Calcineurin inhibitors US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Calcineurin inhibitors. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Calcineurin inhibitors US Medical PG Question 1: A 57-year-old woman comes to the clinic complaining of decreased urine output. She reports that over the past 2 weeks she has been urinating less and less every day. She denies changes in her diet or fluid intake. The patient has a history of lupus nephritis, which has resulted in end stage renal disease. She underwent a renal transplant 2 months ago. Since then she has been on mycophenolate and cyclosporine, which she takes as prescribed. The patient’s temperature is 99°F (37.2°C), blood pressure is 172/102 mmHg, pulse is 88/min, and respirations are 17/min with an oxygen saturation of 97% on room air. Labs show an elevation in serum creatinine and blood urea nitrogen. On physical examination, she has 2+ pitting edema of the bilateral lower extremities. Lungs are clear to auscultation. Urinalysis shows elevated protein. A post-void bladder scan is normal. A renal biopsy is obtained, which shows lymphocyte infiltration and intimal swelling. Which of the following is the next best step in management?
- A. Add diltiazem
- B. Nephrectomy
- C. Start intravenous steroids (Correct Answer)
- D. Add ceftriaxone
- E. Discontinue cyclosporine
Calcineurin inhibitors Explanation: ***Start intravenous steroids***
- The patient presents with **decreased urine output**, elevated creatinine, and a recent kidney transplant with biopsy showing **lymphocyte infiltration** and **intimal swelling**, all highly suggestive of **acute cellular rejection**.
- **High-dose intravenous steroids** (e.g., methylprednisolone) are the first-line treatment for acute cellular rejection to suppress the immune response and preserve graft function.
*Add diltiazem*
- **Diltiazem** is a calcium channel blocker used to treat hypertension and arrhythmias, and it can also interfere with cyclosporine metabolism, potentially increasing its levels.
- While the patient has elevated blood pressure, adding diltiazem would not address the underlying **immune rejection** and would not be the primary intervention.
*Nephrectomy*
- **Nephrectomy** involves surgical removal of the transplanted kidney. This radical intervention is reserved for **irreversible graft failure** or severe complications like overwhelming infection or malignancy.
- Given the acute presentation and possibility of reversing rejection with immunosuppression, nephrectomy is **premature** and not the next best step.
*Add ceftriaxone*
- **Ceftriaxone** is an antibiotic used to treat bacterial infections.
- There is no clinical evidence in the stem (e.g., fever, signs of infection) to suggest a **bacterial infection** as the cause of her symptoms, making antibiotics inappropriate.
*Discontinue cyclosporine*
- **Cyclosporine** is an immunosuppressant essential for preventing transplant rejection. Discontinuing it would immediately increase the risk of more severe and potentially **irreversible rejection**.
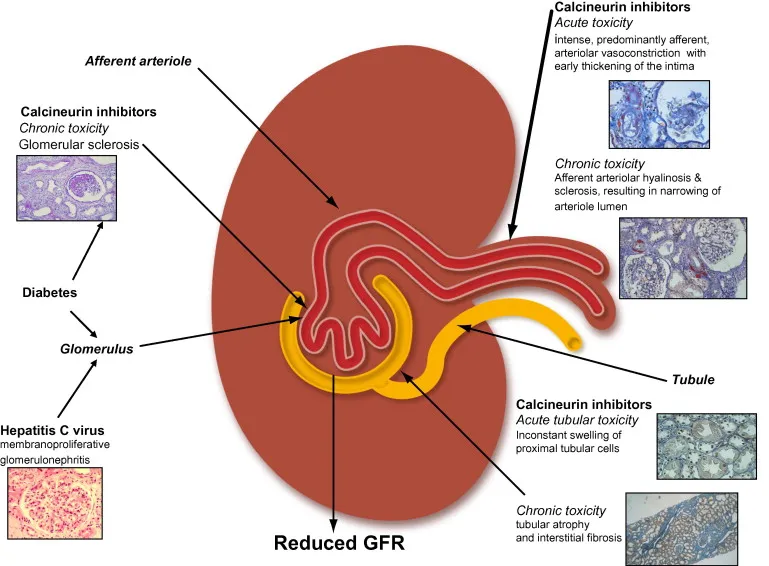
- While cyclosporine can cause nephrotoxicity, the biopsy findings of **cellular infiltration** point more towards rejection rather than primary drug toxicity, and the primary treatment for rejection involves increasing immunosuppression, not withdrawing it.
