Cytochrome P450 system US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cytochrome P450 system. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cytochrome P450 system US Medical PG Question 1: A 63-year-old man comes to the physician for a routine health maintenance examination. He feels well. He has a history of hypertension, atrial fibrillation, bipolar disorder, and osteoarthritis of the knees. Current medications include lisinopril, amiodarone, lamotrigine, and acetaminophen. He started amiodarone 6 months ago and switched from lithium to lamotrigine 4 months ago. The patient does not smoke. He drinks 1–4 beers per week. He does not use illicit drugs. Vital signs are within normal limits. Examination shows no abnormalities. Laboratory studies show:
Serum
Na+ 137 mEq/L
K+ 4.2 mEq/L
Cl- 105 mEq/L
HCO3- 24 mEq/L
Urea nitrogen 14 mg/dL
Creatinine 0.9 mg/dL
Alkaline phosphatase 82 U/L
Aspartate aminotransferase (AST) 110 U/L
Alanine aminotransferase (ALT) 115 U/L
Which of the following is the most appropriate next step in management?
- A. Discontinue amiodarone (Correct Answer)
- B. Discontinue acetaminophen
- C. Follow-up laboratory results in 3 months
- D. Follow-up laboratory results in 6 months
- E. Decrease alcohol consumption
Cytochrome P450 system Explanation: ***Discontinue amiodarone***
* The patient has elevated **AST** and **ALT** levels, suggestive of **drug-induced liver injury**. Amiodarone is a known cause of **hepatotoxicity**, which can occur even with normal baseline liver function.
* **Amiodarone-induced liver injury** can range from asymptomatic transaminase elevation to **fulminant hepatic failure**; therefore, discontinuing the drug is crucial to prevent further liver damage.
*Discontinue acetaminophen*
* Although **acetaminophen** can cause **hepatotoxicity** at high doses, the patient is likely taking it at therapeutic doses for osteoarthritis, as suggested by its use in routine care and the absence of overdose symptoms.
* The chronic nature of amiodarone use (6 months) and its well-established risk of **liver injury** make it a more probable cause of the elevated transaminases than **therapeutic-dose acetaminophen**.
*Follow-up laboratory results in 3 months*
* The current **liver enzyme elevations** (AST 110 U/L, ALT 115 U/L) are significant and indicate acute liver injury. Waiting 3 months for follow-up without intervention significantly risks further liver damage.
* Prompt identification and removal of the offending agent are necessary to prevent potentially irreversible **hepatic injury**.
*Follow-up laboratory results in 6 months*
* Delaying follow-up for 6 months is an inappropriate and potentially harmful approach given the current enzyme elevations. There is an immediate need to identify and address the cause of **liver injury**.
* Such a delay could lead to progression of **liver damage**, especially if the causative agent (e.g., amiodarone) continues to be administered.
*Decrease alcohol consumption*
* While excessive alcohol consumption can cause **elevated liver enzymes**, the patient’s intake of 1–4 beers per week is considered light to moderate and is unlikely to be the sole cause of these significant elevations.
* The presence of a known **hepatotoxic medication** (amiodarone) alongside the elevated enzymes makes the drug a much more probable cause than the patient's modest alcohol intake.
Cytochrome P450 system US Medical PG Question 2: A 14-year-old boy is brought to the emergency department because of a 4-hour history of vomiting, lethargy, and confusion. Three days ago, he was treated with an over-the-counter medication for fever and runny nose. He is oriented only to person. His blood pressure is 100/70 mm Hg. Examination shows bilateral optic disc swelling and hepatomegaly. His blood glucose concentration is 65 mg/dL. Toxicology screening for serum acetaminophen is negative. The over-the-counter medication that was most likely used by this patient has which of the following additional effects?
