GLP-1 receptor agonists US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for GLP-1 receptor agonists. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
GLP-1 receptor agonists US Medical PG Question 1: A 69-year-old man with type 2 diabetes mellitus comes to the physician for a follow-up examination. His only medication is metformin. He has tried to lose weight for several years without success. He is 168 cm (5 ft 6 in) tall and weighs 110 kg (243 lb); BMI is 39 kg/m2. His hemoglobin A1c is 8.5%. Which of the following is the most appropriate antidiabetic drug to address both this patient's glucose control and weight?
- A. Nateglinide
- B. Rosiglitazone
- C. Liraglutide (Correct Answer)
- D. Miglitol
- E. Glipizide
GLP-1 receptor agonists Explanation: ***Liraglutide***
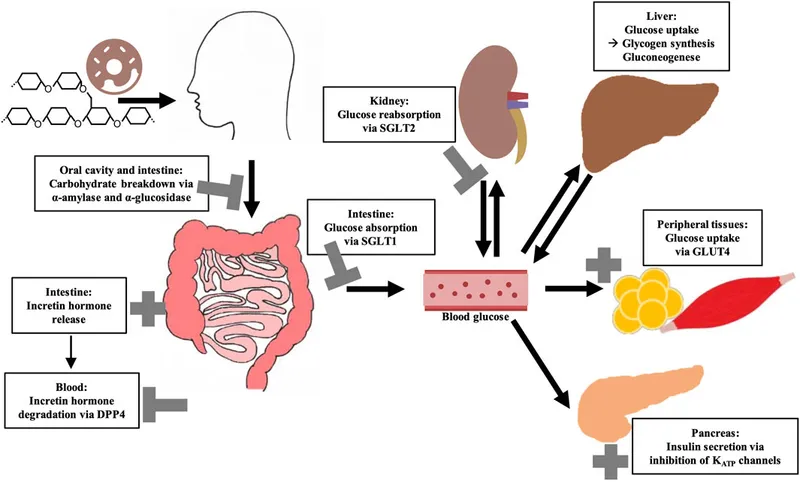
- **Liraglutide** is a **glucagon-like peptide-1 (GLP-1) receptor agonist** that improves glycemic control by increasing glucose-dependent insulin secretion, decreasing glucagon secretion, and slowing gastric emptying.
- A significant side effect of GLP-1 agonists is **weight loss**, making it an ideal choice for this patient who is obese (BMI 39 kg/m2) and struggling with weight management while having suboptimal glycemic control (HbA1c 8.5%).
*Nateglinide*
- **Nateglinide** is a **meglitinide**, which stimulates insulin release from pancreatic beta cells, similar to sulfonylureas, but with a more rapid and short-lived effect.
- While it helps in glucose control, it is often associated with **weight gain** and does not address the patient's desire for weight loss.
*Rosiglitazone*
- **Rosiglitazone** is a **thiazolidinedione (TZD)** that improves insulin sensitivity by acting on PPAR-gamma receptors.
- TZDs are commonly associated with **weight gain** and fluid retention, which would be detrimental to this patient's weight management goals.
*Miglitol*
- **Miglitol** is an **alpha-glucosidase inhibitor** that delays the absorption of carbohydrates from the gut, reducing postprandial glucose excursions.
- While it can help with glucose control and is weight-neutral or may cause modest weight loss, its efficacy in reducing HbA1c is generally lower compared to other agents, and it commonly causes **gastrointestinal side effects** like flatulence and diarrhea.
*Glipizide*
- **Glipizide** is a **sulfonylurea** that stimulates insulin secretion from pancreatic beta cells independently of glucose concentration.
- It is associated with a risk of **hypoglycemia** and often leads to **weight gain**, which is not suitable for a patient who needs to lose weight.
