Corticosteroids US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Corticosteroids. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Corticosteroids US Medical PG Question 1: A previously healthy 61-year-old man comes to the physician because of bilateral knee pain for the past year. The pain is worse with movement and is relieved with rest. Physical examination shows crepitus, pain, and decreased range of motion with complete flexion and extension of both knees. There is no warmth, redness, or swelling. X-rays of both knees show irregular joint space narrowing, osteophytes, and subchondral cysts. Which of the following is the most appropriate pharmacotherapy?
- A. Allopurinol
- B. Naproxen (Correct Answer)
- C. Celecoxib
- D. Infliximab
- E. Prednisone
Corticosteroids Explanation: ***Naproxen***
- The patient's presentation with **bilateral knee pain worse with movement**, relief with rest, crepitus, and characteristic X-ray findings (joint space narrowing, osteophytes, subchondral cysts) is classic for **osteoarthritis (OA)** [3].
- **NSAIDs** like naproxen are **first-line pharmacotherapy** for managing pain and inflammation in osteoarthritis that is not adequately controlled by acetaminophen or topical agents [1].
- As a **non-selective NSAID**, naproxen is an appropriate initial choice for a patient without specified risk factors for GI complications or cardiovascular disease [2].
*Allopurinol*
- **Allopurinol** is a xanthine oxidase inhibitor used to reduce **urate production in hyperuricemia** and prevent gout attacks.
- The patient's symptoms are not consistent with gout, as there is **no acute inflammatory arthritis, redness, warmth, or swelling**.
*Celecoxib*
- **Celecoxib** is a **COX-2 selective NSAID** that can be used for osteoarthritis pain.
- It is generally preferred in patients with **documented GI risk factors** (history of peptic ulcer, concurrent anticoagulation, or advanced age with other risk factors).
- While this 61-year-old patient has age as a consideration, in the absence of other specified GI risk factors, either non-selective or COX-2 selective NSAIDs are reasonable; **naproxen is acceptable as initial therapy** and is more cost-effective.
*Infliximab*
- **Infliximab** is a **biologic disease-modifying antirheumatic drug (DMARD)**, specifically a TNF-alpha inhibitor, used to treat inflammatory arthritides like rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis.
- It is **not indicated for osteoarthritis**, which is a degenerative joint disease rather than an autoimmune inflammatory process.
*Prednisone*
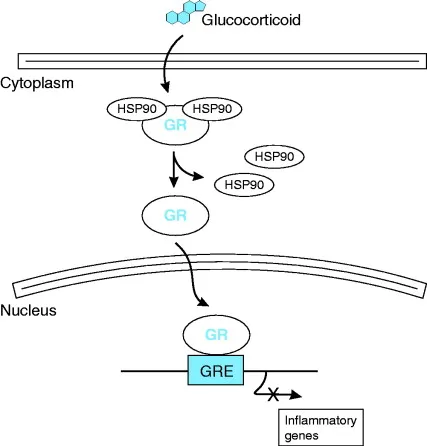
- **Prednisone** is a corticosteroid used to **reduce inflammation** in various conditions, including inflammatory arthritides and acute pain flares.
