TNF inhibitors US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for TNF inhibitors. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
TNF inhibitors US Medical PG Question 1: A 50-year-old woman presents to the clinic with joint pain that has persisted for the last 2 months. She reports having intermittently swollen, painful hands bilaterally. She adds that when she wakes up in the morning, her hands are stiff and do not loosen up until an hour later. The pain tends to improve with movement. Physical examination is significant for warm, swollen, tender proximal interphalangeal joints, metacarpophalangeal joints, and wrists bilaterally. Laboratory results are positive for rheumatoid factor (4-fold greater than the upper limit of normal (ULN)) and anti-cyclic citrullinated peptide (anti-CCP) antibodies (3-fold greater than ULN). CRP and ESR are elevated. Plain X-rays of the hand joints show periarticular osteopenia and bony erosions. She was started on the first-line drug for her condition which inhibits dihydrofolate reductase. Which medication was this patient started on?
- A. Hydroxyurea
- B. Allopurinol
- C. Methotrexate (Correct Answer)
- D. 5-fluorouracil
- E. Leflunomide
TNF inhibitors Explanation: ***Methotrexate***
- The patient's clinical presentation (symmetrical polyarthritis, morning stiffness, elevated inflammatory markers, positive **rheumatoid factor**, and **anti-CCP antibodies**) is classic for **rheumatoid arthritis (RA)**.
- **Methotrexate** is the **first-line disease-modifying anti-rheumatic drug (DMARD)** for RA and acts by inhibiting **dihydrofolate reductase**, thereby interfering with purine and pyrimidine synthesis.
*Hydroxyurea*
- **Hydroxyurea** is an antineoplastic agent that works by inhibiting **ribonucleotide reductase**, not dihydrofolate reductase.
- It is primarily used in conditions like **myeloproliferative disorders** (e.g., chronic myeloid leukemia, polycythemia vera, essential thrombocythemia) and **sickle cell disease**, not rheumatoid arthritis.
*Allopurinol*
- **Allopurinol** is a **xanthine oxidase inhibitor** used to reduce **uric acid production** in conditions like **gout and tumor lysis syndrome**.
- It is not indicated for the treatment of rheumatoid arthritis, nor does it inhibit dihydrofolate reductase.
*5-fluorouracil*
- **5-fluorouracil** is a **pyrimidine analog** that inhibits **thymidylate synthase** (after being metabolized to 5-FdUMP), primarily used in **chemotherapy for various cancers**, especially gastrointestinal malignancies.
- It does not inhibit dihydrofolate reductase and is not used to treat rheumatoid arthritis.
*Leflunomide*
- **Leflunomide** is another DMARD used for rheumatoid arthritis, but it inhibits **dihydroorotate dehydrogenase**, an enzyme involved in *de novo pyrimidine synthesis*, not dihydrofolate reductase.
- While it is a treatment for RA, it is not the medication that acts specifically by inhibiting dihydrofolate reductase.
TNF inhibitors US Medical PG Question 2: A 22-year-old man comes to the physician for a follow-up evaluation for chronic lower back pain. He has back stiffness that lasts all morning and slowly improves throughout the day. He has tried multiple over-the-counter medications, including ibuprofen, without any improvement in his symptoms. Physical examination shows tenderness over the iliac crest bilaterally and limited range of motion of the lumbar spine with forward flexion. The results of HLA-B27 testing are positive. An x-ray of the lumbar spine shows fusion of the lumbar vertebrae and sacroiliac joints. The physician plans to prescribe a new medication but first orders a tuberculin skin test to assess for the risk of latent tuberculosis reactivation. Inhibition of which of the following is the most likely primary mechanism of action of this drug?
- A. mTOR kinase
- B. Calcineurin
- C. NF-κB
- D. Inosine monophosphate dehydrogenase
- E. TNF-α (Correct Answer)
TNF inhibitors Explanation: **TNF-α**
- The clinical presentation with **chronic lower back pain**, morning stiffness, **limited lumbar spine range of motion**, positive **HLA-B27**, and **fusion of lumbar vertebrae and sacroiliac joints** is highly suggestive of **ankylosing spondylitis**.
