Insulin preparations and kinetics US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Insulin preparations and kinetics. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Insulin preparations and kinetics US Medical PG Question 1: A 62-year-old man presents to the emergency department with confusion. The patient’s wife states that her husband has become more somnolent over the past several days and now is very confused. The patient has no complaints himself, but is answering questions inappropriately. The patient has a past medical history of diabetes and hypertension. His temperature is 98.3°F (36.8°C), blood pressure is 127/85 mmHg, pulse is 138/min, respirations are 14/min, and oxygen saturation is 99% on room air. Physical exam is notable for a confused man with dry mucous membranes. Initial laboratory studies are ordered as seen below.
Serum:
Na+: 135 mEq/L
Cl-: 100 mEq/L
K+: 3.0 mEq/L
HCO3-: 23 mEq/L
BUN: 30 mg/dL
Glucose: 1,299 mg/dL
Creatinine: 1.5 mg/dL
Ca2+: 10.2 mg/dL
Which of the following is the most appropriate initial treatment for this patient?
- A. Insulin, normal saline, and potassium (Correct Answer)
- B. Normal saline and potassium
- C. Insulin and potassium
- D. Insulin
- E. Insulin and normal saline
Insulin preparations and kinetics Explanation: ***Insulin, normal saline, and potassium***
- This patient is presenting with **hyperosmolar hyperglycemic state (HHS)**, characterized by severe hyperglycemia (glucose 1299 mg/dL), dehydration (dry mucous membranes, high BUN and creatinine), and altered mental status. The initial treatment involves intravenous fluids to correct dehydration, insulin to lower blood glucose, and potassium supplementation due to potential shifts as insulin is administered.
- **Normal saline** addresses the severe dehydration, **insulin** corrects hyperglycemia, and **potassium supplementation** prevents hypokalemia, which is common during HHS treatment as glucose and potassium shift intracellularly.
*Normal saline and potassium*
- While **normal saline** and **potassium** are crucial for rehydration and electrolyte balance, omitting **insulin** would fail to address the core problem of severe hyperglycemia in HHS.
- Without insulin, blood glucose levels will remain dangerously high, leading to persistent osmotic diuresis and worsening dehydration.
*Insulin and potassium*
- Administering **insulin** without addressing the profound **dehydration** with intravenous fluids can lead to **hypovolemic shock** as insulin further drives glucose and water into cells.
- Rehydration is the priority in HHS management before or concurrent with insulin administration.
*Insulin*
- Giving only **insulin** would be detrimental, as the patient is severely dehydrated and hypokalemic (K+ 3.0 mEq/L, and will drop further with insulin).
- This approach would exacerbate dehydration and could cause life-threatening arrhythmias due to severe hypokalemia.
*Insulin and normal saline*
- While addressing hyperglycemia and dehydration, omitting **potassium supplementation** is dangerous because insulin drives potassium into cells, potentially causing severe **hypokalemia** and cardiac arrhythmias.
- The patient already has a low-normal potassium level, which will likely drop further with insulin treatment.
Insulin preparations and kinetics US Medical PG Question 2: A 21-year-old man presents to the office for a follow-up visit. He was recently diagnosed with type 1 diabetes mellitus after being hospitalized for diabetic ketoacidosis following a respiratory infection. He is here today to discuss treatment options available for his condition. The doctor mentions a recent study in which researchers have developed a new version of the insulin pump that appears efficacious in type 1 diabetics. They are currently comparing it to insulin injection therapy. This new pump is not yet available, but it looks very promising. At what stage of clinical trials is this current treatment most likely at?
- A. Phase 0
- B. Phase 2
- C. Phase 3 (Correct Answer)
- D. Phase 1
- E. Phase 4
Insulin preparations and kinetics Explanation: ***Phase 3***
- **Phase 3 trials** involve large-scale studies comparing the new treatment to standard therapy or placebo, often across multiple centers.
- The scenario describes a "new version of the insulin pump" being compared to "insulin injection therapy," indicating a definitive comparison for efficacy and safety against existing treatments.
*Phase 0*
- **Phase 0 trials** are exploratory, small-scale studies (10-15 subjects) using micro-doses to gather preliminary data on pharmacodynamics and pharmacokinetics, not efficacy comparisons.
- They are typically conducted very early in drug development, examining if the drug behaves as expected in humans.
