Oral hypoglycemic agents US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Oral hypoglycemic agents. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Oral hypoglycemic agents US Medical PG Question 1: A 53-year-old male presents to your office for a regularly scheduled check-up. The patient was diagnosed with type II diabetes mellitus two years ago. To date, diet, exercise, and metformin have failed to control his elevated blood glucose. Past medical history is also significant for hypertension. The patient does not smoke or use cigarettes. Laboratory values show a hemoglobin A1c (HbA1c) of 8.5%. You decide to add sitagliptin to the patient’s medication regimen. Which of the following is the direct mechanism of action of sitagliptin?
- A. Increases secretion of insulin in response to oral glucose loads and delays gastric emptying
- B. Inhibits degradation of endogenous incretins (Correct Answer)
- C. Activates transcription of PPARs to increase peripheral sensitivity to insulin
- D. Depolarizes potassium channels in pancreatic beta cells
- E. Inhibits alpha-glucosidases at the intestinal brush border
Oral hypoglycemic agents Explanation: ***Inhibits degradation of endogenous incretins***
- Sitagliptin is a **DPP-4 inhibitor**, which prevents the breakdown of **incretin hormones** like GLP-1 and GIP.
- By increasing the levels of active incretins, sitagliptin enhances **glucose-dependent insulin secretion** and suppresses glucagon release.
*Increases secretion of insulin in response to oral glucose loads and delays gastric emptying*
- This describes the action of **GLP-1 receptor agonists** (e.g., exenatide, liraglutide), which are injectable medications.
- While sitagliptin *indirectly* increases incretin levels, it does not directly cause significant delays in gastric emptying.
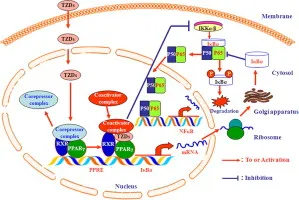
*Activates transcription of PPARs to increase peripheral sensitivity to insulin*
- This is the mechanism of action of **thiazolidinediones** (e.g., pioglitazone), which improve insulin sensitivity in peripheral tissues.
- Sitagliptin's primary action is on incretin metabolism, not direct PPAR-gamma activation.
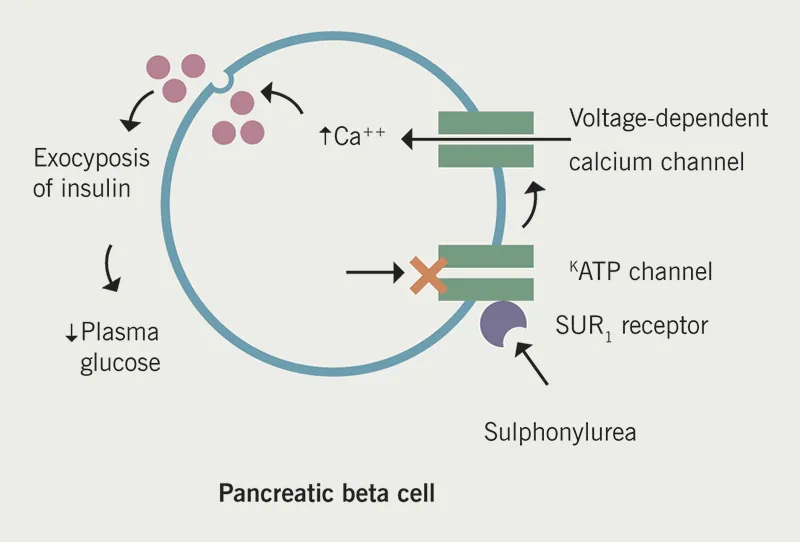
*Depolarizes potassium channels in pancreatic beta cells*
- This mechanism is characteristic of **sulfonylureas** (e.g., glyburide, glipizide), which stimulate insulin release independently of glucose levels.
- Sitagliptin's effect on insulin secretion is glucose-dependent and mediated by incretins, not direct potassium channel depolarization.
*Inhibits alpha-glucosidases at the intestinal brush border*
- This describes the action of **alpha-glucosidase inhibitors** (e.g., acarbose, miglitol), which delay carbohydrate absorption from the gut.
