Posterior pituitary hormones US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Posterior pituitary hormones. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Posterior pituitary hormones US Medical PG Question 1: An investigator is studying a drug that acts on a G protein-coupled receptor in the pituitary gland. Binding of the drug to this receptor leads to increased production of inositol triphosphate (IP3) in the basophilic cells of the anterior pituitary. Administration of this drug every 90 minutes is most likely to be beneficial in the treatment of which of the following conditions?
- A. Prostate cancer
- B. Variceal bleeding
- C. Central diabetes insipidus
- D. Anovulatory infertility (Correct Answer)
- E. Hyperkalemia
Posterior pituitary hormones Explanation: ***Anovulatory infertility***
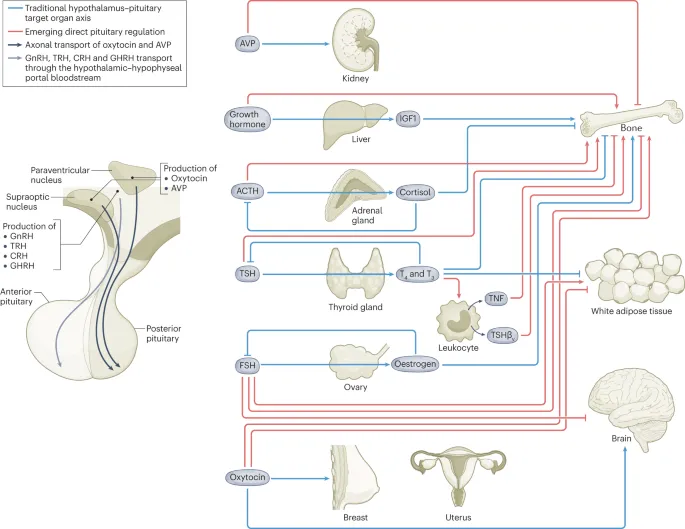
- The drug's action on a G protein-coupled receptor leading to increased **IP3 production** in pituitary basophils suggests activation of the **gonadotropin-releasing hormone (GnRH) receptor**.
- **Pulsatile administration** (e.g., every 90 minutes) of GnRH or its agonists is crucial for stimulating the release of **FSH and LH**, which can induce ovulation in women with anovulatory infertility due to hypothalamic-pituitary dysfunction.
*Prostate cancer*
- While GnRH agonists are used in prostate cancer, they are typically administered **continuously or in depot forms** to desensitize the GnRH receptor, thereby suppressing testosterone production.
- **Pulsatile administration** would rather stimulate testosterone release, which is detrimental in prostate cancer.
*Variceal bleeding*
- **Variceal bleeding** is primarily managed with vasoconstrictors like **octreotide** (a somatostatin analog) or **vasopressin**, which are unrelated to GnRH receptor activation.
- The mechanism of action described (increased IP3 in pituitary basophils) does not align with treatments for variceal bleeding.
*Central diabetes insipidus*
- **Central diabetes insipidus** is caused by a deficiency in **vasopressin (ADH)**, which regulates water balance in the kidneys.
- Treatment involves synthetic ADH (**desmopressin**), not drugs acting on GnRH receptors and affecting pituitary basophils.
*Hyperkalemia*
- **Hyperkalemia** is an electrolyte imbalance characterized by high potassium levels and is managed with medications that shift potassium intracellularly (e.g., insulin, beta-agonists) or promote its excretion (e.g., diuretics, potassium binders).
- The described drug action on pituitary GnRH receptors is unrelated to potassium homeostasis.
Posterior pituitary hormones US Medical PG Question 2: A 72-year-old man is brought in by ambulance to the hospital after being found down at home. On presentation, he appears cachectic and is found to be confused. Specifically, he does not answer questions appropriately and is easily distracted. His wife says that he has been losing weight over the last 3 months and he has a 40 pack-year history of smoking. His serum sodium is found to be 121 mEq/L and his urine osmolality is found to be 415 mOsm/kg. Chest radiograph shows a large central mass in the right lung. Which of the following treatments would be effective in addressing this patient's serum abnormality?