- A. Increased partial thromboplastin time
- B. Decreased uric acid elimination
- C. Decreased expression of glycoprotein IIb/IIIa
- D. Irreversible inhibition of ATP synthase
- E. Irreversible inhibition of cyclooxygenase-1 (Correct Answer)
Cytochrome P450 system Explanation: ***Irreversible inhibition of cyclooxygenase-1***
- The patient's presentation is classic for **Reye syndrome** (vomiting, lethargy, confusion, cerebral edema with optic disc swelling, hepatomegaly, hypoglycemia) following recent viral illness treated with OTC medication
- **Aspirin** is strongly associated with Reye syndrome in children with viral infections and should be avoided in this population
- The "additional effect" of aspirin is its mechanism of action: **irreversible acetylation and inhibition of COX-1 and COX-2**
- This irreversible COX inhibition also explains aspirin's antiplatelet effects (via inhibition of thromboxane A2 synthesis) and anti-inflammatory properties
*Increased partial thromboplastin time*
- PTT measures the intrinsic and common coagulation pathways and is prolonged by **heparin** or clotting factor deficiencies
- Aspirin affects **platelet function** (prolonging bleeding time), not the coagulation cascade measured by PTT
- While Reye syndrome can cause coagulopathy from liver dysfunction, increased PTT is not a direct pharmacologic effect of aspirin
*Decreased uric acid elimination*
- **Low-dose aspirin** (<2 g/day) can decrease renal uric acid excretion and may precipitate gout
- While this is true, it is not the primary or most clinically relevant "additional effect" in this context
- High-dose aspirin actually increases uric acid excretion (uricosuric effect)
*Decreased expression of glycoprotein IIb/IIIa*
- This is the mechanism of **GP IIb/IIIa inhibitors** (abciximab, eptifibatide, tirofiban), not aspirin
- Aspirin inhibits platelet aggregation by preventing thromboxane A2 synthesis, not by affecting GP IIb/IIIa expression
- These are IV antiplatelet agents used in acute coronary syndromes, not OTC medications
*Irreversible inhibition of ATP synthase*
- This is not a mechanism of aspirin or other common OTC fever/cold medications
- While Reye syndrome involves mitochondrial dysfunction, aspirin does not directly inhibit ATP synthase
- The mitochondrial injury in Reye syndrome is likely multifactorial
Cytochrome P450 system US Medical PG Question 3: A 75-year-old female patient comes to the emergency department with altered mental status. She is brought in by her daughter with whom the patient lives. The patient’s daughter said they were watching TV when her mother became unresponsive. On exam the patient withdraws to pain but does not open her eyes or speak. An emergent head CT is done and shows an intracranial bleed. The patient is moved to the ICU and intubated. Further history is obtained from the daughter. The patient has a past medical history of diabetes and a previous stroke. Her medications are metformin and warfarin. The patient is compliant with all of her medications. The daughter says that the patient changed her diet about 1 month ago in response to a diet she saw on a talk show. Which of the following foods is most likely to cause the pathology seen in this patient?
- A. Grapefruit juice (Correct Answer)
- B. St. John’s wort
- C. Green tea
- D. Chili peppers
- E. Spinach
Cytochrome P450 system Explanation: ***Grapefruit juice***
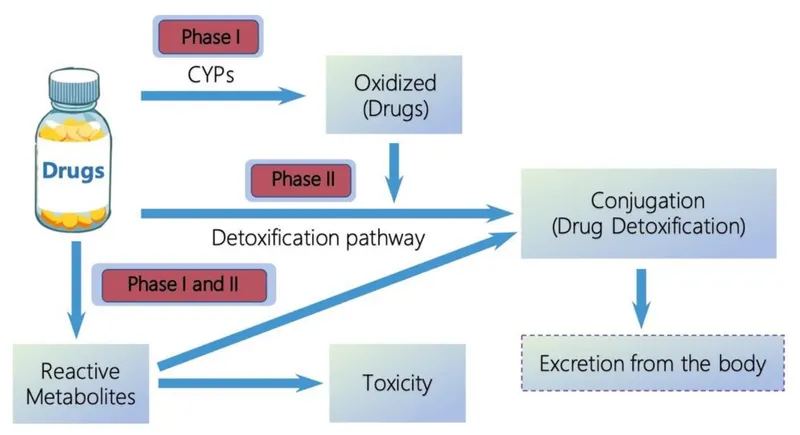
- **Grapefruit juice** is a potent inhibitor of **cytochrome P450 3A4 (CYP3A4)**, which is involved in the metabolism of **warfarin**.
- Inhibition of warfarin metabolism leads to increased warfarin levels, subsequently potentiating its **anticoagulant effect** and significantly increasing the risk of **bleeding**, including dangerous **intracranial hemorrhage**.