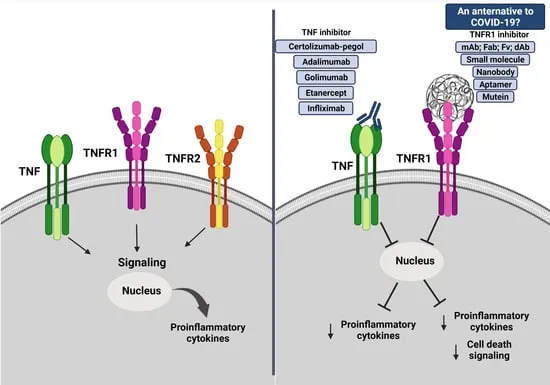
- Biologic medications, specifically **TNF-α inhibitors**, are a cornerstone of treatment for ankylosing spondylitis, especially when conventional therapies like NSAIDs fail. The mention of screening for latent tuberculosis reactivation strongly points to the use of a TNF-α inhibitor, as these drugs increase the risk of TB reactivation.
*mTOR kinase*
- **mTOR inhibitors** (e.g., sirolimus, everolimus) are primarily used as **immunosuppressants** in organ transplantation and in some cancers.
- They are not a first-line or common treatment for ankylosing spondylitis or other spondyloarthropathies.
*Calcineurin*
- **Calcineurin inhibitors** (e.g., cyclosporine, tacrolimus) are potent **immunosuppressants** used in transplant rejection prevention and some autoimmune diseases.
- While they can have immunosuppressive effects, they are not the primary target for the treatment of ankylosing spondylitis.
*NF-κB*
- **NF-κB** is a crucial transcription factor involved in inflammation and immune responses. While relevant to inflammatory conditions, directly targeting NF-κB is not the primary mechanism of action for the most effective biologic therapies used in ankylosing spondylitis.
- **Glucocorticoids** can inhibit NF-κB, but they are not the main long-term treatment for ankylosing spondylitis, and the context points to a biologic.
*Inosine monophosphate dehydrogenase*
- **Inosine monophosphate dehydrogenase (IMPDH) inhibitors** (e.g., mycophenolate mofetil) block purine synthesis, thus inhibiting lymphocyte proliferation.
- These drugs are used in **transplantation** and some **autoimmune diseases** (e.g., lupus, vasculitis) but are not typically used for ankylosing spondylitis.
TNF inhibitors US Medical PG Question 3: A 24-year-old man comes to the physician for a routine health maintenance examination. He feels well. He has type 1 diabetes mellitus. His only medication is insulin. He immigrated from Nepal 2 weeks ago . He lives in a shelter. He has smoked one pack of cigarettes daily for the past 5 years. He has not received any routine childhood vaccinations. The patient appears healthy and well nourished. He is 172 cm (5 ft 8 in) tall and weighs 68 kg (150 lb); BMI is 23 kg/m2. His temperature is 36.8°C (98.2°F), pulse is 72/min, and blood pressure is 123/82 mm Hg. Examination shows a healed scar over his right femur. The remainder of the examination shows no abnormalities. A purified protein derivative (PPD) skin test is performed. Three days later, an induration of 13 mm is noted. Which of the following is the most appropriate initial step in the management of this patient?
- A. Administer isoniazid for 9 months
- B. Collect sputum sample for culture
- C. Perform interferon-γ release assay
- D. Obtain a chest x-ray (Correct Answer)
- E. Perform PCR of the sputum
TNF inhibitors Explanation: ***Obtain a chest x-ray***
- A **positive PPD test** (13 mm induration in a patient with risk factors) indicates possible **latent tuberculosis infection (LTBI)**, but before initiating treatment, it's crucial to rule out **active tuberculosis (TB)**.
