Immunosuppressants

On this page
💊 The Immunosuppressive Arsenal: Mastering Cellular Control
Immunosuppressants represent one of medicine's most elegant paradoxes: strategically weakening the immune system to save lives. You'll master how these agents target distinct molecular checkpoints-from calcineurin's T-cell activation switch to mTOR's growth control hub-transforming transplant rejection and autoimmune disease from death sentences into manageable conditions. By understanding each drug's precise mechanism, you'll predict side effects, avoid dangerous interactions, and deploy these powerful tools with the precision they demand in clinical practice.
📌 Remember: CALM - Calcineurin inhibitors, Antimetabolites, Lymphocyte depleting agents, MTOR inhibitors represent the four pillars of immunosuppression
The immunosuppressive landscape encompasses 13 major drug classes targeting distinct immune pathways. Calcineurin inhibitors achieve 80-90% one-year graft survival rates in kidney transplants, while TNF inhibitors demonstrate 70-80% clinical response rates in rheumatoid arthritis. mTOR inhibitors reduce lymphoma risk by 60% compared to calcineurin inhibitors in post-transplant patients.
- Mechanism-Based Classification
- T-cell targeting agents (65% of immunosuppressive protocols)
- Calcineurin inhibitors: Block IL-2 transcription
- Costimulation blockers: Prevent T-cell activation
- T-cell depleting antibodies: Direct lymphocyte elimination
- B-cell targeting agents (25% of protocols)
- Anti-CD20 monoclonals: B-cell depletion
- Complement inhibitors: Block terminal pathway
- Cytokine modulators (35% of inflammatory conditions)
- TNF inhibitors: Block master inflammatory cytokine
- IL-6 inhibitors: Target acute phase response
- JAK inhibitors: Interrupt cytokine signaling
- T-cell targeting agents (65% of immunosuppressive protocols)
| Drug Class | Primary Target | Onset Time | Peak Effect | Monitoring Parameter | Therapeutic Range |
|---|---|---|---|---|---|
| Calcineurin Inhibitors | T-cell activation | 2-4 hours | 1-3 hours | Trough levels | 5-15 ng/mL (tacrolimus) |
| mTOR Inhibitors | Cell proliferation | 1-2 weeks | 4-6 weeks | Trough levels | 4-12 ng/mL (sirolimus) |
| Antimetabolites | DNA synthesis | 1-3 months | 3-6 months | CBC, LFTs | ANC >1500/μL |
| TNF Inhibitors | Cytokine blockade | 2-8 weeks | 12-16 weeks | Clinical response | 70-80% ACR20 |
| Corticosteroids | Gene transcription | 30 minutes | 2-8 hours | Clinical signs | Varies by indication |
💡 Master This: Every immunosuppressive protocol balances 3 competing priorities - preventing rejection (>90% efficacy), minimizing toxicity (<15% serious adverse events), and preserving infection immunity (<5% opportunistic infections)
The foundation of immunosuppressive mastery lies in understanding that each drug class targets specific immune checkpoints with measurable precision. Connect this mechanistic understanding through targeted pathway inhibition to predict both therapeutic efficacy and adverse effect profiles.