*Phase 2*
- **Phase 2 trials** evaluate the efficacy and further assess safety of a new treatment in a larger group of patients (tens to hundreds).
- While they assess efficacy, they usually don't involve direct comparison with an established standard therapy on the scale implied by the question, which is typically reserved for Phase 3.
*Phase 1*
- **Phase 1 trials** primarily focus on safety, dosage, and side effects in a small group of healthy volunteers or patients with the condition (20-100 subjects).
- These trials are not designed to assess a treatment's efficacy against an existing therapy.
*Phase 4*
- **Phase 4 trials** occur after a drug or device has been approved and marketed, focusing on long-term safety, effectiveness in diverse populations, and new indications.
- The described pump "is not yet available," indicating it has not reached the market and thus is not in Phase 4.
Insulin preparations and kinetics US Medical PG Question 3: A 16-year-old woman presents to the emergency department for evaluation of acute vomiting and abdominal pain. Onset was roughly 3 hours ago while she was sleeping. She has no known past medical history. Her family history is positive for hypothyroidism and diabetes mellitus in her maternal grandmother. On examination, she is found to have fruity breath and poor skin turgor. She appears fatigued and her consciousness is slightly altered. Laboratory results show a blood glucose level of 691 mg/dL, sodium of 125 mg/dL, and elevated serum ketones. Of the following, which is the next best step in patient management?
- A. Administer IV fluids and insulin (Correct Answer)
- B. Initiate basal-bolus insulin regimen
- C. Initiate insulin glargine 10 units at bedtime only
- D. Initiate oral antidiabetic medications
- E. Initiate insulin aspart at mealtimes only
Insulin preparations and kinetics Explanation: ***Administer IV fluids and insulin***
- The patient presents with **fruity breath**, **altered consciousness**, **hyperglycemia (691 mg/dL)**, **hyponatremia**, and **elevated serum ketones**, which are classic signs of **diabetic ketoacidosis (DKA)**.
- The immediate management for DKA involves aggressive **intravenous fluid resuscitation** to correct dehydration and hypovolemia, followed by a continuous **intravenous insulin infusion** to lower blood glucose and suppress ketogenesis.
*Initiate basal-bolus insulin regimen*
- A **basal-bolus insulin regimen** is appropriate for long-term management of diabetes but is not the immediate treatment for acute DKA, which requires continuous intravenous insulin.
- This approach does not address the severe dehydration and electrolyte imbalances seen in DKA, which need urgent fluid replacement.
*Initiate insulin glargine 10 units at bedtime only*
- **Insulin glargine** is a long-acting insulin used for basal insulin coverage, typically in the chronic management of diabetes.
- This dose is insufficient to manage acute DKA, and it also fails to address the critical need for fluid resuscitation.
*Initiate oral antidiabetic medications*
- **Oral antidiabetic medications** are suitable for individuals with type 2 diabetes or milder forms of insulin resistance, not for acute DKA.
- They are ineffective in severe hyperglycemia and metabolic acidosis characteristic of DKA, and do not address dehydration.
*Initiate insulin aspart at mealtimes only*
- **Insulin aspart** is a rapid-acting insulin used to cover mealtime glucose excursions.
- Administering it only at mealtimes is inadequate for acute DKA, which requires continuous insulin infusion and aggressive fluid management.
Insulin preparations and kinetics US Medical PG Question 4: A 22-year-old woman with type 1 diabetes mellitus and mild asthma comes to the physician for a follow-up examination. She has had several episodes of sweating, dizziness, and nausea in the past 2 months that occur during the day and always resolve after she drinks orange juice. She is compliant with her diet and insulin regimen. The physician recommends lowering her insulin dose in certain situations. This recommendation is most important in which of the following situations?
- A. After a stressful exam
- B. During a viral infection
- C. Before exercise (Correct Answer)
- D. After large meals
- E. During pregnancy
Insulin preparations and kinetics Explanation: ***Before exercise***
- Exercise increases **glucose utilization** by muscles, which can lead to **hypoglycemia** in individuals taking insulin if the dose isn't adjusted.
- The patient's symptoms (sweating, dizziness, nausea) are classic for **hypoglycemia**, which resolves with sugar intake (orange juice).