- Sitagliptin does not interfere with carbohydrate digestion or absorption.
Oral hypoglycemic agents US Medical PG Question 2: A 57-year-old woman presents to the emergency department with acute onset confusion, sweating, weakness, and tremors. She says that the symptoms started when she went to dinner with friends and had several drinks of alcohol without eating much food. Her past medical history is significant for type 2 diabetes, and she was recently started on a new medication for this disease. She mentions that her doctor warned her about the risk of low blood sugar, especially if she drinks alcohol or skips meals. Which of the following describes the mechanism of action for the most likely diabetes drug that this patient started taking?
- A. Inhibiting dipeptidyl peptidase
- B. Closing potassium channels (Correct Answer)
- C. Inhibiting alpha-glucosidase
- D. Decreasing hepatic gluconeogenesis
- E. Binding to peroxisome proliferator-activating receptors
Oral hypoglycemic agents Explanation: ***Closing potassium channels***
The patient's symptoms (confusion, sweating, weakness, tremors) along with recent alcohol consumption and a new diabetes medication strongly suggest **hypoglycemia**. **Sulfonylureas** are a class of diabetes drugs known to cause hypoglycemia, especially with alcohol, by binding to and **closing ATP-sensitive potassium channels** on pancreatic beta cells, leading to depolarization and insulin release. The doctor's warning about hypoglycemia risk with alcohol or skipped meals is classic for sulfonylureas.
*Inhibiting dipeptidyl peptidase*
This mechanism describes **DPP-4 inhibitors** (gliptins), which increase levels of endogenous incretins (GLP-1 and GIP) by preventing their breakdown. These drugs have a **low risk of hypoglycemia** when used alone because they work in a glucose-dependent manner. They do not typically cause severe hypoglycemia, especially not to the extent described in this case.
*Inhibiting alpha-glucosidase*
Alpha-glucosidase inhibitors (e.g., **acarbose**, miglitol) delay carbohydrate absorption in the small intestine by inhibiting brush border enzymes. While they can cause gastrointestinal side effects (flatulence, diarrhea), they have a **very low risk of hypoglycemia** because they do not affect insulin secretion directly.
*Decreasing hepatic gluconeogenesis*
This is the primary mechanism of action for **metformin**, which is a biguanide and typically the first-line agent for type 2 diabetes. Metformin reduces glucose production by the liver and has a **very low risk of hypoglycemia** when used as monotherapy, making it an unlikely cause of the patient's acute symptoms.
*Binding to peroxisome proliferator-activating receptors*
This mechanism describes **thiazolidinediones** (TZDs) like pioglitazone and rosiglitazone, which improve insulin sensitivity by activating PPAR-gamma receptors. They typically have a **low risk of hypoglycemia** when used as monotherapy. Their common side effects include weight gain, fluid retention, and increased fracture risk—not acute hypoglycemia.
Oral hypoglycemic agents US Medical PG Question 3: A 55-year-old male is hospitalized for acute heart failure. The patient has a 20-year history of alcoholism and was diagnosed with diabetes mellitus type 2 (DM2) 5 years ago. Physical examination reveals ascites and engorged paraumbilical veins as well as 3+ pitting edema around both ankles. Liver function tests show elevations in gamma glutamyl transferase and aspartate transaminase (AST). Of the following medication, which most likely contributed to this patient's presentation?
- A. Glargine
- B. Pramlintide
- C. Pioglitazone (Correct Answer)
- D. Glipizide
- E. Metformin
Oral hypoglycemic agents Explanation: ***Pioglitazone***
- **Pioglitazone**, a thiazolidinedione, is known to cause **fluid retention** and can exacerbate or precipitate **congestive heart failure**.
- The patient's presentation with **ascites**, **pitting edema**, and **acute heart failure** is consistent with the adverse effects of this medication, especially in a patient with risk factors like alcoholism.
*Glargine*
- **Glargine** is a **long-acting insulin** analog primarily used to control blood glucose levels in diabetes.
