Thyroid hormone replacements US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Thyroid hormone replacements. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Thyroid hormone replacements US Medical PG Question 1: A 39-year-old female presents to the clinic with the complaints of dry skin for a few months. She adds that she also has constipation for which she started eating vegetables and fruits but with no improvement. She lives with her husband and children who often complain when she turns the air conditioning to high as she cannot tolerate low temperatures. She has gained 5 kgs (11.2 lb) since her last visit 2 months back although her diet has not changed much. Her past medical history is relevant for cardiac arrhythmias and diabetes. She is on several medications currently. Her temperature is 98.6° F (37° C), respirations are 15/min, pulse is 57/min and blood pressure is 132/98 mm Hg. A physical examination is within normal limits. Thyroid function test results are given below:
Serum
TSH: 13.0 μU/mL
Thyroxine (T4): 3.0 μg/dL
Triiodothyronine (T3): 100 ng/dL
Which of the following medications is most likely to be responsible for her symptoms?
- A. Amiodarone (Correct Answer)
- B. Digoxin
- C. Metformin
- D. Theophylline
- E. Warfarin
Thyroid hormone replacements Explanation: ***Amiodarone***
- Amiodarone is a known cause of both **hypothyroidism** and **hyperthyroidism** due to its iodine content and direct toxic effects on the thyroid gland. The patient's symptoms (dry skin, constipation, **cold intolerance**, **weight gain**, bradycardia) and thyroid function tests (high TSH, low T4, low T3) are highly consistent with drug-induced hypothyroidism.
- The patient's history of **cardiac arrhythmias** makes amiodarone a plausible medication she would be taking, as it is a common antiarrhythmic drug.
*Digoxin*
- Digoxin is primarily used to treat **heart failure** and certain arrhythmias, but it does not typically cause thyroid dysfunction.
- Its common side effects include gastrointestinal upset, visual disturbances, and various arrhythmias, which do not align with the patient's predominant symptoms of hypothyroidism.
*Metformin*
- Metformin is an oral hypoglycemic agent used to treat **Type 2 diabetes**, a condition the patient also has.
- It does not have substantial effects on thyroid hormone synthesis or metabolism and is not associated with hypothyroidism or hyperthyroidism.
*Theophylline*
- Theophylline is a bronchodilator used in the treatment of **asthma** and **COPD**.
- It is not known to cause thyroid dysfunction, and its side effects mainly involve the central nervous system, gastrointestinal tract, and cardiovascular system.
*Warfarin*
- Warfarin is an **anticoagulant** prescribed to prevent blood clots.
- It has no direct known interaction with thyroid hormone synthesis or metabolism and is not associated with thyroid dysfunction.
Thyroid hormone replacements US Medical PG Question 2: An investigator is studying a drug that acts on the thyroid hormone pathway. Levels of serum free T3 and T4 in healthy participants are measured before and after administration of the drug. After administration, there is a decrease in the average serum free T3 level, while the average serum free T4 level is increased compared to initial serum studies. Inhibition of which of the following is the most likely mechanism of action of this drug?
- A. Thyroid-stimulating hormone
- B. Follicular iodotyrosine deiodinase
- C. Follicular thyroid peroxidase
- D. Peripheral 5'-deiodinase (Correct Answer)
- E. Follicular thyroid proteases
Thyroid hormone replacements Explanation: ***Peripheral 5'-deiodinase***
- Inhibition of **peripheral 5'-deiodinase** would decrease the conversion of **T4 to T3** in the periphery, resulting in lower **free T3** and higher **free T4** levels.
- This enzyme is crucial for activating T4 into the more potent T3, and its blockade explains the observed changes in hormone levels.
*Thyroid-stimulating hormone*
- Inhibition of **TSH** would lead to a decrease in the production and release of both **T3 and T4** from the thyroid gland.
- This contradicts the observed increase in **free T4** levels.