*St. John’s wort*
- **St. John's wort** is a known **CYP3A4 inducer**, meaning it increases the metabolism of drugs like warfarin.
- This typically leads to **decreased warfarin efficacy** and thus an increased risk of **thrombosis**, not bleeding.
*Green tea*
- **Green tea** contains **vitamin K**, which can **antagonize the effects of warfarin**.
- Ingesting large amounts of green tea could potentially *reduce* warfarin's anticoagulant effect, increasing the risk of clotting, rather than bleeding.
*Chili peppers*
- **Chili peppers** do not have a well-documented significant interaction with **warfarin** that would lead to increased bleeding risk.
- Their primary effects relate to gastric irritation or altered sensation, not anticoagulant modulation.
*Spinach*
- **Spinach** is high in **vitamin K**, which is a crucial factor in blood clotting and is directly antagonized by **warfarin**.
- Increased intake of spinach would likely **decrease the efficacy of warfarin**, leading to a higher risk of **clotting**, not bleeding.
Cytochrome P450 system US Medical PG Question 4: A 58-year-old man comes to the physician because of severe muscle aches and fatigue for 3 days. Last week he was diagnosed with atypical pneumonia and treated with clarithromycin. He has hyperlipidemia for which he takes lovastatin. Physical examination shows generalized tenderness of the proximal muscles in the upper and lower extremities. Serum studies show an elevated creatine kinase concentration. This patient's current symptoms are most likely caused by inhibition of which of the following hepatic enzymes?
- A. CYP2E1
- B. CYP3A4 (Correct Answer)
- C. CYP2C9
- D. CYP1A2
- E. CYP2C19
Cytochrome P450 system Explanation: ***CYP3A4***
- The patient is taking **lovastatin**, which is metabolized by **CYP3A4**. **Clarithromycin** is a potent **CYP3A4 inhibitor**.
- Inhibition of **CYP3A4** by clarithromycin leads to increased lovastatin levels, causing statin-induced **myopathy** (muscle aches, fatigue, and elevated creatine kinase).
*CYP2E1*
- This enzyme is primarily involved in the metabolism of compounds like **ethanol** and **acetaminophen**, not lovastatin.
- Its inhibition would not explain the interaction between clarithromycin and lovastatin.
*CYP2C9*
- This enzyme metabolizes drugs such as **warfarin** and **NSAIDs**, but it is not the primary enzyme responsible for lovastatin metabolism or its interaction with clarithromycin.
- Inhibition of **CYP2C9** would not lead to the described myopathy in this context.
*CYP1A2*
- **CYP1A2** is involved in the metabolism of drugs like **caffeine** and **theophylline**.
- It does not play a significant role in the metabolism of lovastatin, and its inhibition would not cause the observed symptoms.
*CYP2C19*
- **CYP2C19** metabolizes drugs such as **clopidogrel** and **omeprazole**.
- It is not the target enzyme for the interaction between lovastatin and clarithromycin.
Cytochrome P450 system US Medical PG Question 5: A 28-year-old woman presents to a psychiatrist with a 10-year history of unexplained anxiety symptoms. To date, she has not visited any psychiatrist, because she believes that she should not take medicines to change her emotions or thoughts. However, after explaining the nature of her disorder, the psychiatrist prescribes daily alprazolam. When she comes for her first follow-up, she reports excellent relief from her symptoms without any side-effects. The psychiatrist encourages her to continue her medication for the next 3 months and then return for a follow-up visit. After 3 months, she tells her psychiatrist that she has been experiencing excessive sedation and drowsiness over the last few weeks. The psychiatrist finds that she is taking alprazolam in the correct dosage, and she is not taking any other medication that causes sedation. Upon asking her about any recent changes in her lifestyle, she mentions that for the last 2 months, she has made a diet change. The psychiatrist tells her that diet change may be the reason why she is experiencing excessive sedation and drowsiness. Which of the following is the most likely diet change the psychiatrist is talking about?
- A. Daily consumption of tomatoes
- B. Daily consumption of St. John's wort
- C. Daily consumption of cruciferous vegetables
- D. Daily consumption of grapefruit juice (Correct Answer)
- E. Daily consumption of charcoal-broiled foods
Cytochrome P450 system Explanation: ***Daily consumption of grapefruit juice***
- **Grapefruit juice** is a potent inhibitor of the **CYP3A4 enzyme**, which is responsible for the metabolism of **alprazolam**.