*After a stressful exam*
- **Stress** typically elevates **counter-regulatory hormones** (e.g., cortisol, epinephrine), which can increase blood glucose levels rather than cause hypoglycemia.
- An insulin dose reduction is usually not necessary and could lead to **hyperglycemia** in this situation.
*During a viral infection*
- Infections, even viral ones, often trigger the release of **stress hormones**, increasing glucose production and leading to **hyperglycemia** and increased insulin requirements.
- Insulin doses usually need to be *increased*, not decreased, during illness to manage elevated blood sugar.
*After large meals*
- Large meals, especially those rich in carbohydrates, would necessitate an **increased or consistent insulin dose** to cover the glucose intake and prevent **postprandial hyperglycemia**.
- Reducing insulin after a large meal would likely lead to uncontrolled high blood sugar rather than prevent hypoglycemia.
*During pregnancy*
- While insulin requirements can fluctuate throughout pregnancy, they generally **increase** in the second and third trimesters due to increased **insulin resistance**.
- Reducing insulin during pregnancy without careful monitoring could lead to uncontrolled **hyperglycemia**, posing risks to both mother and fetus.
Insulin preparations and kinetics US Medical PG Question 5: A 14-year-old female with no past medical history presents to the emergency department with nausea and abdominal pain. On physical examination, her blood pressure is 78/65, her respiratory rate is 30, her breath has a fruity odor, and capillary refill is > 3 seconds. Serum glucose is 820 mg/dL. After starting IV fluids, what is the next best step in the management of this patient?
- A. Intravenous Dextrose in water
- B. Subcutaneous insulin glargine
- C. Intravenous regular insulin (Correct Answer)
- D. Intravenous glucagon
- E. Subcutaneous insulin lispro
Insulin preparations and kinetics Explanation: ***Intravenous regular insulin***
- The patient presents with **diabetic ketoacidosis (DKA)**, characterized by **hyperglycemia**, **fruity breath** (due to ketones), and **hypotension**. Prompt administration of **intravenous regular insulin** is crucial to lower blood glucose and resolve ketoacidosis.
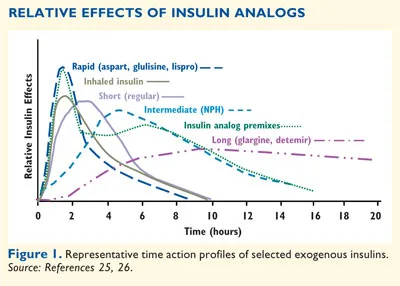
- **Regular insulin** is preferred intravenously due to its **rapid onset** and short duration of action, allowing for precise titration and continuous adjustment based on glucose levels.
*Intravenous Dextrose in water*
- **Dextrose** would further increase the already severely elevated blood glucose level in a patient with DKA, worsening the metabolic derangements.
- Dextrose is typically initiated only after blood glucose drops to safe levels (<200 mg/dL) to prevent **hypoglycemia** during insulin infusion.
*Subcutaneous insulin glargine*
- **Insulin glargine** is a **long-acting insulin** designed for basal insulin coverage, not for acute management of severe hyperglycemia or DKA.
- Its **slow onset of action** and prolonged effect make it unsuitable for the urgent and rapid glucose reduction required in DKA.
*Intravenous glucagon*
- **Glucagon** is a hormone that **raises blood glucose levels**, counteracting the effects of insulin.
- Administering glucagon would exacerbate the severe hyperglycemia present in DKA and is used only in cases of severe hypoglycemia.
*Subcutaneous insulin lispro*
- **Insulin lispro** is a **rapid-acting insulin analog** but is typically given subcutaneously.
- While faster than regular insulin subcutaneously, the **subcutaneous route** has variable absorption in critically ill patients, and the immediate and precisely controllable effect of intravenous regular insulin is needed in DKA.
Insulin preparations and kinetics US Medical PG Question 6: A 56-year-old man presents for a follow-up regarding his management for type 2 diabetes mellitus (DM). He was diagnosed with type 2 DM about 7 years ago and was recently started on insulin therapy because oral agents were insufficient to control his glucose levels. He is currently following a regimen combining insulin lispro and neutral protamine Hagedorn (NPH) insulin. He is taking insulin lispro 3 times a day before meals and NPH insulin once in the morning. He has been on this regimen for about 2 months. He says that his glucose reading at night averages around 200 mg/dL and remains close to 180 mg/dL before his shot of NPH in the morning. The readings during the rest of the day range between 100–120 mg/dL. The patient denies any changes in vision or tingling or numbness in his hands or feet. His latest HbA1C level was 6.2%. Which of the following adjustments to his insulin regimen would be most effective in helping this patient achieve better glycemic control?