- A chest x-ray is the initial step to screen for signs of active disease, such as **infiltrates, cavitations**, or **lymphadenopathy**, which would necessitate a different treatment regimen than LTBI.
*Administer isoniazid for 9 months*
- This is a standard treatment for **LTBI**, but it should only be initiated after **active TB has been ruled out**.
- Treating active TB with LTBI monotherapy would be inadequate and could lead to **drug resistance**.
*Collect sputum sample for culture*
- **Sputum culture** is essential for diagnosing active pulmonary TB and for **drug susceptibility testing**, but it's typically performed *after* a chest x-ray suggests active disease.
- In a patient with a positive PPD and no symptoms, starting with sputum cultures without imaging is not the most appropriate first step.
*Perform interferon-γ release assay*
- **Interferon-γ release assays (IGRAs)**, such as QuantiFERON-TB Gold or T-Spot.TB, are alternative tests for detecting **M. tuberculosis infection**.
- While IGRAs can be used in place of or in conjunction with PPD, they also do not differentiate between latent and active infection, so a chest x-ray would still be required.
*Perform PCR of the sputum*
- **PCR (nucleic acid amplification test)** of sputum rapidly detects *M. tuberculosis* DNA and is a valuable tool for diagnosing **active TB**, especially in cases where rapid results are needed.
- However, like sputum culture, it is usually reserved for situations where there is a strong suspicion of active disease based on clinical symptoms or imaging findings.
TNF inhibitors US Medical PG Question 4: A 55-year-old woman comes to the clinic complaining of joint pain and stiffness for the past year. The pain is mainly concentrated in her hands and is usually worse towards the late afternoon. It is described with a burning quality that surrounds the joint with some numbness and tingling. The stiffness is especially worse in the morning and lasts approximately for 15-20 minutes. Her past medical history is significant for recurrent gastric ulcers. She reports that her mother struggled with lupus and is concerned that she might have the same thing. She denies fever, rashes, ulcers, genitourinary symptoms, weight loss, or bowel changes. Physical examination is significant for mild tenderness at the distal interphalangeal joints bilaterally. What is the best initial medication to prescribe to this patient?
- A. Methotrexate
- B. Hydroxychloroquine
- C. Infliximab
- D. Aspirin
- E. Acetaminophen (Correct Answer)
TNF inhibitors Explanation: ***Acetaminophen***
- Given the patient's symptoms of joint pain worse in the late afternoon, morning stiffness lasting 15-20 minutes, and tenderness at the **distal interphalangeal joints (DIPs)**, **osteoarthritis** is the most likely diagnosis.
- As **acetaminophen** is an **analgesic** and a relatively safe medication, it is considered a first-line treatment for pain management in osteoarthritis, especially given her history of recurrent gastric ulcers which makes NSAIDs less favorable.
*Methotrexate*
- **Methotrexate** is a **disease-modifying antirheumatic drug (DMARD)** primarily used for inflammatory arthritis like **rheumatoid arthritis** or **psoriatic arthritis**.
- Its side effects include **gastrointestinal upset** and **hepatic toxicity**, and it is not a first-line agent for osteoarthritis.
*Hydroxychloroquine*
- **Hydroxychloroquine** is an antimalarial drug used as a DMARD for conditions like **lupus** and **rheumatoid arthritis**.
- While the patient's mother had lupus, her current symptoms are not consistent with lupus, and hydroxychloroquine is not indicated for osteoarthritis.
*Infliximab*
- **Infliximab** is a **biologic agent (TNF-alpha inhibitor)** used for severe inflammatory conditions like **rheumatoid arthritis**, **ankylosing spondylitis**, and inflammatory bowel disease.
- It carries significant risks, including **immunosuppression** and **infusion reactions**, and is not appropriate for initial treatment of osteoarthritis.
*Aspirin*
- **Aspirin**, particularly in anti-inflammatory doses, can cause **gastric irritation** and is contraindicated or used with extreme caution in patients with a history of recurrent gastric ulcers.