- It does not typically cause **fluid retention** or worsen **heart failure** directly, making it an unlikely contributor to these specific symptoms.
*Pramlintide*
- **Pramlintide** is an **amylin analog** used to improve glycemic control by slowing gastric emptying and suppressing glucagon secretion.
- It is not associated with **fluid retention** or the exacerbation of **heart failure**.
*Glipizide*
- **Glipizide** is a **sulfonylurea** that stimulates insulin release from pancreatic beta cells.
- While it can cause hypoglycemia, it does not typically contribute to **fluid retention** or worsen **heart failure**.
*Metformin*
- **Metformin** is a **biguanide** that reduces hepatic glucose production and increases insulin sensitivity.
- It is generally considered **cardioprotective** and does not cause **fluid retention** or exacerbate **heart failure**.
Oral hypoglycemic agents US Medical PG Question 4: A 46-year-old woman presents with palpitations, tremors, and anxiety. She says these symptoms have been present ever since a recent change in her diabetic medication. The most recent time she felt these symptoms, her blood glucose level was 65 mg/dL, and she felt better after eating a cookie. Which of the following is the mechanism of action of the drug most likely to have caused this patient's symptoms?
- A. Inhibition of α-glucosidase
- B. Blocking of the ATP-sensitive K+ channels (Correct Answer)
- C. Block reabsorption of glucose in proximal convoluted tubule (PCT)
- D. Inhibitor of dipeptidyl peptidase (DPP-IV)
- E. Decreased hepatic gluconeogenesis
Oral hypoglycemic agents Explanation: ***Blocking of the ATP-sensitive K+ channels***
- The patient's symptoms of palpitations, tremors, anxiety, and a blood glucose level of 65 mg/dL, which improved after eating, are characteristic of **hypoglycemia**.
- **Sulfonylureas**, such as glyburide or glipizide, cause hypoglycemia by **blocking ATP-sensitive K+ channels** on pancreatic beta cells, leading to insulin release independent of blood glucose levels.
*Inhibition of α-glucosidase*
- This mechanism, characteristic of drugs like **acarbose** and **miglitol**, delays carbohydrate absorption in the gut.
- These drugs typically cause **gastrointestinal side effects** such as flatulence and diarrhea, not hypoglycemia or the associated adrenergic symptoms.
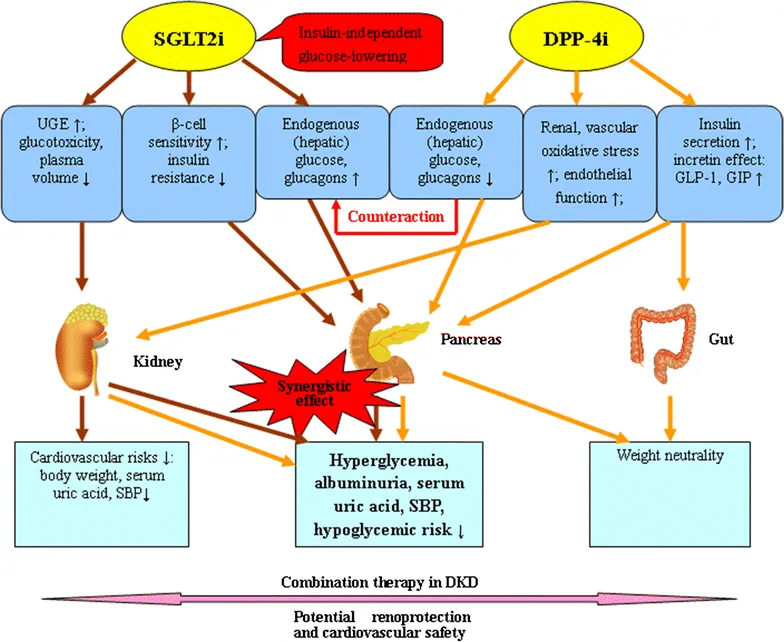
*Block reabsorption of glucose in proximal convoluted tubule (PCT)*
- This action describes **SGLT2 inhibitors** (e.g., canagliflozin, empagliflozin), which increase urinary glucose excretion.