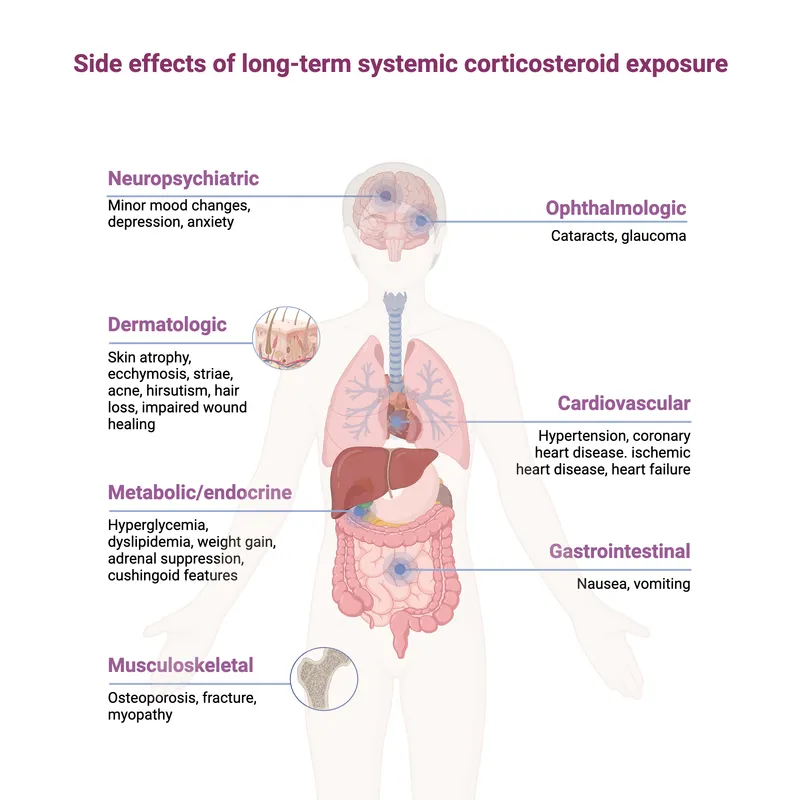
- While it can provide symptomatic relief, it is **not a first-line or long-term pharmacotherapy for osteoarthritis** due to significant **side effects** with chronic use (weight gain, hyperglycemia, osteoporosis, immunosuppression) [1].
Corticosteroids US Medical PG Question 2: A 62-year-old woman is hospitalized for an open reduction of a fracture of her right femur following a motor vehicle accident 2 hours prior. She has had rheumatoid arthritis for 12 years. She was hospitalized 1 month ago for an exacerbation of rheumatoid arthritis. Since then, she has been taking a higher dose of prednisone to control the flare. Her other medications include calcium supplements, methotrexate, and etanercept. She has had appropriate nutrition over the years with regular follow-ups with her healthcare providers. Her vital signs are within normal limits. Cardiovascular examination shows no abnormalities. In order to reduce the risk of post-operative wound failure, which of the following is the most appropriate modification in this patient’s drug regimen?
- A. Replacing prednisone with hydrocortisone
- B. Applying topical vitamin C
- C. Adding zinc supplementation (Correct Answer)
- D. Discontinuing steroids before surgery
- E. Increasing prednisone dose initially and tapering rapidly after 3 days
Corticosteroids Explanation: ***Adding zinc supplementation***
- **Zinc** plays a crucial role in **collagen synthesis**, immune function, and **wound healing**, making supplementation beneficial for reducing post-operative wound failure, especially in patients with chronic inflammatory conditions or those on corticosteroids.
- Chronic inflammation from **rheumatoid arthritis** and long-term **corticosteroid use** can impair zinc absorption and lead to deficiency, which exacerbates wound healing issues.
*Replacing prednisone with hydrocortisone*
- Both **prednisone** and **hydrocortisone** are corticosteroids, and switching between them does not inherently reduce the risk of wound failure.
- While prednisone is converted to prednisolone in the liver, hydrocortisone is directly active; both have similar immunosuppressive and anti-inflammatory effects that can impair wound healing.
*Applying topical vitamin C*
- **Topical vitamin C** is primarily used for its antioxidant properties and role in collagen synthesis in the skin, but its systemic effect on deep surgical wound healing is limited.
- **Systemic vitamin C deficiency** can impair wound healing, but the patient's history of appropriate nutrition suggests this is less likely to be the primary issue.
*Discontinuing steroids before surgery*
- Abruptly discontinuing **prednisone**, especially in a patient on a higher dose for an **RA flare**, carries a high risk of causing an **adrenal crisis**, which is life-threatening.
- Steroids are typically continued at a stress-dose equivalent during surgery to prevent **adrenal insufficiency**, not discontinued.
