T-cell depleting antibodies US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for T-cell depleting antibodies. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
T-cell depleting antibodies US Medical PG Question 1: A 34-year-old female medical professional who works for a non-governmental organization visits her primary care provider for a routine health check-up. She made a recent trip to Sub-Saharan Africa where she participated in a humanitarian medical project. Her medical history and physical examination are unremarkable. A chest radiograph and a tuberculin skin test (PPD) are ordered. The chest radiograph is performed at the side and the PPD reaction measures 12 mm after 72 hours. Which of the following mechanisms is involved in the skin test reaction?
- A. Complement activation
- B. Formation of immune complexes
- C. Th1-mediated delayed-type hypersensitivity (Correct Answer)
- D. IgE cross-linking
T-cell depleting antibodies Explanation: ***Th1-mediated delayed-type hypersensitivity***
- The **tuberculin skin test (PPD)** is a classic example of a **Type IV hypersensitivity reaction**, which is mediated by **T-helper 1 (Th1) cells** [3].
- Upon re-exposure to mycobacterial antigens (tuberculin), previously sensitized Th1 cells release **cytokines** that recruit and activate **macrophages**, leading to the characteristic induration and erythema [3].
*Complement activation*
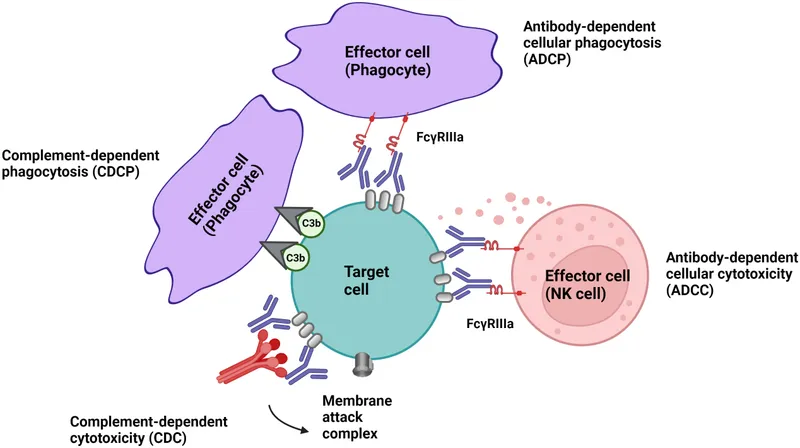
- This mechanism is primarily involved in host defense against microbial infections and in **Type II** and **Type III hypersensitivity reactions**, not Delayed-Type Hypersensitivity [2].
- Activation of the complement system leads to cell lysis, opsonization, and inflammation, but it does not directly drive the PPD skin test response [2].
*Formation of immune complexes*
- This describes a **Type III hypersensitivity reaction**, where **antigen-antibody complexes** deposit in tissues, leading to inflammation and tissue damage [1].
- Examples include serum sickness and Arthus reaction, which are distinct from the cell-mediated PPD response [1].
*IgE cross-linking*
- This mechanism is characteristic of **Type I (immediate) hypersensitivity reactions**, commonly known as allergies [4].
- **IgE antibodies** bind to mast cells and basophils; subsequent cross-linking by antigens triggers the release of mediators like histamine, leading to rapid allergic symptoms [4].
T-cell depleting antibodies US Medical PG Question 2: Two weeks after undergoing allogeneic stem cell transplant for multiple myeloma, a 55-year-old man develops a severely pruritic rash, abdominal cramps, and profuse diarrhea. He appears lethargic. Physical examination shows yellow sclerae. There is a generalized maculopapular rash on his face, trunk, and lower extremities, and desquamation of both soles. His serum alanine aminotransferase is 115 U/L, serum aspartate aminotransferase is 97 U/L, and serum total bilirubin is 2.7 mg/dL. Which of the following is the most likely underlying cause of this patient's condition?