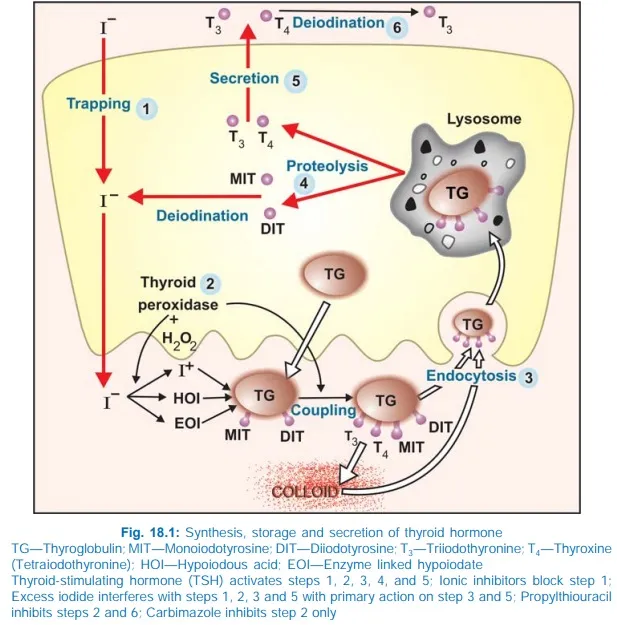
*Follicular iodotyrosine deiodinase*
- This enzyme is involved in recycling iodine from **monoiodotyrosine (MIT)** and **diiodotyrosine (DIT)** within the thyroid follicular cells, which is important for efficient thyroid hormone synthesis.
- Its inhibition would primarily affect iodine availability and synthesis, not directly lead to increased T4 and decreased T3 in the periphery.
*Follicular thyroid peroxidase*
- **Thyroid peroxidase (TPO)** is critical for the **iodination of tyrosine residues** on thyroglobulin and the **coupling of MIT and DIT** to form T3 and T4.
- Inhibition of TPO would decrease the synthesis of both **T3 and T4**, contrary to the observed increase in **free T4**.
*Follicular thyroid proteases*
- **Thyroid proteases** cleave thyroglobulin to release mature **T3 and T4** into the bloodstream.
- Inhibition of these proteases would lead to a decrease in the release of both **T3 and T4**, which does not align with the observed increase in **free T4**.
Thyroid hormone replacements US Medical PG Question 3: A previously healthy 25-year-old woman comes to the physician because of a 1-month history of palpitations that occur on minimal exertion and sometimes at rest. She has no chest discomfort or shortness of breath. She feels nervous and irritable most of the time and attributes these feelings to her boyfriend leaving her 2 months ago. Since then she has started exercising more frequently and taking an herbal weight-loss pill, since which she has lost 6.8 kg (15 lb) of weight. She finds it hard to fall asleep and awakens 1 hour before the alarm goes off each morning. She has been drinking 2 to 3 cups of coffee daily for the past 7 years and has smoked one pack of cigarettes daily for the past 3 years. Her temperature is 37.4°C (99.4°F), pulse is 110/min, respirations are 18/min, and blood pressure is 150/70 mm Hg. Examination shows moist palms. Neurologic examination shows a fine resting tremor of the hands. Deep tendon reflexes are 3+ with a shortened relaxation phase. Which of the following is the most likely cause of this patient's symptoms?
- A. Exogenous hyperthyroidism (Correct Answer)
- B. Pheochromocytoma
- C. Hashimoto thyroiditis
- D. Coffee consumption
- E. Generalized anxiety disorder
Thyroid hormone replacements Explanation: ***Exogenous hyperthyroidism***
- The patient's symptoms including **palpitations, weight loss, nervousness, irritability, insomnia**, and physical findings like **tachycardia, moist palms, fine tremor**, and **hyperreflexia with shortened relaxation phase** are highly indicative of **hyperthyroidism**.
- The use of an **herbal weight-loss pill** strongly suggests the possibility of exogenous thyroid hormone intake or other thyroid-stimulating substances within the pill, leading to **exogenous hyperthyroidism**.
*Pheochromocytoma*
- While **palpitations** and **hypertension** can occur, **pheochromocytoma** is typically characterized by paroxysmal episodes of severe headaches, sweating, and anxiety.
- The chronic nature of the patient's symptoms, along with significant **weight loss** and **hyperreflexia**, are less typical for **pheochromocytoma**.
*Hashimoto thyroiditis*
- **Hashimoto thyroiditis** typically causes **hypothyroidism**, characterized by symptoms like weight gain, fatigue, cold intolerance, and bradycardia.
- While it can sometimes have a transient hyperthyroid phase (hashitoxicosis), the overall clinical picture here is more consistent with sustained **hyperthyroidism**, especially given the suspected external factor.