- Although it has analgesic properties, its anti-inflammatory effects are not specifically targeted at osteoarthritis as a first-line given her ulcer history, and other NSAIDs would be preferred if anti-inflammatory action was needed and gastric issues were not present.
TNF inhibitors US Medical PG Question 5: A 65-year-old man comes to the physician for a routine health maintenance examination. He feels well. His most recent examination 2 years ago included purified protein derivative (PPD) skin testing and showed no abnormalities. He is a retired physician and recently came back from rural China where he completed a voluntary service at a local healthcare center. A PPD skin test is performed. Three days later, an induration of 12 mm is noted. An x-ray of the chest shows no abnormalities. He is started on a drug that inhibits the synthesis of mycolic acid. This patient is at greatest risk of developing which of the following adverse effects?
- A. Cytochrome P-450 induction
- B. Hyperuricemia
- C. Liver injury (Correct Answer)
- D. Optic neuropathy
- E. Nephrotoxicity
TNF inhibitors Explanation: ***Liver injury***
- The drug described is **isoniazid**, which inhibits **mycolic acid synthesis** and is first-line treatment for **latent tuberculosis infection**.
- **Isoniazid-induced hepatotoxicity** is the most significant adverse effect, with risk increasing dramatically in patients **>35 years old** (this patient is 65).
- Additional risk factors include alcohol use, pre-existing liver disease, and concurrent hepatotoxic medications.
- Patients should be monitored with baseline and periodic liver function tests.
*Cytochrome P-450 induction*
- **Rifampin**, not isoniazid, is a potent **CYP450 inducer** that decreases levels of many co-administered drugs.
- Isoniazid is actually a **CYP450 inhibitor** (inhibits CYP2C19, CYP3A4), which can increase levels of other drugs like phenytoin and warfarin.
*Hyperuricemia*
- **Pyrazinamide** is the anti-tuberculosis drug that causes **hyperuricemia** by inhibiting renal tubular secretion of uric acid.
- This can precipitate acute gout attacks in susceptible patients.
- Isoniazid does not affect uric acid metabolism.
*Optic neuropathy*
- **Ethambutol** causes dose-dependent **optic neuropathy**, presenting with decreased visual acuity and **red-green color blindness**.
- Patients on ethambutol require baseline and monthly visual assessments.
- Isoniazid is not associated with optic toxicity.
*Nephrotoxicity*
- **Aminoglycosides** (e.g., streptomycin) and some other antibiotics cause **nephrotoxicity** through tubular damage.
- Isoniazid is not significantly nephrotoxic and does not require renal dose adjustment.
TNF inhibitors US Medical PG Question 6: A 47-year-old woman presents to the physician with complaints of fatigue accompanied by symmetric pain, swelling, and stiffness in her wrists, fingers, knees, and other joints. She describes the stiffness as being particularly severe upon awakening, but gradually improves as she moves throughout her day. Her physician initially suggests that she take NSAIDs. However, after a few months of minimal symptomatic improvement, she is prescribed an immunosuppressive drug that has a mechanism of preventing IL-2 transcription. What is the main toxicity that the patient must be aware of with this particular class of drugs?
- A. Pancytopenia
- B. Osteoporosis
- C. Hepatotoxicity
- D. Nephrotoxicity (Correct Answer)
- E. Hyperglycemia
TNF inhibitors Explanation: ***Nephrotoxicity***
- The drug described, which prevents **IL-2 transcription**, is likely a **calcineurin inhibitor** like cyclosporine or tacrolimus, often used in autoimmune diseases.
- **Nephrotoxicity** (kidney damage) is a major dose-limiting toxicity of calcineurin inhibitors, causing both acute and chronic kidney injury.
*Pancytopenia*
- While some immunosuppressants can cause **pancytopenia** (e.g., azathioprine, methotrexate), it is not the classic or primary toxicity associated with calcineurin inhibitors.