Calcineurin inhibitors US Medical PG Question 2: A 14-year-old boy has undergone kidney transplantation due to stage V chronic kidney disease. A pre-transplantation serologic assessment showed that he is negative for past or present HIV infection, viral hepatitis, EBV, and CMV infection. He has a known allergy for macrolides. The patient has no complaints 1 day after transplantation. His vital signs include: blood pressure 120/70 mm Hg, heart rate 89/min, respiratory rate 17/min, and temperature 37.0°C (98.6°F). On physical examination, the patient appears to be pale, his lungs are clear on auscultation, heart sounds are normal, and his abdomen is non-tender on palpation. His creatinine is 0.65 mg/dL (57.5 µmol/L), GFR is 71.3 mL/min/1.73 m2, and urine output is 0.9 mL/kg/h. Which of the following drugs should be used in the immunosuppressive regimen in this patient?
- A. Belatacept
- B. Sirolimus
- C. Omalizumab
- D. Daclizumab
- E. Basiliximab (Correct Answer)
Calcineurin inhibitors Explanation: **Basiliximab**
- **Basiliximab** is a **monoclonal antibody** that targets the **IL-2 receptor (CD25)** on activated T cells, preventing their proliferation and inducing immunosuppression.
- It is commonly used as **induction therapy** in kidney transplant recipients due to its good safety profile, especially in pediatric patients, without the nephrotoxicity associated with calcineurin inhibitors, minimizing acute rejection risks immediately post-transplant.
*Belatacept*
- **Belatacept** works by co-stimulation blockade, binding to **CD80 and CD86** on antigen-presenting cells to prevent T-cell activation.
- It is typically reserved for patients who cannot tolerate calcineurin inhibitors due to **nephrotoxicity** or require a steroid-sparing regimen, which is not indicated as an immediate need in this patient.
*Sirolimus*
- **Sirolimus** is an **mTOR inhibitor** that works by blocking T-cell proliferation and B-cell differentiation.
- It is associated with several side effects, including **delayed wound healing**, **thrombocytopenia**, and **hyperlipidemia**, which are undesirable in the immediate post-transplant period, especially in a growing adolescent.
*Omalizumab*
- **Omalizumab** is an **anti-IgE monoclonal antibody** primarily used for allergic asthma and chronic spontaneous urticaria.
- It has no role in **immunosuppression for organ transplantation** as its mechanism of action is unrelated to preventing graft rejection.
*Daclizumab*
- **Daclizumab** is another **monoclonal antibody** that also targets the **IL-2 receptor (CD25)**, similar to basiliximab.
- However, daclizumab has been **withdrawn from the market** due to serious adverse effects including severe liver injury and autoimmune encephalitis, making it unavailable for clinical use in transplantation.
Calcineurin inhibitors US Medical PG Question 3: A 50-year-old woman comes to the physician for the evaluation of excessive hair growth on her chin over the past 2 weeks. She also reports progressive enlargement of her gums. Three months ago, she underwent a liver transplantation due to Wilson disease. Following the procedure, the patient was started on transplant rejection prophylaxis. She has a history of poorly-controlled type 2 diabetes mellitus. Temperature is 37°C (98.6°F), pulse is 80/min, respirations are 22/min, and blood pressure is 150/80 mm Hg. Physical examination shows dark-pigmented, coarse hair on the chin, upper lip, and chest. The gingiva and the labial mucosa are swollen. There is a well-healed scar on her right lower abdomen. Which of the following drugs is the most likely cause of this patient's findings?
- A. Daclizumab
- B. Cyclosporine (Correct Answer)
- C. Sirolimus
- D. Methotrexate
- E. Tacrolimus
Calcineurin inhibitors Explanation: **Cyclosporine**
* This patient's **combination of hirsutism** (excessive hair growth) **and gingival hyperplasia** (gum enlargement) is the classic presentation of cyclosporine toxicity, an immunosuppressant commonly used for transplant rejection prophylaxis.