*Coffee consumption*
- Although **caffeine** can cause palpitations, nervousness, and insomnia, the severity and breadth of this patient's symptoms, including significant **weight loss, hyperreflexia**, and **moist palms**, extend far beyond what would typically be attributed solely to coffee intake, especially given her chronic coffee use.
- The new onset and progression of these symptoms, coinciding with the herbal pill, points to a stronger underlying cause.
*Generalized anxiety disorder*
- **Generalized anxiety disorder (GAD)** can explain nervousness, irritability, and insomnia, but it does not typically cause **significant weight loss** or objective physical findings such as **tachycardia, moist palms, fine tremor, and hyperreflexia**.
- These physical signs are hallmarks of a physiological rather than purely psychological condition.
Thyroid hormone replacements US Medical PG Question 4: A 50-year-old woman comes to the physician because of palpitations and irritability. Over the past 4 months, she has had several episodes of heart racing and skipping beats that lasted between 30 seconds and several hours. She has also been arguing with her husband more, often about the temperature being too warm. The patient has also lost 8.8-kg (19.4-lb) over the past 4 months, despite being less strict with her diet. She has mild asthma treated with inhaled bronchodilators. Her pulse is 102/min and blood pressure is 148/98 mm Hg. On physical examination, the skin is warm and moist. A mass is palpated in the anterior neck area. On laboratory studies, thyroid stimulating hormone is undetectable and there are antibodies against the thyrotropin-receptor. Thyroid scintigraphy shows diffusely increased iodine uptake. Two weeks later, a single oral dose of radioactive iodine is administered. This patient will most likely require which of the following in the long-term?
- A. Propranolol therapy
- B. Near-total thyroidectomy
- C. L-thyroxine therapy (Correct Answer)
- D. Methimazole therapy
- E. Estrogen replacement therapy
Thyroid hormone replacements Explanation: * ***L-thyroxine therapy***
* Radioactive iodine ablation for **Graves' disease** often leads to **permanent hypothyroidism**, necessitating **lifelong thyroid hormone replacement** with levothyroxine.
* The patient presents with classic **hyperthyroidism** symptoms (palpitations, irritability, weight loss, heat intolerance, warm/moist skin, goiter, undetectable TSH, positive **TSH receptor antibodies**, diffuse uptake on scintigraphy), treated with radioactive iodine.
* *Propranolol therapy*
* Propranolol is a **beta-blocker** used for symptomatic relief of hyperthyroidism, particularly palpitations and tremors.
* It does **not treat the underlying cause** of hyperthyroidism or subsequent hypothyroidism, and therefore is not a long-term solution after successful radioactive iodine therapy.
* *Near-total thyroidectomy*
* A near-total thyroidectomy is a surgical option for hyperthyroidism, especially in cases of very large goiters, contraindications to radioactive iodine, or malignancy.
* While it also often leads to **hypothyroidism** requiring long-term L-thyroxine, it was **not the chosen treatment modality** in this scenario (radioactive iodine was administered).
* *Methimazole therapy*
* Methimazole is an **antithyroid drug** used to decrease thyroid hormone synthesis in hyperthyroidism.
* It is used as a **primary treatment for hyperthyroidism** or as preparation for definitive therapy like radioactive iodine or surgery; it is not a long-term treatment after successful radioactive iodine ablation has induced hypothyroidism.
* *Estrogen replacement therapy*
* Estrogen replacement therapy is used for symptoms of **menopause** or to prevent osteoporosis, but it has no direct role in the management of thyroid disorders.
* The patient's symptoms are clearly indicative of a **thyroid pathology**, not primarily menopausal symptoms.
Thyroid hormone replacements US Medical PG Question 5: A 64-year-old man who has not seen a physician in over 20 years presents to your office complaining of recently worsening fatigue and weakness, a decreased appetite, distended abdomen, and easy bruising. His family history is notable for a mother with Hashimoto's thyroiditis, a sister with lupus and a brother with type II diabetes. On further questioning, the patient discloses a history of prior alcoholism as well as intravenous drug use, though he currently only smokes a pack per day of cigarettes. On physical exam, you note the following findings (see Figures A-C) as well as several ecchymoses and telangiectasias. As the patient has not seen a physician in many years, you obtain the following laboratory studies:
Leukocyte count: 4,100/mm^3
Hemoglobin: 9.6 g/dL
Platelet count: 87,000/mm^3
Prothrombin time (PT): 21.0 seconds
International Normalized Ratio (INR): 1.8
Serum:
Creatinine: 1.7 mg/dL
Total bilirubin: 3.2 mg/dL
Aspartate aminotransferase (AST): 225 U/L
Alanine aminotransferase (ALT): 103 U/L
Alkaline phosphatase: 162 U/L
Albumin: 2.6 g/dL
Serum thyroxine (T4): 3.1 µg/dL
Thyroid-stimulating hormone (TSH): 3.4 µU/mL
What is the cause of this patient’s low serum thyroxine?
