Antimetabolites (azathioprine, mycophenolate) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Antimetabolites (azathioprine, mycophenolate). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Antimetabolites (azathioprine, mycophenolate) US Medical PG Question 1: A 24-year-old woman of Ashkenazi Jewish descent presents with recurrent bloody diarrhea and abdominal pain. She says she feels well otherwise. Review of systems is significant for a 4 kg weight loss over the past month. Physical examination is significant for multiple aphthous oral ulcers. Colonoscopy reveals a cobblestone pattern of lesions of the mucosa of the intestinal wall with skip lesions involving the terminal ileum and colon. The patient is informed of the diagnosis and medication to treat her condition is prescribed. On a follow-up visit 6 weeks later, the patient presents with non-productive cough, chest pain, dyspnea on exertion, and worsening oral lesions. A chest radiograph reveals a diffuse interstitial pattern. Which of the following enzymes is inhibited by the medication most likely prescribed for her initial diagnosis?
- A. Thymidine kinase
- B. DNA polymerase
- C. Dihydrofolate reductase (Correct Answer)
- D. Hypoxanthine guanine-phosphoribosyltransferase (HGPRT)
- E. Thymidylate synthase
Antimetabolites (azathioprine, mycophenolate) Explanation: ***Dihydrofolate reductase***
- The patient's initial symptoms (recurrent **bloody diarrhea**, **abdominal pain**, **weight loss**, **oral ulcers**, **cobblestone pattern** of lesions in the sigmoid colon) are highly suggestive of **Crohn's disease**. The patient's **Ashkenazi Jewish descent** is also a risk factor for Crohn's disease.
- The worsening oral lesions, cough, chest pain, and **diffuse interstitial pattern** on chest radiograph 6 weeks later are classic signs of **methotrexate toxicity**. Methotrexate, a common treatment for Crohn's disease, inhibits **dihydrofolate reductase**, an enzyme essential for **folate metabolism** and **DNA synthesis**.
*Thymidine kinase*
- **Thymidine kinase** is an enzyme involved in the salvage pathway of pyrimidine synthesis. It is typically inhibited by antiviral drugs like **acyclovir** and **ganciclovir**, which are not used for Crohn's disease.
- Inhibition of thymidine kinase is not associated with the lung and oral toxicities seen in this patient.
*DNA polymerase*
- **DNA polymerase** is crucial for DNA replication and repair. Drugs inhibiting DNA polymerase, such as some **antivirals** (e.g., foscarnet) and **chemotherapeutics** (e.g., cytarabine), are not primary treatments for Crohn's disease.
- Inhibition of DNA polymerase does not directly lead to the specific constellation of symptoms observed from methotrexate toxicity.
*Hypoxanthine guanine-phosphoribosyltransferase (HGPRT)*
- **HGPRT** is an enzyme central to the purine salvage pathway. Its deficiency leads to **Lesch-Nyhan syndrome**.
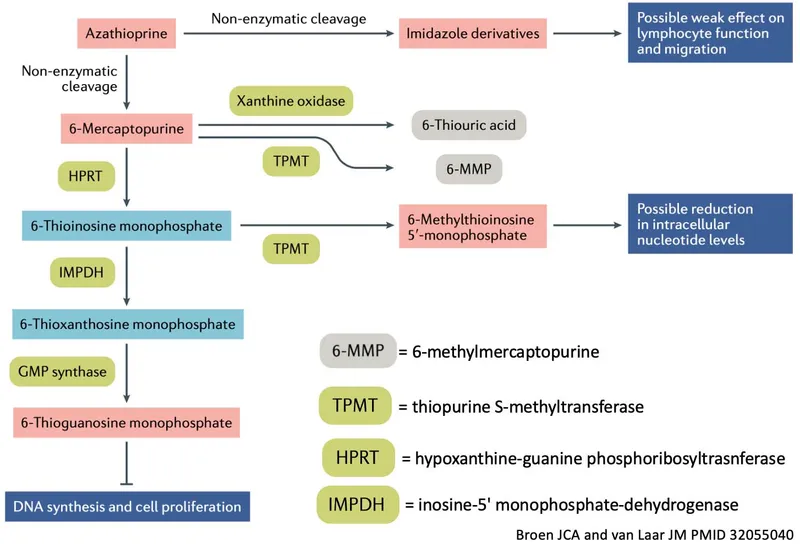
- While some immunosuppressants like **azathioprine** and **mercaptopurine** act as purine analogs and affect purine metabolism, they do not directly inhibit HGPRT and do not typically cause the acute pulmonary toxicity seen with methotrexate.
