Costimulation blockers US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Costimulation blockers. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Costimulation blockers US Medical PG Question 1: An investigator is conducting a study to identify potential risk factors for post-transplant hypertension. The investigator selects post-transplant patients with hypertension and gathers detailed information regarding their age, gender, preoperative blood pressure readings, and current medications. The results of the study reveal that some of the patients had been treated with cyclosporine. This study is best described as which of the following?
- A. Cross-sectional study
- B. Retrospective cohort study
- C. Prospective cohort study
- D. Case series
- E. Case-control study (Correct Answer)
Costimulation blockers Explanation: ***Case-control study***
- A **case-control study** compares individuals with a disease (cases) to individuals without the disease (controls) to identify risk factors retrospectively.
- In this study, the investigator selects post-transplant patients **with hypertension** (the cases) and looks backward at their exposures, including cyclosporine use, to identify potential risk factors.
- The analytical goal of "identifying risk factors" and the observation that **some patients had been treated with cyclosporine** (implying comparison with those who were not) indicates a case-control design.
- Even if controls are not explicitly mentioned, the study design involves analyzing exposure patterns among cases to identify associations with risk factors.
*Case series*
- A **case series** is purely descriptive and involves collecting detailed information on a group of patients with a common condition without any comparison or analytical hypothesis testing.
- While this study does describe patients with post-transplant hypertension, the key difference is the **analytical intent** to identify risk factors, which goes beyond simple description.
- A true case series would simply report clinical characteristics without attempting to establish associations between exposures and outcomes.
*Cross-sectional study*
- A **cross-sectional study** assesses both exposure and outcome simultaneously at a single point in time to determine prevalence.
- This approach would involve surveying a population of post-transplant patients to determine the prevalence of hypertension and associated factors at that moment.
- The study described has already selected patients with the outcome (hypertension), making it retrospective rather than cross-sectional.
*Retrospective cohort study*
- A **retrospective cohort study** examines past data by first classifying patients based on **exposure status** (e.g., cyclosporine use vs. no cyclosporine), then following them forward in time to see who developed the outcome.
- The key difference is that cohort studies **start with exposure** and move to outcome, whereas this study **starts with outcome** (hypertension) and looks back at exposures.
- If the investigator had selected all transplant patients, divided them by cyclosporine exposure, and then determined hypertension rates in each group, it would be a retrospective cohort study.
*Prospective cohort study*
- A **prospective cohort study** identifies a cohort at baseline (before the outcome) and follows them forward in time to observe who develops the outcome.
- This study has already selected patients **with the outcome present**, making it retrospective rather than prospective.
- A prospective design would require identifying transplant patients at the time of transplant and following them over time to see who develops hypertension.
Costimulation blockers US Medical PG Question 2: A 35-year-old woman is admitted to the medical unit for worsening renal failure. Prior to admission, she was seen by her rheumatologist for a follow-up visit and was found to have significant proteinuria and hematuria on urinalysis and an elevated serum creatinine. She reports feeling ill and has noticed blood in her urine. She was diagnosed with systemic lupus erythematosus at the age of 22, and she is currently being treated with ibuprofen for joint pain and prednisone for acute flare-ups. Her blood pressure is 165/105 mmHg. Laboratory testing is remarkable for hypocomplementemia and an elevated anti-DNA antibody. A renal biopsy is performed, which demonstrates 65% glomerular involvement along with the affected glomeruli demonstrating endocapillary and extracapillary glomerulonephritis. In addition to glucocorticoid therapy, the medical team will add mycophenolate mofetil to her treatment regimen. Which of the following is the mechanism of action of mycophenolate mofetil?
- A. Interleukin-2 receptor complex inhibitor
- B. Inosine monophosphate dehydrogenase inhibitor (Correct Answer)
- C. mTOR inhibitor via FKBP binding
- D. Calcineurin inhibitor via cyclophilin binding
- E. T-cell proliferation inhibitor
Costimulation blockers Explanation: ***Inosine monophosphate dehydrogenase inhibitor***
- **Mycophenolate mofetil** (MMF) is a prodrug that inhibits **inosine monophosphate dehydrogenase (IMPDH)**, an enzyme essential for *de novo* purine synthesis.