- A. Antipsychotic
- B. Antidiuretic hormone
- C. Normal saline
- D. Renin
- E. Demeclocycline (Correct Answer)
Posterior pituitary hormones Explanation: ***Demeclocycline***
- This patient presents with **hyponatremia** and **concentrated urine** in the setting of lung cancer, suggestive of **SIADH**. Demeclocycline is a **tetracycline derivative** that inhibits the action of ADH on the renal tubules, promoting water excretion.
- While other treatments like fluid restriction are first-line for SIADH, Demeclocycline is an effective pharmacological treatment, especially for **chronic or severe cases**.
*Antipsychotic*
- Antipsychotics are used to treat **psychotic disorders** and may induce hyponatremia as a side effect, but they do not directly treat the underlying mechanism of SIADH.
- This patient's confusion is likely due to **hyponatremia** and his underlying medical condition, not a primary psychiatric disorder requiring antipsychotics.
*Antidiuretic hormone*
- **Antidiuretic hormone (ADH)**, also known as vasopressin, is the *cause* of SIADH (syndrome of inappropriate ADH secretion), where there is *excessive* ADH secretion. Administering more ADH would worsen the condition.
- The goal of treatment in SIADH is to **reduce the effect or amount of ADH**, not increase it.
*Normal saline*
- Administering **normal saline (0.9% NaCl)** in SIADH can worsen hyponatremia. The kidneys will retain the free water due to ADH, while excreting the sodium, leading to a further drop in serum sodium.
- Normal saline is used for **hypovolemic hyponatremia**, not euvolemic hyponatremia like SIADH.
*Renin*
- **Renin** is an enzyme involved in the **renin-angiotensin-aldosterone system** (RAAS), which primarily regulates blood pressure and fluid balance. It is not directly involved in the pathogenesis or treatment of SIADH.
- The RAAS system's role in hyponatremia is distinct from the ADH-mediated pathology of SIADH.
Posterior pituitary hormones US Medical PG Question 3: A 39-year-old man comes to the physician because of frequent urination for the past 2 months. He has been urinating 10–12 times during the day and 3–4 times during the night. He says he is drinking a lot of water to compensate for any dehydration. He has no history of serious illness and takes no medications. Vital signs are within normal limits. Physical examination shows no abnormalities. He is concerned he may have diabetes mellitus like his parents. Laboratory studies show:
Hemoglobin 14.3 g/dL
Serum
Na+ 149 mEq/L
K+ 3.9 mEq/L
Cl- 102 mEq/L
Glucose 90 mg/dL
Osmolality 306 mOsmol/kg H2O
Urine
Osmolality 210 mOsmol/kg H2O
A water deprivation test is conducted. After 2 hours of fluid restriction, his plasma osmolality is 315 mOsmol/kg H2O and his urine osmolality is 210 mOsmol/kg H2O. One hour after an ADH analog injection, his plasma osmolality is 276 mOsmol/kg H2O and his urine osmolality is 425 mOsmol/kg H2O. Which of the following is the most appropriate next step in management?
- A. Hydrochlorothiazide therapy
- B. Fluid restriction
- C. Desmopressin therapy (Correct Answer)
- D. Tolvaptan therapy
- E. Amiloride therapy
Posterior pituitary hormones Explanation: ***Desmopressin therapy***
- The patient's urine osmolality significantly increased after exogenous **ADH analog (desmopressin)** administration during the water deprivation test, indicating a renal response to ADH.
- This response points to **central diabetes insipidus**, where the body does not produce enough ADH, making desmopressin (an ADH analog) the appropriate replacement therapy.