GLP-1 receptor agonists US Medical PG Question 2: An endocrinologist is working with a pharmaceutical research company on a new drug for diabetes mellitus type 2 (DM2). In their experimental studies, they isolated a component from Gila monster saliva, which was found to have > 50% homology with glucagon-like peptide-1 (GLP1). During the animal studies, the experimental drug was found to have no GLP1 agonist effect. Instead, it irreversibly binds DPP-IV with a higher affinity than GLP1. Which of the following drugs has a similar mechanism of action to this new experimental drug?
- A. Metformin
- B. Sitagliptin (Correct Answer)
- C. Canagliflozin
- D. Pramlintide
- E. Exenatide
GLP-1 receptor agonists Explanation: ***Sitagliptin***
- This drug is a **dipeptidyl peptidase-4 (DPP-4) inhibitor**, which works by preventing the breakdown of **endogenous GLP-1** and other incretin hormones.
- By inhibiting DPP-4, sitagliptin increases the availability of GLP-1, leading to **glucose-dependent insulin secretion** and reduced glucagon secretion.
- **Note:** While sitagliptin is a **reversible** DPP-4 inhibitor and the experimental drug is described as irreversible, sitagliptin shares the same **target enzyme (DPP-4)** and overall therapeutic mechanism, making it the closest match among the options provided.
*Metformin*
- Metformin is a **biguanide** that primarily reduces **hepatic glucose production** and improves insulin sensitivity in peripheral tissues.
- Its mechanism does not involve direct interaction with DPP-4 or GLP-1 pathways, unlike the experimental drug.
*Canagliflozin*
- Canagliflozin is a **sodium-glucose co-transporter 2 (SGLT2) inhibitor** that blocks glucose reabsorption in the kidneys, leading to **increased urinary glucose excretion**.
- Its action is independent of insulin and does not involve the incretin system or DPP-4 inhibition.
*Pramlintide*
- Pramlintide is an **amylin analog** that works by slowing gastric emptying, suppressing glucagon secretion, and promoting satiety.
- It is administered via injection and acts synergistically with insulin, but does not affect DPP-4 enzyme activity.
*Exenatide*
- Exenatide is a **glucagon-like peptide-1 (GLP-1) receptor agonist** that directly mimics the action of GLP-1, stimulating insulin release and suppressing glucagon.
- Notably, exenatide is also derived from Gila monster saliva (similar to the experimental drug's origin), but it acts as a GLP-1 agonist rather than a DPP-4 inhibitor, which is the opposite mechanism described for the experimental drug.
GLP-1 receptor agonists US Medical PG Question 3: A 45-year-old woman comes to the clinic for complaints of abdominal pain and repeated watery stools for the past 2 days. She has a history of bowel complaints for the past 2 years consisting of periods of intermittent loose stools followed by the inability to make a bowel movement. Her past medical history is significant for diabetes controlled with metformin. She denies any abnormal oral intake, weight loss, fever, nausea/vomiting, or similar symptoms in her family. When asked to describe her stool, she reports that “it is just very watery and frequent, but no blood.” The physician prescribes a medication aimed to alleviate her symptoms. What is the most likely mechanism of action of this drug?
- A. Enteric nerve stimulation
- B. Substance P antagonist
- C. mu-opioid receptor agonist (Correct Answer)
- D. PGE1 analog
- E. D2 receptor antagonist
GLP-1 receptor agonists Explanation: ***mu-opioid receptor agonist***
- The patient's history of alternating **diarrhea and constipation**, absence of alarming features like weight loss or bloody stools, and chronic nature are highly suggestive of **Irritable Bowel Syndrome (IBS)**, specifically mixed type (IBS-M) or diarrhea-predominant (IBS-D) experiencing a flare.
- Medications like **loperamide** (an over-the-counter mu-opioid receptor agonist) work by reducing **gastrointestinal motility** and increasing water absorption, effectively treating acute episodes of diarrhea in IBS.
*Enteric nerve stimulation*
- Medications that stimulate enteric nerves generally **increase gut motility**, which would worsen diarrhea rather than alleviate it.
