QT prolongation and torsades de pointes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for QT prolongation and torsades de pointes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
QT prolongation and torsades de pointes US Medical PG Question 1: Two days after admission for myocardial infarction and subsequent coronary angioplasty, a 65-year-old man becomes distressed and diaphoretic in the cardiac intensive care unit. Suddenly he is no longer responsive. Pulse oximetry does not show a tracing. He has a history of hypertension and depression. Prior to his admission, his medication included ramipril and aripiprazole. Examination shows no carotid pulse. An ECG is shown. After beginning chest compressions, which of the following is the most appropriate step in management of the patient?
- A. Intravenous procainamide
- B. Cardiac catheterization
- C. Intravenous amiodarone
- D. Intravenous magnesium sulfate
- E. Defibrillation (Correct Answer)
QT prolongation and torsades de pointes Explanation: ***Defibrillation***
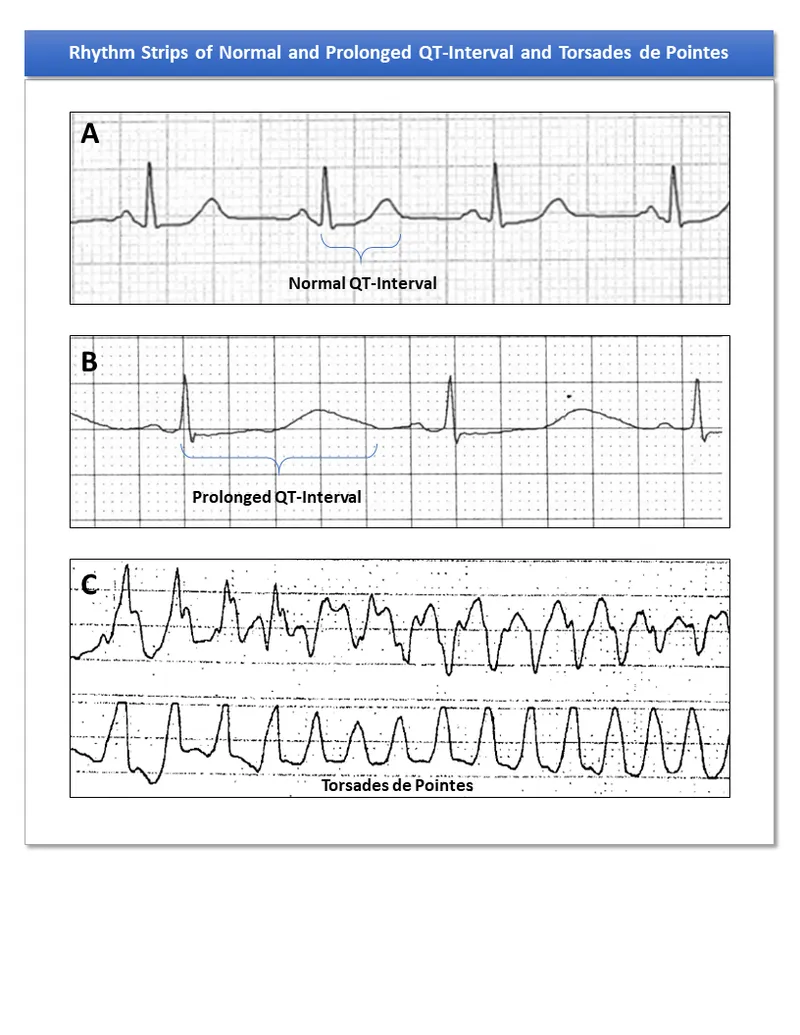
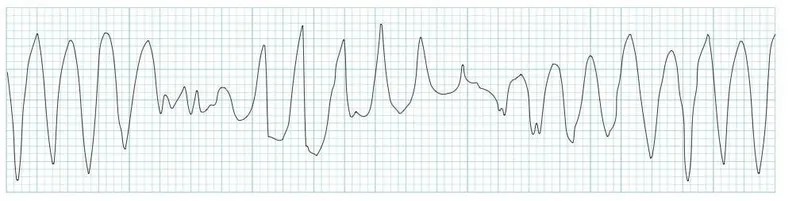
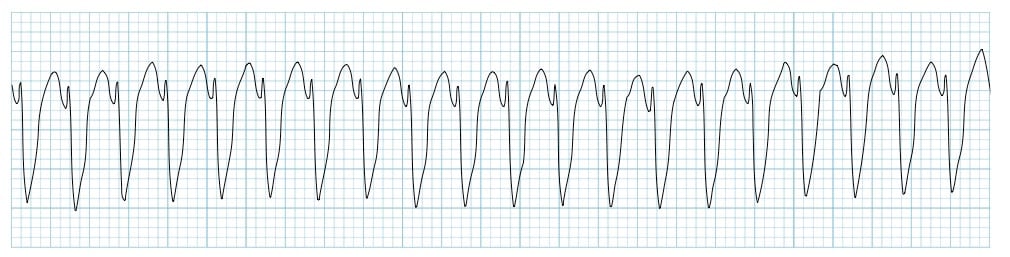
- The ECG shows a **wide complex tachycardia** consistent with either **ventricular fibrillation (VF)** or **pulseless ventricular tachycardia (VT)**.