- While they can cause **genitourinary infections** and **polyuria**, they have a very low risk of hypoglycemia unless combined with insulin or sulfonylureas.
*Inhibitor of dipeptidyl peptidase (DPP-IV)*
- **DPP-IV inhibitors** (e.g., sitagliptin, saxagliptin) prevent the breakdown of incretins, thus enhancing glucose-dependent insulin secretion and suppressing glucagon.
- These drugs typically have a **low risk of hypoglycemia** because their effects on insulin secretion are glucose-dependent.
*Decreased hepatic gluconeogenesis*
- This is the primary mechanism of **metformin**, which also increases insulin sensitivity in peripheral tissues.
- Metformin is associated with **lactic acidosis** and **gastrointestinal upset**, but it does not typically cause hypoglycemia as a monotherapy because it does not stimulate insulin secretion.
Oral hypoglycemic agents US Medical PG Question 5: A 58-year-old man with a 10-year history of type 2 diabetes mellitus and hypertension comes to the physician for a routine examination. Current medications include metformin and captopril. His pulse is 84/min and blood pressure is 120/75 mm Hg. His hemoglobin A1c concentration is 9.5%. The physician adds repaglinide to his treatment regimen. The mechanism of action of this agent is most similar to that of which of the following drugs?
- A. Linagliptin
- B. Glyburide (Correct Answer)
- C. Pioglitazone
- D. Miglitol
- E. Metformin
Oral hypoglycemic agents Explanation: ***Glyburide***
- **Repaglinide** is a meglitinide, and **glyburide** is a sulfonylurea; both classes of drugs stimulate insulin release from pancreatic **beta cells** by closing ATP-sensitive potassium channels.
- This action leads to depolarization of the beta cell membrane, opening of **voltage-gated calcium channels**, and subsequent release of insulin from storage granules.
*Linagliptin*
- **Linagliptin** is a **dipeptidyl peptidase-4 (DPP-4) inhibitor** that works by preventing the breakdown of incretins like GLP-1, thereby increasing postprandial insulin secretion and decreasing glucagon secretion.
- Its mechanism is distinct from repaglinide's direct stimulation of insulin release.
*Pioglitazone*
- **Pioglitazone** is a **thiazolidinedione** that acts by activating **peroxisome proliferator-activated receptor-gamma (PPAR-γ)** in adipose tissue, increasing insulin sensitivity in peripheral tissues.
- This mechanism centers on improving insulin utilization rather than stimulating insulin secretion.
*Miglitol*
- **Miglitol** is an **alpha-glucosidase inhibitor** that delays carbohydrate absorption in the gastrointestinal tract, leading to a flatter postprandial glucose curve.
- Its action focuses on reducing glucose absorption, which is different from directly influencing insulin secretion or sensitivity.
*Metformin*
- **Metformin** is a biguanide that primarily reduces **hepatic glucose production** and improves insulin sensitivity in peripheral tissues.
- It does not directly affect insulin secretion from the pancreas, distinguishing it from repaglinide.
Oral hypoglycemic agents US Medical PG Question 6: A 68-year-old man comes to the physician because of a 6-week history of episodic tremors, headaches, and sweating. During this time, he has gained 2.5-kg (5 lb 8 oz). Two months ago, he was diagnosed with type 2 diabetes mellitus and treatment with an oral antidiabetic drug was initiated. The beneficial effect of the drug that was prescribed for this patient is most likely due to inhibition of which of the following?
- A. ATP-sensitive potassium channels (Correct Answer)
- B. Glycerophosphate dehydrogenase
- C. Sodium-glucose cotransporter-2
- D. Dipeptidyl peptidase-4
- E. Brush-border α-glucosidase
Oral hypoglycemic agents Explanation: ***ATP-sensitive potassium channels***
- The patient's symptoms of episodic tremors, headaches, sweating, and weight gain, along with a recent diagnosis of type 2 diabetes treated with an oral antidiabetic drug, suggest **hypoglycemia** as a side effect.
