoring long-term effects, optimal use, and rare side effects in a diverse patient population.
- This phase is conducted post-market approval, whereas the question describes a drug still in development prior to approval.
*Phase 1*
- **Phase 1 trials** primarily focus on determining the **safety and dosage** of a new drug in a **small group of healthy volunteers** (or sometimes patients with advanced disease if the drug is highly toxic).
- The question states that the safe clinical dose in a healthy patient has already been determined, indicating that Phase 1 has been completed.
*Phase 0*
- **Phase 0 trials** are exploratory, very early-stage studies designed to confirm that the drug reaches the target and acts as intended, typically involving a very small number of doses and participants.
- These trials are conducted much earlier in the development process, preceding the determination of safe clinical doses and large-scale efficacy studies.
*Phase 3*
- **Phase 3 trials** are large-scale studies involving hundreds to thousands of patients to confirm **efficacy**, monitor side effects, compare it to commonly used treatments, and collect information that will allow the drug to be used safely.
- While Phase 3 does assess efficacy, it follows Phase 2 and is typically conducted on a much larger scale before submitting for regulatory approval.
Half-life and steady state concepts US Medical PG Question 6: A researcher is investigating the effects of a new antihypertensive medication on renal physiology. She gives a subject a dose of the new medication, and she then collects plasma and urine samples. She finds the following: Hematocrit: 40%; Serum creatinine: 0.0125 mg/mL; Urine creatinine: 1.25 mg/mL. Urinary output is 1 mL/min. Renal blood flow is 1 L/min. Based on the above information and approximating that the creatinine clearance is equal to the GFR, what answer best approximates filtration fraction in this case?
- A. 10%
- B. 17% (Correct Answer)
- C. 33%
- D. 50%
- E. 25%
Half-life and steady state concepts Explanation: ***17%***
- First, calculate **GFR** using the creatinine clearance formula: GFR = (Urine creatinine × Urinary output) / Serum creatinine = (1.25 mg/mL × 1 mL/min) / 0.0125 mg/mL = **100 mL/min**.
- Next, calculate **Renal Plasma Flow (RPF)** from Renal Blood Flow (RBF) and Hematocrit: RPF = RBF × (1 - Hematocrit) = 1000 mL/min × (1 - 0.40) = **600 mL/min**.
- Finally, calculate **Filtration Fraction (FF)** = GFR / RPF = 100 mL/min / 600 mL/min = 0.1667 = **16.7%, which approximates to 17%**.
- This is the correct answer based on the physiological calculations and represents a normal filtration fraction.
*10%*
- This would correspond to a filtration fraction of 0.10, which would require either a GFR of 60 mL/min (lower than calculated) or an RPF of 1000 mL/min (higher than calculated).
- This value is too low given the provided parameters and doesn't match the calculation from the given data.
*25%*
- This value would suggest FF = 0.25, requiring a GFR of 150 mL/min with the calculated RPF of 600 mL/min.
- This is higher than the calculated GFR of 100 mL/min and doesn't match the given creatinine values.
*33%*
- This would imply FF = 0.33, requiring a GFR of approximately 200 mL/min with RPF of 600 mL/min.
- This is significantly higher than the calculated GFR and would represent an abnormally elevated filtration fraction.
*50%*
- A filtration fraction of 50% is unphysiologically high and would indicate severe pathology.
- This would require a GFR of 300 mL/min with the calculated RPF, which is impossible given the provided creatinine clearance data.
Half-life and steady state concepts US Medical PG Question 7: A researcher is investigating the behavior of two novel chemotherapeutic drugs that he believes will be effective against certain forms of lymphoma. In order to evaluate the safety of these drugs, this researcher measures the concentration and rate of elimination of each drug over time. A partial set of the results is provided below.
Time 1:
Concentration of Drug A: 4 mg/dl
Concentration of Drug B: 3 mg/dl
Elimination of Drug A: 1 mg/minute
Elimination of Drug B: 4 mg/minute
Time 2:
Concentration of Drug A: 2 mg/dl
Concentration of Drug B: 15 mg/dl
Elimination of Drug A: 0.5 mg/minute
Elimination of Drug B: 4 mg/minute
Which of the following statements correctly identifies the most likely relationship between the half-life of these two drugs?