*Thymidylate synthase*
- **Thymidylate synthase** is an enzyme involved in the synthesis of pyrimidine deoxyribonucleotides, particularly dTMP, which is essential for DNA synthesis. It is a target for some **chemotherapeutic agents** like **5-fluorouracil**.
- While methotrexate indirectly affects thymidylate synthesis by depleting folate precursors, its direct mechanism of action is the inhibition of **dihydrofolate reductase**, not thymidylate synthase itself, and 5-fluorouracil toxicity differs from the presented symptoms.
Antimetabolites (azathioprine, mycophenolate) US Medical PG Question 2: A 3-month-old boy is brought to the pediatrician by his mother after she notices orange sand–like crystalline material in her child’s diaper. He is not currently taking any medication and is exclusively breastfed. His immunizations are up to date. The doctor tells the mother that her son may have an X-linked recessive disorder. The boy is prescribed a medication that inhibits an enzyme responsible for the production of the crystals seen in his urine microscopy. Which of the following enzymes is the target of this medication?
- A. Adenosine deaminase
- B. Xanthine oxidase (Correct Answer)
- C. Adenine phosphoribosyltransferase
- D. Hypoxanthine-guanine phosphoribosyltransferase
- E. Aminolevulinic acid synthetase
Antimetabolites (azathioprine, mycophenolate) Explanation: ***Xanthine oxidase***
- The presence of **orange, sand-like crystalline material** in the diaper of a 3-month-old, along with the physician's comment about an **X-linked recessive disorder,** strongly suggests **Lesch-Nyhan syndrome**.
- In Lesch-Nyhan syndrome, a deficiency of **hypoxanthine-guanine phosphoribosyltransferase (HGPRT)** leads to an increase in **uric acid** production, which is then broken down by **xanthine oxidase**. Inhibiting xanthine oxidase with allopurinol is the treatment to reduce uric acid levels.
*Adenosine deaminase*
- Deficiency in **adenosine deaminase (ADA)** causes **severe combined immunodeficiency (SCID)** and would present with recurrent infections rather than crystalline urine.
- ADA is involved in purine metabolism, but its deficiency leads to the accumulation of deoxyadenosine and its phosphorylated derivatives, which are toxic to lymphocytes.
*Adenine phosphoribosyltransferase*
- Deficiency of **adenine phosphoribosyltransferase (APRT)** is associated with **2,8-dihydroxyadenine urolithiasis**, which can also cause renal stones, but it is much rarer than Lesch-Nyhan and typically presents differently (e.g., recurrent stone formation) rather than the classic "orange sand" in infants.
- This enzyme is involved in the salvage pathway of adenine.
*Hypoxanthine-guanine phosphoribosyltransferase*
- This enzyme, **HGPRT**, is the *deficient* enzyme in Lesch-Nyhan syndrome, not the enzyme targeted by medication.
- Its deficiency leads to the overproduction of uric acid precursors (hypoxanthine and guanine), which are then converted to uric acid by xanthine oxidase.
*Aminolevulinic acid synthetase*
- **Aminolevulinic acid synthetase (ALAS)** is involved in **heme synthesis**.
- Disorders related to this enzyme, such as **porphyrias**, would present with neurologic symptoms, psychiatric disturbances, or photosensitivity, not uric acid crystals in the urine.
Antimetabolites (azathioprine, mycophenolate) US Medical PG Question 3: A 54-year-old woman presents with acute pain in her left toe. She says she hasn't been able to wear closed shoes for 2 weeks. Past medical history is significant for gastroesophageal reflux disease, diagnosed 2 years ago. The patient is afebrile and vital signs are within normal limits. Her BMI is 31 kg/m2. On physical examination, the left toe is warm to touch, swollen, and erythematous. A joint fluid aspiration from the left toe is performed and shows needle-shaped negatively birefringent urate crystals. The patient is started on methotrexate for gout prophylaxis. On her follow-up visit 6 weeks later, she has an elevated homocysteine level, a decreased serum folic acid level, and a normal methylmalonic acid level. Which of the following drugs would most likely cause a similar side effect to that seen in this patient?
