Serotonin syndrome US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Serotonin syndrome. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Serotonin syndrome US Medical PG Question 1: A 65-year-old man presents to the emergency department with confusion and a change in his behavior. The patient was in his usual state of health 3 days ago. He became more confused and agitated this morning thus prompting his presentation. The patient has a past medical history of depression, hypertension, diabetes, and Parkinson disease and is currently taking fluoxetine, lisinopril, insulin, metformin, and selegiline (recently added to his medication regimen for worsening Parkinson symptoms). He also takes oxycodone and clonazepam for pain and anxiety; however, he ran out of these medications last night. His temperature is 101°F (38.3°C), blood pressure is 111/78 mmHg, pulse is 117/min, respirations are 22/min, and oxygen saturation is 99% on room air. Physical exam is notable for an irritable, sweaty, and confused elderly man. Neurological exam reveals hyperreflexia of the lower extremities and clonus. Which of the following is the most likely etiology of this patient’s symptoms?
- A. Electrolyte abnormality
- B. Medication complication (Correct Answer)
- C. Viral infection
- D. Substance withdrawal
- E. Bacterial infection
Serotonin syndrome Explanation: ***Medication complication***
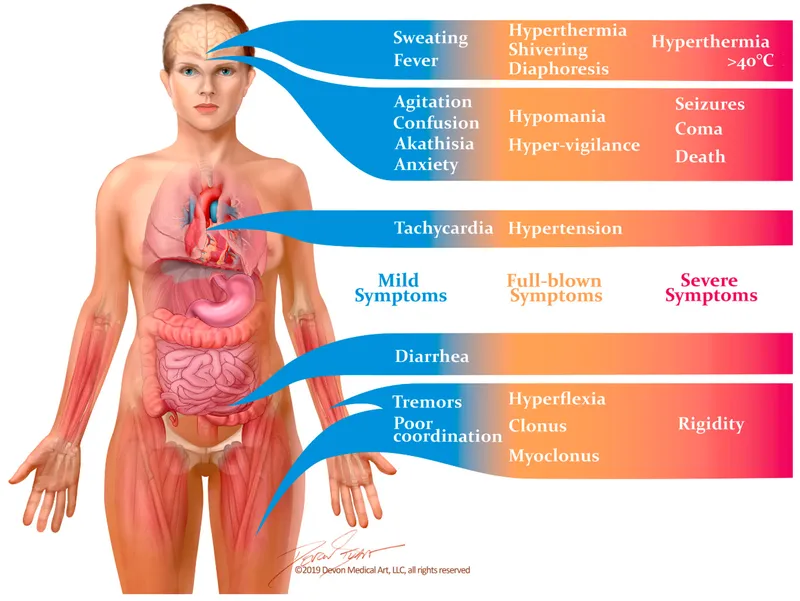
- The combination of **fluoxetine** and **selegiline** can precipitate **serotonin syndrome**, characterized by altered mental status, autonomic dysfunction (fever, tachycardia, sweating), and neuromuscular hyperactivity (hyperreflexia, clonus).
- Both medications increase serotonin levels in the central nervous system; fluoxetine is a selective serotonin reuptake inhibitor (SSRI), and selegiline is a monoamine oxidase type B (MAO-B) inhibitor that, at higher doses, can also inhibit MAO-A, leading to increased serotonin.
*Electrolyte abnormality*
- While electrolyte imbalances can cause confusion and altered mental status, they typically do not present with the specific constellation of fever, tachycardia, sweating, hyperreflexia, and clonus seen here.
- There is no specific information in the clinical presentation to suggest an electrolyte imbalance is the primary cause over a medication-induced syndrome.
*Viral infection*
- Viral infections can cause fever and confusion, but the rapid onset and the specific neurological findings of marked **hyperreflexia** and **clonus** are more indicative of a central nervous system (CNS) disturbance like serotonin syndrome rather than a typical viral encephalopathy or infection.
- The absence of other common viral symptoms (e.g., cough, sore throat, GI symptoms) makes it less likely.