- Calcineurin inhibitors primarily affect **renal function** and can cause other side effects like hypertension or neurotoxicity.
*Osteoporosis*
- **Osteoporosis** is a known side effect of long-term glucocorticoid use, but not typically a primary toxicity of calcineurin inhibitors.
- Glucocorticoids reduce bone formation and increase bone resorption, leading to bone density loss.
*Hepatotoxicity*
- **Hepatotoxicity** (liver damage) can occur with various immunosuppressants, such as methotrexate, but it is not the most prominent or defining toxicity for calcineurin inhibitors.
- While cyclosporine can cause some liver enzyme elevation, **nephrotoxicity** is far more common and severe.
*Hyperglycemia*
- **Hyperglycemia** can be a side effect of some immunosuppressants, particularly **glucocorticoids** and **tacrolimus** (another calcineurin inhibitor).
- However, for the class of drugs that prevent IL-2 transcription (calcineurin inhibitors), **nephrotoxicity** remains the most significant and common major toxicity to be aware of.
TNF inhibitors US Medical PG Question 7: A 32-year-old woman comes to the physician because of pain and stiffness in both of her hands for the past 3 weeks. The pain is most severe early in the day and does not respond to ibuprofen. She has no history of serious illness and takes no medications. Vital signs are within normal limits. Examination shows swelling and tenderness of the wrists and metacarpophalangeal joints bilaterally. Range of motion is decreased due to pain. There are subcutaneous, nontender, firm, mobile nodules on the extensor surface of the forearm. Which of the following is the most appropriate pharmacotherapy for this patient's current symptoms?
- A. Adalimumab
- B. Prednisone (Correct Answer)
- C. Methotrexate
- D. Colchicine
- E. Sulfasalazine
TNF inhibitors Explanation: ***Prednisone***
- The patient presents with **symmetrical polyarthritis** of the small joints, morning stiffness unresponsive to NSAIDs, and **rheumatoid nodules**, which are classic features of **rheumatoid arthritis (RA)**.
- For **immediate symptom control** of acute RA flares, **glucocorticoids** like prednisone are highly effective in rapidly reducing inflammation and pain.
- In clinical practice, prednisone would be used as **bridge therapy** while initiating disease-modifying therapy, providing symptomatic relief within days.
*Methotrexate*
- Methotrexate is a **disease-modifying antirheumatic drug (DMARD)** and is the **first-line agent for long-term RA management** per current guidelines.
- While this should be initiated promptly in newly diagnosed RA, it has a **slow onset of action (6-12 weeks)** and would not provide immediate relief for the patient's current severe symptoms.
- In practice, methotrexate would be started concurrently with a short course of glucocorticoids.
*Adalimumab*
- Adalimumab is a **TNF-alpha inhibitor**, a **biologic DMARD**, used for moderate to severe RA, typically when conventional DMARDs are insufficient.
- It is **not first-line therapy** for newly diagnosed RA and requires prior screening for latent infections due to **immunosuppression risk**.
- Like methotrexate, it has a delayed onset of action and would not provide rapid symptom relief.
*Colchicine*
- Colchicine is primarily used for the treatment of **gout** and **pseudogout**, by inhibiting neutrophil migration and microtubule polymerization.
- It is **not indicated** for the management of rheumatoid arthritis.
*Sulfasalazine*
- Sulfasalazine is a **conventional synthetic DMARD** used in the treatment of RA, particularly in mild to moderate cases or as combination therapy.
- Like methotrexate, it has a **slow onset of action (weeks to months)** and is not appropriate for rapid symptom control in an acute presentation.
TNF inhibitors US Medical PG Question 8: A 29-year-old female presents to her gynecologist complaining of a painful rash around her genitals. She has multiple sexual partners and uses condoms intermittently. Her last STD screen one year ago was negative. On examination, she has bilateral erosive vesicles on her labia majora and painful inguinal lymphadenopathy. She is started on an oral medication that requires a specific thymidine kinase for activation. Which of the following adverse effects is associated with this drug?