- A. Preformed cytotoxic anti-HLA antibodies
- B. Proliferating transplanted B cells
- C. Activated recipient T cells
- D. Donor T cells in the graft (Correct Answer)
- E. Newly formed anti-HLA antibodies
T-cell depleting antibodies Explanation: ***Donor T cells in the graft***
- The symptoms (rash, GI symptoms, liver dysfunction) after an allogeneic stem cell transplant are classic signs of **acute graft-versus-host disease (GVHD)**. This condition occurs when **immunocompetent T cells from the donor graft** recognize the recipient's tissues as foreign and mount an immune attack.
- The rapid onset within two weeks post-transplant, elevated liver enzymes, jaundice (**yellow sclerae**, **elevated bilirubin**), severe pruritic rash, and GI symptoms (**abdominal cramps**, **profuse diarrhea**) are all characteristic manifestations of acute GVHD.
*Preformed cytotoxic anti-HLA antibodies*
- Preformed antibodies would typically cause **hyperacute rejection**, which occurs within minutes to hours of transplantation and involves widespread thrombosis and necrosis of the graft, not the systemic symptoms seen here.
- This reaction is mediated by the recipient's antibodies attacking donor antigens, leading to immediate graft failure.
*Proliferating transplanted B cells*
- Transplanted B cells can contribute to chronic GVHD through antibody production, but they are not the primary mediators of **acute GVHD**; acute GVHD is predominantly a T cell-mediated process.
- Proliferation of donor B cells is more commonly associated with post-transplant lymphoproliferative disorders (PTLD) or chronic GVHD, not the acute presentation described.
*Activated recipient T cells*
- In an allogeneic transplant, the recipient's immune system is usually heavily suppressed beforehand to prevent host-versus-graft rejection.
- If recipient T cells were active, they would primarily cause **rejection of the donor stem cells** (graft rejection), not the systemic symptoms of GVHD, which is a reaction of the donor cells against the host.
*Newly formed anti-HLA antibodies*
- Newly formed antibodies the recipient develops against the donor's HLA antigens would cause graft rejection, a process often delayed but not presenting as the widespread organ damage of acute GVHD.
- These antibodies are part of the host's attempt to reject the foreign graft, not the donor cells attacking the host.
T-cell depleting antibodies US Medical PG Question 3: An investigator is studying the effect of different cytokines on the growth and differentiation of B cells. The investigator isolates a population of B cells from the germinal center of a lymph node. After exposure to a particular cytokine, these B cells begin to produce an antibody that prevents attachment of pathogens to mucous membranes but does not fix complement. Which of the following cytokines is most likely responsible for the observed changes in B-cell function?
- A. Interleukin-5 (Correct Answer)
- B. Interleukin-6
- C. Interleukin-8
- D. Interleukin-2
- E. Interleukin-4
T-cell depleting antibodies Explanation: ***Interleukin-5***
- The antibody described (prevents pathogen attachment to mucous membranes, does not fix complement) is characteristic of **IgA**.
- **IL-5** plays a crucial role in promoting **IgA secretion** by differentiated B cells and supports B cell growth and differentiation in mucosal immunity.
- IL-5 works synergistically with **TGF-β** (the primary cytokine for IgA class switching) to enhance IgA production, particularly in mucosal-associated lymphoid tissue.
- Among the options provided, **IL-5 has the strongest association with IgA production**.
*Interleukin-4*
- **IL-4** is the primary cytokine driving class switching to **IgE** (and IgG4), not IgA.
- IL-4 is central to **allergic responses** and type 2 immunity, promoting B cells to produce IgE antibodies against allergens and parasites.
- It does not play a significant role in IgA production or mucosal immunity.
*Interleukin-6*
- **IL-6** is a pleiotropic cytokine involved in acute phase reactions, inflammation, and promoting B cell **differentiation into plasma cells**.
- While it supports general B cell maturation and antibody secretion, it is not specifically associated with **IgA production** or class switching.
*Interleukin-8*
- **IL-8** (CXCL8) is a **chemokine** that primarily recruits and activates neutrophils during inflammation.
- It has no direct role in B cell class switching or antibody production.
*Interleukin-2*
- **IL-2** is essential for T cell proliferation and differentiation, enhancing **cell-mediated immunity**.