*Substance withdrawal*
- Withdrawal from **oxycodone** (opioid) or **clonazepam** (benzodiazepine) could cause agitation and autonomic symptoms. However, opioid withdrawal typically causes diarrhea, nausea, vomiting, and muscle aches, not hyperreflexia or fever, and benzodiazepine withdrawal usually presents with seizures, anxiety, and tremors, but the hyperreflexia and clonus point more strongly to serotonin syndrome, especially given the medication history.
- The patient ran out of these medications the previous night, which could contribute to some symptoms but doesn't fully explain the specific neurological signs in the context of the recent medication change.
*Bacterial infection*
- A bacterial infection could cause fever and confusion, but typically less specific neurological signs like **hyperreflexia** and **clonus** are not characteristic.
- While a CNS infection like meningitis could present with altered mental status and fever, it would usually involve neck stiffness and specific CSF findings, which are not mentioned.
Serotonin syndrome US Medical PG Question 2: A 49-year-old woman presents to her primary care physician with fatigue. She reports that she has recently been sleeping more than usual and says her “arms and legs feel like lead” for most of the day. She has gained 10 pounds over the past 3 months which she attributes to eating out at restaurants frequently, particularly French cuisine. Her past medical history is notable for social anxiety disorder. She took paroxetine and escitalopram in the past but had severe nausea and headache while taking both. She has a 10 pack-year smoking history and has several glasses of wine per day. Her temperature is 98.6°F (37°C), blood pressure is 130/65 mmHg, pulse is 78/min, and respirations are 16/min. Physical examination reveals an obese woman with a dysphoric affect. She states that her mood is sad but she does experience moments of happiness when she is with her children. The physician starts the patient on a medication to help with her symptoms. Three weeks after the initiation of the medication, the patient presents to the emergency room with a severe headache and agitation. Her temperature is 102.1°F (38.9°C), blood pressure is 180/115 mmHg, pulse is 115/min, and respirations are 24/min. Which of the following is the mechanism of action of the medication that is most likely responsible for this patient’s symptoms?
- A. Inhibition of serotonin and norepinephrine reuptake
- B. Inhibition of the adrenergic alpha-2 receptor and serotonin-2 and -3 receptors
- C. Inhibition of serotonin reuptake
- D. Partial agonism of serotonin-1A receptor
- E. Inhibition of amine degradation (Correct Answer)
Serotonin syndrome Explanation: **Inhibition of amine degradation**
- This mechanism of action describes **monoamine oxidase inhibitors (MAOIs)**. Given the patient's symptoms of **hypertensive crisis** (headache, agitation, hypertension, tachycardia, fever) after starting a new medication and her history of **eating French cuisine** (which could include tyramine-rich foods like aged cheeses and wines), an MAOI is the most likely culprit.
- MAOIs prevent the breakdown of **monoamine neurotransmitters** (serotonin, norepinephrine, dopamine, tyramine), leading to their accumulation. In the presence of **tyramine-rich foods**, this can precipitate a **hypertensive crisis** due to excessive norepinephrine release.
*Inhibition of serotonin and norepinephrine reuptake*
- This describes **SNRIs (serotonin-norepinephrine reuptake inhibitors)** or **TCAs (tricyclic antidepressants)**. While these can cause side effects, a sudden and severe **hypertensive crisis** as described, especially without a clear dietary trigger interaction, is less characteristic than with MAOIs.
- The patient's prior negative experiences with paroxetine and escitalopram (SSRIs) might make a physician choose a different class, but the dramatic symptoms point away from typical SNRI/TCA side effects for this presentation.
*Inhibition of the adrenergic alpha-2 receptor and serotonin-2 and -3 receptors*
- This mechanism is characteristic of **mirtazapine**. While mirtazapine can cause sedation and weight gain (presenting symptoms), it does not typically lead to a **hypertensive crisis** of this severity three weeks after initiation, nor does it have severe food interactions like MAOIs.
- Mirtazapine's primary side effects often include sedation, increased appetite, and weight gain, but not the acute constellation observed here.
