Endocrine drugs (insulin, thyroid medications)

On this page
💉 The Metabolic Command Center: Insulin & Thyroid Mastery
Insulin and thyroid hormones orchestrate two of medicine's most fundamental processes-how cells harvest energy and how fast your body burns it. You'll master the molecular mechanisms behind insulin's glucose gating and thyroid's metabolic thermostat, then translate that knowledge into clinical pattern recognition that distinguishes diabetic ketoacidosis from myxedema coma at the bedside. By integrating pharmacology with diagnostic frameworks and evidence-based protocols, you'll build the discriminating judgment needed to titrate insulin regimens and thyroid replacement with precision.
📌 Remember: INSULIN - Insulin Needs Sugar Uptake, Lipid Inhibition, Na+/K+ pump activation
The endocrine system operates through 3 fundamental mechanisms: hormone synthesis and storage, receptor-mediated signal transduction, and feedback regulation. Insulin exemplifies anabolic hormone action - promoting glucose uptake in muscle (75% of total), suppressing hepatic gluconeogenesis (90% reduction), and inhibiting lipolysis within 15-30 minutes. Thyroid hormones demonstrate nuclear receptor activation, requiring 24-72 hours for protein synthesis and metabolic effects.
⭐ Clinical Pearl: Insulin sensitivity varies 10-fold between individuals - athletic patients may require 0.3-0.5 units/kg/day while insulin-resistant patients need 1.5-2.0 units/kg/day
| Drug Class | Onset | Peak | Duration | Primary Target | Clinical Use |
|---|---|---|---|---|---|
| Rapid Insulin | 5-15 min | 1-2 hrs | 3-5 hrs | Muscle/Liver | Meal coverage |
| Long Insulin | 1-2 hrs | None | 20-24 hrs | Basal metabolism | Background control |
| Levothyroxine | 6-8 hrs | 2-4 days | 7 days | Nuclear receptors | Hypothyroidism |
| Methimazole | 1-2 hrs | 4-6 hrs | 12-24 hrs | Thyroid peroxidase | Hyperthyroidism |
| Propylthiouracil | 30-60 min | 2-4 hrs | 6-8 hrs | TPO + 5'-deiodinase | Thyroid storm |
💉 The Metabolic Command Center: Insulin & Thyroid Mastery
⚡ Insulin's Cellular Symphony: The Glucose Gateway
📌 Remember: RAPID insulin types - Regular, Aspart, Part (Lispro), Insulin glulisine, Detemir (actually long-acting)
Insulin Preparation Categories:
- Ultra-rapid: Lispro, Aspart, Glulisine
- Onset: 5-15 minutes
- Peak: 30-90 minutes
- Duration: 3-5 hours
- Clinical use: Meal coverage, correction doses
- Short-acting: Regular insulin
- Onset: 30-60 minutes
- Peak: 2-4 hours
- Duration: 6-8 hours
- Clinical use: Sliding scale protocols
- Intermediate: NPH insulin
- Onset: 1-2 hours
- Peak: 4-12 hours
- Duration: 12-18 hours
- Clinical use: Twice-daily regimens
- Long-acting: Glargine, Detemir, Degludec
- Onset: 1-2 hours
- Peak: Minimal to none
- Duration: 20-42 hours
- Clinical use: Basal insulin replacement
⭐ Clinical Pearl: Insulin-to-carbohydrate ratios typically range 1:10 to 1:20 (1 unit per 10-20g carbs), while correction factors average 1 unit per 30-50 mg/dL glucose elevation above target
💡 Master This: Insulin's dual-phase secretion - first phase (stored insulin) peaks at 1-3 minutes, second phase (newly synthesized) sustains for 2-3 hours. Type 1 diabetes loses both phases; Type 2 initially loses first phase only.
Understanding insulin kinetics enables precise glycemic control while minimizing hypoglycemic risk patterns.