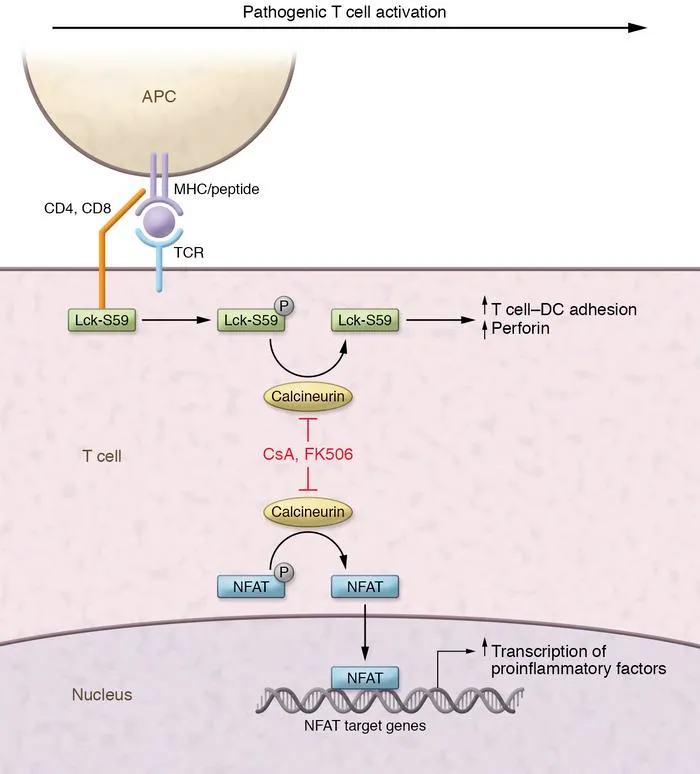
* Cyclosporine is a **calcineurin inhibitor** that prevents T-cell activation and is highly effective in preventing graft rejection.
* The **simultaneous presence of both hirsutism and prominent gingival hyperplasia** is particularly characteristic of cyclosporine.
*Daclizumab*
* **Daclizumab** is a **monoclonal antibody** targeting the IL-2 receptor, which was previously used for transplant prophylaxis but has been discontinued for this indication.
* It is not associated with hirsutism or gingival hyperplasia.
*Sirolimus*
* **Sirolimus** is an **mTOR inhibitor** used as an immunosuppressant, known for side effects like hyperlipidemia, myelosuppression, and delayed wound healing.
* It does **not** typically cause hirsutism or gingival hyperplasia.
*Methotrexate*
* **Methotrexate** is an **antimetabolite** and immunosuppressant commonly used in autoimmune diseases and cancer, with side effects including bone marrow suppression, mucositis, and liver toxicity.
* Hirsutism and gingival hyperplasia are **not** characteristic side effects of methotrexate.
*Tacrolimus*
* **Tacrolimus** is another **calcineurin inhibitor**, similar to cyclosporine, but with a different side effect profile. While tacrolimus can cause hirsutism, **gingival hyperplasia is significantly less common** with tacrolimus compared to cyclosporine.
* The **presence of prominent gingival hyperplasia alongside hirsutism strongly favors cyclosporine** over tacrolimus.
* Tacrolimus is more commonly associated with **neurotoxicity** (e.g., tremor) and **nephrotoxicity**.
Calcineurin inhibitors US Medical PG Question 4: A 68-year-old woman comes to the physician for a follow-up examination. Three months ago, she underwent heart transplantation for restrictive cardiomyopathy and was started on transplant rejection prophylaxis. Her pulse is 76/min and blood pressure is 148/82 mm Hg. Physical examination shows enlargement of the gum tissue. There is a well-healed scar on her chest. Serum studies show hyperlipidemia. The physician recommends removing a drug that decreases T cell activation by inhibiting the transcription of interleukin-2 from the patient's treatment regimen and replacing it with a different medication. Which of the following drugs is the most likely cause of the adverse effects seen in this patient?
- A. Mycophenolate mofetil
- B. Azathioprine
- C. Tacrolimus
- D. Cyclosporine (Correct Answer)
- E. Prednisolone
Calcineurin inhibitors Explanation: ***Cyclosporine***
- The patient's symptoms of **gingival hyperplasia**, **hypertension**, and **hyperlipidemia** are classic side effects associated with cyclosporine.