- A. Transient central hypothyroidism (sick euthyroid syndrome)
- B. Autoimmune thyroiditis
- C. Decreased liver synthetic function (Correct Answer)
- D. Acute hepatitis causing an elevation in thyroxine-binding globulin
- E. Urinary loss of thyroxine-binding globulin due to nephrotic syndrome
Thyroid hormone replacements Explanation: ***Decreased liver synthetic function***
- A low **serum albumin** (2.6 g/dL) is a direct measure of decreased liver synthetic function, which impairs the liver's ability to produce **thyroxine-binding globulins (TBGs)**. Reduced TBGs lead to lower total serum thyroxine (T4) because less T4 is bound and transported in the blood.
- The patient's history of **alcoholism**, current **cirrhosis** (ascites, easy bruising, thrombocytopenia, coagulopathy), and elevated liver enzymes further support severe liver dysfunction as the cause of reduced TBG synthesis and, consequently, low total T4.
*Transient central hypothyroidism (sick euthyroid syndrome)*
- **Sick euthyroid syndrome** typically presents with low total T4, but also often low T3 and TSH that can be normal, low, or slightly elevated, reflecting hypothalamic-pituitary axis dysfunction in the context of severe illness. However, the primary driver here is the severe liver synthetic dysfunction.
- While this patient is severely ill, the pronounced **hypoalbuminemia** directly points to a significant **hepatic synthetic defect** as the more direct cause of the low total T4.
*Autoimmune thyroiditis*
- **Autoimmune thyroiditis**, such as **Hashimoto's thyroiditis**, causes hypothyroidism by destroying thyroid tissue, leading to high TSH and low T4. This patient's TSH is normal (3.4 µU/mL), effectively ruling out primary hypothyroidism.
- While there is a family history of Hashimoto's, the patient's normal TSH level indicates that his low T4 is not due to primary thyroid failure.
*Acute hepatitis causing an elevation in thyroxine-binding globulin*
- **Acute hepatitis** can cause elevated transaminases, but it typically does not lead to an increase in **thyroxine-binding globulin (TBG)**. Liver inflammation acutely, if severe, might impair synthesis or function, but would not elevate TBG to cause low T4.
- **Elevated TBG** would actually *increase* total T4 levels, not decrease them, as more T4 would be bound. This option contradicts the observed findings.
*Urinary loss of thyroxine-binding globulin due to nephrotic syndrome*
- **Nephrotic syndrome** can cause significant proteinuria, leading to urinary loss of proteins, including **thyroxine-binding globulin (TBG)**, which would result in low total T4.
- However, there are no clinical signs or laboratory findings suggestive of **nephrotic syndrome** (e.g., massive proteinuria, peripheral edema from low albumin not liver disease), and this patient's liver disease is a more direct and evident cause of low TBG.
Thyroid hormone replacements US Medical PG Question 6: A 30-year-old woman with a 1-year history of medically-managed Graves disease visits her endocrinologist to discuss her desire to become pregnant and whether pregnancy is safe with her medications. Her temperature is 98.4°F (36.9°C), blood pressure is 110/66 mmHg, pulse is 78/min, respirations are 12/min. The endocrinologist advises that the patient may pursue pregnancy, but first needs to be switched from methimazole to propylthiouracil for her Graves disease due to pregnancy safety considerations. Which of the following is a possible side effect of propylthiouracil that represents a greater risk compared to methimazole?
- A. Thyroid storm
- B. Agranulocytosis
- C. Fulminant hepatic necrosis (Correct Answer)
- D. Skin rash
- E. Aplastic anemia
Thyroid hormone replacements Explanation: ***Fulminant hepatic necrosis***
- Propylthiouracil (PTU) carries a **black box warning** for severe liver injury, including **fulminant hepatic necrosis**, which is a greater risk compared to methimazole.
- This risk is particularly relevant in the context of pregnancy, as PTU is often preferred in the first trimester due to lower teratogenic risk, but its hepatotoxicity must be closely monitored.