- A. Add another dose of insulin lispro in the evening.
- B. Reduce a dose of insulin lispro.
- C. Replace lispro with insulin aspart.
- D. Add insulin glargine to the current regimen.
- E. Add another dose of NPH in the evening. (Correct Answer)
Insulin preparations and kinetics Explanation: ***Add another dose of NPH in the evening.***
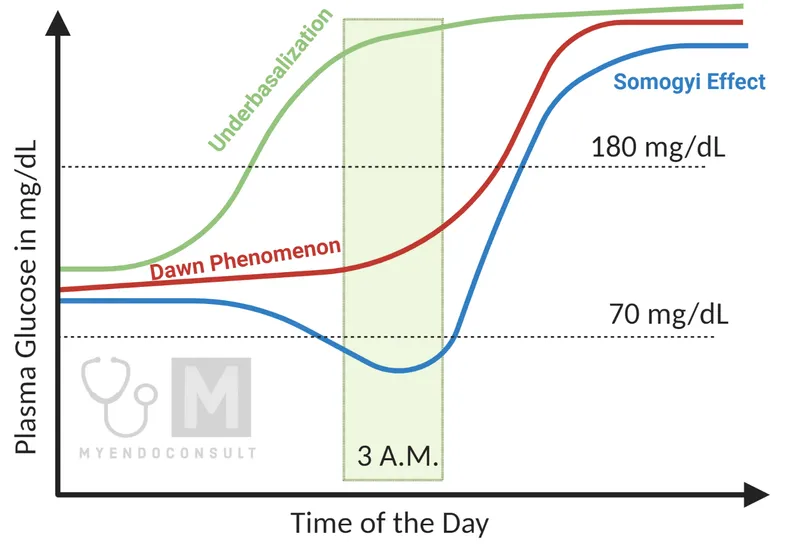
- The patient has persistently elevated **nighttime** and **pre-morning glucose levels** (200 mg/dL and 180 mg/dL, respectively), while daytime levels are well-controlled. This indicates insufficient **basal insulin coverage** overnight.
- Adding a dose of **intermediate-acting NPH insulin** in the evening would provide longer-acting basal insulin to cover the overnight period and address the high morning fasting glucose.
*Add another dose of insulin lispro in the evening.*
- Insulin lispro is a **rapid-acting insulin** primarily used to cover post-prandial glucose spikes. Adding another dose would primarily affect post-dinner glucose, not the sustained overnight hyperglycemia.
- While it might slightly lower evening glucose, its short duration of action would not adequately address the **pre-morning hyperglycemia**.
*Reduce a dose of insulin lispro.*
- The patient's **daytime glucose levels (100–120 mg/dL)** are well-controlled, suggesting that the current lispro doses are appropriate for meal coverage.
- Reducing lispro could lead to **post-prandial hyperglycemia** during the day, worsening overall control.
*Replace lispro with insulin aspart.*
- Both insulin lispro and insulin aspart are **rapid-acting insulins** with very similar pharmacokinetics and duration of action.
- Replacing one with the other would likely not significantly alter the glycemic profile, as the problem lies with **basal insulin coverage**, not rapid-acting insulin.
*Add insulin glargine to the current regimen.*
- While **insulin glargine** is a **long-acting basal insulin** and could address the overnight hyperglycemia, the patient is already on NPH as his basal insulin.
- The simpler and more direct adjustment would be to optimize the **existing NPH regimen** by adding an evening dose, rather than introducing a new type of basal insulin, which might complicate the regimen further or be less cost-effective.
Insulin preparations and kinetics US Medical PG Question 7: A 28-year-old man is brought in by ambulance to the ER, barely conscious, after feeling drowsy and falling to the floor during a presentation several hours ago. His colleague who accompanied him says he has had similar episodes 5 times in the past 3 months. No significant past medical history. His blood pressure is 110/80 mm Hg and pulse is 114/min. His capillary blood glucose is 15 mg/dL. Immediate IV dextrose with thiamine is started, and he rapidly regains consciousness. A contrast CT of the abdomen is performed which reveals a tumor in the pancreas. Which of the following relative laboratory findings would you most likely expect to find in this patient?