- A. Cisplatin
- B. α-Methyldopa
- C. Cephalosporins
- D. Penicillins
- E. Azathioprine (Correct Answer)
Antimetabolites (azathioprine, mycophenolate) Explanation: ***Azathioprine***
- Both methotrexate and azathioprine are **antimetabolites** that cause **myelosuppression** by interfering with nucleic acid synthesis in rapidly dividing cells
- Methotrexate inhibits dihydrofolate reductase, blocking folate metabolism essential for purine and thymidine synthesis, leading to **folate deficiency** (elevated homocysteine, low folate)
- Azathioprine, a purine analog, inhibits purine synthesis and can cause similar **bone marrow suppression**, though through a different mechanism
- Both agents share common toxicities including leukopenia, thrombocytopenia, and increased infection risk
*Cisplatin*
- Cisplatin is a **platinum-based alkylating agent** that cross-links DNA strands
- Primary toxicities are **nephrotoxicity**, ototoxicity, and peripheral neuropathy—not related to folate metabolism or antimetabolite effects
*α-Methyldopa*
- Alpha-methyldopa is a **centrally-acting antihypertensive** (alpha-2 agonist) used especially in pregnancy
- Side effects include sedation, orthostatic hypotension, and hemolytic anemia—**not myelosuppression or folate-related effects**
*Cephalosporins*
- Cephalosporins are **beta-lactam antibiotics** that inhibit bacterial cell wall synthesis
- Well-tolerated with main side effects being **gastrointestinal upset and hypersensitivity reactions**—no antimetabolite effects
*Penicillins*
- Penicillins are **beta-lactam antibiotics** with similar mechanism to cephalosporins
- Primary concern is **hypersensitivity reactions** (rash to anaphylaxis)—no antimetabolite or bone marrow suppression effects
Antimetabolites (azathioprine, mycophenolate) US Medical PG Question 4: An investigator is studying a drug that acts on the thyroid hormone pathway. Levels of serum free T3 and T4 in healthy participants are measured before and after administration of the drug. After administration, there is a decrease in the average serum free T3 level, while the average serum free T4 level is increased compared to initial serum studies. Inhibition of which of the following is the most likely mechanism of action of this drug?
- A. Thyroid-stimulating hormone
- B. Follicular iodotyrosine deiodinase
- C. Follicular thyroid peroxidase
- D. Peripheral 5'-deiodinase (Correct Answer)
- E. Follicular thyroid proteases
Antimetabolites (azathioprine, mycophenolate) Explanation: ***Peripheral 5'-deiodinase***
- Inhibition of **peripheral 5'-deiodinase** would decrease the conversion of **T4 to T3** in the periphery, resulting in lower **free T3** and higher **free T4** levels.
- This enzyme is crucial for activating T4 into the more potent T3, and its blockade explains the observed changes in hormone levels.
*Thyroid-stimulating hormone*
- Inhibition of **TSH** would lead to a decrease in the production and release of both **T3 and T4** from the thyroid gland.
- This contradicts the observed increase in **free T4** levels.
*Follicular iodotyrosine deiodinase*
- This enzyme is involved in recycling iodine from **monoiodotyrosine (MIT)** and **diiodotyrosine (DIT)** within the thyroid follicular cells, which is important for efficient thyroid hormone synthesis.
- Its inhibition would primarily affect iodine availability and synthesis, not directly lead to increased T4 and decreased T3 in the periphery.
*Follicular thyroid peroxidase*
- **Thyroid peroxidase (TPO)** is critical for the **iodination of tyrosine residues** on thyroglobulin and the **coupling of MIT and DIT** to form T3 and T4.
- Inhibition of TPO would decrease the synthesis of both **T3 and T4**, contrary to the observed increase in **free T4**.
*Follicular thyroid proteases*
- **Thyroid proteases** cleave thyroglobulin to release mature **T3 and T4** into the bloodstream.
- Inhibition of these proteases would lead to a decrease in the release of both **T3 and T4**, which does not align with the observed increase in **free T4**.
Antimetabolites (azathioprine, mycophenolate) US Medical PG Question 5: A 68-year-old woman comes to the physician for a follow-up examination. Three months ago, she underwent heart transplantation for restrictive cardiomyopathy and was started on transplant rejection prophylaxis. Her pulse is 76/min and blood pressure is 148/82 mm Hg. Physical examination shows enlargement of the gum tissue. There is a well-healed scar on her chest. Serum studies show hyperlipidemia. The physician recommends removing a drug that decreases T cell activation by inhibiting the transcription of interleukin-2 from the patient's treatment regimen and replacing it with a different medication. Which of the following drugs is the most likely cause of the adverse effects seen in this patient?