*Thyroid storm*
- **Thyroid storm** is a life-threatening exacerbation of hyperthyroidism and is not a direct side effect of antithyroid medications like PTU or methimazole.
- It is a complication of inadequately treated or untreated hyperthyroidism.
*Agranulocytosis*
- **Agranulocytosis** is a rare but serious side effect of both propylthiouracil and methimazole.
- While it is a concern, the risk of fulminant hepatic necrosis is specifically highlighted as being higher with PTU.
*Skin rash*
- **Skin rash** is a common and usually mild side effect that can occur with both methimazole and propylthiouracil.
- It is not typically considered a more severe or distinguishing risk for PTU compared to methimazole.
*Aplastic anemia*
- **Aplastic anemia** is an extremely rare but severe side effect that can be associated with antithyroid drugs, including both PTU and methimazole.
- Although serious, the risk of fulminant hepatic necrosis is a more specifically emphasized and distinct concern for PTU.
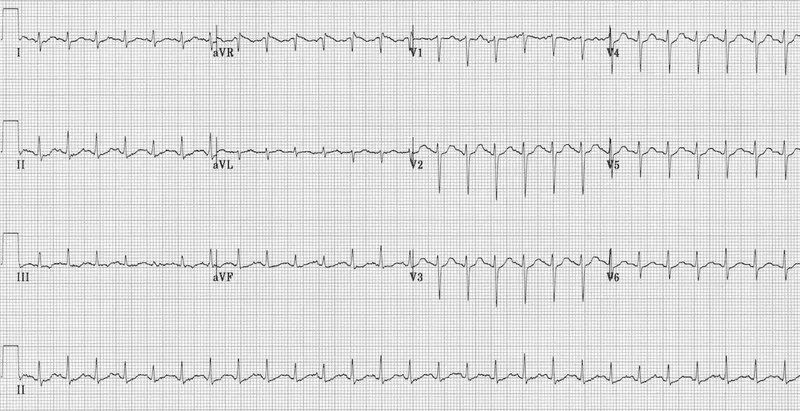
Thyroid hormone replacements US Medical PG Question 7: A previously healthy 27-year-old man comes to the physician because of a 3-week history of anxiety, diarrhea, and a 4.1-kg (9-lb) weight loss. On questioning, he also reports that he noticed a painless mass on his left testicle 2 weeks ago. His pulse is 110/min and irregular and blood pressure is 150/70 mm Hg. Examination shows diaphoresis and a fine tremor of the outstretched fingers. Testicular examination shows a 3-cm, firm, nontender mass on the left scrotum that does not transilluminate. This patient's underlying condition is most likely to be associated with which of the following findings?
- A. Elevated serum AFP
- B. Elevated serum hCG (Correct Answer)
- C. Elevated serum TSH
- D. Proptosis on exophthalmometry
- E. Positive urine metanephrines
Thyroid hormone replacements Explanation: ***Elevated serum hCG***
- The patient presents with symptoms of **hyperthyroidism** (anxiety, weight loss, tachycardia, tremor, diaphoresis) and a **testicular mass**.
- Some **testicular germ cell tumors**, particularly **choriocarcinoma** and some **mixed germ cell tumors**, can produce **hCG**, which has structural similarity to TSH and can stimulate the thyroid gland, leading to **paraneoplastic hyperthyroidism**.
- **Serum hCG** is an important tumor marker for germ cell tumors and would be elevated in this clinical scenario.
*Elevated serum AFP*
- **Alpha-fetoprotein (AFP)** is a tumor marker often elevated in **non-seminomatous germ cell tumors** like **yolk sac tumors** and **embryonal carcinomas**.
- While AFP may be elevated in some testicular tumors, it does not explain the hyperthyroid symptoms, as hCG (not AFP) has TSH-like activity.
*Elevated serum TSH*
- In **hyperthyroidism**, the **thyroid stimulating hormone (TSH)** level is typically **suppressed** due to negative feedback from high thyroid hormone levels.
- An elevated TSH would indicate **primary hypothyroidism**, which contradicts the patient's clinical presentation.
*Proptosis on exophthalmometry*
- **Proptosis** (exophthalmos) is a common finding in **Graves' disease**, an autoimmune cause of hyperthyroidism.