- Inhibition of CYP3A4 leads to **increased plasma concentrations of alprazolam**, enhancing its sedative effects and causing drowsiness.
*Daily consumption of tomatoes*
- **Tomatoes** do not significantly interact with the metabolism of **alprazolam** or other benzodiazepines.
- They are a healthy food item with no known common drug interactions relevant to alprazolam's side effects.
*Daily consumption of St. John's wort*
- **St. John's wort** is a known **CYP3A4 inducer**, meaning it would *decrease* alprazolam levels, potentially leading to reduced efficacy.
- It would not cause increased sedation or drowsiness due to higher alprazolam concentrations.
*Daily consumption of cruciferous vegetables*
- **Cruciferous vegetables** (e.g., broccoli, cabbage) can induce certain CYP enzymes but generally do not significantly interfere with **alprazolam metabolism** to cause increased sedation.
- Their effects on drug metabolism are usually less pronounced or specific to other enzyme systems.
*Daily consumption of charcoal-broiled foods*
- **Charcoal-broiled foods** can induce **CYP1A2 enzymes**, but **alprazolam** is primarily metabolized by CYP3A4.
- Therefore, this dietary change is unlikely to significantly impact alprazolam metabolism or lead to increased sedation.
Cytochrome P450 system US Medical PG Question 6: A 76-year-old man comes to the physician for a follow-up examination. One week ago, he was prescribed azithromycin for acute bacterial sinusitis. He has a history of atrial fibrillation treated with warfarin and metoprolol. Physical examination shows no abnormalities. Compared to one month ago, laboratory studies show a mild increase in INR. Which of the following best explains this patient's laboratory finding?
- A. Drug-induced hepatotoxicity
- B. Depletion of intestinal flora
- C. Inhibition of cytochrome p450 (Correct Answer)
- D. Increased gastrointestinal absorption of warfarin
- E. Increased non-protein bound warfarin fraction
Cytochrome P450 system Explanation: ***Inhibition of cytochrome p450***
- **Azithromycin**, while a weaker inhibitor compared to erythromycin and clarithromycin, **does inhibit CYP3A4 and other cytochrome P450 enzymes** to a clinically significant degree.
- This inhibition **reduces warfarin metabolism**, leading to increased warfarin levels and **enhanced anticoagulant effect**, manifesting as an **increased INR**.
- This pharmacokinetic interaction is well-documented and is the **primary mechanism** for azithromycin-warfarin interaction.
*Depletion of intestinal flora*
- The theory that antibiotics deplete **vitamin K-producing gut bacteria** leading to increased warfarin effect is a **common misconception**.
- Humans obtain vitamin K primarily from **dietary sources** (leafy greens, vegetable oils), not from gut bacterial synthesis; intestinal bacteria contribute minimally to vitamin K stores.
- This mechanism has been **debunked** in modern pharmacology literature and does not explain antibiotic-warfarin interactions.
*Drug-induced hepatotoxicity*
- While hepatotoxicity can impair **clotting factor synthesis** and increase INR, **azithromycin** rarely causes significant liver injury.
- The presentation shows only a **mild INR increase** one week after starting therapy, without other signs of liver dysfunction.
- This acute, mild change is more consistent with a **pharmacokinetic drug interaction** than hepatotoxicity.
*Increased gastrointestinal absorption of warfarin*
- **Warfarin** has high oral bioavailability (~100%) under normal conditions.
- **Azithromycin** does not enhance the **gastrointestinal absorption** of warfarin.
- This mechanism is not supported by pharmacological evidence for this drug interaction.
*Increased non-protein bound warfarin fraction*
- Displacement of warfarin from **plasma protein binding sites** can transiently increase free drug.
- However, **azithromycin** does not significantly displace warfarin from **albumin**.
- This mechanism does not explain the sustained INR elevation seen with azithromycin therapy.
Cytochrome P450 system US Medical PG Question 7: You are currently employed as a clinical researcher working on clinical trials of a new drug to be used for the treatment of Parkinson's disease. Currently, you have already determined the safe clinical dose of the drug in a healthy patient. You are in the phase of drug development where the drug is studied in patients with the target disease to determine its efficacy. Which of the following phases is this new drug currently in?