*Increasing prednisone dose initially and tapering rapidly after 3 days*
- Increasing the **prednisone dose** pre-operatively could further suppress the immune system and impair wound healing, increasing the risk of infection and dehiscence.
- While a **stress-dose steroid** regimen is appropriate, the goal is to provide physiological replacement, not to significantly increase the dose beyond what is necessary to prevent adrenal crisis.
Corticosteroids US Medical PG Question 3: A researcher is studying physiologic and hormonal changes that occur during pregnancy. Specifically, they examine the behavior of progesterone over the course of the menstrual cycle and find that it normally decreases over time; however, during pregnancy this decrease does not occur in the usual time frame. The researcher identifies a circulating factor that appears to be responsible for this difference in progesterone behavior. In order to further examine this factor, the researcher denatures the circulating factor and examines the sizes of its components on a western blot as compared to several other hormones. One of the bands the researcher identifies in this circulating factor is identical to that of another known hormone with which of the following sites of action?
- A. Thyroid gland (Correct Answer)
- B. Adrenal gland
- C. Adipocytes
- D. Bones
- E. Kidney tubules
Corticosteroids Explanation: ***Correct: Thyroid gland***
- The circulating factor described is **human chorionic gonadotropin (hCG)**, which maintains the corpus luteum and progesterone production during early pregnancy
- hCG is a **glycoprotein hormone** composed of an **α subunit** and a **β subunit**
- The **α subunit of hCG is identical** to the α subunits of **TSH (thyroid-stimulating hormone)**, **LH (luteinizing hormone)**, and **FSH (follicle-stimulating hormone)**
- When denatured and examined on Western blot, one of the bands (the α subunit) would be identical to that of **TSH**
- **TSH acts on the thyroid gland** to stimulate thyroid hormone synthesis and release
- This structural similarity explains why very high levels of hCG (as in molar pregnancy or hyperemesis gravidarum) can sometimes cause **thyrotoxicosis** due to cross-reactivity with TSH receptors
*Incorrect: Adrenal gland*
- **ACTH (adrenocorticotropic hormone)** acts on the adrenal cortex to stimulate cortisol production
- ACTH is a **peptide hormone** derived from POMC (pro-opiomelanocortin) and does **NOT share any structural components** with hCG
- There is no identical band between hCG and ACTH on Western blot
*Incorrect: Adipocytes*
- Adipocytes are regulated by hormones like **insulin** and **leptin**
- Neither of these hormones share structural components with hCG
*Incorrect: Bones*
- Bones are primarily regulated by **PTH (parathyroid hormone)**, **calcitonin**, and **vitamin D**
- None of these hormones share structural components with hCG
*Incorrect: Kidney tubules*
- Kidney tubules are regulated by **ADH (antidiuretic hormone/vasopressin)** and **aldosterone**
- Neither shares structural components with hCG
Corticosteroids US Medical PG Question 4: A 45-year-old woman comes to the physician because of fatigue, irregular menses, and recurrent respiratory infections for the past 6 months. Her blood pressure is 151/82 mm Hg. Physical examination shows a round face, thinning of the skin, and multiple bruises on her arms. Further studies confirm the diagnosis of an ACTH-secreting pituitary adenoma. This patient is at greatest risk for which of the following?
- A. Weight loss
- B. Eosinophilia
- C. Bitemporal hemianopsia
- D. Hypoglycemia
- E. Pathologic fracture (Correct Answer)
Corticosteroids Explanation: ***Pathologic fracture***
- This patient has **Cushing's disease** due to an **ACTH-secreting pituitary adenoma**, leading to excess cortisol.
- **Excess cortisol** causes **osteoporosis** by increasing bone resorption and decreasing bone formation, significantly raising the risk of **pathologic fractures**.
- This is the **greatest risk** because **all patients** with chronic hypercortisolism develop bone loss, making fractures highly likely.