- This inhibition selectively blocks the proliferation of **T and B lymphocytes**, which are highly dependent on the *de novo* pathway for purine synthesis, thus suppressing the immune response in conditions like lupus nephritis.
*Interleukin-2 receptor complex inhibitor*
- This mechanism describes drugs like **basiliximab** and **daclizumab**, which are monoclonal antibodies that block the **IL-2 receptor** on T cells, preventing their activation and proliferation.
- These agents are primarily used in **transplantation** to prevent acute rejection, not typically for lupus nephritis.
*mTOR inhibitor via FKBP binding*
- This mechanism belongs to drugs like **sirolimus** (rapamycin) and everolimus, which bind to **FK-binding protein (FKBP)** and then inhibit **mammalian target of rapamycin (mTOR)**.
- While these drugs have immunosuppressive properties and are used in transplantation, they are not the primary mechanism of action for mycophenolate mofetil.
*Calcineurin inhibitor via cyclophilin binding*
- This mechanism describes drugs like **cyclosporine**, which binds to **cyclophilin** and then inhibits **calcineurin**, preventing the dephosphorylation of NFAT (nuclear factor of activated T-cells) and subsequent IL-2 transcription.
- **Tacrolimus** also acts as a calcineurin inhibitor but binds to FKBP. These drugs are used in transplantation and some autoimmune diseases but are not how MMF works.
*T-cell proliferation inhibitor*
- While MMF *does* inhibit T-cell proliferation, this description is a general outcome of many immunosuppressants and not its specific molecular mechanism of action.
- Many drugs can inhibit T-cell proliferation through different pathways, so a more precise description of MMF's action is its inhibition of **IMPDH**.
Costimulation blockers US Medical PG Question 3: A 47-year-old woman presents to the physician with complaints of fatigue accompanied by symmetric pain, swelling, and stiffness in her wrists, fingers, knees, and other joints. She describes the stiffness as being particularly severe upon awakening, but gradually improves as she moves throughout her day. Her physician initially suggests that she take NSAIDs. However, after a few months of minimal symptomatic improvement, she is prescribed an immunosuppressive drug that has a mechanism of preventing IL-2 transcription. What is the main toxicity that the patient must be aware of with this particular class of drugs?
- A. Pancytopenia
- B. Osteoporosis
- C. Hepatotoxicity
- D. Nephrotoxicity (Correct Answer)
- E. Hyperglycemia
Costimulation blockers Explanation: ***Nephrotoxicity***
- The drug described, which prevents **IL-2 transcription**, is likely a **calcineurin inhibitor** like cyclosporine or tacrolimus, often used in autoimmune diseases.
- **Nephrotoxicity** (kidney damage) is a major dose-limiting toxicity of calcineurin inhibitors, causing both acute and chronic kidney injury.
*Pancytopenia*
- While some immunosuppressants can cause **pancytopenia** (e.g., azathioprine, methotrexate), it is not the classic or primary toxicity associated with calcineurin inhibitors.
- Calcineurin inhibitors primarily affect **renal function** and can cause other side effects like hypertension or neurotoxicity.
*Osteoporosis*
- **Osteoporosis** is a known side effect of long-term glucocorticoid use, but not typically a primary toxicity of calcineurin inhibitors.
- Glucocorticoids reduce bone formation and increase bone resorption, leading to bone density loss.
*Hepatotoxicity*
- **Hepatotoxicity** (liver damage) can occur with various immunosuppressants, such as methotrexate, but it is not the most prominent or defining toxicity for calcineurin inhibitors.
- While cyclosporine can cause some liver enzyme elevation, **nephrotoxicity** is far more common and severe.