💊 The Immunosuppressive Arsenal: Mastering Cellular Control
⚡ T-Cell Command Center: Calcineurin's Molecular Switchboard
📌 Remember: CHAIN - Calcium activates calcineurin, Hydrolyzes NFAT phosphates, Allows nuclear translocation, Initiates IL-2 transcription, New T-cell proliferation
-
Cyclosporine Mechanism (60% of transplant centers)
- Binds cyclophilin A with nanomolar affinity
- Forms ternary complex blocking calcineurin active site
- Inhibits >95% of IL-2 production at therapeutic levels
- Trough target: 100-300 ng/mL (kidney transplant)
- Peak target: 800-1400 ng/mL (2-hour post-dose)
- Half-life: 8-27 hours (highly variable)
-
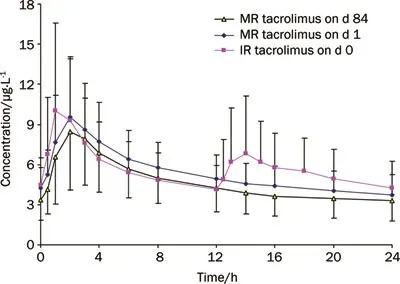
Tacrolimus Mechanism (75% of new transplant protocols)
- Binds FK506-binding protein (FKBP12)
- 10-100x more potent than cyclosporine
- Superior graft survival: +5-8% at 5 years
- Trough target: 5-15 ng/mL (maintenance)
- Trough target: 8-20 ng/mL (early post-transplant)
- Half-life: 12-15 hours (more predictable)
| Parameter | Cyclosporine | Tacrolimus | Clinical Significance |
|---|---|---|---|
| Potency | 1x (reference) | 10-100x | Lower dosing requirements |
| Bioavailability | 30% (variable) | 25% (consistent) | Food effect considerations |
| Protein Binding | 90% | 99% | Drug interaction potential |
| Metabolism | CYP3A4 | CYP3A4 | Identical interaction profile |
| Nephrotoxicity | 60-80% | 40-60% | Tacrolimus preferred |
| Neurotoxicity | 10-15% | 20-30% | Dose-dependent tremor |
💡 Master This: Calcineurin inhibitor nephrotoxicity occurs through 2 distinct mechanisms - acute vasoconstriction (reversible within 24-48 hours) and chronic interstitial fibrosis (irreversible after 6-12 months of exposure)
The precision of calcineurin inhibition allows selective T-cell suppression while preserving innate immunity. Connect this targeted mechanism through therapeutic drug monitoring to optimize the balance between efficacy and toxicity in clinical practice.
⚡ T-Cell Command Center: Calcineurin's Molecular Switchboard
🎯 Cytokine Storm Control: TNF and Beyond
📌 Remember: FIRE - First-line TNF blockers, IL-6 for systemic inflammation, Receptor antagonists (IL-1), Emergent JAK inhibitors for multiple cytokines
- TNF Inhibitor Classes (5 FDA-approved agents)
- Monoclonal antibodies: 3 agents (infliximab, adalimumab, golimumab)
- Half-life: 8-20 days
- Dosing: Every 2-8 weeks
- Immunogenicity: 5-15% develop neutralizing antibodies
- Fusion proteins: 1 agent (etanercept)
- Half-life: 3-5 days
- Dosing: Weekly to twice weekly
- Immunogenicity: <5% neutralizing antibodies
- Certolizumab: PEGylated Fab fragment
- Half-life: 14 days
- Pregnancy category: B (no placental transfer)
- Monoclonal antibodies: 3 agents (infliximab, adalimumab, golimumab)
| TNF Inhibitor | Half-life | Dosing Interval | ACR20 Response | Serious Infection Risk | Annual Cost |
|---|---|---|---|---|---|
| Infliximab | 8-10 days | 8 weeks | 75-80% | 4-6% | $25,000-35,000 |
| Adalimumab | 14 days | 2 weeks | 70-75% | 3-5% | $30,000-40,000 |
| Etanercept | 3-5 days | 1 week | 65-70% | 2-4% | $28,000-38,000 |
| Golimumab | 14 days | 4 weeks | 70-75% | 3-5% | $32,000-42,000 |
| Certolizumab | 14 days | 2-4 weeks | 70-75% | 4-6% | $35,000-45,000 |
- Target: IL-6 receptor blockade
- Indication: RA, giant cell arteritis, cytokine release syndrome
- Efficacy: 70-80% ACR20 response in RA
- Monitoring: Monthly lipids and liver enzymes
- LDL increases 15-25% (paradoxical but benign)
- ALT elevation >3x ULN in 5-10%
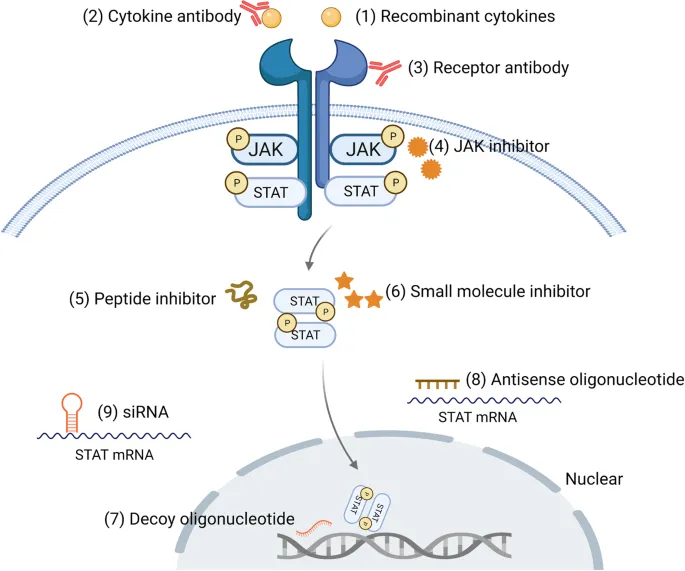
- JAK Inhibitors (4 FDA-approved agents)