*Inhibition of serotonin reuptake*
- This describes **SSRIs (selective serotonin reuptake inhibitors)**. The patient had severe nausea and headache with paroxetine and escitalopram, which are SSRIs. While SSRIs can contribute to **serotonin syndrome** (which shares some features like agitation and hyperthermia), the profound **hypertension** and context of food interaction strongly favor an MAOI-induced hypertensive crisis.
- SSRIs are less likely to cause such a severe **hypertensive crisis** acutely, and the patient's history suggests a physician would likely avoid this class due to past adverse reactions.
*Partial agonism of serotonin-1A receptor*
- This is the mechanism of action for **buspirone**, an anxiolytic. Buspirone is generally well-tolerated and does not cause the severe side effects seen in this patient, particularly **hypertensive crisis** or food interactions.
- Buspirone is often used for generalized anxiety disorder, and while the patient has social anxiety, the described adverse event does not align with buspirone's known side effect profile.
Serotonin syndrome US Medical PG Question 3: A 31-year-old man is brought to the emergency department because of fever and increasing confusion for the past day. He has bipolar disorder with psychotic features and hypothyroidism. Current medications are lithium, haloperidol, and levothyroxine. He drinks one beer with dinner every night. His speech is confused and he is oriented to person only. His temperature is 40°C (104°F), pulse is 124/min, and blood pressure is 160/110 mm Hg. He appears acutely ill. Examination shows diaphoresis and muscle rigidity. Deep tendon reflexes are 1+ bilaterally. There is minor rigidity of the neck with full range of motion. His lungs are clear to auscultation. The abdomen is soft and nontender. His leukocyte count is 15,100/mm3 and serum creatine kinase activity is 1100 U/L. Which of the following is the most likely diagnosis?
- A. Delirium tremens
- B. Neuroleptic malignant syndrome (Correct Answer)
- C. Bacterial meningitis
- D. Herpes simplex encephalitis
- E. Lithium toxicity
Serotonin syndrome Explanation: ***Neuroleptic malignant syndrome***
- The patient presents with **fever (40°C)**, **muscle rigidity**, **altered mental status (confusion)**, **autonomic instability (tachycardia, hypertension, diaphoresis)**, and **elevated creatine kinase**, all classic features of **Neuroleptic Malignant Syndrome (NMS)**.
- The use of **haloperidol**, a high-potency antipsychotic, is a significant risk factor for NMS.
*Delirium tremens*
- While delirium tremens can cause altered mental status, autonomic instability, and fever, it is typically preceded by a history of **heavy chronic alcohol intake** followed by acute withdrawal, which is not indicated by "one beer with dinner every night."
- **Muscle rigidity** and **marked elevation of creatine kinase** are not typical features of delirium tremens.
*Bacterial meningitis*
- Although bacterial meningitis presents with fever and altered mental status, it would typically involve **nuchal rigidity** that limits range of motion, which is not fully present here, and **CSF findings** (e.g., pleocytosis, low glucose) would be diagnostic.
- **Profound muscle rigidity** and **markedly elevated creatine kinase** are not characteristic features of bacterial meningitis.
*Herpes simplex encephalitis*
- This condition presents with fever, altered mental status, and often **focal neurological deficits** or **seizures**, which are not described.
- Diagnosis relies on **characteristic MRI findings** and **CSF PCR for HSV DNA**, and it would not typically cause diffuse **muscle rigidity** or **elevated creatine kinase**.
*Lithium toxicity*
- **Lithium toxicity** typically presents with neurological symptoms like **tremors**, **ataxia**, **nystagmus**, and altered mental status, but it is less commonly associated with **severe muscle rigidity**, **very high fever (40°C)**, or **markedly elevated creatine kinase** unless complicated by severe dehydration or NMS-like features.
- A **high lithium level** would be expected, which is not mentioned as present.