*Hyperglycemia*
- **Hyperglycemia** can be a side effect of some immunosuppressants, particularly **glucocorticoids** and **tacrolimus** (another calcineurin inhibitor).
- However, for the class of drugs that prevent IL-2 transcription (calcineurin inhibitors), **nephrotoxicity** remains the most significant and common major toxicity to be aware of.
Costimulation blockers US Medical PG Question 4: A 14-year-old boy has undergone kidney transplantation due to stage V chronic kidney disease. A pre-transplantation serologic assessment showed that he is negative for past or present HIV infection, viral hepatitis, EBV, and CMV infection. He has a known allergy for macrolides. The patient has no complaints 1 day after transplantation. His vital signs include: blood pressure 120/70 mm Hg, heart rate 89/min, respiratory rate 17/min, and temperature 37.0°C (98.6°F). On physical examination, the patient appears to be pale, his lungs are clear on auscultation, heart sounds are normal, and his abdomen is non-tender on palpation. His creatinine is 0.65 mg/dL (57.5 µmol/L), GFR is 71.3 mL/min/1.73 m2, and urine output is 0.9 mL/kg/h. Which of the following drugs should be used in the immunosuppressive regimen in this patient?
- A. Belatacept
- B. Sirolimus
- C. Omalizumab
- D. Daclizumab
- E. Basiliximab (Correct Answer)
Costimulation blockers Explanation: **Basiliximab**
- **Basiliximab** is a **monoclonal antibody** that targets the **IL-2 receptor (CD25)** on activated T cells, preventing their proliferation and inducing immunosuppression.
- It is commonly used as **induction therapy** in kidney transplant recipients due to its good safety profile, especially in pediatric patients, without the nephrotoxicity associated with calcineurin inhibitors, minimizing acute rejection risks immediately post-transplant.
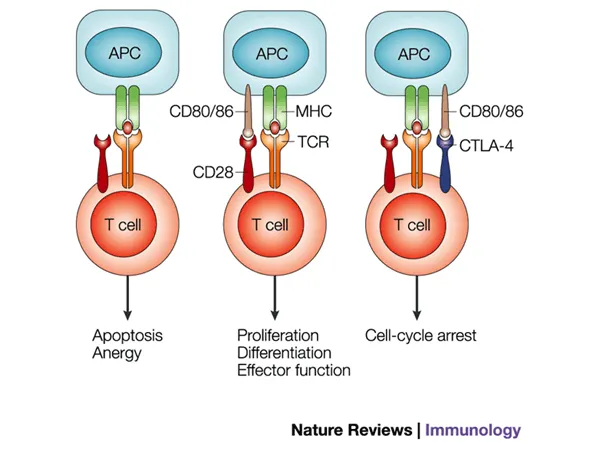
*Belatacept*
- **Belatacept** works by co-stimulation blockade, binding to **CD80 and CD86** on antigen-presenting cells to prevent T-cell activation.
- It is typically reserved for patients who cannot tolerate calcineurin inhibitors due to **nephrotoxicity** or require a steroid-sparing regimen, which is not indicated as an immediate need in this patient.
*Sirolimus*
- **Sirolimus** is an **mTOR inhibitor** that works by blocking T-cell proliferation and B-cell differentiation.
- It is associated with several side effects, including **delayed wound healing**, **thrombocytopenia**, and **hyperlipidemia**, which are undesirable in the immediate post-transplant period, especially in a growing adolescent.
*Omalizumab*
- **Omalizumab** is an **anti-IgE monoclonal antibody** primarily used for allergic asthma and chronic spontaneous urticaria.
- It has no role in **immunosuppression for organ transplantation** as its mechanism of action is unrelated to preventing graft rejection.
*Daclizumab*
- **Daclizumab** is another **monoclonal antibody** that also targets the **IL-2 receptor (CD25)**, similar to basiliximab.
- However, daclizumab has been **withdrawn from the market** due to serious adverse effects including severe liver injury and autoimmune encephalitis, making it unavailable for clinical use in transplantation.