⚡ Insulin's Cellular Symphony: The Glucose Gateway
🎯 Thyroid's Nuclear Command: The Metabolic Thermostat
📌 Remember: THYROID synthesis - Transport iodide, Halogenation (oxidation), Yield MIT/DIT, Recombine to T3/T4, Organification, Incorporate into thyroglobulin, Degrade and release
Thyroid Hormone Physiology:
- T4 (Thyroxine): 80% of thyroid output
- Half-life: 7 days
- Protein binding: 99.97% (TBG, albumin)
- Biological activity: Prohormone (converted to T3)
- T3 (Triiodothyronine): 20% of thyroid output
- Half-life: 1-2 days
- Protein binding: 99.7%
- Biological activity: 3-4x more potent than T4
- Reverse T3: Inactive metabolite
- Increases during illness, starvation
- Blocks T3 receptors competitively
⭐ Clinical Pearl: Free T4 represents only 0.03% of total T4 but determines biological activity. TSH changes log-linearly - a 50% decrease in free T4 causes 100-fold TSH increase
| Parameter | Normal Range | Hypothyroid | Hyperthyroid | Clinical Significance |
|---|---|---|---|---|
| TSH | 0.4-4.0 mU/L | >10 mU/L | <0.1 mU/L | Most sensitive marker |
| Free T4 | 0.8-1.8 ng/dL | <0.8 ng/dL | >1.8 ng/dL | Reflects thyroid function |
| Free T3 | 2.3-4.2 pg/mL | <2.3 pg/mL | >4.2 pg/mL | Active hormone level |
| Anti-TPO | <35 IU/mL | >100 IU/mL | Variable | Autoimmune marker |
| TRAb | <1.75 IU/L | Normal | >1.75 IU/L | Graves' disease |
Thyroid hormone regulation demonstrates the precision required for optimal metabolic homeostasis across all physiological systems.
🎯 Thyroid's Nuclear Command: The Metabolic Thermostat
🔧 Clinical Pattern Recognition: The Diagnostic Framework
Diabetes Classification Patterns:
-
Type 1 Diabetes (5-10% of cases)
- Age: Usually <30 years (can occur any age)
- Onset: Acute (weeks to months)
- Body habitus: Normal to thin