- A. The half-life of drug A is always longer than that of drug B
- B. The half-life of both drug A and drug B are constant
- C. The half-life of both drug A and drug B are variable
- D. The half-life of drug A is variable but that of drug B is constant
- E. The half-life of drug A is constant but that of drug B is variable (Correct Answer)
Half-life and steady state concepts Explanation: ***The half-life of drug A is constant but that of drug B is variable***
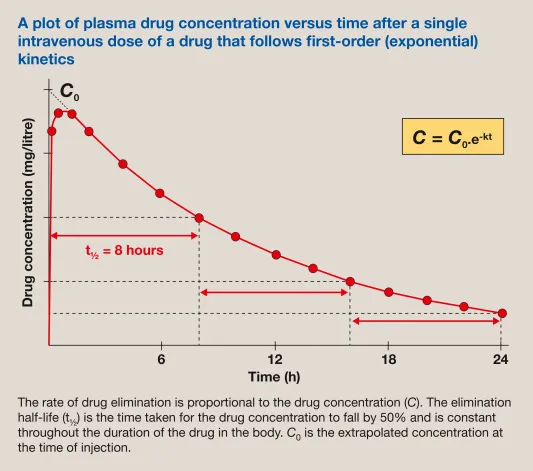
- Drug A shows a **constant fraction** eliminated per unit time (1 mg/minute from 4 mg/dl, then 0.5 mg/minute from 2 mg/dl), indicating **first-order kinetics** and thus a constant half-life.
- Drug B's elimination rate remains constant (4 mg/minute) despite varying concentrations (3 mg/dl then 15 mg/dl), which suggests **zero-order kinetics** and a variable half-life dependent on concentration.
*The half-life of drug A is always longer than that of drug B*
- This statement is incorrect because Drug B exhibits **zero-order kinetics**, meaning its **half-life changes** with concentration, making a constant comparison invalid.
- At very high concentrations, Drug B's half-life could actually be longer than Drug A's if the elimination rate is slow relative to the large amount of drug.
*The half-life of both drug A and drug B are constant*
- This is incorrect because Drug B demonstrates **zero-order kinetics**, where the elimination rate is constant, but the **half-life is variable** and directly depends on the drug concentration.
- For zero-order kinetics, a constant amount of drug is eliminated per unit time, not a constant fraction, which causes the half-life to change.
*The half-life of both drug A and drug B are variable*
- This is incorrect because Drug A exhibits **first-order kinetics**, where a **constant proportion** of the drug is eliminated per unit time, resulting in a **constant half-life**.
- Its elimination rate is directly proportional to its concentration (1 mg/min from 4 mg/dl, 0.5 mg/min from 2 mg/dl), which defines first-order kinetics.
*The half-life of drug A is variable but that of drug B is constant*
- This statement is the opposite of what the data indicates for Drug A; Drug A's elimination is **proportional to its concentration**, signifying **first-order kinetics** and a constant half-life.
- Drug B's elimination rate is constant regardless of concentration, which points to **zero-order kinetics** and thus a variable half-life.
Half-life and steady state concepts US Medical PG Question 8: An experimental infusable drug, X729, is currently being studied to determine its pharmacokinetics. The drug was found to have a half life of 1.5 hours and is eliminated by first order kinetics. What is the minimum number of hours required to reach a steady state concentration of >90%?
- A. 6 (Correct Answer)
- B. 3
- C. 7.5
- D. 1.5
- E. 4.5
Half-life and steady state concepts Explanation: ***6***
- For a drug eliminated by **first-order kinetics**, approximately **4 to 5 half-lives** are required to reach **steady-state concentration**.
- To reach >90% of steady-state, at least **4 half-lives** are needed, where **93.75%** of the steady state is achieved.
- The time taken would be **4 half-lives × 1.5 hours/half-life = 6 hours**, making this the **minimum time** to exceed 90%.
*3*
- This represents only **2 half-lives** (2 × 1.5 hours = 3 hours), which would achieve roughly **75%** of the steady-state concentration.
- This is insufficient to reach >90% of the steady-state concentration.
*7.5*
- This time point represents **5 half-lives** (5 × 1.5 hours = 7.5 hours), which would achieve approximately **97%** of the steady-state concentration.
- While this does exceed 90%, the question asks for the **minimum** number of hours required, and 90% is already exceeded at 6 hours (4 half-lives).
*1.5*
- This is only **1 half-life**, which would achieve approximately **50%** of the steady-state concentration.
- This is far too early to reach a >90% steady-state concentration.
*4.5*
- This represents **3 half-lives** (3 × 1.5 hours = 4.5 hours), achieving approximately **87.5%** of the steady-state concentration.
- While close to 90%, it does not quite reach "greater than 90%".