- While it can indirectly affect B cell responses through T cell help, it is not directly responsible for promoting **IgA production** or class switching.
T-cell depleting antibodies US Medical PG Question 4: A researcher is studying the circulating factors that are released when immune cells are exposed to antigens. Specifically, she is studying a population of CD2+ cells that have been activated acutely. In order to determine which factors are secreted by these cells, she cultures the cells in media and collects the used media from these plates after several days. She then purifies a small factor from this media and uses it to stimulate various immune cell types. She finds that this factor primarily seems to increase the growth and prolong the survival of other CD2+ cells. Which of the following is most likely the factor that was purified by this researcher?
- A. Interleukin-2 (Correct Answer)
- B. Interleukin-3
- C. Interleukin-4
- D. Interleukin-5
- E. Interleukin-1
T-cell depleting antibodies Explanation: ***Interleukin-2***
- **Interleukin-2 (IL-2)** is a crucial cytokine for the **growth**, **proliferation**, and **survival** of T lymphocytes, which are CD2+ cells.
- Activated T cells, like the acute CD2+ cells in the scenario, are a primary source of IL-2, and IL-2 acts in an **autocrine** and **paracrine** fashion to stimulate other T cells.
*Interleukin-3*
- **Interleukin-3 (IL-3)** primarily stimulates the growth and differentiation of **hematopoietic stem cells** and progenitors, not specifically mature CD2+ cells.
- It plays a role in the development of various myeloid cell lineages and mast cells, and its main effect is not confined to T cells.
*Interleukin-4*
- **Interleukin-4 (IL-4)** is critical for the differentiation of naive T helper cells into **Th2 cells** and is a key cytokine for **B cell proliferation** and **antibody class switching** to IgE.
- While it has immunomodulatory effects on T cells, its primary role is not in promoting the generalized growth and survival of other CD2+ cells.
*Interleukin-5*
- **Interleukin-5 (IL-5)** is predominantly involved in the growth, differentiation, and activation of **eosinophils**.
- It also plays a role in B cell growth and IgA production, but its effects are not primarily on universal CD2+ cell growth and survival.
*Interleukin-1*
- **Interleukin-1 (IL-1)** is a **pro-inflammatory cytokine** produced by macrophages, monocytes, and other immune cells in response to infection or injury.
- It primarily mediates **acute phase responses**, fever, and activates endothelial cells, but its main function is not to promote the growth and survival of T lymphocytes.
T-cell depleting antibodies US Medical PG Question 5: A 61-year-old man presents to the emergency department with new-onset dizziness. He reports associated symptoms of confusion, headaches, and loss of coordination. The patient’s wife also mentions he has had recent frequent nosebleeds. Physical examination demonstrates a double vision. Routine blood work is significant for a slightly reduced platelet count. A noncontrast CT of the head is normal. A serum protein electrophoresis is performed and shows an elevated IgM spike. The consulting hematologist strongly suspects Waldenström’s macroglobulinemia. Which of the following is the best course of treatment for this patient?
- A. Plasmapheresis (Correct Answer)
- B. Vincristine
- C. Cyclophosphamide
- D. Rituximab
- E. Prednisone
T-cell depleting antibodies Explanation: ***Plasmapheresis***
- This patient presents with symptoms of **hyperviscosity syndrome** (dizziness, confusion, headaches, loss of coordination, double vision, nosebleeds) due to high levels of IgM, which is characteristic of Waldenström's macroglobulinemia.
- **Plasmapheresis** is the most effective initial treatment to rapidly reduce the IgM level and relieve these acute neurological and hemorrhagic symptoms by removing the excess globulins from the plasma.
*Vincristine*
- **Vincristine** is a chemotherapy agent used in the treatment of Waldenström's macroglobulinemia, but it is typically used as part of a multi-drug regimen for long-term disease control, not for acute management of hyperviscosity.
- Its mechanism involves inhibiting microtubule formation, which is a slower process and would not provide immediate relief for the crisis.
*Cyclophosphamide*
- **Cyclophosphamide** is an alkylating agent, often part of chemotherapy regimens for Waldenström's macroglobulinemia, especially for long-term disease control to reduce IgM production.