- Sulfonylureas, a common class of oral antidiabetic drugs, exert their effect by **inhibiting ATP-sensitive potassium channels** on pancreatic beta cells, leading to insulin release and potentially hypoglycemia.
*Glycerophosphate dehydrogenase*
- This enzyme is involved in **glycerol metabolism** and is not a primary target for oral antidiabetic drugs that cause hypoglycemia.
- Its inhibition would not directly lead to increased insulin secretion or the described pattern of symptoms.
*Sodium-glucose cotransporter-2*
- **SGLT2 inhibitors** (e.g., canagliflozin) work by blocking glucose reabsorption in the kidneys, leading to glucose excretion in urine.
- While they can cause some weight loss, they are less likely to cause symptomatic hypoglycemia unless combined with other agents, and their mechanism does not involve ATP-sensitive potassium channels.
*Dipeptidyl peptidase-4*
- **DPP-4 inhibitors** (e.g., sitagliptin) prevent the breakdown of incretin hormones, thereby increasing insulin secretion in a glucose-dependent manner.
- These drugs generally have a **low risk of hypoglycemia** because their effect on insulin release diminishes as blood glucose normalizes.
*Brush-border α-glucosidase*
- **Alpha-glucosidase inhibitors** (e.g., acarbose) delay carbohydrate absorption in the gut.
- They primarily target **postprandial hyperglycemia** and, when used alone, cause very little risk of hypoglycemia because they do not directly stimulate insulin secretion.
Oral hypoglycemic agents US Medical PG Question 7: A 60-year-old African-American female presents to your office complaining of dysuria, paresthesias, and blurry vision. Her body mass index is 37.2 kg/m2. Which of the following drugs would most significantly increase the levels of C-peptide in the blood when administered to this patient?
- A. Acarbose
- B. Glipizide (Correct Answer)
- C. Insulin
- D. Metformin
- E. NPH
Oral hypoglycemic agents Explanation: ***Glipizide***
- **Glipizide** is a **sulfonylurea** that stimulates insulin secretion from pancreatic beta cells, leading to increased C-peptide levels.
- Increased insulin secretion by glipizide is independent of meals and can cause **hypoglycemia**.
*Acarbose*
- **Acarbose** is an **alpha-glucosidase inhibitor** that delays glucose absorption from the gut, reducing post-prandial glucose spikes.
- It does not directly affect insulin secretion or C-peptide levels.
*Insulin*
- Administering exogenous **insulin** directly lowers blood glucose but does not stimulate endogenous insulin production, and therefore does not increase C-peptide.
- C-peptide is a marker of endogenous insulin secretion; an increase would only be seen if the body produced more insulin.
*Metformin*
- **Metformin** primarily reduces **hepatic glucose production** and improves insulin sensitivity in peripheral tissues.
- It does not directly stimulate insulin secretion from the pancreas and therefore does not increase C-peptide levels.
*NPH*
- **NPH (Neutral Protamine Hagedorn)** is an intermediate-acting exogenous insulin formulation.
- As an exogenous insulin, it does not stimulate the pancreas to produce more insulin or C-peptide.
Oral hypoglycemic agents US Medical PG Question 8: A 49-year-old woman presents to the family medicine clinic with concerns about her weight. She has been constantly gaining weight for a decade now as she has not been able to control her diet. She has tried exercising but says that she is too lazy for this method of weight loss to work. Her temperature is 37° C (98.6° F), respirations are 15/min, pulse is 67/min, and blood pressure is 122/88 mm Hg. Her BMI is 30. Her labs from her past visit show:
Fasting blood glucose: 149 mg/dL
Glycated hemoglobin (HbA1c): 9.1%
Triglycerides: 175 mg/dL
LDL-Cholesterol: 102 mg/dL
HDL-Cholesterol: 35 mg/dL
Total Cholesterol: 180 mg/dL
Serum creatinine: 1.0 mg/dL
BUN: 12 mg/dL
Serum:
Albumin: 4.2 gm/dL
Alkaline phosphatase: 150 U/L
Alanine aminotransferase: 76 U/L
Aspartate aminotransferase: 88 U/L
After discussing the long term issues that will arise if her health does not improve, she agrees to modify her lifestyle and diet. Which of the following would be the best pharmacotherapy for this patient?