- In a patient who is **unresponsive and pulseless**, both VF and pulseless VT are treated identically with **immediate unsynchronized defibrillation** after initiating CPR, according to **ACLS guidelines**.
- **Defibrillation** is the definitive treatment to restore a perfusing rhythm and is the priority intervention after chest compressions have begun.
*Intravenous procainamide*
- **Procainamide** is an antiarrhythmic drug used for certain types of **stable ventricular tachycardia** or wide-complex tachycardia of uncertain type when the patient has a pulse.
- It is **contraindicated** in pulseless arrhythmias like VF or pulseless VT, where electrical therapy (defibrillation) is paramount.
- Administration would cause dangerous delay in definitive treatment.
*Cardiac catheterization*
- **Cardiac catheterization** is an invasive diagnostic and interventional procedure typically performed to evaluate and treat coronary artery disease.
- It is **not an immediate life-saving intervention** for a patient in **cardiac arrest**, which requires immediate electrical therapy.
- Catheterization may be considered after return of spontaneous circulation (ROSC) to address underlying ischemia.
*Intravenous amiodarone*
- **Amiodarone** is an antiarrhythmic agent used in **VF/pulseless VT that is refractory to initial defibrillation attempts** and after epinephrine administration.
- It is administered **after initial defibrillation attempts have failed**, not as the primary or first-line treatment.
- The ACLS algorithm recommends amiodarone after the third shock if VF/pulseless VT persists.
*Intravenous magnesium sulfate*
- **Magnesium sulfate** is the treatment of choice for **Torsades de Pointes**, a polymorphic ventricular tachycardia often associated with **prolonged QT interval**.
- The clinical presentation and ECG do not suggest Torsades de Pointes, and magnesium is not indicated as the initial treatment for VF or monomorphic VT.
- Magnesium may also be considered for refractory VF/VT with suspected hypomagnesemia.
QT prolongation and torsades de pointes US Medical PG Question 2: A 62-year-old man is brought to the emergency department because of syncope. He reports sudden onset of palpitations followed by loss of consciousness while carrying his groceries to his car. He is unable to recall any further details and does not have any chest pain or dizziness. He has a history of hypertension, type 2 diabetes mellitus, gastroparesis, and osteoarthritis of the knees. Medications include lisinopril, metformin, and ondansetron as needed for nausea. He also takes methadone daily for chronic pain. Apart from an abrasion on his forehead, he appears well. His temperature is 37.2 °C (98.9 F), heart rate is 104/min and regular, and blood pressure is 135/70 mm Hg. While he is in the emergency department, he loses consciousness again. Telemetry shows polymorphic ventricular tachycardia with cyclic alteration of the QRS axis that spontaneously resolves after 30 seconds. Results of a complete blood count, serum electrolyte concentrations, and serum thyroid studies show no abnormalities. Cardiac enzymes are within normal limits. Which of the following is the most likely underlying cause of this patient's syncope?