- A. Glucose: ↑, Insulin: ↓, C-Peptide: ↓, Ketoacidosis: Present
- B. Glucose: Normal, Insulin: Normal, C-Peptide: Normal, Ketoacidosis: Absent
- C. Glucose: ↓, Insulin: ↑, C-Peptide: ↑, Ketoacidosis: Absent (Correct Answer)
- D. Glucose: ↓, Insulin: ↑, C-Peptide: ↓, Ketoacidosis: Absent
- E. Glucose: ↑, Insulin: ↑/Normal, C-Peptide: ↑/Normal, Ketoacidosis: Absent
Insulin preparations and kinetics Explanation: ***Glucose: ↓, Insulin: ↑, C-Peptide: ↑, Ketoacidosis: Absent***
- The patient's **hypoglycemia (15 mg/dL)**, coupled with a pancreatic tumor and recurrent episodes, strongly suggests an **insulinoma**.
- An **insulinoma** is an insulin-secreting tumor, leading to **high insulin** and **C-peptide** levels in the presence of low glucose, and typically no ketoacidosis because insulin inhibits ketogenesis.
*Glucose: ↑, Insulin: ↓, C-Peptide: ↓, Ketoacidosis: Present*
- This profile describes **Type 1 Diabetes Mellitus** or severe insulin deficiency, where high glucose is due to lack of insulin production and subsequent diabetic ketoacidosis.
- The patient's symptoms (hypoglycemia) and the presence of a pancreatic tumor producing insulin are contradictory to this profile.
*Glucose: Normal, Insulin: Normal, C-Peptide: Normal, Ketoacidosis: Absent*
- This profile represents a **healthy individual** with normal metabolic function, which is inconsistent with the patient's severe hypoglycemia and recurrent collapses.
- It would not explain the patient's symptoms or the pancreatic tumor's function.
*Glucose: ↓, Insulin: ↑, C-Peptide: ↓, Ketoacidosis: Absent*
- This finding would be typical of **exogenous insulin administration** (e.g., insulin overdose) where insulin levels are high, but C-peptide (which is co-secreted with endogenous insulin) is low.
- While hypoglycemia is present, the low C-peptide contradicts the presence of an endogenous insulin-secreting pancreatic tumor.
*Glucose: ↑, Insulin: ↑/Normal, C-Peptide: ↑/Normal, Ketoacidosis: Absent*
- These findings could be seen in conditions like **Type 2 Diabetes** with **insulin resistance** or Cushing's syndrome where glucose and insulin might be elevated, but the patient's primary presentation is severe hypoglycemia.
- This profile does not align with the patient's profound hypoglycemia and clinical picture of an insulinoma.
Insulin preparations and kinetics US Medical PG Question 8: A 14-year-old boy is rushed to the emergency room after he became disoriented at home. His parents say that the boy was doing well until 2 days ago when he got sick and vomited several times. They thought he was recovering but today he appeared to be disoriented since the morning. His vitals are normal except shallow rapid breathing at a rate of 33/min. His blood sugar level is 654 mg/dL and urine is positive for ketone bodies. He is diagnosed with diabetic ketoacidosis and is managed with fluids and insulin. He responds well to the therapy. His parents are told that their son has type 1 diabetes and insulin therapy options are being discussed. Which of the following types of insulin can be used in this patient for the rapid action required during mealtimes?
- A. Insulin detemir
- B. Insulin degludec
- C. NPH insulin
- D. Insulin glargine
- E. Insulin lispro (Correct Answer)
Insulin preparations and kinetics Explanation: ***Insulin lispro***
- **Insulin lispro** is a **rapid-acting insulin analog** designed to be taken immediately before or with a meal, offering quick onset (5-15 minutes) and short duration of action.
- Its rapid action helps to control **postprandial glucose spikes**, closely mimicking the physiological insulin response to food, which is crucial for mealtime coverage in **Type 1 diabetes**.
*Insulin detemir*
- **Insulin detemir** is a **long-acting insulin analog** used for basal insulin coverage, providing a relatively constant insulin level over an extended period (12-24 hours).