Serotonin syndrome US Medical PG Question 4: A 25-year-old woman presents to her college campus clinic with the complaint of being unable to get up for her morning classes. She says that, because of this, her grades are being affected. For the past 6 weeks, she says she has been feeling depressed because her boyfriend dumped her. She finds herself very sleepy, sleeping in most mornings, eating more snacks and fast foods, and feeling drained of energy. She is comforted by her friend’s efforts to cheer her up but still feels guarded around any other boy that shows interest in her. The patient says she had similar symptoms 7 years ago for which she was prescribed several selective serotonin reuptake inhibitors (SSRIs) and a tricyclic antidepressant (TCA). However, none of the medications provided any long-term relief. She has prescribed a trial of Phenelzine to treat her symptoms. Past medical history is significant for a long-standing seizure disorder well managed with phenytoin. Which of the following statements would most likely be relevant to this patient’s new medication?
- A. “This medication is known to cause anorgasmia during treatment.”
- B. “You will have a risk for cardiotoxicity from this medication.”
- C. “A common side effect of this medication is sedation.”
- D. “While taking this medication, you should avoid drinking red wine.” (Correct Answer)
- E. “While on this medication, you may have a decreased seizure threshold.”
Serotonin syndrome Explanation: ***"While taking this medication, you should avoid drinking red wine."***
- Phenelzine is a **monoamine oxidase inhibitor (MAOI)**. MAOIs inhibit the breakdown of **tyramine**, an amine found in fermented foods like red wine, aged cheeses, cured meats, and pickled foods.
- Consuming tyramine-rich foods with an MAOI can lead to a **hypertensive crisis**, characterized by a sudden, severe increase in blood pressure which can cause headaches, palpitations, and potentially stroke.
- This dietary counseling is **essential and immediately actionable** patient education when starting an MAOI.
*"This medication is known to cause anorgasmia during treatment."*
- While sexual dysfunction can occur with many antidepressants, **anorgasmia** is much more common and severe with **SSRIs (Selective Serotonin Reuptake Inhibitors)** than with MAOIs.
- MAOIs like phenelzine have a different mechanism of action and generally have a lower incidence of sexual side effects compared to SSRIs.
*"You will have a risk for cardiotoxicity from this medication."*
- **Cardiotoxicity** is a significant concern with **tricyclic antidepressants (TCAs)**, especially in overdose, due to their effects on cardiac sodium channels and potential for arrhythmias.
- While MAOIs can cause **orthostatic hypotension**, direct cardiotoxicity is not a primary concern with phenelzine.
*"A common side effect of this medication is sedation."*
- Phenelzine is generally considered **activating** rather than sedating, and can sometimes lead to insomnia or agitation.
- The patient's current hypersomnia is a symptom of her **atypical depression**, not a predicted side effect of phenelzine. In fact, phenelzine may help improve this symptom.
*"While on this medication, you may have a decreased seizure threshold."*
- This statement is actually **medically accurate** - MAOIs including phenelzine can lower (decrease) the seizure threshold, meaning they increase seizure risk.
- This is relevant given the patient's seizure disorder managed with phenytoin and warrants monitoring.
- However, the **dietary tyramine restriction** is the more critical and immediately actionable counseling point when initiating MAOI therapy, as hypertensive crisis can occur with the very first exposure to tyramine-rich foods.
Serotonin syndrome US Medical PG Question 5: A 22-year-old woman is brought to the emergency department after being struck by a car while crossing the street. She has major depressive disorder with psychosis. Current medications include sertraline and haloperidol. Vital signs are within normal limits. X-ray of the lower extremity shows a mid-shaft femur fracture. The patient is taken to the operating room for surgical repair of the fracture. As the surgeon begins the internal fixation, the patient shows muscle rigidity and profuse diaphoresis. Her temperature is 39°C (102.2°F), pulse is 130/min, respirations are 24/min, and blood pressure is 146/70 mm Hg. The pupils are equal and reactive to light. The end tidal CO2 is 85 mm Hg. Which of the following is the most appropriate treatment for this patient's condition?