- Mechanism: Block JAK1/2/3/TYK2 kinases
- Advantage: Oral administration, rapid onset
- Efficacy: 60-75% ACR20 response
- Black box warnings: Thrombosis risk (0.3-0.5% annually)
- Age >65 years: 2x increased risk
- Cardiovascular risk factors: 3x increased risk
⭐ Clinical Pearl: Pre-treatment screening for latent tuberculosis is mandatory for all TNF inhibitors, as reactivation risk increases 2-8 fold with 25% mortality if unrecognized
💡 Master This: Cytokine inhibitors demonstrate paradoxical effects - blocking inflammation can unmask latent infections (TB, hepatitis B) while simultaneously improving cardiovascular outcomes through 30-40% reduction in major adverse cardiac events
Understanding cytokine networks enables prediction of both therapeutic responses and infection risks. Connect this knowledge through careful patient selection to maximize clinical benefits while minimizing serious adverse events.
🎯 Cytokine Storm Control: TNF and Beyond
🧬 Cellular Assembly Line: Antimetabolite Precision
📌 Remember: PURINES - Purine synthesis targeted, Uracil incorporation blocked, Rapidly dividing cells affected, IMPDH enzyme inhibited, Nucleotide depletion occurs, Effector cells suppressed, Selective lymphocyte impact
-
Azathioprine Mechanism (Classic antimetabolite)
- Prodrug converted to 6-mercaptopurine (6-MP)
- Inhibits de novo purine synthesis at multiple steps
- Preferentially affects T-cells > B-cells
- Dosing: 1-3 mg/kg/day (target 2-2.5 mg/kg)
- Onset: 6-12 weeks for full effect
- Half-life: 3-5 hours (6-MP), 5 days (active metabolites)
- TPMT polymorphisms affect 8-10% of population
- Deficient activity: 0.3% (severe toxicity risk)
- Intermediate activity: 10% (dose reduction needed)
-
Mycophenolate Mechanism (Modern standard)
- Inhibits IMPDH type II (lymphocyte-specific isoform)
- Blocks guanosine synthesis selectively
- 10-100x more selective than azathioprine
- MMF dosing: 1000-1500 mg twice daily
- EC-MPS dosing: 720-1080 mg daily
- Therapeutic level: 1-3.5 mg/L (MPA AUC)
| Parameter | Azathioprine | Mycophenolate | Clinical Advantage |
|---|---|---|---|
| Selectivity | Moderate | High (10-100x) | Fewer off-target effects |
| GI Toxicity | 15-20% | 30-45% | Dose-limiting for MMF |
| Bone Marrow | 5-10% | 2-5% | Better hematologic profile |
| Hepatotoxicity | 5-15% | <2% | Safer liver profile |
| Teratogenicity | Category D | Category D | Both require contraception |
| Drug Interactions | Allopurinol (4x ↑) | Antacids (40% ↓) | Different interaction profiles |
- Complete blood count: Every 2-4 weeks initially
- Target ANC: >1500/μL
- Target platelets: >100,000/μL
- Dose reduction if ANC <1000/μL
- Liver function tests: Monthly for first 3 months
- Hold if ALT >3x upper limit normal
- Resume at 50% dose when normalized
- TPMT genotyping: Before azathioprine initiation
- Deficient: Contraindicated
- Intermediate: Start 50% standard dose
⭐ Clinical Pearl: Mycophenolate-associated diarrhea affects 30-45% of patients and represents the #1 cause of drug discontinuation, but switching from MMF to enteric-coated MPS reduces GI toxicity by 40-50%
💡 Master This: Antimetabolite toxicity follows predictable patterns - GI effects peak at 2-4 weeks, bone marrow suppression at 4-8 weeks, and hepatotoxicity at 8-12 weeks, allowing proactive monitoring and dose adjustments
The selective targeting of proliferating immune cells makes antimetabolites ideal maintenance immunosuppressants. Connect this mechanism through therapeutic drug monitoring to optimize dosing while minimizing dose-limiting toxicities.