- It is not suitable for **mealtime insulin coverage** due to its slow onset of action and prolonged duration, which would not effectively manage postprandial glucose excursions.
*Insulin degludec*
- **Insulin degludec** is an **ultra-long-acting basal insulin analog** with a duration of action exceeding 42 hours, providing stable basal coverage.
- Its extremely slow onset and prolonged duration make it unsuitable for **prandial (mealtime) insulin**, as it cannot address the rapid rise in blood glucose following a meal.
*NPH insulin*
- **NPH (Neutral Protamine Hagedorn) insulin** is an **intermediate-acting insulin** that provides basal insulin coverage, with an onset of 2-4 hours and a peak effect around 6-10 hours.
- Its slow onset and prolonged action make it unsuitable for **mealtime insulin coverage**, as it would not adequately prevent the rapid rise in blood sugar immediately after eating.
*Insulin glargine*
- **Insulin glargine** is a **long-acting insulin analog** used for **basal insulin coverage**, providing a relatively flat and peakless insulin profile over 24 hours.
- It is not used for **prandial (mealtime) insulin** because its slow onset and sustained action would not effectively counteract the rapid rise in blood glucose following a meal.
Insulin preparations and kinetics US Medical PG Question 9: A 71-year-old male is admitted to the hospital with a Staphylococcal aureus infection of his decubitus ulcers. He is diabetic and has a body mass index of 45. His temperature is 37°C (98.6°F), respirations are 15/min, pulse is 67/min and blood pressure is 122/98 mm Hg. The nurse is monitoring his blood glucose and records it as 63 mg/dL. She then asks the resident on call if the patient should receive glargine insulin as ordered seeing his glucose levels. Which of the following would be the most appropriate response by the resident?
- A. No, due to his S. aureus infection he is more likely to have low blood glucose and glargine insulin should be held until he has recovered.
- B. No, glargine insulin was probably ordered in error as it is not recommended in type 2 diabetes.
- C. No, glargine insulin should be stopped and replaced with lispro insulin until his blood glucose increases.
- D. Yes, glargine insulin is a long-acting insulin and should still be given to control his blood glucose over the next 24 hours.
- E. No, glargine insulin should not be given during an episode of hypoglycemia as it will further lower blood glucose. (Correct Answer)
Insulin preparations and kinetics Explanation: ***No, glargine insulin should not be given during an episode of hypoglycemia as it will further lower blood glucose.***
- The patient's blood glucose is **63 mg/dL**, which is **hypoglycemic** (typically defined as <70 mg/dL). Administering additional long-acting insulin like glargine would further decrease blood glucose and potentially cause serious harm.
- **Glargine insulin** is a **long-acting basal insulin** designed to provide a steady release of insulin over 24 hours. While crucial for long-term glucose control, it should be held during acute hypoglycemic episodes to prevent severe glucose drops.
*No, due to his S. aureus infection he is more likely to have low blood glucose and glargine insulin should be held until he has recovered.*
- Infections, especially severe ones, cause **physiological stress** and typically lead to **increased blood glucose levels** due to elevated counter-regulatory hormones, not lower levels.
- While insulin should be held during a hypoglycemic episode, the reasoning given here regarding infection causing low blood glucose is generally incorrect; infections usually cause hyperglycemia.
*No, glargine insulin was probably ordered in error as it is not recommended in type 2 diabetes.*
- **Glargine insulin** is a commonly used and **effective basal insulin** for managing type 2 diabetes, especially when oral agents or other shorter-acting insulins are insufficient.
- Basal insulin, like glargine, is a cornerstone in the treatment of many patients with **type 2 diabetes** to maintain stable glucose levels overnight and between meals.
*No, glargine insulin should be stopped and replaced with lispro insulin until his blood glucose increases.*
- **Lispro insulin** is a **rapid-acting insulin** used to cover meals or correct acute hyperglycemia; it is not a direct replacement for basal insulin like glargine, particularly in a hypoglycemic state.
- **Stopping glargine** during hypoglycemia is correct, but replacing it with another insulin, especially rapid-acting, without addressing the hypoglycemia and understanding the cause would be inappropriate and potentially dangerous.