- A. Mycophenolate mofetil
- B. Azathioprine
- C. Tacrolimus
- D. Cyclosporine (Correct Answer)
- E. Prednisolone
Antimetabolites (azathioprine, mycophenolate) Explanation: ***Cyclosporine***
- The patient's symptoms of **gingival hyperplasia**, **hypertension**, and **hyperlipidemia** are classic side effects associated with cyclosporine.
- Cyclosporine is a calcineurin inhibitor that **decreases T-cell activation** by inhibiting IL-2 transcription, matching the drug description.
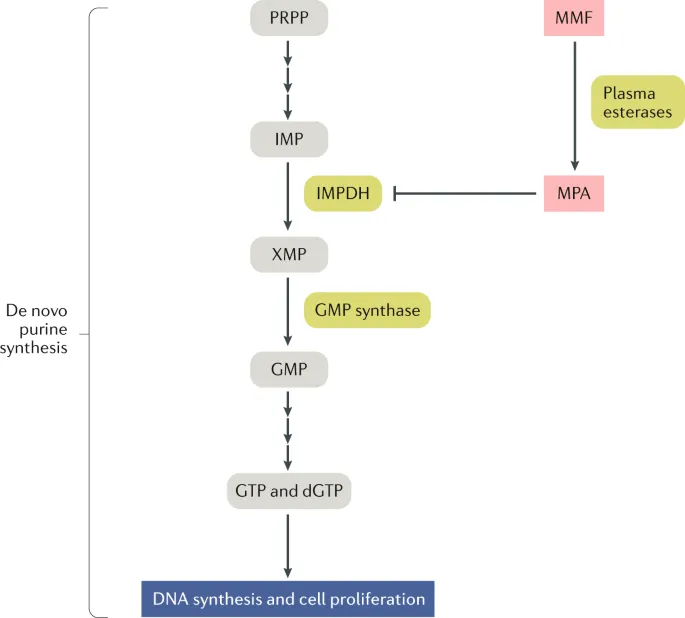
*Mycophenolate mofetil*
- Mycophenolate mofetil is an **antiproliferative agent** that inhibits purine synthesis, primarily affecting lymphocytes.
- Its common side effects are mainly **hematologic** (leukopenia, anemia) and **gastrointestinal** (diarrhea, nausea), not gingival hyperplasia or hypertension.
*Azathioprine*
- Azathioprine is a **purine analog** that impairs DNA synthesis and inhibits lymphocyte proliferation.
- Key side effects include **myelosuppression** (leukopenia, thrombocytopenia) and **hepatotoxicity**, which are not present here.
*Tacrolimus*
- Tacrolimus is also a **calcineurin inhibitor** that inhibits IL-2 transcription, similar to cyclosporine.
- While it can cause **hypertension** and **hyperlipidemia**, it is less commonly associated with **gingival hyperplasia** than cyclosporine.
*Prednisolone*
- Prednisolone is a **corticosteroid** used for immunosuppression, acting broadly on the immune system.
- Common side effects include **hyperglycemia**, **osteoporosis**, and **cataracts**, not specific gingival overgrowth.
Antimetabolites (azathioprine, mycophenolate) US Medical PG Question 6: A drug that inhibits mRNA synthesis has the well-documented side effect of red-orange body fluids. For which of the following is this drug used as monotherapy?
- A. Brucellosis
- B. Tuberculosis
- C. Methicillin-resistant staphylococcus aureus infection
- D. Mycobacterium avium intracellulare infection
- E. Neisseria meningitidis prophylaxis (Correct Answer)
Antimetabolites (azathioprine, mycophenolate) Explanation: ***Neisseria meningitidis prophylaxis***
- The drug described is **rifampin**, which inhibits bacterial **DNA-dependent RNA polymerase**, thereby blocking **mRNA synthesis** and causes characteristic **red-orange discoloration of body fluids** (tears, urine, sweat).
- Rifampin is used as **monotherapy** for **prophylaxis** against **Neisseria meningitidis** infection in close contacts of infected patients.
- This is the **only indication** where rifampin monotherapy is appropriate, as prophylaxis requires short-term use where resistance development is not a concern.
*Tuberculosis*
- Rifampin is a **first-line agent** for tuberculosis treatment and a cornerstone of all TB regimens.
- However, it is **never used as monotherapy** for TB due to rapid development of resistance.