- C-peptide: <0.6 ng/mL (undetectable)
- Autoantibodies: Positive (GAD, IA-2, ZnT8)
- Ketosis: Prone (DKA risk)
- Insulin requirement: Absolute from diagnosis
-
Type 2 Diabetes (90-95% of cases)
- Age: Usually >40 years (increasing in youth)
- Onset: Gradual (months to years)
- Body habitus: Overweight/obese (80% of patients)
- C-peptide: >1.0 ng/mL (preserved initially)
- Autoantibodies: Negative
- Ketosis: Resistant (rare DKA)
- Insulin requirement: Relative (progressive)
📌 Remember: LADA (Latent Autoimmune Diabetes in Adults) - Late onset, Autoantibody positive, Diabetic, Adults who initially respond to oral agents
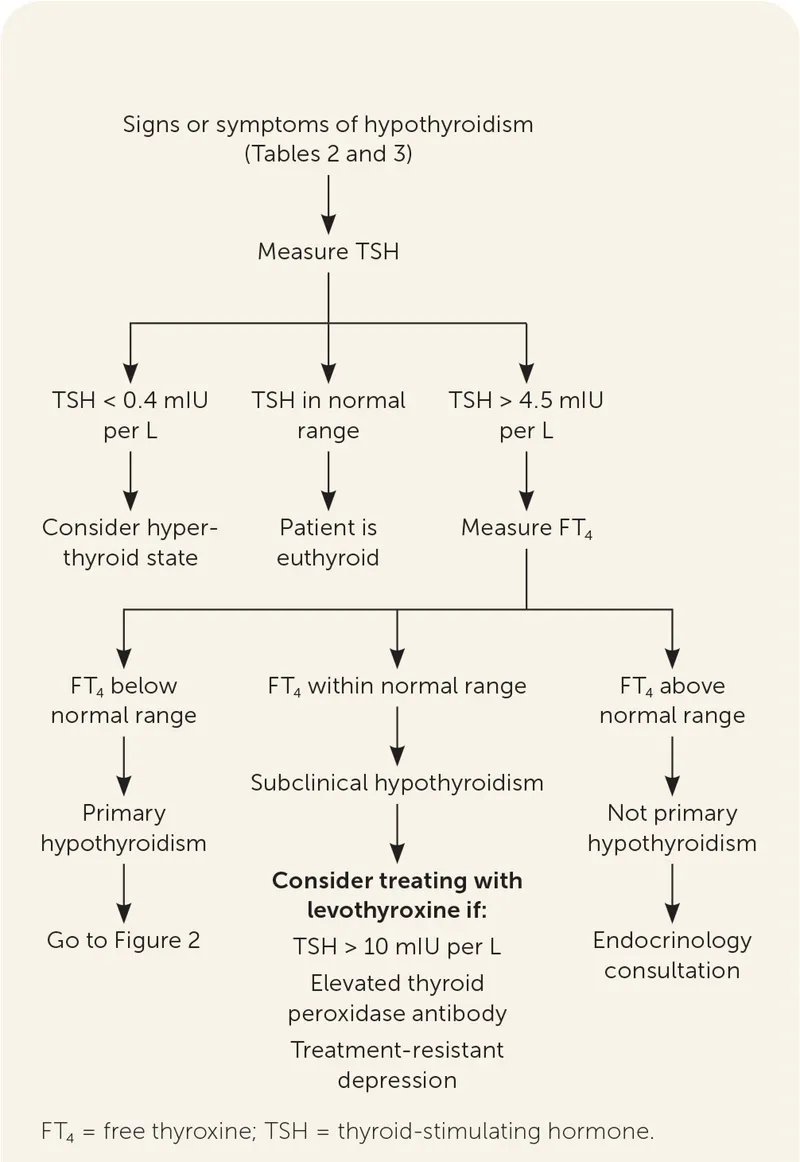
Thyroid Dysfunction Patterns:
-
Primary Hypothyroidism (95% of cases)
- TSH: Elevated (>4.0 mU/L)
- Free T4: Low (<0.8 ng/dL)
- Symptoms: Fatigue, weight gain, cold intolerance
- Causes: Hashimoto's (90%), iodine deficiency, medications
-
Secondary Hypothyroidism (5% of cases)
- TSH: Low or normal (<2.0 mU/L)
- Free T4: Low (<0.8 ng/dL)
- Symptoms: Pituitary dysfunction signs
- Causes: Pituitary adenoma, surgery, radiation
-
Subclinical Hypothyroidism
- TSH: 4.0-10.0 mU/L
- Free T4: Normal (0.8-1.8 ng/dL)
- Symptoms: Minimal or absent
- Treatment: Controversial (treat if TSH >10 or symptoms)
⭐ Clinical Pearl: Honeymoon period in Type 1 diabetes occurs in 80% of patients, lasting 3-12 months with residual beta-cell function requiring <0.5 units/kg/day insulin
💡 Master This: Dawn phenomenon (morning glucose elevation) affects 75% of diabetics due to cortisol and growth hormone surges between 4-8 AM, requiring basal insulin adjustment or dawn-specific rapid insulin
Recognition of these patterns enables rapid diagnosis and appropriate therapeutic intervention strategies.