- A. Phase 4
- B. Phase 1
- C. Phase 2 (Correct Answer)
- D. Phase 0
- E. Phase 3
Cytochrome P450 system Explanation: ***Phase 2***
- **Phase 2 trials** involve studying the drug in patients with the target disease to assess its **efficacy** and further evaluate safety, typically involving a few hundred patients.
- The question describes a stage after safe dosing in healthy patients (Phase 1) and before large-scale efficacy confirmation (Phase 3), focusing on efficacy in the target population.
*Phase 4*
- **Phase 4 trials** occur **after a drug has been approved** and marketed, monitoring long-term effects, optimal use, and rare side effects in a diverse patient population.
- This phase is conducted post-market approval, whereas the question describes a drug still in development prior to approval.
*Phase 1*
- **Phase 1 trials** primarily focus on determining the **safety and dosage** of a new drug in a **small group of healthy volunteers** (or sometimes patients with advanced disease if the drug is highly toxic).
- The question states that the safe clinical dose in a healthy patient has already been determined, indicating that Phase 1 has been completed.
*Phase 0*
- **Phase 0 trials** are exploratory, very early-stage studies designed to confirm that the drug reaches the target and acts as intended, typically involving a very small number of doses and participants.
- These trials are conducted much earlier in the development process, preceding the determination of safe clinical doses and large-scale efficacy studies.
*Phase 3*
- **Phase 3 trials** are large-scale studies involving hundreds to thousands of patients to confirm **efficacy**, monitor side effects, compare it to commonly used treatments, and collect information that will allow the drug to be used safely.
- While Phase 3 does assess efficacy, it follows Phase 2 and is typically conducted on a much larger scale before submitting for regulatory approval.
Cytochrome P450 system US Medical PG Question 8: Scientists are developing a new non-steroidal anti-inflammatory drug for osteoarthritis. Their hope is that the new drug will have a higher potency but the same efficacy as ibuprofen in the hope of minimizing gastrointestinal side effects. If ibuprofen is curve C in the figure provided, which of the following would be the curve for the new drug based on the scientists’ specifications? The desired therapeutic effect in patients is represented by the dashed line Y.
- A. Curve B
- B. Curve D
- C. Curve C
- D. Curve E
- E. Curve A (Correct Answer)
Cytochrome P450 system Explanation: ***Curve A***
- A drug with **higher potency** will achieve its maximal effect at a lower concentration, shifting the curve to the **left** (from C to A).
- **Same efficacy** means the drug reaches the **same maximal effect** (height on the y-axis) as ibuprofen (curve C), which curve A does.
*Curve B*
- This curve represents a drug with **lower potency** than ibuprofen, as it requires a higher concentration to achieve its maximal effect, shifting the curve to the right.
- While it has the same efficacy, it does not meet the requirement of higher potency.
*Curve D*
- Curve D shows a drug with **higher potency** (shifted left) but **lower efficacy** (lower maximal effect) compared to ibuprofen.
- The scientists are looking for the same efficacy, not lower efficacy.
*Curve E*
- Curve E represents a drug with **lower efficacy** (lower maximal effect) than ibuprofen.
- It also appears to have lower potency as the curve is shifted to the right, failing both criteria.
*Curve C*
- This curve is ibuprofen itself, meaning there is no change in potency or efficacy.
- The new drug needs to have higher potency while maintaining the same efficacy as ibuprofen.
Cytochrome P450 system US Medical PG Question 9: Serum studies show a troponin T concentration of 6.73 ng/mL (N < 0.01), and fingerstick blood glucose concentration of 145 mg/dL. The cardiac catheterization team is activated. Treatment with unfractionated heparin, aspirin, ticagrelor, and sublingual nitroglycerin is begun, and the patient's pain subsides. His temperature is 37.3°C (99.1°F), pulse is 65/min, respirations are 23/min, and blood pressure is 91/60 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 96%. Which of the following is the most appropriate additional pharmacotherapy?
- A. Intravenous morphine
- B. Intravenous furosemide
- C. Intravenous insulin
- D. Oral atorvastatin (Correct Answer)
- E. Intravenous nitroglycerin
Cytochrome P450 system Explanation: ***Oral atorvastatin***
- All patients with **acute coronary syndrome (ACS)** should receive high-intensity statin therapy, such as **atorvastatin 80 mg daily**, as early as possible.