- This mechanism is characteristic of **prokinetic agents**, which are used to treat conditions like gastroparesis, not diarrhea.
*Substance P antagonist*
- **Substance P** is a neuropeptide involved in pain transmission and inflammation, and its antagonists have been investigated for conditions like IBS with pain.
- However, they do not directly address the primary symptom of **watery stools** by altering motility or absorption.
*PGE1 analog*
- **PGE1 analogs** (e.g., misoprostol) are used to protect the gastric mucosa and can cause **diarrhea** as a side effect due to increased intestinal motility and fluid secretion.
- This mechanism would exacerbate the patient's symptoms rather than relieve them.
*D2 receptor antagonist*
- **D2 receptor antagonists** (e.g., metoclopramide) are primarily antiemetics and prokinetic agents that **increase gastric emptying** and intestinal transit.
- While they can relieve nausea and vomiting, they are not first-line treatments for diarrhea and could potentially worsen it in some cases due to increased motility.
GLP-1 receptor agonists US Medical PG Question 4: A 30-year-old obese female presents with new-onset headaches, ringing in her ears, and blurry vision. Ibuprofen and avoidance of light has not relieved her symptoms. She denies a history of recent trauma, fever, chills, and fatigue. Past medical history is significant for type 2 diabetes mellitus managed with metformin. She has had 20/20 vision her whole life and wonders if she might need to get eyeglasses. She has 2 healthy school-age children. Her temperature is 36.8°C (98.2°F), heart rate is 90/min, respiratory rate is 15/min, and blood pressure is 135/80 mm Hg. Physical exam is notable for decreased lateral eye movement, and the funduscopic findings are shown in the picture. Laboratory findings are within normal limits and brain imaging is normal. Lumbar puncture demonstrates an elevated opening pressure and normal CSF composition. Which of the following is a side effect of the medication used to treat this condition?
- A. Elevated liver function tests
- B. Rhabdomyolysis
- C. Kidney stones (Correct Answer)
- D. Pancreatitis
- E. Decreased white blood cell count
GLP-1 receptor agonists Explanation: ***Kidney stones***
- The patient's symptoms (headaches, tinnitus, blurry vision), **obesity**, normal brain imaging, and **elevated CSF opening pressure with normal CSF composition** are classic for **idiopathic intracranial hypertension (IIH)**, also known as pseudotumor cerebri.
- The first-line medical treatment for IIH is **acetazolamide**, a carbonic anhydrase inhibitor, which commonly causes **kidney stones** due to altered urine pH and reduced citrate excretion.
*Elevated liver function tests*
- While some medications can cause elevated liver function tests, this is not a typical or common side effect of **acetazolamide**.
- **Acetaminophen** overdose or certain antibiotics are more frequently associated with this side effect.
*Rhabdomyolysis*
- **Rhabdomyolysis** is characterized by muscle breakdown and is often associated with statin use, significant trauma, or certain illicit drugs.
- It is not a known side effect of **acetazolamide**.
*Pancreatitis*
- **Pancreatitis** can be a side effect of various medications (e.g., thiopurines, certain diuretics), but it is not commonly associated with **acetazolamide**.
- The patient's history of Type 2 Diabetes is a risk factor for pancreatitis, but not directly linked to the treatment of IIH.
*Decreased white blood cell count*
- A decrease in white blood cell count (leukopenia or agranulocytosis) is a serious but rare side effect of certain medications, such as **clozapine** or **methimazole**.
- It is not a typical side effect of **acetazolamide**.