- Like vincristine, it works by damaging DNA in cancer cells, a process that is too slow to address the immediate, life-threatening symptoms of hyperviscosity syndrome.
*Rituximab*
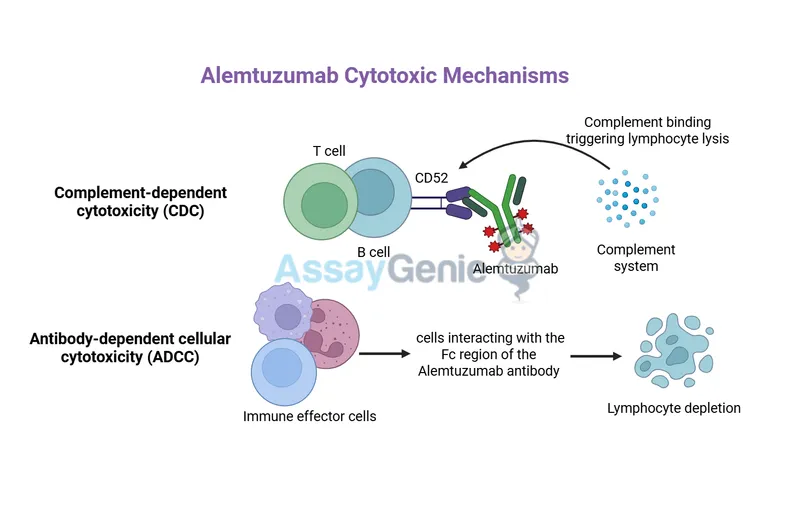
- **Rituximab** is an anti-CD20 monoclonal antibody that targets B-cells, often used in Waldenström's macroglobulinemia to reduce the malignant B-cell clone and subsequent IgM production.
- While effective for disease control, its therapeutic effects take weeks to materialize and would not provide rapid relief for acute hyperviscosity.
*Prednisone*
- **Prednisone** is a corticosteroid that can be used in some hematologic malignancies to reduce inflammation or induce apoptosis in certain cell types.
- However, in Waldenström's macroglobulinemia, corticosteroids alone are not effective in rapidly reducing the large IgM burden causing hyperviscosity, and their role is often supportive or part of combination chemotherapy.
T-cell depleting antibodies US Medical PG Question 6: A 35-year-old woman is admitted to the medical unit for worsening renal failure. Prior to admission, she was seen by her rheumatologist for a follow-up visit and was found to have significant proteinuria and hematuria on urinalysis and an elevated serum creatinine. She reports feeling ill and has noticed blood in her urine. She was diagnosed with systemic lupus erythematosus at the age of 22, and she is currently being treated with ibuprofen for joint pain and prednisone for acute flare-ups. Her blood pressure is 165/105 mmHg. Laboratory testing is remarkable for hypocomplementemia and an elevated anti-DNA antibody. A renal biopsy is performed, which demonstrates 65% glomerular involvement along with the affected glomeruli demonstrating endocapillary and extracapillary glomerulonephritis. In addition to glucocorticoid therapy, the medical team will add mycophenolate mofetil to her treatment regimen. Which of the following is the mechanism of action of mycophenolate mofetil?
- A. Interleukin-2 receptor complex inhibitor
- B. Inosine monophosphate dehydrogenase inhibitor (Correct Answer)
- C. mTOR inhibitor via FKBP binding
- D. Calcineurin inhibitor via cyclophilin binding
- E. T-cell proliferation inhibitor
T-cell depleting antibodies Explanation: ***Inosine monophosphate dehydrogenase inhibitor***
- **Mycophenolate mofetil** (MMF) is a prodrug that inhibits **inosine monophosphate dehydrogenase (IMPDH)**, an enzyme essential for *de novo* purine synthesis.
- This inhibition selectively blocks the proliferation of **T and B lymphocytes**, which are highly dependent on the *de novo* pathway for purine synthesis, thus suppressing the immune response in conditions like lupus nephritis.