🔧 Clinical Pattern Recognition: The Diagnostic Framework
🔍 Therapeutic Discrimination: The Treatment Matrix
Insulin Regimen Selection Matrix:
| Clinical Scenario | Regimen Type | Insulin Combination | Injection Frequency | Glycemic Control |
|---|---|---|---|---|
| Type 1, Active | Basal-Bolus | Glargine + Lispro | 4x daily | HbA1c <7% |
| Type 2, Stable | Basal-Plus | Glargine + Metformin | 1x daily | HbA1c 7-8% |
| Elderly, Frail | Conservative | NPH + Regular | 2x daily | HbA1c 8-9% |
| Hospitalized | Sliding Scale | Regular insulin | q6h PRN | 150-200 mg/dL |
| Pregnancy | Intensive | NPH + Regular | 4-6x daily | HbA1c <6% |
-
Levothyroxine (T4 replacement)
- First-line for hypothyroidism (95% of cases)
- Dose: 1.6 mcg/kg/day (healthy adults)
- Dose: 1.0 mcg/kg/day (elderly, cardiac disease)
- Monitoring: TSH every 6-8 weeks until stable
- Goal TSH: 0.4-2.5 mU/L (most patients)
-
Liothyronine (T3 replacement)
- Second-line for T4 conversion defects
- Dose: 25-75 mcg/day divided doses
- Half-life: 24 hours (requires 2-3x daily)
- Monitoring: Free T3 levels
- Risk: Cardiac arrhythmias at high doses
-
Desiccated Thyroid (T4 + T3 combination)
- Alternative for T4 intolerance
- Dose: 60-120 mg daily (1-2 grains)
- T4:T3 ratio: 4.2:1 (physiologic is 14:1)
- Monitoring: Both TSH and Free T3
📌 Remember: THYROID dosing factors - Thinner patients need more, Heart disease needs less, Younger patients need more, Renal disease affects clearance, Older patients need less, Interactions reduce absorption, Drug timing matters
⭐ Clinical Pearl: Insulin stacking occurs when rapid-acting insulin doses overlap - 3-hour duration means doses given <3 hours apart cause cumulative hypoglycemic risk
💡 Master This: Levothyroxine absorption decreases 50% with food, 30% with coffee, 75% with calcium/iron supplements. Morning fasting administration 1 hour before food optimizes bioavailability.
Therapeutic selection requires matching drug characteristics to patient-specific factors and clinical goals.
🔍 Therapeutic Discrimination: The Treatment Matrix
⚖️ Evidence-Based Treatment Algorithms: The Clinical Protocols
Diabetic Ketoacidosis (DKA) Protocol:
DKA Management Targets:
- Glucose reduction: 50-75 mg/dL/hour (avoid >100 mg/dL/hour)
- Insulin rate: 0.1 units/kg/hour IV (adjust based on glucose response)
- Fluid replacement: 1-2 L first hour, then 250-500 mL/hour
- Potassium: Maintain 4.0-5.0 mEq/L (add 20-40 mEq/L to fluids)
- Bicarbonate: Only if pH <6.9 (controversial, may worsen outcomes)
Thyroid Storm Treatment Protocol:
- Beta-blockade: Propranolol 1-2 mg IV q5min or 40-80 mg PO q6h
- Antithyroid: PTU 300-400 mg loading, then 100-200 mg q6h
- Iodine: SSKI 5 drops q6h or Lugol's 10 drops q8h (1 hour after PTU)
- Steroids: Hydrocortisone 100-300 mg q8h IV
- Supportive: Cooling, fluids, treat precipitating factors
📌 Remember: PTU preferred over methimazole in thyroid storm because it blocks peripheral T4→T3 conversion in addition to thyroid hormone synthesis
| Emergency | Recognition | Initial Treatment | Target Parameters | Timeline |
|---|---|---|---|---|
| DKA | Glucose >250, pH <7.3, Ketones + | Insulin 0.1 U/kg/hr IV | pH >7.3, HCO3 >15 | 12-24 hours |
| HHS | Glucose >600, Osmolality >320 | Fluids first, then insulin | Glucose <300 | 24-48 hours |
| Thyroid Storm | Fever, tachycardia, altered mental status | PTU + propranolol + steroids | HR <100, temp normal | 24-72 hours |
| Severe Hypoglycemia | Glucose <40, altered consciousness | D50W 25g IV or glucagon 1mg | Glucose >70 | 15-30 minutes |
💡 Master This: Hypoglycemia treatment follows 15-15 rule - 15g fast-acting carbs, recheck in 15 minutes. Severe hypoglycemia requires D50W 25g IV (50mL of 50% dextrose) or glucagon 1mg IM/SC.