- Cyclosporine is a calcineurin inhibitor that **decreases T-cell activation** by inhibiting IL-2 transcription, matching the drug description.
*Mycophenolate mofetil*
- Mycophenolate mofetil is an **antiproliferative agent** that inhibits purine synthesis, primarily affecting lymphocytes.
- Its common side effects are mainly **hematologic** (leukopenia, anemia) and **gastrointestinal** (diarrhea, nausea), not gingival hyperplasia or hypertension.
*Azathioprine*
- Azathioprine is a **purine analog** that impairs DNA synthesis and inhibits lymphocyte proliferation.
- Key side effects include **myelosuppression** (leukopenia, thrombocytopenia) and **hepatotoxicity**, which are not present here.
*Tacrolimus*
- Tacrolimus is also a **calcineurin inhibitor** that inhibits IL-2 transcription, similar to cyclosporine.
- While it can cause **hypertension** and **hyperlipidemia**, it is less commonly associated with **gingival hyperplasia** than cyclosporine.
*Prednisolone*
- Prednisolone is a **corticosteroid** used for immunosuppression, acting broadly on the immune system.
- Common side effects include **hyperglycemia**, **osteoporosis**, and **cataracts**, not specific gingival overgrowth.
Calcineurin inhibitors US Medical PG Question 5: A 29-year-old female presents to her gynecologist complaining of a painful rash around her genitals. She has multiple sexual partners and uses condoms intermittently. Her last STD screen one year ago was negative. On examination, she has bilateral erosive vesicles on her labia majora and painful inguinal lymphadenopathy. She is started on an oral medication that requires a specific thymidine kinase for activation. Which of the following adverse effects is associated with this drug?
- A. Photosensitivity
- B. Deafness
- C. Renal failure (Correct Answer)
- D. Gingival hyperplasia
- E. Pulmonary fibrosis
Calcineurin inhibitors Explanation: ***Renal failure***
- The patient's symptoms (painful genital rash, erosive vesicles, inguinal lymphadenopathy) are highly suggestive of **herpes simplex virus (HSV) infection**, likely genital herpes.
- The drug described is an antiviral agent like **acyclovir, valacyclovir, or famciclovir**, which require **viral thymidine kinase** for activation and are known to cause **renal impairment** (nephrotoxicity) as an adverse effect, especially with high doses or in dehydrated patients due to crystal nephropathy.
*Photosensitivity*
- **Photosensitivity** is a common side effect of some antibiotics (e.g., tetracyclines, sulfonamides), diuretics (e.g., thiazides), and antifungals, but it is **not a prominent adverse effect of acyclovir or its derivatives**.
- While theoretical, it is not a clinically significant or frequently observed adverse effect associated with the class of antiviral drugs used for HSV.
*Deafness*
- **Ototoxicity**, leading to deafness or hearing loss, is a well-known adverse effect of certain classes of drugs, such as **aminoglycoside antibiotics** (e.g., gentamicin) and **loop diuretics** (e.g., furosemide).
- It is **not an adverse effect** associated with antiviral medications like acyclovir.
*Gingival hyperplasia*
- **Gingival hyperplasia** (overgrowth of gum tissue) is a recognized side effect of specific medications including **phenytoin** (an anticonvulsant), **cyclosporine** (an immunosuppressant), and **calcium channel blockers** (e.g., nifedipine, amlodipine).
- This adverse effect is **not associated with antiviral drugs** used to treat herpes simplex.
*Pulmonary fibrosis*
- **Pulmonary fibrosis** is a serious adverse effect linked to various drugs like **amiodarone** (an antiarrhythmic), **bleomycin** (a chemotherapeutic agent), **methotrexate** (an immunosuppressant/chemotherapeutic), and **nitrofurantoin** (an antibiotic).
- **Antiviral medications for HSV** do not typically cause pulmonary fibrosis.
Calcineurin inhibitors US Medical PG Question 6: A 19-year-old South Asian male presents to the family physician concerned that he is beginning to go bald. He is especially troubled because his father and grandfather "went completely bald by the age of 25," and he is willing to try anything to prevent his hair loss. The family physician prescribes a medication that prevents the conversion of testosterone to dihydrotestosterone. Which of the following enzymes is inhibited by this medication?