*Weight loss*
- Patients with Cushing's disease typically experience **weight gain**, particularly centrally (truncal obesity), due to **cortisol-induced fat redistribution**.
- **Fatigue** is common, but weight loss is not a characteristic feature of Cushing's syndrome.
*Eosinophilia*
- **Hypercortisolism** (Cushing's syndrome) usually causes **eosinopenia** (decreased eosinophil count) and **lymphopenia**, not eosinophilia.
- Cortisol has an anti-inflammatory and immunosuppressive effect, leading to a reduction in circulating eosinophils and lymphocytes.
*Bitemporal hemianopsia*
- While an **ACTH-secreting pituitary adenoma** is present, **bitemporal hemianopsia** occurs only when a pituitary tumor becomes a **macroadenoma** (>10mm) and compresses the **optic chiasm**.
- Most ACTH-secreting adenomas are **microadenomas** (<10mm) that cause symptoms through **hormonal excess**, not mass effect.
- The clinical picture here reflects **Cushing's syndrome** from hypercortisolism, which affects **all patients** regardless of tumor size, whereas visual field defects occur only with large tumors.
*Hypoglycemia*
- **Excess cortisol** **increases gluconeogenesis** and **insulin resistance**, leading to **hyperglycemia**, not hypoglycemia.
- This is a common metabolic complication of Cushing's syndrome, often progressing to **steroid-induced diabetes mellitus**.
Corticosteroids US Medical PG Question 5: A 47-year-old woman presents to the physician with complaints of fatigue accompanied by symmetric pain, swelling, and stiffness in her wrists, fingers, knees, and other joints. She describes the stiffness as being particularly severe upon awakening, but gradually improves as she moves throughout her day. Her physician initially suggests that she take NSAIDs. However, after a few months of minimal symptomatic improvement, she is prescribed an immunosuppressive drug that has a mechanism of preventing IL-2 transcription. What is the main toxicity that the patient must be aware of with this particular class of drugs?
- A. Pancytopenia
- B. Osteoporosis
- C. Hepatotoxicity
- D. Nephrotoxicity (Correct Answer)
- E. Hyperglycemia
Corticosteroids Explanation: ***Nephrotoxicity***
- The drug described, which prevents **IL-2 transcription**, is likely a **calcineurin inhibitor** like cyclosporine or tacrolimus, often used in autoimmune diseases.
- **Nephrotoxicity** (kidney damage) is a major dose-limiting toxicity of calcineurin inhibitors, causing both acute and chronic kidney injury.
*Pancytopenia*
- While some immunosuppressants can cause **pancytopenia** (e.g., azathioprine, methotrexate), it is not the classic or primary toxicity associated with calcineurin inhibitors.
- Calcineurin inhibitors primarily affect **renal function** and can cause other side effects like hypertension or neurotoxicity.
*Osteoporosis*
- **Osteoporosis** is a known side effect of long-term glucocorticoid use, but not typically a primary toxicity of calcineurin inhibitors.
- Glucocorticoids reduce bone formation and increase bone resorption, leading to bone density loss.
*Hepatotoxicity*
- **Hepatotoxicity** (liver damage) can occur with various immunosuppressants, such as methotrexate, but it is not the most prominent or defining toxicity for calcineurin inhibitors.
- While cyclosporine can cause some liver enzyme elevation, **nephrotoxicity** is far more common and severe.
*Hyperglycemia*
- **Hyperglycemia** can be a side effect of some immunosuppressants, particularly **glucocorticoids** and **tacrolimus** (another calcineurin inhibitor).
- However, for the class of drugs that prevent IL-2 transcription (calcineurin inhibitors), **nephrotoxicity** remains the most significant and common major toxicity to be aware of.