*Hydrochlorothiazide therapy*
- **Thiazide diuretics** are sometimes used in **nephrogenic diabetes insipidus** (where kidneys don't respond to ADH) to induce a mild volume depletion, increasing proximal tubule reabsorption of water, but they are not the primary treatment for central DI.
- The patient's response to exogenous ADH rules out nephrogenic DI as the primary problem.
*Fluid restriction*
- This patient is already experiencing **polyuria** and **polydipsia**, and fluid restriction would worsen his **hypernatremia** and dehydration without addressing the underlying ADH deficiency.
- Fluid restriction is part of the diagnostic **water deprivation test**, not a therapeutic management for diabetes insipidus.
*Tolvaptan therapy*
- **Tolvaptan** is an **ADH receptor antagonist** used in conditions like **hyponatremia** due to SIADH to promote water excretion, which would be counterproductive in a patient with diabetes insipidus.
- It would worsen the patient's condition by further impairing water reabsorption and increasing urine output.
*Amiloride therapy*
- **Amiloride**, a **potassium-sparing diuretic**, is primarily used for hypertension, heart failure, and to counteract potassium loss from other diuretics.
- It has no role in the direct treatment of diabetes insipidus and would not address the ADH deficiency or renal unresponsiveness to ADH.
Posterior pituitary hormones US Medical PG Question 4: A 29-year-old patient presents to her primary care physician with persistent amenorrhea and inability to breastfeed over the last 5 months. She says that she has also been very tired since her baby was born and this fatigue was accompanied by an inability to deal with cold weather despite having no problem with cold prior to becoming pregnant. She has gained an additional 5 pounds since delivery. Review of her hospital records reveals that she had a vaginal delivery that was complicated by severe hemorrhage and episodes of hypotension. Which of the following hormone levels is most likely to be normal in this patient?
- A. Thyroid hormone
- B. Cortisol
- C. Aldosterone (Correct Answer)
- D. Follicle-stimulating hormone (FSH)
- E. Prolactin
Posterior pituitary hormones Explanation: **Aldosterone**
- **Aldosterone** is primarily regulated by the **renin-angiotensin-aldosterone system** (RAAS) and is produced by the adrenal cortex, which is not directly affected by pituitary ischemia in Sheehan's syndrome.
- The symptoms described (amenorrhea, inability to breastfeed, fatigue, cold intolerance, weight gain) are classic for **Sheehan's syndrome**, which involves panhypopituitarism due to **ischemic necrosis of the pituitary gland** following severe postpartum hemorrhage. However, aldosterone production generally remains intact.
*Thyroid hormone*
- The pituitary gland produces **thyroid-stimulating hormone (TSH)**, which is essential for thyroid hormone production. Sheehan's syndrome leads to TSH deficiency, resulting in **secondary hypothyroidism** (low thyroid hormone).
- The patient's symptoms of fatigue, cold intolerance, and weight gain are consistent with hypothyroidism.
*Cortisol*
- The pituitary gland produces **adrenocorticotropic hormone (ACTH)**, which stimulates cortisol production from the adrenal cortex. Sheehan's syndrome causes ACTH deficiency, leading to **secondary adrenal insufficiency** (low cortisol).
- Fatigue is a common symptom of cortisol deficiency.
*Follicle-stimulating hormone (FSH)*
- **FSH** is produced by the pituitary gland and is crucial for ovarian function, including follicular development and estrogen production.
- Deficiency of FSH (and LH) due to Sheehan's syndrome results in **secondary amenorrhea** and an inability to ovulate.
*Prolactin*
- **Prolactin** is produced by the pituitary gland and is necessary for lactation.
- In Sheehan's syndrome, prolactin deficiency directly leads to the **inability to breastfeed**.