- A. Prinzmetal angina
- B. Fast accessory conduction pathway
- C. Brugada syndrome
- D. Prolonged QT interval (Correct Answer)
- E. Hypomagnesemia
QT prolongation and torsades de pointes Explanation: ***Prolonged QT interval***
- The patient experienced **polymorphic ventricular tachycardia** with cyclic alteration of the **QRS axis** (Torsades de Pointes), which is characteristic of a prolonged QT interval.
- **Methadone is known to prolong the QT interval**, and the patient's history of syncope preceded by palpitations is consistent with this arrhythmia.
*Prinzmetal angina*
- Prinzmetal angina involves **coronary artery spasm**, leading to **transient myocardial ischemia**, typically causing chest pain, not primarily syncope from polymorphic VT.
- While it can cause arrhythmias, the characteristic EKG finding would be **ST-segment elevation during pain**, which is not described.
*Fast accessory conduction pathway*
- A fast accessory pathway (e.g., in Wolfe-Parkinson-White syndrome) can lead to **AV reentrant tachycardia** or **pre-excitation** with atrial fibrillation, but not typically polymorphic VT with cyclic QRS alteration.
- The EKG would show a **delta wave** and a short PR interval, which is not mentioned.
*Brugada syndrome*
- Brugada syndrome is an inherited channelopathy **characterized by specific EKG patterns** (e.g., coved-type ST elevation in V1-V3) and an increased risk of sudden cardiac death due to ventricular arrhythmias.
- The patient's EKG findings of polymorphic VT with cyclic QRS alteration are not typical of Brugada syndrome-induced arrhythmia.
*Hypomagnesemia*
- While **hypomagnesemia can prolong the QT interval** and lead to Torsades de Pointes, the patient's **serum electrolyte concentrations were normal**, ruling out this direct cause.
- Magnesium levels would need to be critically low for such an effect, and this is typically detected on blood tests.
QT prolongation and torsades de pointes US Medical PG Question 3: An investigator is comparing the risk of adverse effects among various antiarrhythmic medications. One of the drugs being studied primarily acts by blocking the outward flow of K+ during myocyte repolarization. Further investigation shows that the use of this drug is associated with a lower rate of ventricular tachycardia, ventricular fibrillation, and torsades de pointes when compared to similar drugs. Which of the following drugs is most likely being studied?
- A. Verapamil
- B. Procainamide
- C. Esmolol
- D. Amiodarone (Correct Answer)
- E. Sotalol
QT prolongation and torsades de pointes Explanation: ***Amiodarone***
- Amiodarone is a **Class III antiarrhythmic drug** that primarily blocks **potassium channels**, thereby prolonging repolarization and the effective refractory period in cardiac myocytes.
- While it has properties of all four Vaughn-Williams classes, its dominant action as a potassium channel blocker makes it highly effective in preventing and treating various arrhythmias, including **ventricular tachycardia (VT)** and **ventricular fibrillation (VF)**, and it has a relatively lower risk of **torsades de pointes (TdP)** compared to other Class III drugs due to its broader ion channel effects.
*Verapamil*
- Verapamil is a **Class IV antiarrhythmic drug (non-dihydropyridine calcium channel blocker)** that primarily blocks **L-type calcium channels**, slowing conduction through the AV node.
- It is mainly used for **supraventricular tachycardias** and rate control in atrial fibrillation, not typically for ventricular arrhythmias like VT/VF.
*Procainamide*
- Procainamide is a **Class IA antiarrhythmic drug** that blocks **sodium channels** and also prolongs repolarization by blocking some potassium channels, but its primary effect is on sodium channels.
- Class IA drugs are known to **increase the QT interval** and carry a significant risk of **torsades de pointes**, making them less favorable for preventing VT/VF with adverse effect concerns.
*Esmolol*
- Esmolol is a **Class II antiarrhythmic drug (beta-blocker)** that primarily acts by **blocking beta-adrenergic receptors**, thereby reducing heart rate, contractility, and AV nodal conduction.
- While useful in some arrhythmias, its main mechanism is not potassium channel blockade, and it is not typically preferred for the direct prevention of VT/VF in situations with concerns about TdP.
*Sotalol*
- Sotalol is a **Class III antiarrhythmic drug** that primarily acts as a **potassium channel blocker**, prolonging the action potential duration and effective refractory period, and also has **beta-blocking properties**.