- A. Photosensitivity
- B. Deafness
- C. Renal failure (Correct Answer)
- D. Gingival hyperplasia
- E. Pulmonary fibrosis
TNF inhibitors Explanation: ***Renal failure***
- The patient's symptoms (painful genital rash, erosive vesicles, inguinal lymphadenopathy) are highly suggestive of **herpes simplex virus (HSV) infection**, likely genital herpes.
- The drug described is an antiviral agent like **acyclovir, valacyclovir, or famciclovir**, which require **viral thymidine kinase** for activation and are known to cause **renal impairment** (nephrotoxicity) as an adverse effect, especially with high doses or in dehydrated patients due to crystal nephropathy.
*Photosensitivity*
- **Photosensitivity** is a common side effect of some antibiotics (e.g., tetracyclines, sulfonamides), diuretics (e.g., thiazides), and antifungals, but it is **not a prominent adverse effect of acyclovir or its derivatives**.
- While theoretical, it is not a clinically significant or frequently observed adverse effect associated with the class of antiviral drugs used for HSV.
*Deafness*
- **Ototoxicity**, leading to deafness or hearing loss, is a well-known adverse effect of certain classes of drugs, such as **aminoglycoside antibiotics** (e.g., gentamicin) and **loop diuretics** (e.g., furosemide).
- It is **not an adverse effect** associated with antiviral medications like acyclovir.
*Gingival hyperplasia*
- **Gingival hyperplasia** (overgrowth of gum tissue) is a recognized side effect of specific medications including **phenytoin** (an anticonvulsant), **cyclosporine** (an immunosuppressant), and **calcium channel blockers** (e.g., nifedipine, amlodipine).
- This adverse effect is **not associated with antiviral drugs** used to treat herpes simplex.
*Pulmonary fibrosis*
- **Pulmonary fibrosis** is a serious adverse effect linked to various drugs like **amiodarone** (an antiarrhythmic), **bleomycin** (a chemotherapeutic agent), **methotrexate** (an immunosuppressant/chemotherapeutic), and **nitrofurantoin** (an antibiotic).
- **Antiviral medications for HSV** do not typically cause pulmonary fibrosis.
TNF inhibitors US Medical PG Question 9: A 38-year-old woman comes to the physician for a follow-up examination. Two years ago, she was diagnosed with multiple sclerosis. Three weeks ago, she was admitted and treated for right lower leg weakness with high-dose methylprednisone for 5 days. She has had 4 exacerbations over the past 6 months. Current medications include interferon beta and a multivitamin. Her temperature is 37°C (98.6°F), pulse is 90/min, and blood pressure is 116/74 mm Hg. Examination shows pallor of the right optic disk. Neurologic examination shows no focal findings. She is anxious about the number of exacerbations and repeated hospitalizations. She is counseled about the second-line treatment options available to her. She consents to treatment with natalizumab. However, she has read online about its adverse effects and is concerned. This patient is at increased risk for which of the following complications?
- A. Tuberculosis
- B. Syndrome of inappropriate antidiuretic hormone
- C. Parkinsonism
- D. Progressive multifocal leukoencephalopathy (Correct Answer)
- E. Aplastic anemia
TNF inhibitors Explanation: ***Progressive multifocal leukoencephalopathy***
- **Natalizumab** is a monoclonal antibody that blocks the binding of leukocytes to endothelial cells, preventing their entry into the central nervous system. This immunosuppressive effect increases the risk of **progressive multifocal leukoencephalopathy (PML)**, especially in patients who are positive for the **JC virus**.
- PML is a serious and often fatal opportunistic infection of the brain caused by the **JC virus**, which demyelinates axons and leads to severe neurological deficits.
*Tuberculosis*
- While some immunosuppressants can reactivate **latent tuberculosis**, natalizumab is not typically associated with an increased risk of TB compared to other immunomodulatory drugs like TNF-alpha inhibitors.