GLP-1 receptor agonists US Medical PG Question 5: A 58-year-old male presents to the clinic for a follow-up visit. He takes metformin every day and says that he is compliant with his medication but can not control his diet. Three months prior, his HbA1c was 8.2% when he was started on metformin. He does not have any complaints on this visit. His temperature is 37°C (98.6°F), respirations are 15/min, pulse is 67/min and blood pressure is 122/88 mm Hg. His BMI is 33. Physical examination is within normal limits. Blood is drawn for laboratory tests and the results are given below:
Fasting blood glucose 150 mg/dL
Glycated hemoglobin (HbA1c) 7.2 %
Serum Creatinine 1.1 mg/dL
BUN 12 mg/dL
The physician wants to initiate another medication for his blood glucose control, specifically one that does not carry a risk of weight gain. Addition of which of the following drugs would be most suitable for this patient?
- A. Sitagliptin (Correct Answer)
- B. Glimepiride
- C. Rosiglitazone
- D. Glyburide
- E. Pioglitazone
GLP-1 receptor agonists Explanation: ***Sitagliptin***
- This is a **dipeptidyl peptidase-4 (DPP-4) inhibitor** that enhances incretin effects, leading to glucose-dependent insulin secretion and suppressed glucagon.
- DPP-4 inhibitors like sitagliptin are **weight-neutral** and pose a low risk of hypoglycemia, making them suitable additions for patients who need further glycemic control without weight gain, especially with their current BMI.
*Glimepiride*
- This is a **sulfonylurea** that stimulates insulin release from pancreatic beta cells independently of glucose levels.
- Sulfonylureas are associated with a **risk of weight gain** and hypoglycemia, which is an undesirable effect for this patient.
*Rosiglitazone*
- This is a **thiazolidinedione (TZD)** that improves insulin sensitivity in peripheral tissues and the liver.
- TZDs, including rosiglitazone, are associated with **weight gain** due to fluid retention and increased adipogenesis, and can also cause congestive heart failure.
*Glyburide*
- This is also a **sulfonylurea**, similar to glimepiride, that stimulates insulin secretion.
- Like other sulfonylureas, glyburide carries a significant risk of **weight gain** and hypoglycemia, making it less ideal for this patient.
*Pioglitazone*
- This is another **thiazolidinedione (TZD)** that improves insulin sensitivity.
- Pioglitazone is known to cause **weight gain** and fluid retention, and it has a black box warning for exacerbating heart failure.
GLP-1 receptor agonists US Medical PG Question 6: A 49-year-old woman presents to the family medicine clinic with concerns about her weight. She has been constantly gaining weight for a decade now as she has not been able to control her diet. She has tried exercising but says that she is too lazy for this method of weight loss to work. Her temperature is 37° C (98.6° F), respirations are 15/min, pulse is 67/min, and blood pressure is 122/88 mm Hg. Her BMI is 30. Her labs from her past visit show:
Fasting blood glucose: 149 mg/dL
Glycated hemoglobin (HbA1c): 9.1%
Triglycerides: 175 mg/dL
LDL-Cholesterol: 102 mg/dL
HDL-Cholesterol: 35 mg/dL
Total Cholesterol: 180 mg/dL
Serum creatinine: 1.0 mg/dL
BUN: 12 mg/dL
Serum:
Albumin: 4.2 gm/dL
Alkaline phosphatase: 150 U/L
Alanine aminotransferase: 76 U/L
Aspartate aminotransferase: 88 U/L
After discussing the long term issues that will arise if her health does not improve, she agrees to modify her lifestyle and diet. Which of the following would be the best pharmacotherapy for this patient?
- A. Insulin
- B. Metformin (Correct Answer)
- C. Dietary modification alone
- D. Sitagliptin
- E. Glipizide
GLP-1 receptor agonists Explanation: ***Metformin***
- This patient has newly diagnosed **type 2 diabetes mellitus** (Fasting blood glucose 149 mg/dL, HbA1c 9.1%) in the setting of obesity (BMI 30). **Metformin** is the **first-line pharmacotherapy** for type 2 diabetes due to its efficacy, favorable safety profile, and potential for weight neutrality or modest weight loss.