- A. Fat embolectomy
- B. Bromocriptine therapy
- C. Propranolol therapy
- D. Dantrolene therapy (Correct Answer)
- E. Cyproheptadine therapy
Serotonin syndrome Explanation: ***Dantrolene therapy***
- The patient's presentation with **muscle rigidity**, **hyperthermia** (39°C), **tachycardia**, **tachypnea**, **hypertension**, and **markedly elevated end-tidal CO2 (85 mm Hg)** developing acutely **during surgery** is diagnostic of **malignant hyperthermia (MH)**.
- MH is a life-threatening hypermetabolic crisis triggered by **volatile anesthetic agents** (e.g., sevoflurane, isoflurane) or **succinylcholine** in genetically susceptible individuals with mutations in the ryanodine receptor (RYR1).
- **Dantrolene** is the specific antidote for MH, working by inhibiting calcium release from the sarcoplasmic reticulum, thereby reducing muscle contractility and heat production.
- The **extremely elevated end-tidal CO2** reflects the hypermetabolic state and is a key diagnostic feature distinguishing MH from other conditions.
*Fat embolectomy*
- **Fat embolism syndrome** can occur 24-72 hours after long bone fractures and presents with **respiratory insufficiency**, **neurologic dysfunction** (confusion, altered mental status), and a **petechial rash** (classic triad).
- While the patient has a femur fracture, the **acute intraoperative onset**, **muscle rigidity**, and **markedly elevated end-tidal CO2** are not consistent with fat embolism syndrome.
*Bromocriptine therapy*
- **Bromocriptine**, a dopamine agonist, is used in the treatment of **neuroleptic malignant syndrome (NMS)**, which shares features with MH (rigidity, hyperthermia, autonomic instability).
- However, NMS typically develops over **days to weeks** after antipsychotic exposure or dose changes, not acutely during surgery.
- The **intraoperative timing** and **extremely elevated end-tidal CO2** point to malignant hyperthermia triggered by anesthetic agents, not NMS.
*Propranolol therapy*
- **Propranolol**, a non-selective beta-blocker, may help manage **tachycardia** and **hypertension** symptomatically.
- However, it does not address the underlying pathophysiology of MH (**uncontrolled calcium release** and **hypermetabolic crisis**) and is not a primary treatment.
- Dantrolene is the specific and life-saving therapy for MH.
*Cyproheptadine therapy*
- **Cyproheptadine**, a serotonin antagonist, is the treatment for **serotonin syndrome**, which can present with hyperthermia, rigidity, and autonomic instability.
- However, serotonin syndrome typically features **hyperreflexia** and **clonus** rather than the **lead-pipe rigidity** seen here, and develops after serotonergic drug exposure or interactions.
- The **intraoperative timing**, **muscle rigidity**, and **markedly elevated end-tidal CO2** are pathognomonic for **malignant hyperthermia**, not serotonin syndrome.
Serotonin syndrome US Medical PG Question 6: A 31-year-old woman is brought to the emergency room after an apparent suicide attempt. She is unable to provide a history, but her husband reports that he found her at home severely confused and agitated. She reportedly mentioned swallowing several of her pills but was unable to provide additional details. Her husband reports that she has a history of Crohn disease, major depressive disorder, social anxiety disorder, and prior heroin and alcohol abuse. She has not taken heroin or alcohol for 5 years and attends Alcoholics Anonymous and Narcotics Anonymous regularly. She takes multiple medications but he is unable to recount which medications she takes and they are not in the electronic medical record. Her temperature is 103.9°F (39.9°C), blood pressure is 160/95 mmHg, pulse is 125/min, and respirations are 28/min. On exam, she appears agitated, diaphoretic, and is responding to internal stimuli. She has clonus in her bilateral feet. Pupils are 3 mm and reactive to light. Patellar and Achilles reflexes are 3+ bilaterally. She is given alprazolam for her agitation but she remains severely agitated and confused. Which of the following medications should be given to this patient?