- A. Cyclooxygenase 2
- B. Desmolase
- C. Aromatase
- D. cGMP phosphodiesterase
- E. 5-alpha-reductase (Correct Answer)
Calcineurin inhibitors Explanation: ***5-alpha-reductase***
- The medication described inhibits the conversion of **testosterone to dihydrotestosterone (DHT)**, which is catalyzed by the enzyme **5-alpha-reductase**.
- **Androgenetic alopecia** (male pattern baldness) is driven by DHT, and inhibiting this enzyme reduces DHT levels in the scalp, thereby slowing hair loss.
*Cyclooxygenase 2*
- **Cyclooxygenase 2 (COX-2)** is involved in the synthesis of **prostaglandins** from arachidonic acid, mediating inflammation and pain.
- COX-2 inhibitors are used as anti-inflammatory drugs (e.g., celecoxib), not for male pattern baldness.
*Desmolase*
- **Cholesterol desmolase** (CYP11A1) is an enzyme that catalyzes the first committed step in **steroidogenesis**, converting cholesterol to pregnenolone.
- Inhibition of desmolase would affect the synthesis of all steroid hormones, not specifically target the conversion of testosterone to DHT for hair loss treatment.
*Aromatase*
- **Aromatase** is an enzyme responsible for converting androgens (like testosterone) into **estrogens**.
- Aromatase inhibitors are used in the treatment of estrogen-receptor positive breast cancer, not male pattern baldness.
*cGMP phosphodiesterase*
- **cGMP phosphodiesterase (PDE5)** is an enzyme that breaks down cyclic GMP (cGMP), which is involved in smooth muscle relaxation.
- PDE5 inhibitors (e.g., sildenafil) are used to treat **erectile dysfunction** and **pulmonary hypertension**, not hair loss.
Calcineurin inhibitors US Medical PG Question 7: A previously healthy 30-year-old man comes to the physician because of a 2-week history of lesions on his elbows. He has no history of serious illness and takes no medications. Physical examination shows skin lesions on bilateral elbows. A photograph of his right elbow is shown. Which of the following is the most appropriate treatment for this patient's skin condition?
- A. Diphenhydramine
- B. Ketoconazole
- C. Dapsone
- D. Terbinafine
- E. Calcipotriene (Correct Answer)
Calcineurin inhibitors Explanation: ***Calcipotriene***
- The image shows **erythematous plaques with silvery scales on the elbow**, which is characteristic of **psoriasis**.
- **Calcipotriene** (a vitamin D analog) is a topical medication commonly used to treat localized psoriasis by inhibiting keratinocyte proliferation and promoting their differentiation.
*Diphenhydramine*
- **Diphenhydramine** is an antihistamine primarily used for allergic reactions and insomnia.
- It would not address the underlying inflammatory and hyperproliferative pathology of psoriasis.
*Ketoconazole*
- **Ketoconazole** is an antifungal medication used to treat fungal infections of the skin.
- The presented skin lesions are consistent with psoriasis, not a fungal infection.
*Dapsone*
- **Dapsone** is an antibacterial and anti-inflammatory drug used for conditions like leprosy, dermatitis herpetiformis, and some autoimmune skin conditions.
- It is not a first-line treatment for typical plaque psoriasis as seen in this patient.
*Terbinafine*
- **Terbinafine** is an antifungal medication, primarily used for dermatophyte infections such as ringworm or athlete's foot.
- It would be ineffective for psoriasis, which is an autoimmune inflammatory condition.
Calcineurin inhibitors US Medical PG Question 8: A previously healthy 13-year-old boy is brought to the emergency department by his parents for the evaluation of several episodes of vomiting since this morning. He reports nausea and severe headache. Over the past four days, he has had fever, a runny nose, and a sore throat. His mother gave him an analgesic drug that she uses for rheumatoid arthritis. He has not had any trauma. Last month, the patient traveled to Mexico with his family. He is at the 85th percentile for height and 25th percentile for weight. He appears weak. His temperature is 38°C (100°F), pulse is 90/min, respirations are 18/min, and blood pressure is 100/60 mm Hg. Mental status examination shows psychomotor agitation alternating with lethargy. Examination shows bilateral optic disc swelling. Serum studies show:
Urea nitrogen 30 mg/dL
Glucose 70 mg/dL
Aspartate aminotransferase (AST, GOT) 60 U/L
Alanine aminotransferase (ALT, GPT) 60 U/L
Arterial blood gas analysis on room air shows a pH of 7.30. Which of the following is the most likely cause of this patient's symptoms?