- However, the presence of a **testicular mass** strongly suggests a paraneoplastic etiology for the hyperthyroidism, making Graves' disease less likely as the primary underlying condition.
*Positive urine metanephrines*
- **Urine metanephrines** are markers elevated in **pheochromocytoma**, a tumor of the adrenal medulla that secretes catecholamines.
- While pheochromocytoma can cause hypertension, tachycardia, and anxiety, it does not typically present with a testicular mass or directly cause weight loss through a thyroid-like mechanism.
Thyroid hormone replacements US Medical PG Question 8: A 43-year-old woman comes to the physician because of a 3-month history of tremor, diarrhea, and a 5-kg (11-lb) weight loss. Her pulse is 110/min. Examination shows protrusion of the eyeball when looking forward. A bruit is heard over the anterior neck on auscultation. Serum studies show autoantibodies to the thyroid-stimulating hormone receptor. The patient decides to undergo definitive treatment for her condition with a radioactive tracer. The success of this treatment directly depends on the activity of which of the following?
- A. Anion-oxidizing enzyme
- B. Transmembrane carrier (Correct Answer)
- C. Lysosomal protease
- D. Binding globulin
- E. Hormone-activating enzyme
Thyroid hormone replacements Explanation: ***Transmembrane carrier***
- Radioactive iodine treatment relies on the uptake of iodine by thyroid follicular cells via the **sodium-iodide symporter (NIS)**, a **transmembrane carrier protein**.
- NIS actively transports iodide into thyroid cells, allowing the radioactive iodine to concentrate in the thyroid and destroy overactive tissue.
*Anion-oxidizing enzyme*
- This refers to **thyroid peroxidase (TPO)**, an enzyme that oxidizes iodide to iodine, incorporates iodine into thyroglobulin, and couples iodinated tyrosines.
- While essential for thyroid hormone synthesis, TPO's activity does not directly determine the success of **radioactive iodine uptake** for treatment.
*Lysosomal protease*
- **Lysosomal proteases** are involved in the breakdown of thyroglobulin to release thyroid hormones (T3 and T4) into circulation.
- They are important for the *release* of hormones but not for the *uptake* of iodine for radioactive treatment.
*Binding globulin*
- **Thyroxine-binding globulin (TBG)** is a plasma protein that transports thyroid hormones in the blood, maintaining a reservoir of T3 and T4.
- TBG's activity affects the availability of free thyroid hormones but has no direct role in the cellular uptake of radioactive iodine by the thyroid gland.
*Hormone-activating enzyme*
- This typically refers to deiodinases, enzymes that convert T4 (prohormone) into the more active T3 in peripheral tissues.
- These enzymes act *outside* the thyroid gland to activate hormones, and their activity does not directly influence the uptake of radioactive iodine.
Thyroid hormone replacements US Medical PG Question 9: An 18-year-old girl comes to the clinic because she is concerned about her weight. She states that she is on her school’s cheerleading team and is upset because she feels she is the “fattest” girl on the team despite her healthy diet. She says that in the last 2 weeks since practice began, she has lost 2 lbs. The patient has bipolar disorder I. Her medications include lithium and a combined oral contraceptive that was recently started by her gynecologist, because “everyone is on it." Her mother has hypothyroidism and is treated with levothyroxine. The patient’s BMI is 23.2 kg/m2. Thyroid function labs are drawn and shown below:
Thyroid-stimulating hormone (TSH): 4.0 mIU/L
Serum thyroxine (T4): 18 ug/dL
Free thyroxine (Free T4): 1.4 ng/dl (normal range: 0.7-1.9 ng/dL)
Serum triiodothyronine (T3): 210 ng/dL
Free triiodothyronine (T3): 6.0 pg/mL (normal range: 3.0-7.0 pg/mL)
Which of the following is the most likely cause of the patient’s abnormal lab values?
- A. Familial hyperthyroidism
- B. Hypocholesterolemia
- C. Lithium
- D. Oral contraception-induced (Correct Answer)
- E. Surreptitious use of levothyroxine
Thyroid hormone replacements Explanation: ***Oral contraception-induced***
- The patient's **total T4 and T3 are elevated**, while **free T4 and T3** are within normal limits, indicating an increase in thyroid-binding globulin (TBG).
- Oral contraceptives, specifically **estrogen**, increase the synthesis of TBG in the liver, leading to higher total thyroid hormone levels as more hormone is bound.