- A. Naloxone
- B. Ammonium chloride
- C. N-acetylcysteine
- D. Flumazenil
- E. Cyproheptadine (Correct Answer)
Serotonin syndrome Explanation: ***Cyproheptadine***
- The patient's presentation with **agitation**, **confusion**, **diaphoresis**, **hyperthermia** (103.9°F), **tachycardia**, **hypertension**, **clonus**, and **hyperreflexia** is highly suggestive of **serotonin syndrome**.
- **Cyproheptadine**, a **serotonin antagonist**, is the appropriate treatment for serotonin syndrome, especially when benzodiazepines like alprazolam have failed to control symptoms.
*Naloxone*
- **Naloxone** is an **opioid antagonist** used to reverse opioid overdose.
- While the patient has a history of heroin abuse, her vital signs and neurological examination (e.g., hyperreflexia, clonus) are inconsistent with opioid overdose, which typically presents with **respiratory depression** and **miosis**.
*Ammonium chloride*
- **Ammonium chloride** is an **acidifying agent** used in some poisonings to promote renal excretion of basic drugs.
- It is not indicated for the constellation of symptoms presented and can be dangerous if the specific toxin is unknown or if the patient has an acid-base disturbance.
*N-acetylcysteine*
- **N-acetylcysteine (NAC)** is the antidote for **acetaminophen overdose**.
- There is no clinical evidence in the patient's presentation to suggest acetaminophen toxicity.
*Flumazenil*
- **Flumazenil** is a **benzodiazepine receptor antagonist** used to reverse the effects of benzodiazepine overdose.
- While the patient was given alprazolam, her severe agitation and neurological findings (clonus, hyperreflexia) would not be indicative of benzodiazepine overdose; rather, benzodiazepines are used to *treat* the agitation seen in stimulant toxicity or serotonin syndrome.
Serotonin syndrome US Medical PG Question 7: A 28-year-old man is brought to the emergency department after he was found half dressed and incoherent in the middle of the road. In the emergency department he states that he has not slept for 36 hours and that he has incredible ideas that will make him a billionaire within a few months. He also states that secret agents from Russia are pursuing him and that he heard one of them speaking through the hospital intercom. His past medical history is significant only for a broken arm at age 13. On presentation, his temperature is 102.2°F (39°C), blood pressure is 139/88 mmHg, pulse is 112/min, and respirations are 17/min. Physical exam reveals pupillary dilation and psychomotor agitation. Which of the following mechanisms is most likely responsible for this patient's symptoms?
- A. N-methyl-D-aspartate receptor antagonist
- B. Gamma-aminobutyric acid receptor agonist
- C. Increased biogenic amine release (Correct Answer)
- D. 5-HT receptor agonist
- E. Opioid receptor agonist
Serotonin syndrome Explanation: ***Increased biogenic amine release***
- The patient exhibits a classic constellation of symptoms consistent with **stimulant intoxication**, including **psychomotor agitation**, **pupillary dilation**, **tachycardia**, **hyperthermia**, **insomnia**, **grandiosity**, and **paranoia**.
- Stimulants like **amphetamines** and **cocaine** primarily exert their effects by increasing the release and inhibiting the reuptake of **biogenic amines** (dopamine, norepinephrine, serotonin) in the brain, leading to an exaggerated sympathetic response and altered mental status.
*N-methyl-D-aspartate receptor antagonist*
- **NMDA receptor antagonists** (e.g., phencyclidine - PCP, ketamine) are associated with dissociative symptoms, nystagmus, and sometimes aggression, but generally do not present with the prominent **hyperthermia** and grandiosity seen here.
- While they can cause psychotic symptoms, the specific combination of signs points more strongly to **stimulant intoxication**.
*Gamma-aminobutyric acid receptor agonist*
- **GABA receptor agonists** (e.g., benzodiazepines, barbiturates) cause **CNS depression**, sedation, respiratory depression, and ataxia.
- These effects are contrary to the patient's presentation of **agitation**, **increased heart rate**, and **hyperthermia**.
*5-HT receptor agonist*
- While drugs like **LSD** and **MDMA** (ecstasy) act as 5-HT receptor agonists and can cause hallucinations and altered perception, the prominent **paranoia**, **grandiosity**, and **significant hyperthermia** in this scenario are more characteristic of stimulant toxicity, which involves a broader increase in biogenic amine release beyond just serotonin.