- Metformin works by **decreasing hepatic glucose production**, decreasing intestinal glucose absorption, and increasing insulin sensitivity.
*Insulin*
- While insulin is highly effective in lowering blood glucose, it is typically reserved for patients with **very high HbA1c** (often >10%), **symptomatic hyperglycemia**, or those who have failed oral pharmacotherapy, it can also cause **weight gain**.
- Initiating insulin as first-line therapy can be overly aggressive and may lead to **hypoglycemia** in patients who can respond to oral agents.
*Dietary modification alone*
- Although **lifestyle changes** (diet and exercise) are crucial and can be remarkably effective, this patient's **HbA1c of 9.1%** indicates that **monotherapy with diet and exercise alone is insufficient** to achieve glycemic control.
- Pharmacotherapy is generally recommended for HbA1c levels **above 7.5%**, even with a commitment to lifestyle changes.
*Sitagliptin*
- **Sitagliptin** is a **DPP-4 inhibitor** that increases insulin secretion and decreases glucagon secretion in a glucose-dependent manner.
- It is often considered a **second-line agent** or an add-on therapy, as its HbA1c-lowering effect is generally less potent than metformin.
*Glipizide*
- **Glipizide** is a **sulfonylurea** that works by stimulating insulin release from pancreatic beta cells.
- It can cause **weight gain** and has a significant risk of **hypoglycemia**, making it a less favorable first-line agent, especially in an obese patient, compared to metformin.
GLP-1 receptor agonists US Medical PG Question 7: A 57-year-old woman presents to her physician for a checkup. The past medical history is significant for diabetes mellitus type 2, and a history of myocardial infarction. The current medications are aspirin, lisinopril, metoprolol, atorvastatin, and metformin. The patient’s HbA1c is 7.9%, and her fasting blood glucose is 8.9 mmol/L (160 mg/dL). Which of the following statements regarding the use of exenatide in this patient is most correct?
- A. It cannot be used in combination with metformin
- B. It requires daily subcutaneous injection
- C. It has a high risk of causing severe hypoglycemia when used alone
- D. It is contraindicated in patients with a history of myocardial infarction
- E. It is associated with weight loss in most patients (Correct Answer)
GLP-1 receptor agonists Explanation: ***It is associated with weight loss in most patients***
- Exenatide and other **GLP-1 receptor agonists** are consistently associated with **modest weight loss** (typically 2-5 kg) in the majority of patients.
- This occurs through multiple mechanisms: **delayed gastric emptying**, **increased satiety**, and **reduced appetite** via central nervous system effects.
- Weight loss is a significant **clinical benefit** in overweight diabetic patients and is one reason these agents are preferred in this population.
*It cannot be used in combination with metformin*
- Exenatide is **commonly combined with metformin** and this is an FDA-approved combination.
- They have **complementary mechanisms**: metformin reduces hepatic glucose production while exenatide enhances glucose-dependent insulin secretion.
- This combination is a **standard therapeutic approach** for type 2 diabetes management.
*It requires daily subcutaneous injection*
- The original exenatide formulation (Byetta) requires **twice-daily subcutaneous injections**, not once daily.
- An **extended-release formulation** (Bydureon) is available as a **once-weekly injection**.
- The statement is imprecise and not universally applicable to all exenatide formulations.
*It has a high risk of causing severe hypoglycemia when used alone*
- GLP-1 receptor agonists have a **low risk of hypoglycemia** when used as monotherapy because their insulinotropic effect is **glucose-dependent**.
- Insulin secretion only occurs when glucose levels are elevated, providing a **built-in safety mechanism**.
- Hypoglycemia risk increases when combined with **sulfonylureas or insulin**, but not with metformin alone.
*It is contraindicated in patients with a history of myocardial infarction*
- This is **FALSE**. Exenatide is **NOT contraindicated** in patients with prior MI.
- In fact, several GLP-1 receptor agonists have demonstrated **cardiovascular benefits** in outcome trials (LEADER, SUSTAIN-6).