Costimulation blockers US Medical PG Question 5: The patient is admitted to the hospital. A stereotactic brain biopsy of the suspicious lesion is performed that shows many large lymphocytes with irregular nuclei. Which of the following is the most appropriate treatment?
- A. Methotrexate (Correct Answer)
- B. Pyrimethamine and sulfadiazine
- C. Intrathecal glucocorticoids
- D. Surgical resection
- E. Temozolomide
Costimulation blockers Explanation: ***Methotrexate***
- A brain biopsy showing **large lymphocytes with irregular nuclei** is highly suggestive of **primary central nervous system lymphoma (PCNSL)**. High-dose methotrexate is the cornerstone of PCNSL treatment due to its ability to cross the **blood-brain barrier** effectively.
- Methotrexate is a **folate antagonist** that inhibits DNA synthesis, making it effective against rapidly dividing cancer cells, including lymphoma cells in the brain.
*Pyrimethamine and sulfadiazine*
- This combination is the standard treatment for **cerebral toxoplasmosis**, an opportunistic infection often seen in immunocompromised patients, which can present as a brain lesion.
- However, the biopsy finding of **lymphoma cells** rules out toxoplasmosis as the primary diagnosis, making this treatment inappropriate.
*Intrathecal glucocorticoids*
- **Glucocorticoids** can be used to reduce **peritumoral edema** and provide symptomatic relief in PCNSL, but they are not a definitive treatment for the lymphoma itself.
- While sometimes used as an adjunct, high-dose glucocorticoids can induce **lymphoma cell apoptosis**, potentially confounding diagnostic biopsy results if administered before the biopsy.
*Surgical resection*
- **Gross total resection** is generally not feasible or recommended for PCNSL because these tumors tend to be multifocal and deeply infiltrating, making complete removal difficult and often associated with significant neurological morbidity.
- The primary treatment for PCNSL is **chemotherapy** (especially high-dose methotrexate) and sometimes radiation, rather than surgery.
*Temozolomide*
- **Temozolomide** is an **oral alkylating agent** primarily used in the treatment of **glioblastoma multiforme** and anaplastic astrocytoma, as well as other high-grade gliomas.
- While it can cross the blood-brain barrier, it is not the primary or most effective chemotherapy for PCNSL, which responds better to methotrexate-based regimens.
Costimulation blockers US Medical PG Question 6: A 68-year-old woman comes to the physician for a follow-up examination. Three months ago, she underwent heart transplantation for restrictive cardiomyopathy and was started on transplant rejection prophylaxis. Her pulse is 76/min and blood pressure is 148/82 mm Hg. Physical examination shows enlargement of the gum tissue. There is a well-healed scar on her chest. Serum studies show hyperlipidemia. The physician recommends removing a drug that decreases T cell activation by inhibiting the transcription of interleukin-2 from the patient's treatment regimen and replacing it with a different medication. Which of the following drugs is the most likely cause of the adverse effects seen in this patient?
- A. Mycophenolate mofetil
- B. Azathioprine
- C. Tacrolimus
- D. Cyclosporine (Correct Answer)
- E. Prednisolone
Costimulation blockers Explanation: ***Cyclosporine***
- The patient's symptoms of **gingival hyperplasia**, **hypertension**, and **hyperlipidemia** are classic side effects associated with cyclosporine.
- Cyclosporine is a calcineurin inhibitor that **decreases T-cell activation** by inhibiting IL-2 transcription, matching the drug description.
*Mycophenolate mofetil*
- Mycophenolate mofetil is an **antiproliferative agent** that inhibits purine synthesis, primarily affecting lymphocytes.
- Its common side effects are mainly **hematologic** (leukopenia, anemia) and **gastrointestinal** (diarrhea, nausea), not gingival hyperplasia or hypertension.
*Azathioprine*
- Azathioprine is a **purine analog** that impairs DNA synthesis and inhibits lymphocyte proliferation.