- A. Insulin
- B. Metformin (Correct Answer)
- C. Dietary modification alone
- D. Sitagliptin
- E. Glipizide
Oral hypoglycemic agents Explanation: ***Metformin***
- This patient has newly diagnosed **type 2 diabetes mellitus** (Fasting blood glucose 149 mg/dL, HbA1c 9.1%) in the setting of obesity (BMI 30). **Metformin** is the **first-line pharmacotherapy** for type 2 diabetes due to its efficacy, favorable safety profile, and potential for weight neutrality or modest weight loss.
- Metformin works by **decreasing hepatic glucose production**, decreasing intestinal glucose absorption, and increasing insulin sensitivity.
*Insulin*
- While insulin is highly effective in lowering blood glucose, it is typically reserved for patients with **very high HbA1c** (often >10%), **symptomatic hyperglycemia**, or those who have failed oral pharmacotherapy, it can also cause **weight gain**.
- Initiating insulin as first-line therapy can be overly aggressive and may lead to **hypoglycemia** in patients who can respond to oral agents.
*Dietary modification alone*
- Although **lifestyle changes** (diet and exercise) are crucial and can be remarkably effective, this patient's **HbA1c of 9.1%** indicates that **monotherapy with diet and exercise alone is insufficient** to achieve glycemic control.
- Pharmacotherapy is generally recommended for HbA1c levels **above 7.5%**, even with a commitment to lifestyle changes.
*Sitagliptin*
- **Sitagliptin** is a **DPP-4 inhibitor** that increases insulin secretion and decreases glucagon secretion in a glucose-dependent manner.
- It is often considered a **second-line agent** or an add-on therapy, as its HbA1c-lowering effect is generally less potent than metformin.
*Glipizide*
- **Glipizide** is a **sulfonylurea** that works by stimulating insulin release from pancreatic beta cells.
- It can cause **weight gain** and has a significant risk of **hypoglycemia**, making it a less favorable first-line agent, especially in an obese patient, compared to metformin.
Oral hypoglycemic agents US Medical PG Question 9: A 67-year-old man presents to his physician with increased thirst and polyuria for the past 4 months. Patient also notes a decrease in his vision for the past 6 months and tingling in his feet. The medical history is significant for a chronic pyelonephritis and stage 2 chronic kidney disease. The current medications include losartan and atorvastatin. He reports a daily alcohol intake of 3 glasses of whiskey. The blood pressure is 140/90 mm Hg and the heart rate is 63/min. The BMI is 35.4 kg/m2. On physical examination, there is 2+ pitting edema of the lower legs and face. The pulmonary, cardiac, and abdominal examinations are within normal limits. There is no costovertebral angle tenderness noted. Ophthalmoscopy shows numerous microaneurysms and retinal hemorrhages concentrated in the fundus. The neurological examination reveals a symmetric decrease in vibration and 2 point discrimination in the patient’s feet and legs extending up to the lower third of the calves. The ankle-deep tendon reflexes are decreased bilaterally. The laboratory test results are as follows:
Serum glucose (fasting) 140 mg/dL
HbA1c 8.5%
BUN 27 mg/dL
Serum creatinine 1.3 mg/dL
eGFR 55 mL/min
The patient is prescribed the first-line drug recommended for his condition. Which of the following side effect is associated with this drug?
- A. Lactic acidosis (Correct Answer)
- B. Infections
- C. Hypoglycemia
- D. Iron deficiency anemia
- E. Hyperkalemia
Oral hypoglycemic agents Explanation: ***Lactic acidosis***
- The patient presents with classic **Type 2 Diabetes Mellitus** (polyuria, polydipsia, HbA1c 8.5%, fasting glucose 140 mg/dL, diabetic retinopathy, peripheral neuropathy).
- **Metformin** is the first-line medication for Type 2 Diabetes according to all major guidelines (ADA, AACE).