- Current **ADA/ACC guidelines recommend** GLP-1 agonists in diabetic patients with established cardiovascular disease for risk reduction.
- The only absolute contraindication for exenatide is personal or family history of **medullary thyroid carcinoma** or **MEN 2 syndrome**.
GLP-1 receptor agonists US Medical PG Question 8: A 40-year-old woman with a recent history of carcinoma of the breast status post mastectomy and adjuvant chemotherapy one week ago presents for follow-up. She reports adequate pain control managed with the analgesic drug she was prescribed. Past medical history is significant for hepatitis C and major depressive disorder. The patient denies any history of smoking or alcohol use but says she is currently using intravenous heroin and has been for the past 10 years. However, she reports that she has been using much less heroin since she started taking the pain medication, which is confirmed by the toxicology screen. Which of the following is the primary mechanism of action of the analgesic drug she was most likely prescribed?
- A. Pure antagonist at opioid receptors
- B. Pure agonist at the µ-opioid receptor (Correct Answer)
- C. Inhibits prostaglandin synthesis
- D. Mixed agonist-antagonist at opioid receptors
- E. Central action via blockade of serotonin reuptake
GLP-1 receptor agonists Explanation: ***Pure agonist at the µ-opioid receptor***
- Opioid analgesics, commonly prescribed for **post-mastectomy pain** and cancer-related pain, primarily exert their effects by acting as **pure agonists at the µ-opioid receptor**.
- This activation leads to profound **analgesia** by modulating pain perception and emotional response to pain in the central nervous system.
*Pure antagonist at opioid receptors*
- A **pure antagonist** would block opioid receptors and **reverse** the effects of opioid agonists, not provide analgesia.
- Such drugs are used to treat **opioid overdose** (e.g., naloxone) or to manage addiction by preventing opioid effects.
*Inhibits prostaglandin synthesis*
- This is the mechanism of action for **NSAIDs** (non-steroidal anti-inflammatory drugs), which primarily treat **mild to moderate pain** and inflammation.
- NSAIDs are generally insufficient for severe **post-surgical** or **cancer pain** of the magnitude experienced by this patient.
*Mixed agonist-antagonist at opioid receptors*
- Mixed agonist-antagonists provide analgesia by acting as agonists at some opioid receptors while acting as antagonists at others (e.g., **buprenorphine**).
- While they can provide pain relief, their use in acute severe pain is often limited, and they can sometimes **precipitate withdrawal** in patients chronically using full opioid agonists.
*Central action via blockade of serotonin reuptake*
- This is the primary mechanism of action for **antidepressants** (SSRIs) and some drugs used for **neuropathic pain** (e.g., tramadol with additional opioid action).
- While some antidepressants have analgesic properties, this mechanism alone is not typically the primary one for the potent pain relief needed post-mastectomy, which usually requires an **opioid**.
GLP-1 receptor agonists US Medical PG Question 9: A 52-year-old man presents to his primary care physician complaining of a blistering rash in his inguinal region. Upon further questioning, he also endorses an unintended weight loss, diarrhea, polydipsia, and polyuria. A fingerstick glucose test shows elevated glucose even though this patient has no previous history of diabetes. After referral to an endocrinologist, the patient is found to have elevated serum glucagon and is diagnosed with glucagonoma. Which of the following is a function of glucagon?
- A. Inhibition of insulin release
- B. Increased glycolysis
- C. Increased lipolysis (Correct Answer)
- D. Decreased glycogenolysis
- E. Decreased ketone body production
GLP-1 receptor agonists Explanation: ***Increased lipolysis***
- **Glucagon** promotes the breakdown of **triglycerides** in adipose tissue into **fatty acids** and glycerol, which can then be used for energy.
- This metabolic effect contributes to **gluconeogenesis** by providing substrates, helping to raise blood glucose levels.