Half-life and steady state concepts US Medical PG Question 9: A patient is receiving daily administrations of Compound X. Compound X is freely filtered in the glomeruli and undergoes net secretion in the renal tubules. The majority of this tubular secretion occurs in the proximal tubule. Additional information regarding this patient's renal function and the renal processing of Compound X is included below:
Inulin clearance: 120 mL/min
Plasma concentration of Inulin: 1 mg/mL
PAH clearance: 600 mL/min
Plasma concentration of PAH: 0.2 mg/mL
Total Tubular Secretion of Compound X: 60 mg/min
Net Renal Excretion of Compound X: 300 mg/min
Which of the following is the best estimate of the plasma concentration of Compound X in this patient?
- A. 2 mg/mL (Correct Answer)
- B. 3 mg/mL
- C. There is insufficient information available to estimate the plasma concentration of Compound X
- D. 1 mg/mL
- E. 0.5 mg/mL
Half-life and steady state concepts Explanation: ***2 mg/mL***
* The **net renal excretion of Compound X (300 mg/min)** is the sum of the filtered load and the net tubular secretion.
* Given that Compound X is **freely filtered** and undergoes **net secretion (60 mg/min)**, we can calculate the filtered load and subsequently its plasma concentration.
* **Net excretion = Filtered load + Net tubular secretion**
* **300 mg/min = Filtered load + 60 mg/min**
* **Filtered load = 300 mg/min - 60 mg/min = 240 mg/min**
* Since **Filtered load = Glomerular Filtration Rate (GFR) * Plasma concentration (P_X)**, and GFR is estimated by **inulin clearance (120 mL/min)**:
* **240 mg/min = 120 mL/min * P_X**
* **P_X = 240 mg/min / 120 mL/min = 2 mg/mL**.
*3 mg/mL*
* This value would imply a significantly higher filtered load or a different contribution from tubular secretion.
* Calculations using this plasma concentration would not align with the provided excretion and secretion rates.
*There is insufficient information available to estimate the plasma concentration of Compound X*
* The problem provides all necessary values: **Inulin clearance (GFR)**, **net tubular secretion of Compound X**, and **net renal excretion of Compound X**.
* These parameters are sufficient to determine the filtered load and thus the plasma concentration of Compound X.
*1 mg/mL*
* A plasma concentration of 1 mg/mL would result in a lower filtered load than calculated and would not account for the observed net renal excretion.
* **Filtered load = 120 mL/min * 1 mg/mL = 120 mg/min**. Total excretion would then be 120 mg/min + 60 mg/min = 180 mg/min, which contradicts the given 300 mg/min.
*0.5 mg/mL*
* This plasma concentration would lead to an even lower filtered load, making it impossible to achieve the *net renal excretion of Compound X* given the tubular secretion.
* **Filtered load = 120 mL/min * 0.5 mg/mL = 60 mg/min**. Total excretion would be 60 mg/min + 60 mg/min = 120 mg/min, which is much lower than the given 300 mg/min.
Half-life and steady state concepts US Medical PG Question 10: A 65-year-old female patient with a past medical history of diabetes mellitus and an allergy to penicillin develops an infected abscess positive for MRSA on the third day of her hospital stay. She is started on an IV infusion of vancomycin at a dose of 1000 mg every 12 hours. Vancomycin is eliminated by first-order kinetics and has a half life of 6 hours. The volume of distribution of vancomycin is 0.5 L/kg. Assuming no loading dose is given, how long will it take for the drug to reach 94% of its plasma steady state concentration?
- A. 30 hours
- B. 12 hours
- C. 6 hours
- D. 18 hours
- E. 24 hours (Correct Answer)
Half-life and steady state concepts Explanation: ***24 hours***
- For a drug eliminated by **first-order kinetics**, it takes approximately **4 half-lives** to reach **93.75%** of steady state concentration, which is conventionally rounded to **94%**.
- Since the half-life of vancomycin is **6 hours**, reaching 94% of steady state requires: 4 × 6 hours = **24 hours**.
- This follows the pharmacokinetic principle that each half-life brings the drug closer to steady state: 1 t½ = 50%, 2 t½ = 75%, 3 t½ = 87.5%, 4 t½ = 93.75%.
*30 hours*
- This duration represents **five half-lives** (5 × 6 hours), at which point approximately **96.875%** (often rounded to 97%) of steady state would be reached.
- This exceeds the 94% target specified in the question.
*18 hours*
- This duration represents **three half-lives** (3 × 6 hours), at which point approximately **87.5%** of steady state concentration would be reached.
- This falls short of the 94% target.
*12 hours*
- This duration represents **two half-lives** (2 × 6 hours), at which point approximately **75%** of steady state concentration would be reached.
- This is insufficient time to reach 94% of plasma steady state concentration.
*6 hours*
- This duration represents **one half-life**, at which point approximately **50%** of steady state concentration would be reached.
- This is far too short to achieve near-steady state levels.
More Half-life and steady state concepts US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.