- A. Infection with hepatitis A virus
- B. Reye syndrome (Correct Answer)
- C. Autoimmune destruction of pancreatic beta cells
- D. Ruptured aneurysm in the circle of Willis
- E. Antifreeze ingestion
Calcineurin inhibitors Explanation: ***Reye syndrome***
- The combination of a recent **viral illness** (fever, runny nose, sore throat) treated with an **analgesic used for rheumatoid arthritis** (likely aspirin), followed by **encephalopathy** (psychomotor agitation, lethargy, severe headache, vomiting, optic disc swelling) and **liver dysfunction** (elevated AST/ALT, elevated urea nitrogen, acidosis), is highly characteristic of Reye syndrome.
- This syndrome is particularly associated with **aspirin use in children** recovering from viral infections, leading to mitochondrial damage in the liver and brain.
*Infection with hepatitis A virus*
- While hepatitis A can cause **nausea, vomiting**, and **elevated liver enzymes**, it is less likely to cause the severe neurological symptoms and metabolic derangements seen here, such as **optic disc swelling** and **acidosis**.
- The history of aspirin use after a viral illness points more strongly towards Reye syndrome over hepatitis A, despite a travel history to Mexico.
*Autoimmune destruction of pancreatic beta cells*
- This describes **Type 1 diabetes mellitus**, which would present with symptoms like **polyuria, polydipsia, weight loss**, and sometimes diabetic ketoacidosis.
- The patient's presentation with acute encephalopathy, liver dysfunction, and a normal blood glucose level makes this diagnosis unlikely.
*Ruptured aneurysm in the circle of Willis*
- A ruptured aneurysm would cause a **sudden, severe headache** and neurological deficits, but it would not explain the preceding viral illness, the **liver enzyme elevations**, or the **metabolic acidosis**.
- While optic disc swelling can occur with increased intracranial pressure, the overall clinical picture does not align.
*Antifreeze ingestion*
- Antifreeze (ethylene glycol) ingestion causes **severe metabolic acidosis** with a high anion gap, **renal failure**, and neurological symptoms.
- While it can explain the acidosis and altered mental status, there is **no history of exposure** and it would not account for the preceding viral illness or the specific pattern of liver enzyme elevation associated with Reye syndrome.
Calcineurin inhibitors US Medical PG Question 9: A 65-year-old woman with COPD comes to the emergency department with 2-day history of worsening shortness of breath and cough. She often has a mild productive cough, but she noticed that her sputum is more yellow than usual. She has not had any recent fevers, chills, sore throat, or a runny nose. Her only medication is a salmeterol inhaler that she uses twice daily. Her temperature is 36.7°C (98°F), pulse is 104/min, blood pressure is 134/73 mm Hg, respiratory rate is 22/min, and oxygen saturation is 85%. She appears uncomfortable and shows labored breathing. Lung auscultation reveals coarse bibasilar inspiratory crackles. A plain film of the chest shows mild hyperinflation and flattening of the diaphragm but no consolidation. She is started on supplemental oxygen via nasal cannula. Which of the following is the most appropriate initial pharmacotherapy?
- A. Albuterol and montelukast
- B. Albuterol and theophylline
- C. Prednisone and albuterol (Correct Answer)
- D. Roflumilast and prednisone
- E. Prednisone and salmeterol
Calcineurin inhibitors Explanation: ***Prednisone and albuterol***
- This patient is experiencing an **acute exacerbation of COPD** (AECOPD) characterized by worsening dyspnea, increased sputum purulence (yellow sputum), and elevated respiratory rate, despite no fever or chills. AECOPD is managed with **systemic corticosteroids** (like prednisone) and **short-acting bronchodilators** (like albuterol).