Evidence-based protocols ensure optimal outcomes while minimizing treatment-related complications.
⚖️ Evidence-Based Treatment Algorithms: The Clinical Protocols
🔗 Advanced Integration: The Endocrine Network
Multi-Hormonal Integration Patterns:
-
Insulin-Cortisol Axis
- Cortisol increases insulin resistance by 30-50%
- Dawn phenomenon: Cortisol surge at 4-8 AM raises glucose 20-40 mg/dL
- Stress hyperglycemia: Cortisol elevation can increase insulin needs 2-3 fold
- Clinical correlation: Cushing's syndrome causes diabetes in 80% of patients
-
Thyroid-Insulin Interactions
- Hyperthyroidism increases insulin clearance by 40% (higher insulin needs)
- Hypothyroidism decreases glucose absorption and insulin sensitivity
- T3 enhances GLUT4 expression and glucose uptake
- Clinical correlation: Thyroid dysfunction affects glycemic control in 60% of diabetics
Advanced Therapeutic Considerations:
-
Sick Day Management
- Illness increases insulin resistance by 50-100%
- Stress hormones (cortisol, epinephrine) oppose insulin action
- Dehydration concentrates glucose and reduces insulin effectiveness
- Protocol: Never stop insulin, increase monitoring frequency, liberal fluid intake
-
Drug Interactions
- Steroids: Increase insulin needs 2-4 fold within 24-48 hours
- Beta-blockers: Mask hypoglycemic symptoms and delay recovery
- Thiazides: Increase glucose 10-15 mg/dL through insulin resistance
- Levothyroxine: Warfarin potentiation (30% dose reduction often needed)
📌 Remember: STRESS effects on glucose - Steroids raise glucose, Thiazides raise glucose, Respiratory infections raise glucose, Epinephrine raises glucose, Surgery raises glucose, Sickness raises glucose
Cutting-Edge Therapeutic Insights:
-
Continuous Glucose Monitoring (CGM)
- Real-time glucose data every 1-5 minutes
- Time-in-range goal: >70% between 70-180 mg/dL
- Glycemic variability predicts complications independent of HbA1c
- Clinical benefit: 0.3-0.5% HbA1c reduction with reduced hypoglycemia
-
Automated Insulin Delivery (AID)
- Hybrid closed-loop systems adjust basal insulin every 5 minutes
- Time-in-range improvement: 70% to 85% in clinical trials
- Overnight glucose control: 90% time-in-range achievable
- Limitation: Still requires meal bolusing and carb counting
⭐ Clinical Pearl: Thyroid hormone replacement affects cardiac contractility within 24-48 hours but metabolic effects require 2-6 weeks. Cardiac patients need gradual titration starting at 25-50 mcg daily.
💡 Master This: Reverse T3 elevation during critical illness represents adaptive response - low T3 syndrome should NOT be treated with thyroid hormone replacement as it may worsen outcomes.
Understanding endocrine integration enables sophisticated management of complex metabolic disorders.