- While it blocks potassium channels, sotalol carries a **higher risk of torsades de pointes** compared to amiodarone, especially at higher doses and in patients with underlying heart conditions.
QT prolongation and torsades de pointes US Medical PG Question 4: A 27-year-old man presents to the clinic for his annual physical examination. He was diagnosed with a rare arrhythmia a couple of years ago following an episode of dizziness. A mutation in the gene encoding for the L-type calcium channel protein was identified by genetic testing. He feels fine today. His vitals include: blood pressure 122/89 mm Hg, pulse 90/min, respiratory rate 14/min, and temperature 36.7°C (98.0°F). The cardiac examination is unremarkable. The patient has been conducting some internet research on how the heart works and specifically asks you about his own “ventricular action potential”. Which of the following would you expect to see in this patient?
- A. Abnormal phase 2 (Correct Answer)
- B. Abnormal phase 4
- C. Abnormal phase 0
- D. Abnormal phase 3
- E. Abnormal phase 1
QT prolongation and torsades de pointes Explanation: ***Abnormal phase 2***
- Phase 2 of the ventricular action potential, also known as the **plateau phase**, is primarily maintained by the influx of **L-type calcium channels** and the efflux of potassium.
- A mutation in the gene encoding for the L-type calcium channel protein would directly affect phase 2 and likely **result in an abnormal plateau phase** of the action potential.
*Abnormal phase 4*
- Phase 4 represents the **resting membrane potential** in ventricular myocytes and is maintained by **inward-rectifier potassium channels**.
- Mutations affecting L-type calcium channels would not directly or primarily cause an abnormality in the resting potential.
*Abnormal phase 0*
- Phase 0, the **depolarization phase**, is driven by the rapid influx of **sodium ions** through fast voltage-gated sodium channels.
- While calcium channels play a minor role, their primary impact is not on the initial rapid upstroke of phase 0.
*Abnormal phase 3*
- Phase 3, the **repolarization phase**, is primarily mediated by the **efflux of potassium ions** through various potassium channels (e.g., delayed rectifier potassium channels).
- Although calcium channel inactivation contributes to the end of the plateau, the **dominant ion flux** determining phase 3 is potassium efflux.
*Abnormal phase 1*
- Phase 1, the **initial repolarization phase**, is characterized by the **inactivation of sodium channels** and a brief efflux of potassium ions through transient outward potassium channels.
- L-type calcium channel activity is just beginning during this phase and is not the primary determinant of its shape.
QT prolongation and torsades de pointes US Medical PG Question 5: Four days into hospitalization for severe pneumonia, a 76-year-old woman suddenly becomes unresponsive. She has no history of heart disease. She is on clarithromycin and ceftriaxone. Her carotid pulse is not detected. A single-lead ECG strip is shown. Previous ECG shows QT prolongation. Laboratory studies show:
Serum
Na+ 145 mEq/L
K+ 6.1 mEq/L
Ca2+ 10.5 mEq/L
Mg2+ 1.8 mEq/L
Thyroid-stimulating hormone 0.1 μU/mL
Cardiopulmonary resuscitation has been initiated. Which of the following is the most likely underlying cause of this patient’s recent condition?
- A. Clarithromycin (Correct Answer)
- B. Hypercalcemia
- C. Thyrotoxicosis
- D. Septic shock
- E. Hyperkalemia
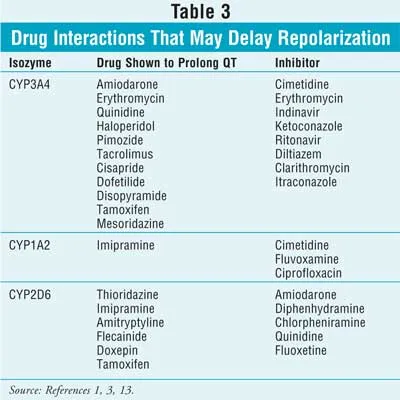
QT prolongation and torsades de pointes Explanation: ***Clarithromycin***
- The patient presents with sudden unresponsiveness and unpalpable carotid pulse, characteristic of **cardiac arrest**, specifically likely due to **Torsades de Pointes (TdP)**, given the history of **QT prolongation** and the ECG findings (not shown but implied by the clinical context).