Corticosteroids US Medical PG Question 6: A 32-year-old woman comes to the physician because of weight gain, generalized weakness, and irregular menstrual cycles for the past 16 months. She began having symptoms of insomnia and depression 10 months ago. More recently, she has been having difficulties rising from a chair. She has a 2-year history of hypertension. Current medications include citalopram and hydrochlorothiazide. She is 168 cm (5 ft 6 in) tall and weighs 100 kg (220 lb). BMI is 36 kg/m2. Her pulse is 92/min, respirations are 18/min, and blood pressure is 134/76 mm Hg. She appears tired and has a full, plethoric face and central obesity. Examination of the skin shows violaceous linear striations on her lower abdomen. Two midnight serum cortisol studies show measurements of 288 μg/L and 253 μg/L (N < 90); a 24-hour urinary cortisol measurement was 395 μg (N < 300). Upon follow-up laboratory examination, the patient's serum ACTH levels were also elevated at 136 pg/mL (N = 7–50). Which of the following is the most appropriate next step in evaluation?
- A. MRI of the head with contrast
- B. High-dose dexamethasone suppression test (Correct Answer)
- C. Measure ACTH levels in inferior petrosal sinuses
- D. Bilateral adrenalectomy
- E. CT scan of the abdomen with contrast
Corticosteroids Explanation: ***High-dose dexamethasone suppression test***
- Elevated **midnight serum cortisol** and **24-hour urinary cortisol**, combined with elevated **ACTH levels**, confirm **ACTH-dependent Cushing's syndrome**.
- A high-dose dexamethasone suppression test helps **differentiate** between a pituitary adenoma (Cushing's disease), which typically suppresses with high-dose dexamethasone, and ectopic ACTH production, which usually does not.
*MRI of the head with contrast*
- While an MRI of the head might eventually be performed to localize a pituitary adenoma, it is **not the immediate next step** after establishing ACTH dependency.
- The high-dose dexamethasone suppression test provides crucial **functional information** about the source of ACTH prior to imaging.
*Measure ACTH levels in inferior petrosal sinuses*
- **Inferior petrosal sinus sampling (IPSS)** is used to **confirm and lateralize** a pituitary source of ACTH when imaging studies are equivocal or negative.
- This is an **invasive procedure** typically reserved for after the high-dose dexamethasone suppression test has been performed and further distinction is needed.
*Bilateral adrenalectomy*
- **Bilateral adrenalectomy** is a treatment option for Cushing's syndrome, particularly for severe cases or when other treatments fail.
- It is an **irreversible surgical procedure** and would only be considered after a definitive diagnosis and localization of the source of excess cortisol.
*CT scan of the abdomen with contrast*
- A CT scan of the abdomen is primarily used to evaluate for **adrenal adenomas or carcinomas** in cases of **ACTH-independent Cushing's syndrome**.
- Given the **elevated ACTH levels**, an adrenal etiology is less likely, making this an inappropriate next step.
Corticosteroids US Medical PG Question 7: Steroid hormone synthesis, lipid synthesis, and chemical detoxification are activities of which of the following?
- A. Peroxisomes
- B. Nucleolus
- C. Rough Endoplasmic Reticulum
- D. Smooth Endoplasmic Reticulum (Correct Answer)
- E. Golgi bodies
Corticosteroids Explanation: ***Smooth Endoplasmic Reticulum***
- The **smooth endoplasmic reticulum (SER)** is rich in enzymes that catalyze the synthesis of **lipids**, including steroid hormones, and is crucial for the detoxification of drugs and poisons, particularly in liver cells.
- Its tubular structure, devoid of ribosomes, differentiates its functions from the rough ER, focusing on metabolic processes like **calcium ion storage** and carbohydrate metabolism.
*Peroxisomes*
- Peroxisomes are primarily involved in the breakdown of **fatty acids** and amino acids, producing hydrogen peroxide as a byproduct.
- They also play a role in detoxification but are not the primary site for steroid hormone or general lipid synthesis.
*Nucleolus*
- The **nucleolus** is a dense structure within the nucleus responsible for synthesizing **ribosomal RNA (rRNA)** and assembling ribosomes.