🔗 Advanced Integration: The Endocrine Network
🎯 Clinical Mastery Arsenal: The Practitioner's Toolkit
Essential Clinical Thresholds:
| Parameter | Target Range | Action Required | Clinical Significance |
|---|---|---|---|
| HbA1c | <7.0% (most patients) | >8.0%: Intensify therapy | 1% reduction = 21% microvascular risk |
| Fasting Glucose | 80-130 mg/dL | >180 mg/dL: Adjust basal insulin | Reflects overnight control |
| 2-hr Postprandial | <180 mg/dL | >250 mg/dL: Adjust meal insulin | Predicts cardiovascular risk |
| TSH | 0.4-2.5 mU/L | >10 mU/L: Start levothyroxine | Most sensitive thyroid marker |
| Free T4 | 0.8-1.8 ng/dL | <0.8 ng/dL: Increase dose | Reflects thyroid hormone status |
-
Insulin Dosing Calculations
- Total Daily Dose: 0.5-1.0 units/kg (Type 1), 0.5-1.5 units/kg (Type 2)
- Basal:Bolus Ratio: 50:50 (adjust based on patterns)
- Carb Ratio: 500 rule (500 ÷ TDD = grams carb per unit)
- Correction Factor: 1800 rule (1800 ÷ TDD = mg/dL drop per unit)
-
Thyroid Dosing Principles
- Initial Dose: 1.6 mcg/kg/day (healthy adults)
- Elderly/Cardiac: 25-50 mcg/day, increase by 12.5-25 mcg every 6-8 weeks
- Dose Adjustments: 12.5-25 mcg increments based on TSH response
- Monitoring: TSH every 6-8 weeks until stable, then annually
📌 Remember: MONITORING essentials - Monthly glucose logs, Optimal HbA1c <7%, Nightly glucose checks, Insulin adjustment protocols, Thyroid function annually, Ocular exams yearly, Renal function monitoring, Immunizations current, Neuropathy screening, Glucagon emergency kit
Emergency Recognition Patterns:
-
Severe Hypoglycemia: Glucose <54 mg/dL or cognitive impairment
- Treatment: 15-20g glucose PO or D50W 25g IV or Glucagon 1mg IM
- Recovery time: 15-20 minutes with appropriate treatment
- Follow-up: Complex carbohydrate to prevent rebound
-
Hyperglycemic Crisis: DKA (glucose >250, pH <7.3) or HHS (glucose >600, osmolality >320)
- Initial: IV fluids, insulin infusion, electrolyte monitoring
- Monitoring: Hourly glucose, q4h electrolytes, continuous cardiac monitoring
- Resolution: pH >7.3, HCO3 >15, anion gap <12
⭐ Clinical Pearl: Insulin pump therapy reduces severe hypoglycemia by 80% and improves HbA1c by 0.2-0.5% compared to multiple daily injections in motivated patients
💡 Master This: Levothyroxine bioequivalence varies ±12.5% between manufacturers. Brand consistency or generic consistency prevents TSH fluctuations requiring dose adjustments.
Advanced Monitoring Strategies:
-
Continuous Glucose Monitoring Metrics
- Time-in-Range (70-180 mg/dL): >70% goal
- Time-below-Range (<70 mg/dL): <4% goal
- Time-above-Range (>180 mg/dL): <25% goal
- Coefficient of Variation: <36% indicates stable glucose
-
Thyroid Function Optimization
- Free T4: Upper half of normal range for symptom resolution
- Free T3: Monitor if symptoms persist with normal TSH/T4
- Reverse T3: Consider in illness or persistent symptoms
- Antibodies: Annual monitoring in autoimmune thyroid disease
This comprehensive toolkit enables precise, evidence-based endocrine management across all clinical scenarios.
🎯 Clinical Mastery Arsenal: The Practitioner's Toolkit
Practice Questions: Endocrine drugs (insulin, thyroid medications)
Test your understanding with these related questions
A 22-year-old woman with type 1 diabetes mellitus and mild asthma comes to the physician for a follow-up examination. She has had several episodes of sweating, dizziness, and nausea in the past 2 months that occur during the day and always resolve after she drinks orange juice. She is compliant with her diet and insulin regimen. The physician recommends lowering her insulin dose in certain situations. This recommendation is most important in which of the following situations?