🧬 Cellular Assembly Line: Antimetabolite Precision
🔄 Growth Control Matrix: mTOR's Cellular Checkpoint
📌 Remember: GROWTH - Growth factor signals, Rapamycin blocks mTOR, Oligomerization prevented, With protein synthesis halted, T-cell proliferation stops, Halting immune responses
-
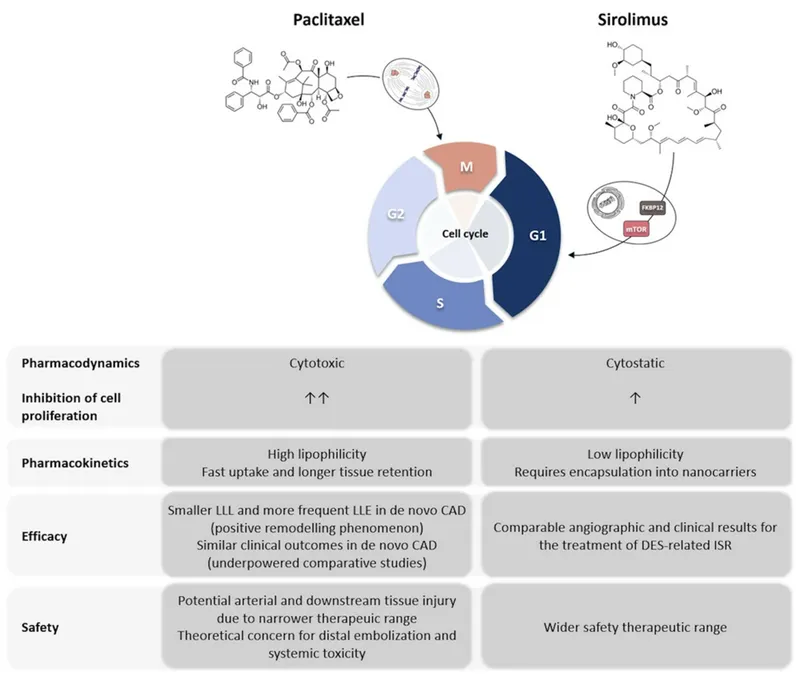
Sirolimus (Rapamycin) (Prototype mTOR inhibitor)
- Binds FKBP12 (same as tacrolimus)
- Forms complex inhibiting mTORC1 specifically
- Blocks S6K1 and 4E-BP1 phosphorylation
- Loading dose: 6-15 mg on day 1
- Maintenance: 2-5 mg daily
- Target trough: 4-12 ng/mL (varies by indication)
- Half-life: 60-70 hours (very long)
-
Everolimus (Optimized analog)
- Shorter half-life: 18-35 hours
- More predictable pharmacokinetics
- Twice daily dosing: 0.75-1.5 mg BID
- Target trough: 3-8 ng/mL
- Less drug interactions than sirolimus
- FDA-approved for multiple indications
| Parameter | Sirolimus | Everolimus | Clinical Impact |
|---|---|---|---|
| Half-life | 60-70 hours | 18-35 hours | Dosing frequency |
| Bioavailability | 15% (variable) | 30% (consistent) | Dose predictability |
| Food Effect | 35% reduction | 22% reduction | Administration timing |
| CYP3A4 Substrate | Strong | Moderate | Drug interaction risk |
| Wound Healing | Delayed (30%) | Delayed (20%) | Surgical considerations |
| Hyperlipidemia | 60-80% | 50-70% | Monitoring requirements |
- Nephroprotective: Preserves GFR long-term
- Anti-neoplastic: 60-70% reduction in post-transplant malignancy
- Anti-viral: Reduces CMV reactivation by 40-50%
- Cardiac protection: Reduces coronary artery vasculopathy
- Drug-eluting stents: Prevent restenosis (<5% vs 20-30%)
- LAM treatment: Stabilizes lung function decline
- Characteristic Toxicities
- Hyperlipidemia: 60-80% incidence
- Total cholesterol increases 30-50%
- Triglycerides increase 50-100%
- Requires statin therapy in >70%
- Proteinuria: 20-30% develop significant proteinuria
- Usually non-progressive
- ACE inhibitors provide protection
- Pneumonitis: 5-15% incidence (dose-dependent)
- Non-infectious inflammatory process
- Requires drug discontinuation
- Hyperlipidemia: 60-80% incidence
⭐ Clinical Pearl: mTOR inhibitor conversion from calcineurin inhibitors improves long-term graft function but requires careful timing - conversion >3 months post-transplant reduces acute rejection risk to <10%
💡 Master This: mTOR inhibitors demonstrate context-dependent effects - immunosuppressive in lymphocytes, anti-proliferative in smooth muscle cells, and pro-autophagy in aging cells, explaining their diverse clinical applications beyond transplantation
The dual role of mTOR in immune activation and cellular growth makes these inhibitors uniquely valuable for long-term immunosuppression. Connect this mechanistic understanding through careful patient selection to optimize both graft survival and patient outcomes.