- Standard TB treatment requires **multidrug therapy** with rifampin, isoniazid, pyrazinamide, and ethambutol (RIPE) for initial phase.
*Methicillin-resistant Staphylococcus aureus infection*
- Rifampin is sometimes used in **combination** with other antibiotics (e.g., vancomycin, daptomycin) to treat **MRSA infections**, especially those involving **prosthetic devices** or **biofilms**.
- It is **not used as monotherapy** for active MRSA infections due to extremely high rates of spontaneous resistance.
*Mycobacterium avium intracellulare infection*
- **Mycobacterium avium complex (MAC)** infections require a multidrug regimen, typically including **macrolides (azithromycin or clarithromycin)**, **ethambutol**, and sometimes **rifabutin** (a rifamycin derivative preferred over rifampin).
- **Monotherapy is never appropriate** for MAC infections due to resistance concerns and treatment failure.
*Brucellosis*
- **Brucellosis** treatment requires **combination therapy**, typically **doxycycline plus rifampin** for 6 weeks or longer.
- **Rifampin monotherapy** is inadequate for eradicating Brucella infection and leads to treatment failure and resistance development.
Antimetabolites (azathioprine, mycophenolate) US Medical PG Question 7: A 26-year-old G1P0 woman is brought to the emergency room by her spouse for persistently erratic behavior. Her spouse reports that she has been sleeping > 1 hour a night, and it sometimes seems like she’s talking to herself. She has maxed out their credit cards on baby clothes. The patient’s spouse reports this has been going on for over a month. Since first seeing a physician, she has been prescribed multiple first and second generation antipsychotics, but the patient’s spouse reports that her behavior has failed to improve. Upon examination, the patient is speaking rapidly and occasionally gets up to pace the room. She reports she is doing “amazing,” and that she is “so excited for the baby to get here because I’m going to be the best mom.” She denies illicit drug use, audiovisual hallucinations, or suicidal ideation. The attending psychiatrist prescribes a class of medication the patient has not yet tried to treat the patient’s psychiatric condition. In terms of this new medication, which of the following is the patient’s newborn most likely at increased risk for?
- A. Ototoxicity
- B. Attention deficit hyperactivity disorder
- C. Right ventricular atrialization (Correct Answer)
- D. Renal defects
- E. Caudal regression syndrome
Antimetabolites (azathioprine, mycophenolate) Explanation: ***Right ventricular atrialization***
- The patient's presentation of persistent **erratic behavior**, **reduced sleep**, rapid speech, and increased spending, enduring for over a month, is highly suggestive of a **manic episode** in the context of **bipolar I disorder**. Since antipsychotics have been ineffective, the next step is often **lithium**.
- **Lithium** exposure during the first trimester of pregnancy is associated with an increased risk of **Ebstein's anomaly**, a congenital heart defect characterized by **right ventricular atrialization** (displacement of the tricuspid valve leaflets into the right ventricle), leading to tricuspid regurgitation and right heart failure.
*Ototoxicity*
- **Ototoxicity** in newborns is typically associated with exposure to medications such as **aminoglycoside antibiotics** (e.g., gentamicin) or certain diuretics (e.g., furosemide) during pregnancy.
- Lithium is not known to cause ototoxicity as a primary birth defect.
*Attention deficit hyperactivity disorder*
- While various prenatal exposures can influence neurodevelopment, there is currently **no strong evidence** linking in-utero lithium exposure specifically to an increased risk of **ADHD** in offspring.
- ADHD is a complex neurodevelopmental disorder with multifactorial origins, including genetic and environmental factors.
*Renal defects*
- While lithium is primarily excreted by the kidneys and can cause **renal dysfunction** in adults (e.g., nephrogenic diabetes insipidus), it is not a prominent teratogen known to cause specific **structural renal defects** in newborns when exposed during pregnancy.
- Renal anomalies are more commonly associated with other medications or genetic syndromes.
*Caudal regression syndrome*
- **Caudal regression syndrome** is a severe congenital anomaly affecting the development of the lower spine and limbs. It is strongly associated with **poorly controlled maternal diabetes**.
- There is no established link between in-utero lithium exposure and caudal regression syndrome.