- It has no direct role in steroid hormone synthesis, lipid metabolism, or chemical detoxification.
*Rough Endoplasmic Reticulum*
- The **rough endoplasmic reticulum (RER)** is studded with **ribosomes** and is primarily involved in the synthesis and modification of **proteins** destined for secretion or insertion into membranes.
- While it's part of the endomembrane system, it does not directly perform lipid synthesis or chemical detoxification as its main functions.
*Golgi bodies*
- **Golgi bodies (or Golgi apparatus)** are responsible for modifying, sorting, and packaging **proteins and lipids** synthesized in the ER into vesicles for secretion or delivery to other organelles.
- They do not perform the initial synthesis of steroid hormones or lipids, nor are they the primary site for chemical detoxification.
Corticosteroids US Medical PG Question 8: A 67-year-old woman is admitted to the hospital because of a 2-day history of fever, headache, jaw pain, and decreased vision in the right eye. Her erythrocyte sedimentation rate is 84 mm per hour. Treatment with methylprednisolone is initiated but her symptoms do not improve. The physician recommends the administration of a new drug. Three days after treatment with the new drug is started, visual acuity in the right eye increases. The beneficial effect of this drug is most likely due to inhibition of which of the following molecules?
- A. Leukotriene D4
- B. Interleukin-4
- C. Complement component 5
- D. Interleukin-6 (Correct Answer)
- E. Thromboxane A2
Corticosteroids Explanation: ***Interleukin-6***
- The patient's symptoms (fever, headache, jaw pain, decreased vision, elevated ESR) are classic for **giant cell arteritis (GCA)**. GCA involves transmural inflammation of medium to large arteries, often affecting the temporal artery and ophthalmic artery.
- **Tocilizumab**, a monoclonal antibody that targets the **IL-6 receptor**, is an approved treatment for GCA, especially in cases unresponsive to corticosteroids or for steroid-sparing effects. Its efficacy in improving vision and reducing inflammation supports its action on IL-6.
*Leukotriene D4*
- **Leukotriene D4** is a potent bronchoconstrictor and mediator in allergic and asthmatic responses.
- Inhibitors of leukotriene D4, such as montelukast, are used to treat **asthma** and **allergic rhinitis**, not vasculitis like GCA.
*Interleukin-4*
- **Interleukin-4** is a key cytokine in the **Th2 immune response**, promoting B-cell activation, **IgE production**, and allergic inflammation.
- Drugs targeting IL-4 (or its receptor) are used in conditions like **atopic dermatitis** and **asthma**, not GCA, which is primarily a Th1-mediated inflammatory disease.
*Complement component 5*
- **Complement component 5 (C5)** is a central molecule in the **complement cascade**, playing a role in inflammation and cell lysis.
- While the complement system can be involved in various inflammatory conditions, specific C5 inhibition is primarily seen with drugs like **Eculizumab** for paroxysmal nocturnal hemoglobinuria or atypical hemolytic uremic syndrome, which are distinct from GCA.
*Thromboxane A2*
- **Thromboxane A2** is a potent vasoconstrictor and platelet aggregator, primarily produced by platelets.
- Its inhibition, typically by **aspirin**, is used for **antiplatelet effects** in cardiovascular disease and stroke prevention, not for the direct treatment of large vessel vasculitis or to rapidly resolve visual loss in GCA.
Corticosteroids US Medical PG Question 9: A 56-year-old woman undergoes open reduction and internal fixation of the distal tibia 1 day after a fall. She has had rheumatoid arthritis for 12 years and diabetes mellitus for 2 years. Her medications over the past year have included metformin, prednisone, calcium supplements, and methotrexate. Prior to surgery, insulin was added to her medications, and the dose of prednisone was increased. She has had appropriate nutrition over the years with regular follow-ups with her healthcare professional. Which of the following is the most appropriate supplement to prevent wound failure in this patient?