Posterior pituitary hormones US Medical PG Question 5: A 42-year-old woman comes to the physician because of urinary leakage over the last year. She reports involuntarily losing small amounts of urine after experiencing a sudden need to void. She has difficulty making it to the bathroom in time, and only feels comfortable going out into public if she has documented the location of all nearby restrooms. She also has begun to wake up at night to urinate. These symptoms have persisted despite 6 months of bladder training and weight loss and reducing soda and coffee intake. Physical examination shows no abnormalities. The most appropriate pharmacotherapy for this patient is a drug that has which of the following mechanisms of action?
- A. Agonism of muscarinic M2 receptors
- B. Antagonism of beta-3 adrenergic receptors
- C. Antagonism of alpha-1 adrenergic receptors
- D. Antagonism of muscarinic M3 receptors (Correct Answer)
- E. Agonism of beta-2 adrenergic receptors
Posterior pituitary hormones Explanation: ***Antagonism of muscarinic M3 receptors***
- The patient's symptoms of **sudden urge to void**, difficulty making it to the bathroom, and nocturia, especially after conservative management failure, are classic for **urge incontinence** or overactive bladder.
- Urge incontinence is caused by **detrusor muscle overactivity**, which is primarily mediated by **M3 muscarinic receptors**; thus, M3 antagonists (e.g., oxybutynin, solifenacin) relax the detrusor.
*Agonism of muscarinic M2 receptors*
- While M2 receptors are present in the bladder, their role in detrusor contraction is less prominent than M3 receptors. Agonism of M2 receptors would theoretically enhance bladder contraction, worsening symptoms.
- No current pharmacotherapy for urge incontinence primarily targets M2 agonism for therapeutic benefit.
*Antagonism of beta-3 adrenergic receptors*
- **Beta-3 adrenergic receptor agonists** (e.g., mirabegron) are used to treat overactive bladder by relaxing the detrusor muscle, but antagonism of these receptors would promote detrusor contraction and worsen symptoms.
- Antagonism of beta-3 receptors is counterproductive as it would increase bladder tone, exacerbating urinary urgency and frequency.
*Antagonism of alpha-1 adrenergic receptors*
- **Alpha-1 adrenergic receptors** are primarily located in the **bladder neck** and **urethra**, mediating smooth muscle contraction to maintain continence.
- Antagonism of these receptors (e.g., with tamsulosin) is used to relax the bladder neck in conditions like benign prostatic hyperplasia to improve urine flow, but would worsen urge incontinence by reducing outflow resistance.
*Agonism of beta-2 adrenergic receptors*
- Beta-2 adrenergic receptors are present in the detrusor muscle, but their agonism has a relatively minor effect on detrusor relaxation compared to beta-3 agonists.
- While beta-2 agonists can cause some detrusor relaxation, they are not the primary or most effective pharmacotherapeutic target for urge incontinence.
Posterior pituitary hormones US Medical PG Question 6: Five minutes after initiating a change of position and oxygen inhalation, the oxytocin infusion is discontinued. A repeat CTG that is done 10 minutes later shows recurrent variable decelerations and a total of 3 uterine contractions in 10 minutes. Which of the following is the most appropriate next step in management?
- A. Restart oxytocin infusion
- B. Emergent Cesarean section
- C. Administer terbutaline
- D. Monitor without intervention
- E. Amnioinfusion (Correct Answer)
Posterior pituitary hormones Explanation: ***Amnioinfusion***
- **Recurrent variable decelerations** persisting after discontinuing oxytocin and changing maternal position often indicate **cord compression**, which can be relieved by amnioinfusion.
- Adding fluid to the amniotic cavity **cushions the umbilical cord**, reducing compression during uterine contractions.
*Restart oxytocin infusion*
- Reinitiating oxytocin would likely **worsen the recurrent variable decelerations** by increasing uterine contraction frequency and intensity, thereby exacerbating cord compression.
- The goal is to alleviate fetal distress, not to intensify uterine activity that is already causing issues.
*Emergent Cesarean section*
- While an emergent Cesarean section is indicated for **unresolved fetal distress**, it's usually considered after less invasive measures, such as amnioinfusion, have failed.