Antimetabolites (azathioprine, mycophenolate) US Medical PG Question 8: A 6-month-old infant boy is brought to the clinic for a check-up by a couple who recently adopted him from foster care. The biological mother was from a rehabilitation facility and was found incompetent to care for the child, hence he was handed over to foster care. No other information is available regarding his prenatal or birth history. On examination, his weight is found to be below the 3rd percentile. Physical appearance is remarkable for midfacial hypoplasia with a flattened nasal bridge, smooth philtrum, and thin lips. Auscultation reveals a grade 3/6 holosystolic murmur at the left lower sternal border. Developmental delay is noted as well. Which of the following teratogens is most likely to be associated with the infant's presentation?
- A. Lithium
- B. Tobacco
- C. Phenytoin
- D. Alcohol (Correct Answer)
- E. Cocaine
Antimetabolites (azathioprine, mycophenolate) Explanation: ***Alcohol***
- The combination of **facial dysmorphology** (midfacial hypoplasia, flattened nasal bridge, smooth philtrum, thin lips), **growth restriction** (weight below 3rd percentile), **cardiac defect** (holosystolic murmur), and **developmental delay** is highly characteristic of **Fetal Alcohol Syndrome (FAS)**.
- The biological mother's history of being in a **rehabilitation facility** suggests a potential history of substance abuse, making maternal alcohol consumption during pregnancy a strong possibility.
*Lithium*
- Maternal lithium use is associated with **Ebstein's anomaly**, a specific congenital heart defect, but typically does not cause the widespread facial dysmorphism and growth restriction seen in this infant.
- While it can cause cardiac defects, the overall constellation of findings points away from lithium as the primary teratogen.
*Tobacco*
- Maternal tobacco use is primarily associated with **low birth weight**, premature birth, and an increased risk of specific birth defects like **cleft lip and palate**.
- It does not typically cause the characteristic facial features, significant cardiac anomalies, or widespread developmental delay observed in this case.
*Phenytoin*
- Phenytoin, an anticonvulsant, can cause **fetal hydantoin syndrome**, characterized by specific facial features (e.g., hypertelorism, short nose, cleft lip/palate), **digital hypoplasia**, and intellectual disability.
- While it can cause some overlapping features like growth deficiency and developmental delay, the specific craniofacial features described for this infant are more typical of FAS.
*Cocaine*
- Cocaine exposure during pregnancy is associated with a range of problems including **preterm birth**, **placental abruption**, and **genitourinary defects**.
- Its teratogenic effects often involve vascular disruption leading to limb defects or cerebral infarctions, rather than the characteristic facial dysmorphology and cardiac defects described in this infant.
Antimetabolites (azathioprine, mycophenolate) US Medical PG Question 9: A 44-year-old man, with a history of intravenous (IV) drug use, presented to the emergency department due to worsening non-productive cough, exertional dyspnea, and night sweats. His cough started 3 weeks ago and progressively worsened. He is homeless and well-known by the hospital staff. He was previously admitted to the hospital after an overdose of opioids. He takes no medication. At the hospital, the vital signs included: blood pressure 101/68 mm Hg, heart rate 99/min, respiratory rate 20/min, oxygen saturation of 91% on room air, and oral temperature of 37.4°C (99.3°F). His chest X-ray showed left perihilar shadowing. The laboratory results included:
WBC count 8,800/mm3
Arterial pH 7.39
Rapid HIV testing positive with an elevated viral load
PaCO2 41 mm Hg
PaO2 76 mm Hg
He was admitted for the treatment of presumed sepsis and pneumonia, and he was immediately started on IV ceftriaxone. An induced sputum specimen shows multiple kidney bean-shaped cysts that are approximately 5 um. These cysts stain positive with methenamine silver. What is the preferred antibiotic therapeutic regimen for this condition?
- A. Intravenous liposomal amphotericin B with flucytosine
- B. Isoniazid, rifabutin, pyrazinamide and ethambutol
- C. Fluconazole with flucytosine
- D. Trimethoprim-sulfamethoxazole (Correct Answer)
- E. Clindamycin and primaquine, with adjunctive prednisone
Antimetabolites (azathioprine, mycophenolate) Explanation: ***Trimethoprim-sulfamethoxazole***
- The patient's symptoms (non-productive cough, dyspnea, night sweats), history of **IV drug use**, positive **HIV** test with elevated viral load, and chest X-ray findings are highly suggestive of **Pneumocystis pneumonia (PcP)**.
- The sputum analysis showing **kidney bean-shaped cysts** approximately 5 µm and staining positive with **methenamine silver** confirms PcP caused by *Pneumocystis jirovecii*. **Trimethoprim-sulfamethoxazole (TMP-SMX)** is the first-line treatment for PcP.