- MDMA, in particular, can cause hyperthermia, but the full clinical picture is more suggestive of traditional stimulants.
*Opioid receptor agonist*
- **Opioid receptor agonists** (e.g., heroin, morphine) typically cause **CNS depression**, **miosis** (pinpoint pupils), respiratory depression, and sedation.
- These effects are the **opposite** of the patient's symptoms of pupillary dilation, agitation, and hyperthermia.
Serotonin syndrome US Medical PG Question 8: A 50-year-old woman presents with acute onset fever and chills for the past hour. She mentions earlier in the day she felt blue, so she took some St. John’s wort because she was told by a friend that it helps with depression. Past medical history is significant for hypertension, diabetes mellitus, and depression managed medically with captopril, metformin, and fluoxetine. She has no history of allergies. Her pulse is 130/min, the respiratory rate is 18/min, the blood pressure is 176/92 mm Hg, and the temperature is 38.5°C (101.3°F). On physical examination, the patient is profusely diaphoretic and extremely irritable when asked questions. Oriented x 3. The abdomen is soft and nontender with no hepatosplenomegaly. Increased bowel sounds are heard in the abdomen. Deep tendon reflexes are 3+ bilaterally and clonus is elicited. The sensation is decreased in the feet bilaterally. Mydriasis is present. Fingerstick glucose is 140 mg/dL. An ECG shows sinus tachycardia but is otherwise normal. Which of the following is the most likely cause of this patient’s condition?
- A. Sepsis
- B. Anaphylactic reaction
- C. Diabetic ketoacidosis
- D. Neuroleptic malignant syndrome
- E. Serotonin syndrome (Correct Answer)
Serotonin syndrome Explanation: ***Serotonin syndrome***
- The patient's presentation with **fever, diaphoresis, hypertension, tachycardia, hyperreflexia, clonus, mydriasis**, and **agitation** after combining an **SSRI (fluoxetine)** with **St. John's wort** (a serotonin-enhancing herbal supplement) is highly characteristic of serotonin syndrome.
- This condition results from excessive serotonergic activity in the central and peripheral nervous system.
*Sepsis*
- While **fever, chills, and tachycardia** can be indicators of sepsis, the presence of specific neurological and neuromuscular signs like **hyperreflexia, clonus, and mydriasis** points away from it.
- The patient's **irritable state and normal mental orientation** is less typical for severe sepsis, which often involves altered mental status.
*Anaphylactic reaction*
- **Anaphylaxis** presents with rapid onset of symptoms such as **urticaria, angioedema, bronchospasm, and hypotension**, which are not observed in this patient.
- There is no history of allergen exposure, and the prominent neurological symptoms are not typical of anaphylaxis.
*Diabetic ketoacidosis*
- **DKA** is characterized by **hyperglycemia, metabolic acidosis, and ketonemia**, often presenting with Kussmaul respirations and fruity breath odor.
- The patient's **fingerstick glucose (140 mg/dL)** is not significantly elevated, and there is no mention of deep, rapid breathing or other DKA-specific symptoms.
*Neuroleptic malignant syndrome*
- **NMS** is typically associated with exposure to **dopamine antagonists (antipsychotics)** and is characterized by **severe muscle rigidity, hyperthermia, altered mental status, and autonomic instability.**
- While some symptoms overlap, this patient's history of St. John's wort and fluoxetine points to increased serotonin, and the specific neuromuscular findings like clonus are more indicative of serotonin syndrome.
Serotonin syndrome US Medical PG Question 9: A patient on SSRI sertraline was also prescribed amitriptyline and subsequently developed serotonin toxicity. What is the likely treatment for serotonin toxicity?
- A. Flumazenil
- B. Cyproheptadine (Correct Answer)
- C. L-Carnitine
- D. Leucovorin
- E. Naloxone
Serotonin syndrome Explanation: ***Cyproheptadine***
- **Cyproheptadine** is a serotonin antagonist that can help reverse the effects of excessive serotonin in the central nervous system.