- There is still an opportunity for a simpler intervention to resolve the issue before resorting to surgery.
*Administer terbutaline*
- Terbutaline is a **tocolytic agent** used to reduce uterine contractions, which can be helpful in cases of tachysystole or hyperstimulation.
- In this scenario, the contraction frequency is low (3 in 10 minutes), so reducing contractions is not the primary aim; rather, the focus is on resolving the cord compression causing decelerations.
*Monitor without intervention*
- **Recurrent variable decelerations** are an concerning sign of **fetal distress** and require intervention to prevent potential harm to the fetus.
- Simply monitoring without intervention would be inappropriate and could lead to worsening fetal hypoxemia and acidosis.
Posterior pituitary hormones US Medical PG Question 7: A 65-year-old woman is brought to the emergency department by her husband who found her lying unconscious at home. He says that the patient has been complaining of progressively worsening weakness and confusion for the past week. Her past medical history is significant for hypertension, systemic lupus erythematosus, and trigeminal neuralgia. Her medications include metoprolol, valsartan, prednisone, and carbamazepine. On admission, blood pressure is 130/70 mm Hg, pulse rate is 100 /min, respiratory rate is 17/min, and temperature is 36.5°C (97.7ºF). She regained consciousness while on the way to the hospital but is still drowsy and disoriented. Physical examination is normal. Finger-stick glucose level is 110 mg/dl. Other laboratory studies show:
Na+ 120 mEq/L (136—145 mEq/L)
K+ 3.5 mEq/L (3.5—5.0 mEq/L)
CI- 107 mEq/L (95—105 mEq/L)
Creatinine 0.8 mg/dL (0.6—1.2 mg/dL)
Serum osmolality 250 mOsm/kg (275—295 mOsm/kg)
Urine Na+ 70 mEq/L
Urine osmolality 350 mOsm/kg
She is admitted to the hospital for further management. Which of the following is the next best step in the management of this patient's condition?
- A. Rapid resuscitation with hypertonic saline (Correct Answer)
- B. Fluid restriction
- C. Tolvaptan
- D. Lithium
- E. Desmopressin
Posterior pituitary hormones Explanation: **Rapid resuscitation with hypertonic saline**
- The patient presents with **severe hyponatremia** (120 mEq/L) and neurological symptoms (drowsiness, disorientation, history of unconsciousness), indicating a need for **urgent correction** to prevent cerebral edema.
- **Hypertonic saline** (e.g., 3%) is indicated for severe symptomatic hyponatremia to rapidly increase serum sodium levels and reduce brain swelling.
*Fluid restriction*
- **Fluid restriction** is a conservative measure appropriate for **mild to moderate asymptomatic hyponatremia** or as an adjunct in SIADH management once severe symptoms are controlled.
- It would be too slow to address the patient's acute neurological symptoms and severe hyponatremia, potentially delaying critical treatment.
*Tolvaptan*
- **Tolvaptan** is a **vasopressin receptor antagonist** used in the treatment of **euvolemic or hypervolemic hyponatremia**, often in the context of SIADH.
- Its use is generally reserved for patients who have not responded to fluid restriction and is **contraindicated** in patients with severe symptoms or to rapidly correct severe hyponatremia due to the risk of overly rapid correction and osmotic demyelination syndrome.
*Lithium*
- **Lithium** is primarily used as a **mood stabilizer** in psychiatric conditions, particularly bipolar disorder.
- It can cause **nephrogenic diabetes insipidus** as a side effect and is not a treatment for hyponatremia.
*Desmopressin*
- **Desmopressin** is a synthetic analog of **antidiuretic hormone (ADH)** and is used to treat **diabetes insipidus** or nocturnal enuresis.
- Administering desmopressin would **worsen hyponatremia** by promoting water reabsorption, making it an inappropriate choice for this patient.