🔄 Growth Control Matrix: mTOR's Cellular Checkpoint
🎪 Antibody Precision Strike: Cellular Elimination Protocols
📌 Remember: DEPLETE - Depleting antibodies target surface markers, Eliminate specific cell populations, Potent immunosuppression achieved, Lymphocyte counts drop dramatically, Effects last weeks to months, Timing critical for efficacy, Expensive but highly effective
-
T-Cell Depleting Agents
- Alemtuzumab (Anti-CD52)
- Targets CD52 on all lymphocytes
- Single dose: 30 mg IV (induction)
- Depletes >99% T-cells for 6-12 months
- Profound lymphopenia: <100 cells/μL
- Antithymocyte Globulin (ATG)
- Polyclonal rabbit antibodies
- Dose: 1.5 mg/kg daily for 3-7 days
- Targets multiple T-cell antigens
- Cytokine release syndrome: 60-80% incidence
- Alemtuzumab (Anti-CD52)
-
B-Cell Depleting Agents
- Rituximab (Anti-CD20)
- Depletes mature B-cells (not plasma cells)
- Standard dose: 375 mg/m² weekly × 4
- B-cell recovery: 6-12 months
- Preserves humoral memory (plasma cells CD20-negative)
- Ofatumumab (Second-generation anti-CD20)
- Higher affinity binding to CD20
- Enhanced complement activation
- Effective in rituximab-resistant cases
- Rituximab (Anti-CD20)
| Antibody | Target | Depletion Duration | Primary Indication | Infusion Reactions | Annual Cost |
|---|---|---|---|---|---|
| Alemtuzumab | CD52 | 6-12 months | MS, transplant | 90-95% | $50,000-70,000 |
| ATG | Multiple T-cell | 2-4 weeks | Rejection treatment | 60-80% | $15,000-25,000 |
| Rituximab | CD20 | 6-12 months | Autoimmune, lymphoma | 30-50% | $20,000-30,000 |
| Basiliximab | CD25 | 4-6 weeks | Transplant induction | <5% | $8,000-12,000 |
| Daclizumab | CD25 | 8-12 weeks | Discontinued | <5% | N/A |
- Basiliximab: Chimeric monoclonal antibody
- Dose: 20 mg on days 0 and 4
- Blocks IL-2 receptor α-chain
- Minimal side effects (<5% infusion reactions)
- Standard induction in low-risk transplants
- Mechanism: Competitive inhibition of IL-2 binding
- Saturates receptors for 4-6 weeks
- No cell depletion (just functional blockade)
- Infusion Reaction Management
- Premedication protocol:
- Methylprednisolone 500-1000 mg IV
- Diphenhydramine 50 mg IV
- Acetaminophen 650 mg PO
- Cytokine release syndrome (CRS)
- Fever >38.5°C in 60-90%
- Hypotension requiring pressors: 10-20%
- Tocilizumab for severe CRS
- Premedication protocol:
⭐ Clinical Pearl: Alemtuzumab induction provides equivalent 5-year graft survival to conventional immunosuppression while allowing steroid-free and calcineurin inhibitor-minimization protocols in >80% of patients
💡 Master This: Depleting antibodies create immunological windows lasting weeks to months, requiring careful infection prophylaxis with PCP prevention for 6-12 months and CMV monitoring for 12-24 months post-treatment
The precision of antibody-mediated cell depletion enables targeted immunosuppression with predictable kinetics. Connect this knowledge through appropriate patient selection and monitoring protocols to maximize therapeutic benefits while minimizing infectious complications.