- It works by blocking **serotonin 5-HT2A receptors**, which are implicated in the pathophysiology of serotonin toxicity.
*Flumazenil*
- **Flumazenil** is a benzodiazepine receptor antagonist used to reverse the effects of benzodiazepine overdose.
- It has no role in the treatment of **serotonin toxicity**, as it does not affect serotonin pathways.
*L-Carnitine*
- **L-Carnitine** is a mitochondrial co-factor used in fatty acid metabolism, sometimes supplemented for certain metabolic disorders or muscle pain.
- It does not have any direct action on **serotonin receptors** or the serotonin system, making it ineffective for serotonin toxicity.
*Leucovorin*
- **Leucovorin** (folinic acid) is used to counteract the effects of methotrexate toxicity or to enhance the effects of fluorouracil in chemotherapy.
- It is not involved in modulating **neurotransmitter levels** or reversing the symptoms of serotonin toxicity.
*Naloxone*
- **Naloxone** is an opioid receptor antagonist used to reverse opioid overdose.
- It has no effect on **serotonin receptors** or serotonergic pathways, making it ineffective for treating serotonin toxicity.
Serotonin syndrome US Medical PG Question 10: A 58-year-old female presents to her primary care physician with a 1-month history of facial and chest flushing, as well as intermittent diarrhea and occasional difficulty breathing. On physical exam, a new-onset systolic ejection murmur is auscultated and is loudest at the left second intercostal space. Subsequent echocardiography reveals leaflet thickening secondary to fibrous plaque deposition on both the pulmonic and tricuspid valves. Which of the following laboratory abnormalities would most likely be found in this patient?
- A. Elevated urinary 5-hydroxyindoleacetic acid (Correct Answer)
- B. Elevated serum bicarbonate
- C. Elevated serum potassium
- D. Decreased serum chromogranin A
- E. Elevated urinary vanillylmandelic acid
Serotonin syndrome Explanation: **Elevated urinary 5-hydroxyindoleacetic acid**
* This patient's symptoms (flushing, diarrhea, dyspnea, and cardiac valve abnormalities, especially right-sided with fibrous plaque deposition) are classic for **carcinoid syndrome**. This syndrome is caused by neuroendocrine tumors, often in the gastrointestinal tract, that secrete large amounts of serotonin.
* **5-hydroxyindoleacetic acid (5-HIAA)** is the main metabolite of **serotonin**, and its elevated levels in urine are a key diagnostic marker for carcinoid syndrome.
*Elevated serum bicarbonate*
* **Elevated serum bicarbonate** is typically associated with **metabolic alkalosis**, which is not a direct or expected finding in carcinoid syndrome.
* Carcinoid syndrome can lead to electrolyte imbalances due to diarrhea, but metabolic alkalosis through elevated bicarbonate is not a primary or characteristic feature.
*Elevated serum potassium*
* **Elevated serum potassium** (hyperkalemia) is not a common or direct consequence of carcinoid syndrome.
* While severe diarrhea can sometimes lead to electrolyte disturbances, it more typically causes **hypokalemia** due to potassium loss, not hyperkalemia.
*Decreased serum chromogranin A*
* **Chromogranin A** is a general marker for neuroendocrine tumors; however, in actively secreting tumors like those causing carcinoid syndrome, **serum chromogranin A** levels would most likely be **elevated**, not decreased.
* It serves as a useful diagnostic and prognostic marker for neuroendocrine tumors, indicating tumor burden and activity.
*Elevated urinary vanillylmandelic acid*
* **Elevated urinary vanillylmandelic acid (VMA)** is a diagnostic marker for **pheochromocytoma** and **paraganglioma**, tumors that secrete catecholamines (epinephrine and norepinephrine).
* While some symptoms like flushing can overlap, the specific cardiac and gastrointestinal symptoms described, along with the right-sided valvular lesions, are characteristic of carcinoid syndrome, not pheochromocytoma.
More Serotonin syndrome US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.