Posterior pituitary hormones US Medical PG Question 8: A neurophysiologist describes the mechanism of a specific type of synaptic transmission to his students. While illustrating this, he points out that when the action potential reaches the presynaptic terminal of a chemical synapse, the voltage-gated Ca2+ channels open. Ca2+ ions trigger the release of neurotransmitters from vesicles in the presynaptic terminal. In this type of synaptic transmission, increased cytosolic Ca2+ levels cause the release of a neurotransmitter from small vesicles with dense cores. Which of the following neurotransmitters is most likely to be the one that is released into the synaptic cleft in this type of synapse?
- A. Epinephrine
- B. Glutamate
- C. Glycine
- D. GABA (γ-amino butyric acid)
- E. Norepinephrine (Correct Answer)
Posterior pituitary hormones Explanation: ***Norepinephrine***
- **Norepinephrine** is the primary catecholamine neurotransmitter stored in **small vesicles with dense cores** (dense-core vesicles).
- It is released from **sympathetic postganglionic neurons** and central nervous system neurons, particularly from the **locus coeruleus**.
- Dense-core vesicles are the hallmark of catecholaminergic neurons, and norepinephrine is the most abundant neuronal catecholamine.
- The description perfectly matches noradrenergic synaptic transmission.
*Epinephrine*
- While epinephrine is also a catecholamine stored in dense-core vesicles, it functions primarily as a **hormone** released from the **adrenal medulla** (not a neurotransmitter).
- Only a **very small number** of CNS neurons use epinephrine as a neurotransmitter (mainly in medullary regions).
- In the context of synaptic transmission, norepinephrine is far more common.
*Glutamate*
- **Glutamate** is the primary excitatory neurotransmitter in the CNS but is stored in **small, clear synaptic vesicles**, not dense-core vesicles.
- It does not fit the description of dense-core vesicle storage.
*Glycine*
- **Glycine** is an inhibitory neurotransmitter stored in **small, clear synaptic vesicles**.
- Found predominantly in the **spinal cord** and brainstem, not in dense-core vesicles.
*GABA (γ-amino butyric acid)*
- **GABA** is the main inhibitory neurotransmitter stored in **small, clear synaptic vesicles**.
- Not associated with dense-core vesicle storage.
Posterior pituitary hormones US Medical PG Question 9: A 10-year-old girl is brought to the physician by her parents due to 2 months of a progressively worsening headache. The headaches were initially infrequent and her parents attributed them to stress from a recent move. However, over the last week the headaches have gotten significantly worse and she had one episode of vomiting this morning when she woke up. Her medical history is remarkable for a hospitalization during infancy for bacterial meningitis. On physical exam, the patient has difficulty looking up. The lower portion of her pupil is covered by the lower eyelid and there is sclera visible below the upper eyelid. A magnetic resonance imaging (MRI) of the brain is shown. Which of the following is the most likely diagnosis?
- A. Ependymoma
- B. Medulloblastoma
- C. Craniopharyngioma
- D. Pinealoma (Correct Answer)
- E. Pituitary Adenoma
Posterior pituitary hormones Explanation: ***Pinealoma***
- The constellation of a progressively worsening headache, vomiting, and difficulty looking up (Parinaud's syndrome or **dorsal midbrain syndrome**) with **hydrocephalus** visible on MRI points strongly to a **pineal region tumor** that compresses the **tectal plate** and obstructs CSF flow. The visible sclera below the upper eyelid is due to **retraction of the upper eyelids**, a component of Parinaud's syndrome.
- The MRI shows significant **ventricular dilation**, particularly of the lateral and third ventricles, indicating **obstructive hydrocephalus**, which is consistent with a mass in the pineal region compressing the **cerebral aqueduct**.
*Ependymoma*
- Ependymomas most commonly occur in the **fourth ventricle** in children and can cause hydrocephalus by obstructing CSF flow at that level.
- However, typical symptoms would be more associated with **cerebellar dysfunction** (ataxia, nystagmus), and Parinaud's syndrome is not characteristic.