- Prednisone reduces **airway inflammation**, while albuterol provides rapid **bronchodilation** to relieve bronchospasm and improve airflow.
*Albuterol and montelukast*
- **Montelukast** is a leukotriene receptor antagonist used for chronic asthma management and sometimes for COPD patients with an asthmatic component, but it is not a first-line agent for acute exacerbations.
- While **albuterol** is appropriate, montelukast works too slowly to be the primary acute anti-inflammatory agent needed for an AECOPD.
*Albuterol and theophylline*
- **Theophylline** is a phosphodiesterase inhibitor that can improve lung function but has a narrow therapeutic index and significant side effects, making it a less preferred option, especially in acute settings.
- While **albuterol** is appropriate, theophylline is not generally used as an initial agent for AECOPD given safer and more effective alternatives like corticosteroids.
*Roflumilast and prednisone*
- **Roflumilast** is a phosphodiesterase-4 inhibitor used to reduce exacerbations in patients with severe COPD and chronic bronchitis, but it is a chronic medication and not indicated for acute management.
- While **prednisone** is appropriate, roflumilast is not an acute bronchodilator for immediate relief.
*Prednisone and salmeterol*
- **Salmeterol** is a **long-acting beta-agonist (LABA)**, which is part of the patient's maintenance therapy for COPD. In an acute exacerbation, **short-acting bronchodilators** like albuterol are preferred for rapid relief.
- While **prednisone** is appropriate, continuing salmeterol alone as the bronchodilator in an acute setting is insufficient without a short-acting agent.
Calcineurin inhibitors US Medical PG Question 10: A 35-year-old woman presents to the clinic with a 2-week history of headaches. She was in her usual state of health until 2 weeks ago, when she started having headaches. The headaches are throughout her whole head and rated as a 7/10. They are worse in the mornings and when she bends over. She has some mild nausea, but no vomiting. The headaches are not throbbing and are not associated with photophobia or phonophobia. On further questioning, she has noticed more hair than usual on her pillow in the morning and coming out in her hands when she washes her hair. The past medical history is unremarkable; she takes no prescription medications, but for the past year she has been taking an oral 'health supplement' recommended by her sister, which she orders over the internet. She cannot recall the supplement's name and does not know its contents. The physical exam is notable for some mild hepatomegaly but is otherwise unremarkable. This patient's presentation is most likely related to which of the following micronutrients?
- A. Vitamin D
- B. Vitamin B12
- C. Vitamin C
- D. Vitamin K
- E. Vitamin A (Correct Answer)
Calcineurin inhibitors Explanation: ***Vitamin A***
- The patient's symptoms, including **headaches worse in the mornings and with bending over**, **mild nausea**, and **diffuse hair loss**, along with **hepatomegaly**, are classic signs of **chronic vitamin A toxicity** (**hypervitaminosis A**).
- The likely source is a high-dose oral "health supplement" of unknown content, as vitamin A is a fat-soluble vitamin stored in the liver, leading to toxicity with excessive intake.
*Vitamin D*
- **Vitamin D toxicity** (hypervitaminosis D) typically presents with **hypercalcemia**, leading to symptoms like polyuria, polydipsia, renal stones, and muscle weakness, which are not described here.
- While headaches can occur, **hair loss** and **hepatomegaly** are not characteristic features of vitamin D toxicity.
*Vitamin B12*
- **Vitamin B12 toxicity** is extremely rare, as it is a water-soluble vitamin and excess is readily excreted.
- There are no well-established adverse effects or toxicity syndromes associated with high doses of vitamin B12 that would explain these symptoms.
*Vitamin C*
- **Vitamin C** is a water-soluble vitamin, and acute toxicity is uncommon because excess is excreted in urine.
- High doses can lead to **gastrointestinal upset** (diarrhea, nausea, abdominal cramps) and, rarely, kidney stones, but not the constellation of headache, hair loss, and hepatomegaly seen in this patient.
*Vitamin K*
- **Vitamin K toxicity** is generally rare and primarily associated with synthetic forms (menadione).
- In infants, high doses can cause **hemolytic anemia** and **jaundice**, but these symptoms are not typical for adults, nor do they explain the described presentation of headache, hair loss, and hepatomegaly.
More Calcineurin inhibitors US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.