*Intravenous liposomal amphotericin B with flucytosine*
- This regimen is primarily used for severe fungal infections like **cryptococcal meningitis** or disseminated candidiasis, not *Pneumocystis jirovecii* pneumonia.
- While *Pneumocystis* was once considered a fungus, it is now classified as a unique organism requiring specific antiprotozoal-like treatment, not typical antifungal agents.
*Isoniazid, rifabutin, pyrazinamide and ethambutol*
- This is a standard multi-drug regimen for treating **active tuberculosis (TB)**.
- Although TB can cause similar pulmonary symptoms in immunocompromised patients, the sputum microscopy findings of *Pneumocystis* cysts rule out TB as the primary diagnosis requiring this specific regimen.
*Fluconazole with flucytosine*
- **Fluconazole** is an antifungal drug primarily used for candidiasis and cryptococcal infections, but it is **not effective** against *Pneumocystis jirovecii*.
- **Flucytosine** is also an antifungal agent used in combination with amphotericin B for severe fungal infections, but it has no role in treating PcP.
*Clindamycin and primaquine, with adjunctive prednisone*
- This combination is an **alternative treatment regimen** for moderate to severe PcP, often used in patients who cannot tolerate TMP-SMX due to adverse effects.
- While it is a valid treatment option, **TMP-SMX** remains the **preferred first-line therapy** due to its efficacy and broader availability, unless contraindications exist.
Antimetabolites (azathioprine, mycophenolate) US Medical PG Question 10: A 59-year-old man presents with intense, sharp pain in his toe for the past hour. He reports similar symptoms in the past and this is his 2nd visit to the emergency department this year with the same complaint. The patient is afebrile and the vital signs are within normal limits. On physical examination, there is significant erythema, swelling, warmth, and moderate pain on palpation of the right 1st toe. The remainder of the examination is unremarkable. A plain radiograph of the right foot reveals no abnormalities. Joint arthrocentesis of the inflamed toe reveals urate crystals. Laboratory studies show:
Serum glucose (random) 170 mg/dL
Sodium 140 mEq/L
Potassium 4.1 mEq/L
Chloride 100 mEq/L
Uric acid 7.2 mg/dL
Serum creatinine 0.8 mg/dL
Blood urea nitrogen 9 mg/dL
Cholesterol, total 170 mg/dL
HDL-cholesterol 43 mg/dL
LDL-cholesterol 73 mg/dL
Triglycerides 135 mg/dL
HDL: high-density lipoprotein; LDL: low-density lipoprotein
Ibuprofen is prescribed for the acute treatment of this patient's symptoms. He is also put on chronic therapy to prevent the recurrence of future attacks. Which of the following drugs is 1st-line for chronic therapy of gout?
- A. Methotrexate
- B. Indomethacin
- C. Probenecid
- D. Colchicine
- E. Allopurinol (Correct Answer)
Antimetabolites (azathioprine, mycophenolate) Explanation: ***Allopurinol***
- Allopurinol is a **xanthine oxidase inhibitor** that reduces uric acid production, making it the **first-line therapy** for **chronic gout management**.
- It effectively **lowers serum uric acid levels** to prevent recurrent attacks and dissolution of urate crystals.
*Methotrexate*
- Methotrexate is a **disease-modifying antirheumatic drug (DMARD)** primarily used in conditions like **rheumatoid arthritis** and **psoriasis**.
- It is **not indicated for gout** as it does not target uric acid metabolism.
*Indomethacin*
- Indomethacin is an **NSAID** commonly used for the **acute treatment of gout flares** due to its potent anti-inflammatory effects.
- It is **not suitable for chronic management** or prevention of gout due to potential long-term side effects and lack of effect on uric acid levels.
*Probenecid*
- Probenecid is a **uricosuric agent** that increases renal excretion of uric acid.
- While it lowers uric acid, it is typically considered a **second-line agent** for chronic gout, especially in patients with underexcretion of uric acid, or as an alternative to allopurinol if it cannot be tolerated.
*Colchicine*
- Colchicine is used for both **acute gout flares** and as **prophylaxis** during the initiation of uric acid-lowering therapy to prevent flares.
- It is **not a first-line drug for chronic gout management** as it does not lower uric acid levels; it primarily reduces inflammation.
More Antimetabolites (azathioprine, mycophenolate) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.