- Key side effects include **myelosuppression** (leukopenia, thrombocytopenia) and **hepatotoxicity**, which are not present here.
*Tacrolimus*
- Tacrolimus is also a **calcineurin inhibitor** that inhibits IL-2 transcription, similar to cyclosporine.
- While it can cause **hypertension** and **hyperlipidemia**, it is less commonly associated with **gingival hyperplasia** than cyclosporine.
*Prednisolone*
- Prednisolone is a **corticosteroid** used for immunosuppression, acting broadly on the immune system.
- Common side effects include **hyperglycemia**, **osteoporosis**, and **cataracts**, not specific gingival overgrowth.
Costimulation blockers US Medical PG Question 7: An HIV-positive patient with a CD4+ count of 45 is receiving recommended first-line treatment for a case of cytomegalovirus retinitis. Coadministration with which of the following agents would be most likely to precipitate a deficiency of neutrophils in this patient?
- A. Ritonavir
- B. Raltegravir
- C. Foscarnet
- D. Efavirenz
- E. Zidovudine (Correct Answer)
Costimulation blockers Explanation: ***Zidovudine***
- **Zidovudine (AZT)** is a nucleoside reverse transcriptase inhibitor (NRTI) that is well-known for causing **myelosuppression**, particularly **neutropenia** and **anemia**.
- In an HIV-positive patient with a low **CD4+ count** and concurrent treatment for **CMV retinitis** (which often involves drugs like ganciclovir that can also cause myelosuppression), adding zidovudine significantly increases the risk of severe neutropenia.
*Ritonavir*
- **Ritonavir** is a protease inhibitor primarily known for its role as a **pharmacokinetic booster** in HIV therapy, enhancing the levels of other antiretrovirals.
- While it can cause gastrointestinal side effects and hepatotoxicity, **myelosuppression** and specifically neutropenia are not its primary or common adverse effects.
*Raltegravir*
- **Raltegravir** is an integrase strand transfer inhibitor (INSTI) generally well-tolerated with a favorable side effect profile.
- Common side effects include headache, nausea, and fatigue, but it is **not typically associated with significant myelosuppression** or neutropenia.
*Foscarnet*
- **Foscarnet** is an antiviral agent used for treating CMV retinitis, particularly in cases of ganciclovir resistance.
- Its major dose-limiting toxicities include **nephrotoxicity** and **electrolyte disturbances** (e.g., hypocalcemia, hypomagnesemia), not primarily neutropenia.
*Efavirenz*
- **Efavirenz** is a non-nucleoside reverse transcriptase inhibitor (NNRTI) associated with central nervous system side effects such as dizziness, insomnia, and vivid dreams.
- While skin rash and hepatotoxicity can occur, **bone marrow suppression** leading to neutropenia is not a characteristic or frequent adverse effect of efavirenz.
Costimulation blockers US Medical PG Question 8: A 44-year-old man, with a history of intravenous (IV) drug use, presented to the emergency department due to worsening non-productive cough, exertional dyspnea, and night sweats. His cough started 3 weeks ago and progressively worsened. He is homeless and well-known by the hospital staff. He was previously admitted to the hospital after an overdose of opioids. He takes no medication. At the hospital, the vital signs included: blood pressure 101/68 mm Hg, heart rate 99/min, respiratory rate 20/min, oxygen saturation of 91% on room air, and oral temperature of 37.4°C (99.3°F). His chest X-ray showed left perihilar shadowing. The laboratory results included:
WBC count 8,800/mm3
Arterial pH 7.39
Rapid HIV testing positive with an elevated viral load
PaCO2 41 mm Hg
PaO2 76 mm Hg
He was admitted for the treatment of presumed sepsis and pneumonia, and he was immediately started on IV ceftriaxone. An induced sputum specimen shows multiple kidney bean-shaped cysts that are approximately 5 um. These cysts stain positive with methenamine silver. What is the preferred antibiotic therapeutic regimen for this condition?