- Statins stabilize plaques, reduce inflammation, and improve endothelial function, which are crucial in the acute setting of a myocardial infarction.
*Intravenous morphine*
- Morphine can be used for persistent chest pain refractory to nitroglycerin, but its routine use is now questioned due to potential adverse effects like hypotension and delayed antiplatelet absorption.
- The patient's pain has already subsided with initial treatment, and his blood pressure is already low (91/60 mm Hg), making morphine less appropriate.
*Intravenous furosemide*
- Furosemide is a loop diuretic primarily used for treating **fluid overload** and **pulmonary edema**, which are not indicated by the patient's current presentation (oxygen saturation 96%, no mention of crackles or dyspnea).
- Its use in a patient with **borderline hypotension** could worsen hemodynamic stability.
*Intravenous insulin*
- While the patient has elevated fingerstick glucose (145 mg/dL), this level does not immediately require intravenous insulin unless there is evidence of **diabetic ketoacidosis** or **hyperosmolar hyperglycemic state**, or persistent severe hyperglycemia.
- More moderate hyperglycemia can often be managed with subcutaneous insulin or diet in the acute phase, and focuses remain on cardiac stabilization.
*Intravenous nitroglycerin*
- Intravenous nitroglycerin is indicated for ongoing ischemic chest pain or uncontrolled hypertension in ACS, but the patient's pain has subsided and he is **hypotensive** (91/60 mm Hg).
- Administering more nitroglycerin would likely worsen his hypotension and could compromise coronary perfusion.
Cytochrome P450 system US Medical PG Question 10: A 44-year-old man presents to the clinic with recurrent epigastric pain following meals for a month. He adds that the pain radiates up his neck and throat. Over the counter antacids have not helped. On further questioning, he endorses foul breath upon waking in the morning and worsening of pain when lying down. He denies any recent weight loss. His temperature is 37°C (98.6°F), respirations are 15/min, pulse is 70/min, and blood pressure is 100/84 mm Hg. A physical examination is performed which is within normal limits except for mild tenderness on deep palpation of the epigastrium. An ECG performed in the clinic shows no abnormalities. What is the next best step in the management of this patient?
- A. Liquid antacid
- B. Lansoprazole (Correct Answer)
- C. Endoscopy
- D. Barium swallow
- E. Ranitidine
Cytochrome P450 system Explanation: ***Correct Option: Lansoprazole***
- The patient's symptoms, including **postprandial epigastric pain that radiates up the neck and throat**, **foul breath**, and **worsening pain when lying down**, are highly suggestive of **gastroesophageal reflux disease (GERD)**.
- **Proton pump inhibitors (PPIs)** such as lansoprazole are the most effective medications for symptom relief and healing in GERD due to their potent and sustained acid suppression.
- PPIs are first-line therapy for patients with **moderate-to-severe GERD symptoms** or those who have failed antacid therapy.
*Incorrect Option: Liquid antacid*
- While antacids can provide **temporary relief** for heartburn, they do not address the underlying pathology of GERD and are generally **insufficient for chronic or severe symptoms**.
- The patient has already tried **over-the-counter antacids without relief**, indicating that a stronger medication is needed.
*Incorrect Option: Endoscopy*
- **Endoscopy** is typically reserved for patients with **alarm symptoms** (e.g., dysphagia, odynophagia, weight loss, GI bleeding, anemia) or those who **fail to respond to an empiric trial of PPIs**.
- This patient does not have alarm symptoms, and a trial of PPIs is the appropriate initial step.
*Incorrect Option: Barium swallow*
- A **barium swallow** (esophagogram) can be useful for evaluating **structural abnormalities** of the esophagus, such as strictures, rings, or motility disorders.
- However, it has **limited sensitivity for diagnosing GERD** itself and is not typically the first-line diagnostic or therapeutic step in uncomplicated GERD.
*Incorrect Option: Ranitidine*
- **Ranitidine** is an **H2 receptor antagonist** that reduces stomach acid production, but it is generally **less potent and less effective than PPIs** for controlling GERD symptoms and healing erosions.
- It might be considered for milder cases or as an add-on therapy, but a PPI like lansoprazole is preferred for initial empiric treatment given the persistent symptoms.
More Cytochrome P450 system US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.