*Interleukin-2 receptor complex inhibitor*
- This mechanism describes drugs like **basiliximab** and **daclizumab**, which are monoclonal antibodies that block the **IL-2 receptor** on T cells, preventing their activation and proliferation.
- These agents are primarily used in **transplantation** to prevent acute rejection, not typically for lupus nephritis.
*mTOR inhibitor via FKBP binding*
- This mechanism belongs to drugs like **sirolimus** (rapamycin) and everolimus, which bind to **FK-binding protein (FKBP)** and then inhibit **mammalian target of rapamycin (mTOR)**.
- While these drugs have immunosuppressive properties and are used in transplantation, they are not the primary mechanism of action for mycophenolate mofetil.
*Calcineurin inhibitor via cyclophilin binding*
- This mechanism describes drugs like **cyclosporine**, which binds to **cyclophilin** and then inhibits **calcineurin**, preventing the dephosphorylation of NFAT (nuclear factor of activated T-cells) and subsequent IL-2 transcription.
- **Tacrolimus** also acts as a calcineurin inhibitor but binds to FKBP. These drugs are used in transplantation and some autoimmune diseases but are not how MMF works.
*T-cell proliferation inhibitor*
- While MMF *does* inhibit T-cell proliferation, this description is a general outcome of many immunosuppressants and not its specific molecular mechanism of action.
- Many drugs can inhibit T-cell proliferation through different pathways, so a more precise description of MMF's action is its inhibition of **IMPDH**.
T-cell depleting antibodies US Medical PG Question 7: A 6-year-old boy is brought to the physician because of headache, cough, runny nose, and a low-grade fever since waking up that morning. He has been healthy except for a urinary tract infection one week ago that has resolved with trimethoprim-sulfamethoxazole therapy. Both parents have a history of allergic rhinitis. His temperature is 37.8°C (100°F). Physical exam shows rhinorrhea and tenderness over the frontal and maxillary sinuses. There is cervical lymphadenopathy. Laboratory studies show:
Hemoglobin 14.2 g/dL
Leukocyte count 2,700/mm3
Segmented neutrophils 30%
Bands 1%
Eosinophils 4%
Basophils 0%
Lymphocytes 56%
Monocytes 9%
Platelet count 155,000/mm3
Which of the following is the most likely underlying cause of this patient's symptoms?
- A. CMV infection
- B. EBV infection
- C. Acute lymphocytic leukemia
- D. Medication side effect (Correct Answer)
- E. Acute myelogenous leukemia
T-cell depleting antibodies Explanation: ***Medication side effect***
- The patient's recent **trimethoprim-sulfamethoxazole (TMP-SMX)** treatment and current **leukopenia** (WBC 2,700/mm³, normal 5,000-10,000/mm³) with **neutropenia** (absolute neutrophil count ~840/mm³) strongly suggest **drug-induced bone marrow suppression**.
- TMP-SMX is a folate antagonist known to cause dose-dependent bone marrow suppression, particularly affecting neutrophils and occasionally platelets. The platelet count (155,000/mm³) is at the lower limit of normal, which may represent early marrow effect.
- While the patient's current symptoms (rhinorrhea, cough, sinus tenderness, low-grade fever) suggest an **acute viral upper respiratory infection**, the question asks for the "most likely underlying cause." The **leukopenia with neutropenia** is the most significant abnormal finding and represents the drug effect that predisposes to or complicates infections.
- The combination of recent antibiotic exposure and cytopenias makes medication side effect the primary diagnosis.
*CMV infection*
- CMV can cause **leukopenia**, but typically presents with more prominent constitutional symptoms including prolonged fever, malaise, hepatosplenomegaly, and atypical lymphocytosis.
- The acute onset of URI symptoms and temporal relationship to antibiotic use makes drug-induced marrow suppression more likely.
*EBV infection*
- EBV (infectious mononucleosis) characteristically causes **lymphocytosis with atypical lymphocytes**, not leukopenia.
- Classic features include **pharyngitis**, **posterior cervical lymphadenopathy**, **splenomegaly**, and fatigue, which are not present here.