- A. Glutamine
- B. Zinc
- C. Vitamin A
- D. Arginine
- E. Vitamin C (Correct Answer)
Corticosteroids Explanation: ***Vitamin C***
- This patient is at high risk for **wound healing complications** due to her comorbidities (diabetes, rheumatoid arthritis) and medications (prednisone, methotrexate). **Vitamin C** (ascorbic acid) is essential for **collagen synthesis** and cross-linking, which is crucial for wound strength and tissue repair.
- While other options play a role in wound healing, Vitamin C is particularly important in patients with **impaired healing** due to chronic inflammation, corticosteroid use, and metabolic disorders, as it counteracts their negative effects on collagen formation.
*Glutamine*
- **Glutamine** is an important fuel for rapidly dividing cells, including immune cells and fibroblasts, and can be beneficial in catabolic states.
- However, its role in directly counteracting the specific challenges of this patient's wound healing (corticosteroid use, diabetes, rheumatoid arthritis) is **less direct** compared to Vitamin C's role in collagen synthesis.
*Zinc*
- **Zinc** is a cofactor for numerous enzymes involved in cell proliferation, immune function, and collagen synthesis.
- While important, zinc deficiency is not explicitly indicated, and its role as a primary intervention to prevent wound failure in a patient with **prednisone-induced healing impairment** is secondary to vitamin C.
*Vitamin A*
- **Vitamin A** can help reverse the negative effects of **corticosteroids** on wound healing by promoting epithelialization and collagen synthesis.
- While relevant due to prednisone use, its overall importance in **collagen formation** and direct wound strength is not as profound or broad as Vitamin C.
*Arginine*
- **Arginine** is a precursor for nitric oxide, which improves blood flow to wounds, and is involved in collagen formation and immune function.
- Although beneficial for wound healing, particularly in critically ill patients, it is **not the most appropriate single supplement** for addressing the specific collagen synthesis impairment seen in this patient's context of corticosteroid use and chronic disease.
Corticosteroids US Medical PG Question 10: A 4-year-old boy presents to the Emergency Department with wheezing and shortness of breath after playing with the new family pet. Which of the following immunological factors is most involved in generating the antibodies necessary for mast cell Fc-receptor cross-linking and degranulation?
- A. IL-5
- B. IL-13
- C. IL-2
- D. IL-4 (Correct Answer)
- E. IL-10
Corticosteroids Explanation: **IL-4**
- **IL-4** is a primary cytokine responsible for promoting **Th2 differentiation** and inducing **B cell class switching to IgE**, which is critical for allergic reactions.
- The IgE antibodies then bind to **Fc receptors on mast cells**, leading to cross-linking and degranulation upon re-exposure to the allergen.
*IL-5*
- **IL-5** is primarily involved in the growth, differentiation, and activation of **eosinophils**, which are important in late-phase allergic reactions and parasitic infections.
- While it plays a role in allergic inflammation, it does not directly drive the production of IgE antibodies crucial for initial mast cell sensitization.
*IL-13*
- **IL-13** shares many functions with IL-4, including promoting **IgE production** and contributing to airway hyperresponsiveness and mucus secretion in asthma.
- However, **IL-4** is considered the foundational cytokine for initial IgE class switching, even though IL-13 can synergize or contribute later.
*IL-2*
- **IL-2** is primarily known for its role in the **proliferation and differentiation of T cells**, including regulatory T cells, and general immune activation.
- It does not directly promote B cell class switching to IgE or directly induce allergic antibody production.
*IL-10*
- **IL-10** is an **immunosuppressive cytokine** that *inhibits* the production of pro-inflammatory cytokines and can downregulate immune responses.
- Its role is generally to *suppress* allergic responses rather than generate the antibodies (IgE) necessary for mast cell degranulation.
More Corticosteroids US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.
 Widespread, dose-dependent effects. 📌 Remember CUSHINGOID side effects.
Widespread, dose-dependent effects. 📌 Remember CUSHINGOID side effects.