- While **lactic acidosis** is a rare side effect of metformin, it is the most **serious** adverse effect and the answer to this question.
- This patient has multiple risk factors for lactic acidosis: **moderate renal impairment** (eGFR 55 mL/min), **chronic alcohol use** (3 glasses whiskey daily), and advanced age.
- Note: Current guidelines allow metformin use at eGFR ≥30 mL/min with dose adjustment, so metformin is not contraindicated in this patient but requires careful monitoring.
- The most common side effects of metformin are GI-related (diarrhea, nausea), but lactic acidosis is the most clinically significant.
*Infections*
- Increased risk of **genitourinary infections** is associated with **SGLT2 inhibitors** (canagliflozin, empagliflozin, dapagliflozin), not metformin.
- While the patient has a history of chronic pyelonephritis, this is unrelated to metformin therapy.
*Hypoglycemia*
- **Metformin** decreases hepatic glucose production and improves insulin sensitivity without stimulating insulin secretion.
- Metformin monotherapy **rarely causes hypoglycemia**, which is more common with sulfonylureas (glyburide, glipizide) or insulin.
*Iron deficiency anemia*
- Iron deficiency anemia is **not** a recognized side effect of metformin.
- Note: Metformin is associated with **Vitamin B12 deficiency** (due to malabsorption) leading to megaloblastic anemia, but not iron deficiency anemia.
*Hyperkalemia*
- Hyperkalemia is **not** a side effect of metformin.
- This patient's losartan (ARB) and chronic kidney disease could cause hyperkalemia, but this is unrelated to metformin therapy.
Oral hypoglycemic agents US Medical PG Question 10: A 56-year-old man with type 2 diabetes mellitus comes to the physician for a follow-up examination. Three months ago, the patient was started on metformin therapy after counseling on diet, exercise, and weight reduction failed to reduce his hyperglycemia. Physical examination shows no abnormalities. His hemoglobin A1c is 8.4%. Pioglitazone is added to the patient's medication regimen. Which of the following cellular changes is most likely to occur in response to this new drug?
- A. Depolarization of pancreatic β-cells
- B. Decreased sodium-dependent glucose cotransport
- C. Decreased breakdown of glucagon-like peptide 1
- D. Increased transcription of adipokines (Correct Answer)
- E. Autophosphorylation of receptor tyrosine kinase
Oral hypoglycemic agents Explanation: ***Increased transcription of adipokines***
- **Pioglitazone** is a **thiazolidinedione (TZD)** that acts as an **agonist for peroxisome proliferator-activated receptor-gamma (PPAR-γ)**.
- Activation of PPAR-γ in adipocytes leads to increased transcription of genes involved in **glucose uptake and lipid metabolism**, including certain **adipokines** that improve insulin sensitivity.
*Depolarization of pancreatic β-cells*
- This is the mechanism of **sulfonylureas** (e.g., glipizide, glyburide) or **meglitinides** (e.g., repaglinide, nateglinide), which stimulate insulin release by closing K+ channels and depolarizing β-cells.
- Pioglitazone does not directly stimulate insulin secretion from β-cells.
*Decreased sodium-dependent glucose cotransport*
- This is the mechanism of **SGLT2 inhibitors** (e.g., empagliflozin, canagliflozin, dapagliflozin), which reduce glucose reabsorption in the renal tubules.
- Pioglitazone primarily acts by sensitizing peripheral tissues to insulin.
*Decreased breakdown of glucagon-like peptide 1*
- This is the mechanism of **DPP-4 inhibitors** (e.g., sitagliptin, saxagliptin), which prevent the degradation of GLP-1, thereby increasing its levels and effect.
- Pioglitazone does not directly affect GLP-1 metabolism.
*Autophosphorylation of receptor tyrosine kinase*
- This is the initial step in the **insulin signaling pathway** when insulin binds to its receptor.
- While pioglitazone improves insulin sensitivity, it does not directly cause autophosphorylation of the insulin receptor itself; rather, it upregulates pathways downstream or parallel to it that enhance insulin's effects.
More Oral hypoglycemic agents US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.