- The lymphocyte percentage (56%) is within normal range for age, not elevated.
*Acute lymphocytic leukemia*
- **ALL** would present with more severe constitutional symptoms (high fever, bone pain, significant fatigue) and typically shows **circulating blasts** on peripheral smear.
- The cytopenias in ALL are usually more profound (severe anemia, marked thrombocytopenia <50,000/mm³).
- The absence of blasts in the differential and relatively preserved hemoglobin (14.2 g/dL) argue against leukemia.
*Acute myelogenous leukemia*
- **AML** presents with severe symptoms including fatigue, bleeding diathesis, and recurrent infections.
- Peripheral smear typically shows **myeloblasts** with Auer rods in some cases.
- The patient's mild symptoms, absence of blasts, and normal hemoglobin make AML highly unlikely.
T-cell depleting antibodies US Medical PG Question 8: A 47-year-old woman presents to the physician with complaints of fatigue accompanied by symmetric pain, swelling, and stiffness in her wrists, fingers, knees, and other joints. She describes the stiffness as being particularly severe upon awakening, but gradually improves as she moves throughout her day. Her physician initially suggests that she take NSAIDs. However, after a few months of minimal symptomatic improvement, she is prescribed an immunosuppressive drug that has a mechanism of preventing IL-2 transcription. What is the main toxicity that the patient must be aware of with this particular class of drugs?
- A. Pancytopenia
- B. Osteoporosis
- C. Hepatotoxicity
- D. Nephrotoxicity (Correct Answer)
- E. Hyperglycemia
T-cell depleting antibodies Explanation: ***Nephrotoxicity***
- The drug described, which prevents **IL-2 transcription**, is likely a **calcineurin inhibitor** like cyclosporine or tacrolimus, often used in autoimmune diseases.
- **Nephrotoxicity** (kidney damage) is a major dose-limiting toxicity of calcineurin inhibitors, causing both acute and chronic kidney injury.
*Pancytopenia*
- While some immunosuppressants can cause **pancytopenia** (e.g., azathioprine, methotrexate), it is not the classic or primary toxicity associated with calcineurin inhibitors.
- Calcineurin inhibitors primarily affect **renal function** and can cause other side effects like hypertension or neurotoxicity.
*Osteoporosis*
- **Osteoporosis** is a known side effect of long-term glucocorticoid use, but not typically a primary toxicity of calcineurin inhibitors.
- Glucocorticoids reduce bone formation and increase bone resorption, leading to bone density loss.
*Hepatotoxicity*
- **Hepatotoxicity** (liver damage) can occur with various immunosuppressants, such as methotrexate, but it is not the most prominent or defining toxicity for calcineurin inhibitors.
- While cyclosporine can cause some liver enzyme elevation, **nephrotoxicity** is far more common and severe.
*Hyperglycemia*
- **Hyperglycemia** can be a side effect of some immunosuppressants, particularly **glucocorticoids** and **tacrolimus** (another calcineurin inhibitor).
- However, for the class of drugs that prevent IL-2 transcription (calcineurin inhibitors), **nephrotoxicity** remains the most significant and common major toxicity to be aware of.
T-cell depleting antibodies US Medical PG Question 9: A 68-year-old man is brought to the emergency department 25 minutes after he was found shaking violently on the bathroom floor. His wife reports that he has become increasingly confused over the past 2 days and that he has been sleeping more than usual. He was started on chemotherapy 4 months ago for chronic lymphocytic leukemia. He is confused and oriented to person only. Neurological examination shows right-sided ptosis and diffuse hyperreflexia. An MRI of the brain shows disseminated, nonenhancing white matter lesions with no mass effect. A polymerase chain reaction assay of the cerebrospinal fluid confirms infection with a virus that has double-stranded, circular DNA. An antineoplastic drug with which of the following mechanisms of action is most likely responsible for this patient's current condition?