- A. Intravenous liposomal amphotericin B with flucytosine
- B. Isoniazid, rifabutin, pyrazinamide and ethambutol
- C. Fluconazole with flucytosine
- D. Trimethoprim-sulfamethoxazole (Correct Answer)
- E. Clindamycin and primaquine, with adjunctive prednisone
Costimulation blockers Explanation: ***Trimethoprim-sulfamethoxazole***
- The patient's symptoms (non-productive cough, dyspnea, night sweats), history of **IV drug use**, positive **HIV** test with elevated viral load, and chest X-ray findings are highly suggestive of **Pneumocystis pneumonia (PcP)**.
- The sputum analysis showing **kidney bean-shaped cysts** approximately 5 µm and staining positive with **methenamine silver** confirms PcP caused by *Pneumocystis jirovecii*. **Trimethoprim-sulfamethoxazole (TMP-SMX)** is the first-line treatment for PcP.
*Intravenous liposomal amphotericin B with flucytosine*
- This regimen is primarily used for severe fungal infections like **cryptococcal meningitis** or disseminated candidiasis, not *Pneumocystis jirovecii* pneumonia.
- While *Pneumocystis* was once considered a fungus, it is now classified as a unique organism requiring specific antiprotozoal-like treatment, not typical antifungal agents.
*Isoniazid, rifabutin, pyrazinamide and ethambutol*
- This is a standard multi-drug regimen for treating **active tuberculosis (TB)**.
- Although TB can cause similar pulmonary symptoms in immunocompromised patients, the sputum microscopy findings of *Pneumocystis* cysts rule out TB as the primary diagnosis requiring this specific regimen.
*Fluconazole with flucytosine*
- **Fluconazole** is an antifungal drug primarily used for candidiasis and cryptococcal infections, but it is **not effective** against *Pneumocystis jirovecii*.
- **Flucytosine** is also an antifungal agent used in combination with amphotericin B for severe fungal infections, but it has no role in treating PcP.
*Clindamycin and primaquine, with adjunctive prednisone*
- This combination is an **alternative treatment regimen** for moderate to severe PcP, often used in patients who cannot tolerate TMP-SMX due to adverse effects.
- While it is a valid treatment option, **TMP-SMX** remains the **preferred first-line therapy** due to its efficacy and broader availability, unless contraindications exist.
Costimulation blockers US Medical PG Question 9: A 50-year-old woman comes to the physician for the evaluation of excessive hair growth on her chin over the past 2 weeks. She also reports progressive enlargement of her gums. Three months ago, she underwent a liver transplantation due to Wilson disease. Following the procedure, the patient was started on transplant rejection prophylaxis. She has a history of poorly-controlled type 2 diabetes mellitus. Temperature is 37°C (98.6°F), pulse is 80/min, respirations are 22/min, and blood pressure is 150/80 mm Hg. Physical examination shows dark-pigmented, coarse hair on the chin, upper lip, and chest. The gingiva and the labial mucosa are swollen. There is a well-healed scar on her right lower abdomen. Which of the following drugs is the most likely cause of this patient's findings?
- A. Daclizumab
- B. Cyclosporine (Correct Answer)
- C. Sirolimus
- D. Methotrexate
- E. Tacrolimus
Costimulation blockers Explanation: **Cyclosporine**
* This patient's **combination of hirsutism** (excessive hair growth) **and gingival hyperplasia** (gum enlargement) is the classic presentation of cyclosporine toxicity, an immunosuppressant commonly used for transplant rejection prophylaxis.
* Cyclosporine is a **calcineurin inhibitor** that prevents T-cell activation and is highly effective in preventing graft rejection.
* The **simultaneous presence of both hirsutism and prominent gingival hyperplasia** is particularly characteristic of cyclosporine.
*Daclizumab*
* **Daclizumab** is a **monoclonal antibody** targeting the IL-2 receptor, which was previously used for transplant prophylaxis but has been discontinued for this indication.