*Familial hyperthyroidism*
- Familial hyperthyroidism would present with genuinely **elevated free T4 and T3** levels, alongside suppressed TSH, indicating true hyperthyroidism.
- The patient's **normal free T4 and T3** and slightly elevated TSH rule out true hyperthyroidism.
*Hypocholesterolemia*
- While thyroid hormones can affect lipid metabolism, **hypocholesterolemia is not a direct cause** of altered thyroid lab values.
- It is also not a common side effect of oral contraceptives, nor is it related to the specific pattern of elevated total T4/T3 with normal free hormones.
*Lithium*
- Lithium is known to **cause hypothyroidism** (elevated TSH, low T4/T3) or, less commonly, hyperthyroidism, but not isolated elevated total T4/T3 with normal free hormones due to increased TBG.
- The patient's normal free thyroid hormones and only slightly elevated TSH are not consistent with significant lithium-induced thyroid dysfunction.
*Surreptitious use of levothyroxine*
- Surreptitious use of exogenous **levothyroxine** would typically result in suppressed TSH and elevated free T4, as the gland would be overstimulated or shut down.
- The patient's normal free T4 and elevated total T4/T3 are not indicative of levothyroxine abuse.
Thyroid hormone replacements US Medical PG Question 10: A 4-year-old-female presents with a flattened, reddish 2 cm lump located at the base of the tongue. The patient's mother reports her having trouble swallowing, often leading to feeding difficulties. The mother also reports lethargy, constipation, dry skin, and hypothermia. Which of the following is the most appropriate management of this patient’s presentation?
- A. Week-long course of penicillin
- B. No treatment is necessary, counsel mother on alternative feeding techniques
- C. Thyroid hormone replacement therapy with levothyroxine (Correct Answer)
- D. Combination therapy of methimazole and Beta-blockers
- E. Radioactive iodine ablation
Thyroid hormone replacements Explanation: ***Thyroid hormone replacement therapy with levothyroxine***
- The patient's symptoms of **lethargy, constipation, dry skin, and hypothermia** are classic signs of **hypothyroidism**
- The **flattened, reddish 2 cm lump at the base of the tongue** causing **dysphagia** is highly suggestive of a **lingual thyroid**, a developmental anomaly where thyroid tissue fails to descend from the base of the tongue during embryonic development
- In **90% of lingual thyroid cases**, this ectopic tissue represents the **only functioning thyroid tissue** in the body, leading to hypothyroidism
- **Levothyroxine replacement** is the first-line management, addressing the hypothyroidism and often reducing the size of the lingual thyroid mass, improving swallowing difficulties
- Surgical excision is reserved for cases where medical management fails or severe airway/swallowing obstruction persists
*Week-long course of penicillin*
- Penicillin is an **antibiotic** used to treat **bacterial infections**
- The patient's symptoms indicate an **endocrine disorder** (hypothyroidism) and **developmental anomaly** (lingual thyroid), not an infectious process
- No signs of infection such as fever, leukocytosis, or acute inflammation are present
*No treatment is necessary, counsel mother on alternative feeding techniques*
- Given the **significant systemic symptoms** of hypothyroidism (lethargy, constipation, dry skin, hypothermia) and feeding difficulties, **treatment is clearly necessary**
- **Untreated congenital hypothyroidism** in a child leads to severe developmental delays, intellectual disability, and growth retardation (cretinism)
- While feeding techniques may help with dysphagia, they do not address the underlying hypothyroidism requiring urgent treatment
*Combination therapy of methimazole and Beta-blockers*
- **Methimazole** (antithyroid medication) and **beta-blockers** are used to treat **hyperthyroidism** (overactive thyroid)
- The patient's symptoms (lethargy, constipation, hypothermia, dry skin) are characteristic of **hypothyroidism** (underactive thyroid), making antithyroid therapy completely inappropriate
- This would further suppress thyroid function and worsen the patient's condition
*Radioactive iodine ablation*
- **Radioactive iodine (I-131) ablation** is used to treat **hyperthyroidism** (Graves' disease, toxic nodules) or **thyroid cancer**
- It is a **destructive treatment** that eliminates thyroid tissue
- In this patient with a **lingual thyroid likely representing the only functioning thyroid tissue**, ablation would cause **complete thyroid failure** and severe, permanent hypothyroidism
- Radioactive iodine is also **contraindicated in children** except for specific cases of thyroid cancer
More Thyroid hormone replacements US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.