*Inhibition of insulin release*
- **Glucagon** generally **stimulates insulin release** in the presence of high blood glucose or certain amino acids, aiming to maintain glucose homeostasis.
- Its primary role is to counteract insulin's effects, not inhibit its secretion directly.
*Increased glycolysis*
- **Glucagon's** main function is to **increase blood glucose**, so it **inhibits glycolysis**, which is the breakdown of glucose for energy, to preserve glucose for other tissues.
- Instead, it promotes processes like **gluconeogenesis** and **glycogenolysis** to release glucose.
*Decreased glycogenolysis*
- **Glucagon** is a key hormone that **stimulates glycogenolysis**, the breakdown of stored **glycogen** in the liver, to release glucose into the bloodstream.
- This action helps to rapidly raise blood glucose levels, particularly during periods of fasting or low blood sugar.
*Decreased ketone body production*
- **Glucagon** generally **promotes ketone body production** (ketogenesis) in the liver by increasing the availability of fatty acids through lipolysis and shifting metabolism towards **fat oxidation**.
- This occurs when glucose is scarce, providing an alternative fuel source for the brain and other tissues.
GLP-1 receptor agonists US Medical PG Question 10: A 43-year-old male with a history of thyroid cancer status post total thyroidectomy presents to his primary care physician after repeated bouts of headaches. His headaches are preceded by periods of anxiety, palpitations, and sweating. The patient says he is unable to pinpoint any precipitating factors and instead says the events occur without warning. Of note, the patient's father and uncle also have a history of thyroid cancer. On exam his vitals are: T 36.8 HR 87, BP 135/93, RR 14, and O2 Sat 100% on room air. The patient's TSH is within normal limits, and he reports taking his levothyroxine as prescribed. What is the next best step in diagnosing this patient's chief complaint?
- A. 24-hour urine free cortisol
- B. Plasma aldosterone/renin ratio
- C. Abdominal CT scan with and without IV contrast
- D. Plasma fractionated metanephrines (Correct Answer)
- E. High dose dexamethasone suppression test
GLP-1 receptor agonists Explanation: ***Plasma fractionated metanephrines***
- The patient's symptoms of **anxiety, palpitations, sweating, and headaches** occurring in discrete "attacks" are classic for a **pheochromocytoma**, a tumor that secretes catecholamines.
- Given the patient's and his family's history of **thyroid cancer**, specifically likely **medullary thyroid cancer** due to the familial link, there is a high suspicion for **Multiple Endocrine Neoplasia type 2 (MEN2)**, which commonly includes pheochromocytoma. **Plasma fractionated metanephrines** are the most sensitive screening test for pheochromocytoma.
*24-hour urine free cortisol*
- This test is used to detect **Cushing's syndrome**, which involves excessive cortisol production.
- Although Cushing's can cause **hypertension**, the paroxysmal symptoms of anxiety, palpitations, and sweating are not typical of Cushing's syndrome.
*Plasma aldosterone/renin ratio*
- This ratio is used to screen for **primary hyperaldosteronism**, a cause of secondary hypertension.
- While the patient has **hypertension (135/93 mm Hg)**, his symptom complex of episodic anxiety, palpitations, and sweating is not characteristic of primary hyperaldosteronism.
*Abdominal CT scan with and without IV contrast*
- An abdominal CT scan can visualize adrenal masses, but it is typically performed *after* biochemical confirmation of a pheochromocytoma to localize the tumor.
- Performing imaging before biochemical testing risks incidentalomas or missing a biochemically active but small tumor, and it is not the most appropriate *next step* in diagnosis given the strong clinical suspicion.
*High dose dexamethasone suppression test*
- This test is specifically used to differentiate between **Cushing's disease** (pituitary ACTH excess) and other causes of Cushing's syndrome.
- The patient's symptoms are not consistent with excessive cortisol production, making this test inappropriate for his chief complaint.
More GLP-1 receptor agonists US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.