*Yes, glargine insulin is a long-acting insulin and should still be given to control his blood glucose over the next 24 hours.*
- While glargine is a long-acting insulin, administering it during an active state of **hypoglycemia (63 mg/dL)** is not appropriate, as it would worsen the low blood sugar.
- The immediate priority in hypoglycemia is to **safely raise blood glucose**, not to administer more insulin, regardless of its duration of action.
Insulin preparations and kinetics US Medical PG Question 10: A researcher is tracing the fate of C-peptide, a product of preproinsulin cleavage. Which of the following is a true statement regarding the fate of C-peptide?
- A. C-peptide exits the cells via a protein channel
- B. C-peptide is further cleaved into insulin
- C. C-peptide is packaged with insulin in secretory vesicles (Correct Answer)
- D. C-peptide is immediately degraded by the proteasome
- E. C-peptide activates an intracellular signaling cascade
Insulin preparations and kinetics Explanation: ***C-peptide is packaged with insulin in secretory vesicles***
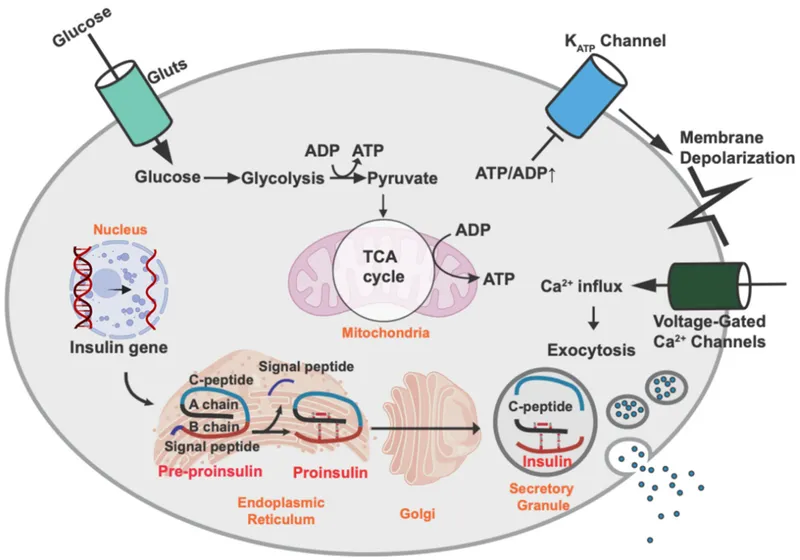
- Preproinsulin is cleaved in the **endoplasmic reticulum** to proinsulin (signal peptide removal), which is then transported to the **Golgi apparatus**.
- In the Golgi, proinsulin is cleaved by **prohormone convertases** into **insulin** and **C-peptide**, and both are stored together in **secretory vesicles** within the pancreatic beta cells.
- Upon stimulation, both insulin and C-peptide are **co-secreted** via exocytosis in equimolar amounts, making C-peptide a useful marker of endogenous insulin secretion.
*C-peptide exits the cells via a protein channel*
- C-peptide exits the beta cells via **exocytosis** of secretory granules, not through specific protein channels.
- It is **co-secreted with insulin** when secretory vesicles fuse with the plasma membrane.
- Its presence in the bloodstream in equimolar amounts with insulin makes it an indirect measure of **insulin secretion**.
*C-peptide is further cleaved into insulin*
- **C-peptide** is a product of proinsulin cleavage, alongside insulin; it is not further processed into insulin.
- Insulin itself is composed of two **peptide chains (A and B)** linked by disulfide bonds, formed after C-peptide is removed from proinsulin.
*C-peptide is immediately degraded by the proteasome*
- C-peptide is not immediately degraded by the **proteasome** upon synthesis.
- After secretion, it circulates in the blood with a **longer half-life** than insulin (approximately 30 minutes versus 4-6 minutes), allowing it to be a useful marker of endogenous insulin production.
- Its degradation occurs primarily in the **kidney**.
*C-peptide activates an intracellular signaling cascade*
- While there is some research suggesting C-peptide may have independent **biological activity** and activate certain signaling pathways extracellularly, its primary role in the context of the insulin synthesis pathway is as a **byproduct** of proinsulin processing.
- Its clinical utility is primarily as a **biomarker** of endogenous insulin secretion, particularly useful in distinguishing between endogenous and exogenous insulin in diabetic patients.
More Insulin preparations and kinetics US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.