*Medulloblastoma*
- Medulloblastomas are highly malignant **cerebellar tumors** in children, typically arising from the vermis, and often cause **ataxia**, truncal instability, and hydrocephalus due to fourth ventricle obstruction.
- While they cause hydrocephalus and headaches, they do not typically present with Parinaud's syndrome.
*Craniopharyngioma*
- Craniopharyngiomas are **suprasellar tumors** that originate from Rathke's pouch remnants and can cause headaches, visual field defects (**bitemporal hemianopsia**), and **endocrine dysfunction** (e.g., growth delays, diabetes insipidus).
- They are typically located anteriorly, compressing the **optic chiasm** and hypothalamus, not directly obstructing the cerebral aqueduct to cause Parinaud's syndrome.
*Pituitary Adenoma*
- Pituitary adenomas are rare in children and typically cause symptoms related to **hormonal overproduction** or compression of adjacent structures, such as **visual field defects** (bitemporal hemianopsia).
- While large adenomas can cause headaches, they are not typically associated with **Parinaud's syndrome** or rapid-onset **obstructive hydrocephalus** in this manner.
Posterior pituitary hormones US Medical PG Question 10: A 42-year-old man who is employed as a construction worker presents to his primary care physician with complaints of moderate headaches and profuse sweating. He reports the need to carry up to 3 additional shirt changes to work because they drench quickly even with tasks of low physical exertion. His coworkers have commented about his changing glove and boot sizes, which have increased at least 4 times since he joined the company 10 years ago. Physical examination is unremarkable except for blood pressure of 160/95 mm Hg, hyperhidrosis, noticeably large pores, hypertrichosis, widely spaced teeth, and prognathism. Which of the following best explains the patient’s clinical manifestations?
- A. Increased serum cortisol
- B. Increased thyroid-stimulating hormone
- C. Increased serum metanephrines
- D. Increased serum insulin-like growth factor 1 (IGF-1) (Correct Answer)
- E. Increased serum testosterone
Posterior pituitary hormones Explanation: ***Increased serum insulin-like growth factor 1 (IGF-1)***
- Elevated **IGF-1** levels are indicative of **acromegaly**, a condition caused by excess growth hormone (GH) secretion, which explains the gradual changes in glove and boot sizes, prognathism, widely spaced teeth, and large pores.
- The symptoms of **profuse sweating**, **hypertrichosis**, **headaches**, and **hypertension** are common clinical manifestations of acromegaly due to the systemic effects of chronic GH excess.
*Increased serum cortisol*
- **Increased cortisol** (Cushing's syndrome) would present with central obesity, moon facies, buffalo hump, and striae, which are not described in the patient.
- While hypertension and hyperhidrosis can occur in Cushing's, the characteristic physical changes related to growth are absent.
*Increased thyroid-stimulating hormone*
- Elevated **TSH** suggests **hypothyroidism**, which would typically cause fatigue, weight gain, cold intolerance, and bradycardia, rather than profuse sweating and hypertension.
- **Hyperthyroidism** (low TSH, high thyroid hormones) can cause sweating and hypertension, but it would not explain the gradual increase in body and appendage size.
*Increased serum metanephrines*
- Elevated **metanephrines** are a hallmark of **pheochromocytoma**, which typically presents with paroxysmal episodes of hypertension, palpitations, and sweating.
- While sweating and hypertension are present, the absence of episodic symptoms and the long-term changes in body size make pheochromocytoma less likely.
*Increased serum testosterone*
- **Increased testosterone** in a male would typically lead to increased muscle mass, acne, and potentially male-pattern baldness, but not the specific skeletal and soft tissue growth patterns observed, such as increased shoe and glove size or prognathism.
- While some skin changes might occur, **hyperhidrosis** and the dramatic facial and extremity changes are not characteristic features of testosterone excess.
More Posterior pituitary hormones US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.