🎪 Antibody Precision Strike: Cellular Elimination Protocols
🎯 Immunosuppressive Mastery: The Clinical Command Center
📌 Remember: MASTER - Monitor drug levels religiously, Adjust for interactions and toxicity, Screen for infections proactively, Taper gradually when indicated, Educate patients thoroughly, Recognize rejection early
- Essential Clinical Arsenal
- Therapeutic Drug Monitoring Targets
- Tacrolimus trough: 5-15 ng/mL (maintenance)
- Sirolimus trough: 4-12 ng/mL (varies by indication)
- Mycophenolic acid AUC: 30-60 mg·h/L
- Cyclosporine C2: 800-1400 ng/mL (2-hour post-dose)
- Critical Drug Interactions (>50 clinically significant)
- CYP3A4 inhibitors: Increase CNI/mTORi levels 2-5x
- CYP3A4 inducers: Decrease levels 50-80%
- Proton pump inhibitors: Reduce MMF absorption 25-40%
- Therapeutic Drug Monitoring Targets
| Clinical Scenario | First-Line Protocol | Monitoring Priority | Success Rate | Key Pearls |
|---|---|---|---|---|
| Low-risk kidney transplant | Tacrolimus + MMF + Steroids | Trough levels, GFR | 95% 1-year survival | Steroid withdrawal at 6 months |
| High-risk heart transplant | Induction + Triple therapy | Rejection surveillance | 85% 1-year survival | Endomyocardial biopsy protocol |
| Rheumatoid arthritis | MTX + TNF inhibitor | TB screening, response | 70-80% ACR20 | Combination superior to monotherapy |
| Lupus nephritis | MMF + Corticosteroids | Proteinuria, GFR | 80% complete remission | Avoid cyclophosphamide if possible |
| Severe psoriasis | TNF inhibitor monotherapy | PASI response | 75% PASI-75 | Screen for psoriatic arthritis |
- Acute cellular rejection
- Creatinine rise >25% from baseline
- Fever, graft tenderness in 60-70%
- Biopsy confirmation required
- Treatment: High-dose steroids or ATG
- Antibody-mediated rejection
- DSA positivity with C4d staining
- Worse prognosis than cellular rejection
- Treatment: Plasmapheresis + IVIG + rituximab
- Infection Risk Stratification
- High-risk period: First 6 months post-transplant
- CMV reactivation: 30-60% without prophylaxis
- PCP pneumonia: 5-15% without prophylaxis
- Bacterial infections: 40-60% in first year
- Prophylaxis protocols
- Valganciclovir: 900 mg daily for 3-6 months
- Trimethoprim-sulfamethoxazole: Daily for 6-12 months
- Nystatin: Oral thrush prevention
- High-risk period: First 6 months post-transplant
⭐ Clinical Pearl: Immunosuppressive drug interactions cause >30% of therapeutic failures, with CYP3A4 interactions being the most clinically significant - always check interaction potential before prescribing any new medication
💡 Master This: Successful immunosuppression requires dynamic optimization - initial protocols achieve rapid control, maintenance regimens preserve function, and long-term management minimizes toxicity while maintaining efficacy thresholds >85%
The integration of mechanistic knowledge with clinical monitoring creates a systematic approach to immunosuppressive management that optimizes patient outcomes across diverse clinical scenarios.
🎯 Immunosuppressive Mastery: The Clinical Command Center
Practice Questions: Immunosuppressants
Test your understanding with these related questions
Two weeks after undergoing allogeneic stem cell transplant for multiple myeloma, a 55-year-old man develops a severely pruritic rash, abdominal cramps, and profuse diarrhea. He appears lethargic. Physical examination shows yellow sclerae. There is a generalized maculopapular rash on his face, trunk, and lower extremities, and desquamation of both soles. His serum alanine aminotransferase is 115 U/L, serum aspartate aminotransferase is 97 U/L, and serum total bilirubin is 2.7 mg/dL. Which of the following is the most likely underlying cause of this patient's condition?