* It is not associated with hirsutism or gingival hyperplasia.
*Sirolimus*
* **Sirolimus** is an **mTOR inhibitor** used as an immunosuppressant, known for side effects like hyperlipidemia, myelosuppression, and delayed wound healing.
* It does **not** typically cause hirsutism or gingival hyperplasia.
*Methotrexate*
* **Methotrexate** is an **antimetabolite** and immunosuppressant commonly used in autoimmune diseases and cancer, with side effects including bone marrow suppression, mucositis, and liver toxicity.
* Hirsutism and gingival hyperplasia are **not** characteristic side effects of methotrexate.
*Tacrolimus*
* **Tacrolimus** is another **calcineurin inhibitor**, similar to cyclosporine, but with a different side effect profile. While tacrolimus can cause hirsutism, **gingival hyperplasia is significantly less common** with tacrolimus compared to cyclosporine.
* The **presence of prominent gingival hyperplasia alongside hirsutism strongly favors cyclosporine** over tacrolimus.
* Tacrolimus is more commonly associated with **neurotoxicity** (e.g., tremor) and **nephrotoxicity**.
Costimulation blockers US Medical PG Question 10: A 38-year-old woman comes to the physician for a follow-up examination. Two years ago, she was diagnosed with multiple sclerosis. Three weeks ago, she was admitted and treated for right lower leg weakness with high-dose methylprednisone for 5 days. She has had 4 exacerbations over the past 6 months. Current medications include interferon beta and a multivitamin. Her temperature is 37°C (98.6°F), pulse is 90/min, and blood pressure is 116/74 mm Hg. Examination shows pallor of the right optic disk. Neurologic examination shows no focal findings. She is anxious about the number of exacerbations and repeated hospitalizations. She is counseled about the second-line treatment options available to her. She consents to treatment with natalizumab. However, she has read online about its adverse effects and is concerned. This patient is at increased risk for which of the following complications?
- A. Tuberculosis
- B. Syndrome of inappropriate antidiuretic hormone
- C. Parkinsonism
- D. Progressive multifocal leukoencephalopathy (Correct Answer)
- E. Aplastic anemia
Costimulation blockers Explanation: ***Progressive multifocal leukoencephalopathy***
- **Natalizumab** is a monoclonal antibody that blocks the binding of leukocytes to endothelial cells, preventing their entry into the central nervous system. This immunosuppressive effect increases the risk of **progressive multifocal leukoencephalopathy (PML)**, especially in patients who are positive for the **JC virus**.
- PML is a serious and often fatal opportunistic infection of the brain caused by the **JC virus**, which demyelinates axons and leads to severe neurological deficits.
*Tuberculosis*
- While some immunosuppressants can reactivate **latent tuberculosis**, natalizumab is not typically associated with an increased risk of TB compared to other immunomodulatory drugs like TNF-alpha inhibitors.
- The mechanism of action of natalizumab (alpha-4 integrin blocker) does not directly impede the immune response responsible for containing mycobacterial infections to the same extent as other treatments.
*Syndrome of inappropriate antidiuretic hormone*
- **SIADH** is not a known adverse effect of natalizumab.
- SIADH is characterized by excessive secretion of **antidiuretic hormone**, leading to hyponatremia, and is often associated with certain medications (e.g., SSRIs, carbamazepine) or underlying conditions like malignancy or pulmonary disease.
*Parkinsonism*
- Parkinsonism involves symptoms like **bradykinesia**, rigidity, and tremor, and is a neurodegenerative disorder.
- There is **no evidence** suggesting a causal link between natalizumab treatment and the development of Parkinsonism.
*Aplastic anemia*
- **Aplastic anemia** is a rare but severe condition where the bone marrow fails to produce blood cells.
- This adverse effect is not associated with natalizumab; it is more commonly linked to certain **chemotherapeutic agents**, radiation, or specific antimicrobial drugs like chloramphenicol.
More Costimulation blockers US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.