- The mechanism of action of natalizumab (alpha-4 integrin blocker) does not directly impede the immune response responsible for containing mycobacterial infections to the same extent as other treatments.
*Syndrome of inappropriate antidiuretic hormone*
- **SIADH** is not a known adverse effect of natalizumab.
- SIADH is characterized by excessive secretion of **antidiuretic hormone**, leading to hyponatremia, and is often associated with certain medications (e.g., SSRIs, carbamazepine) or underlying conditions like malignancy or pulmonary disease.
*Parkinsonism*
- Parkinsonism involves symptoms like **bradykinesia**, rigidity, and tremor, and is a neurodegenerative disorder.
- There is **no evidence** suggesting a causal link between natalizumab treatment and the development of Parkinsonism.
*Aplastic anemia*
- **Aplastic anemia** is a rare but severe condition where the bone marrow fails to produce blood cells.
- This adverse effect is not associated with natalizumab; it is more commonly linked to certain **chemotherapeutic agents**, radiation, or specific antimicrobial drugs like chloramphenicol.
TNF inhibitors US Medical PG Question 10: A 50-year-old woman comes to the physician for the evaluation of excessive hair growth on her chin over the past 2 weeks. She also reports progressive enlargement of her gums. Three months ago, she underwent a liver transplantation due to Wilson disease. Following the procedure, the patient was started on transplant rejection prophylaxis. She has a history of poorly-controlled type 2 diabetes mellitus. Temperature is 37°C (98.6°F), pulse is 80/min, respirations are 22/min, and blood pressure is 150/80 mm Hg. Physical examination shows dark-pigmented, coarse hair on the chin, upper lip, and chest. The gingiva and the labial mucosa are swollen. There is a well-healed scar on her right lower abdomen. Which of the following drugs is the most likely cause of this patient's findings?
- A. Daclizumab
- B. Cyclosporine (Correct Answer)
- C. Sirolimus
- D. Methotrexate
- E. Tacrolimus
TNF inhibitors Explanation: **Cyclosporine**
* This patient's **combination of hirsutism** (excessive hair growth) **and gingival hyperplasia** (gum enlargement) is the classic presentation of cyclosporine toxicity, an immunosuppressant commonly used for transplant rejection prophylaxis.
* Cyclosporine is a **calcineurin inhibitor** that prevents T-cell activation and is highly effective in preventing graft rejection.
* The **simultaneous presence of both hirsutism and prominent gingival hyperplasia** is particularly characteristic of cyclosporine.
*Daclizumab*
* **Daclizumab** is a **monoclonal antibody** targeting the IL-2 receptor, which was previously used for transplant prophylaxis but has been discontinued for this indication.
* It is not associated with hirsutism or gingival hyperplasia.
*Sirolimus*
* **Sirolimus** is an **mTOR inhibitor** used as an immunosuppressant, known for side effects like hyperlipidemia, myelosuppression, and delayed wound healing.
* It does **not** typically cause hirsutism or gingival hyperplasia.
*Methotrexate*
* **Methotrexate** is an **antimetabolite** and immunosuppressant commonly used in autoimmune diseases and cancer, with side effects including bone marrow suppression, mucositis, and liver toxicity.
* Hirsutism and gingival hyperplasia are **not** characteristic side effects of methotrexate.
*Tacrolimus*
* **Tacrolimus** is another **calcineurin inhibitor**, similar to cyclosporine, but with a different side effect profile. While tacrolimus can cause hirsutism, **gingival hyperplasia is significantly less common** with tacrolimus compared to cyclosporine.
* The **presence of prominent gingival hyperplasia alongside hirsutism strongly favors cyclosporine** over tacrolimus.
* Tacrolimus is more commonly associated with **neurotoxicity** (e.g., tremor) and **nephrotoxicity**.
More TNF inhibitors US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.