- A. Monoclonal antibody against CD20+ (Correct Answer)
- B. Monoclonal antibody against EGFR
- C. Tyrosine kinase inhibitor
- D. Topoisomerase II inhibitor
- E. Free radical formation
T-cell depleting antibodies Explanation: **Monoclonal antibody against CD20+**
- The patient's presentation with **progressive multifocal leukoencephalopathy (PML)**, characterized by neurological deficits, white matter lesions, and a positive PCR for a **double-stranded, circular DNA virus (JC virus)**, strongly suggests a compromised immune system, likely due to chronic lymphocytic leukemia (CLL) treatment.
- **Rituximab**, a monoclonal antibody that targets **CD20+ B-lymphocytes**, is a common treatment for CLL and is associated with an increased risk of PML due to its immunosuppressive effects.
*Monoclonal antibody against EGFR*
- **Epidermal growth factor receptor (EGFR) inhibitors** (e.g., cetuximab, erlotinib) are used in various cancers but are not typically associated with the development of PML.
- Side effects of EGFR inhibitors commonly include skin rashes, diarrhea, and stomatitis, not the neurological symptoms seen here.
*Tyrosine kinase inhibitor*
- **Tyrosine kinase inhibitors (TKIs)**, such as imatinib or ibrutinib, are used in certain leukemias and other cancers.
- While TKIs can have various side effects, they are not primarily known for causing B-cell depletion or an increased risk of PML like rituximab.
*Topoisomerase II inhibitor*
- **Topoisomerase II inhibitors** (e.g., etoposide, doxorubicin) are chemotherapy agents that induce DNA damage.
- Their primary toxicities include myelosuppression, cardiotoxicity (for anthracyclines), and secondary malignancies, not opportunistic viral infections like PML.
*Free radical formation*
- **Free radical formation** is a mechanism of action for certain chemotherapeutic agents like **bleomycin** or **anthracyclines**, which cause DNA damage.
- While these drugs have significant side effects, they are not typically linked to the selective immunosuppression that leads to PML in the context of CLL treatment.
T-cell depleting antibodies US Medical PG Question 10: An otherwise healthy 13-year-old boy is brought to the physician because of asthma attacks that have been increasing in frequency and severity over the past 4 weeks. He was first diagnosed with asthma 6 months ago. Current medications include high-dose inhaled fluticasone and salmeterol daily, with additional albuterol as needed. He has required several courses of oral corticosteroids. A medication is added to his therapy regimen that results in downregulation of the high-affinity IgE receptor (FcεRI) on mast cells and basophils. Which of the following drugs was most likely added to the patient's medication regimen?
- A. Infliximab
- B. Theophylline
- C. Zileuton
- D. Nedocromil
- E. Omalizumab (Correct Answer)
T-cell depleting antibodies Explanation: ***Omalizumab***
- **Omalizumab** is a **monoclonal antibody** that targets and binds to free IgE, preventing its binding to **FcεRI receptors** on mast cells and basophils.
- By reducing free IgE, it leads to a **downregulation of FcεRI receptors**, thereby decreasing mediator release and reducing asthma symptoms in severe, persistent asthma.
*Infliximab*
- **Infliximab** is an **anti-TNF-α monoclonal antibody** used primarily in inflammatory conditions like **rheumatoid arthritis**, **Crohn's disease**, and **ankylosing spondylitis**.
- It does not directly affect IgE or its receptors, thus it is not indicated for the treatment of **asthma**.
*Theophylline*
- **Theophylline** is a **phosphodiesterase inhibitor** that causes bronchodilation by increasing intracellular cAMP.
- It does not modulate IgE or its receptors, and its use is limited by a narrow **therapeutic index** and potential for side effects.
*Zileuton*
- **Zileuton** is a **5-lipoxygenase inhibitor** that blocks the synthesis of **leukotrienes**, potent bronchoconstrictors and inflammatory mediators in asthma.
- While effective in some asthma patients, it does not act on IgE or its receptors.
*Nedocromil*
- **Nedocromil** is a **mast cell stabilizer** that inhibits the release of inflammatory mediators from mast cells.
- It does not directly impact IgE levels or the expression of **FcεRI receptors** on mast cells and basophils, making it less suitable for severe, refractory asthma requiring IgE-pathway modulation.
More T-cell depleting antibodies US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.