- **Clarithromycin** is a macrolide antibiotic known to prolong the QT interval and increase the risk of TdP, especially in patients with pre-existing QT prolongation or electrolyte abnormalities.
*Hypercalcemia*
- While **hypercalcemia** can cause cardiac arrhythmias, the provided calcium level (10.5 mEq/L) is only mildly elevated and typically does not precipitate TdP or sudden cardiac arrest in this manner.
- More significant hypercalcemia is usually required to cause severe cardiac manifestations, and its effect on the QT interval is generally to **shorten** it, not prolong it.
*Thyrotoxicosis*
- The patient's **TSH of 0.1 µU/mL** indicates suppressed TSH, consistent with hyperthyroidism or thyrotoxicosis. While thyrotoxicosis can cause arrhythmias, it typically manifests as **atrial fibrillation** or **sinus tachycardia**, not TdP or sudden cardiac arrest in this acute presentation.
- The primary concern here is QT prolongation leading to TdP, which is not a direct or common complication of thyrotoxicosis.
*Septic shock*
- The patient has severe pneumonia and could be at risk of **septic shock**, which can cause cardiovascular collapse. However, the presentation with sudden unresponsiveness, unpalpable pulse, and context of QT prolongation points more specifically to an **arrhythmic cause** rather than generalized circulatory failure as the primary etiology of this acute event.
- While shock can lead to electrolyte disturbances and contribute to cardiac instability, the immediate cause of unresponsiveness is likely an arrhythmia like TdP, which is directly linked to the medication.
*Hyperkalemia*
- The patient's **potassium level of 6.1 mEq/L** indicates significant hyperkalemia, which can indeed cause severe cardiac arrhythmias, including **ventricular fibrillation** and **asystole**.
- However, hyperkalemia typically **shortens the QT interval** and widens the QRS complex, which is opposite to the pre-existing QT prolongation observed before the event.
QT prolongation and torsades de pointes US Medical PG Question 6: A 51-year-old woman schedules an appointment with her physician with complaints of upper abdominal pain, nausea, and early satiety for the last 6 months. She has type 1 diabetes for the past 10 years and is on subcutaneous insulin therapy. She complains of occasional heartburn and lost 4.5 kg (10 lb) in the past 6 months without any changes in her diet. The medical history is significant for long QT syndrome. The vital signs include: pulse 74/min, respirations 18/min, temperature 37.7°C (99.9°F), and blood pressure 140/84 mm Hg. Abdominal examination is negative for organomegaly or a palpable mass, but there is a presence of succussion splash. She has slightly decreased vision in both her eyes and fundoscopy reveals diabetic changes in the retina. Esophagogastroduodenoscopy is performed, which is negative for obstruction, but a small ulcer is noted near the cardiac end of the stomach with some food particles. Which of the following drugs would be inappropriate in the management of this patient's condition?
- A. Bethanechol
- B. Domperidone
- C. Erythromycin
- D. Promethazine
- E. Cisapride (Correct Answer)
QT prolongation and torsades de pointes Explanation: ***Cisapride***
- Cisapride is a **prokinetic agent** that was largely withdrawn due to its propensity to cause **QT prolongation** and life-threatening arrhythmias, which is critically contraindicated in patients with a history of **long QT syndrome**.
- The patient's history of **long QT syndrome** makes cisapride an inappropriate and dangerous choice for managing her diabetic gastroparesis.
*Bethanechol*
- Bethanechol is a **muscarinic agonist** that can increase gastric motility, but it is not typically first-line for gastroparesis due to potential systemic cholinergic side effects.
- While it aids in stomach emptying, its use must be weighed against its side-effect profile, though it doesn't directly interact with QT interval.
*Domperidone*
- Domperidone is a **dopamine D2 receptor antagonist** that acts as a prokinetic and antiemetic, primarily in the periphery, minimizing central nervous system side effects.
- While generally safer regarding QT prolongation than some other prokinetics, it can still prolong the QT interval in high doses or in susceptible individuals, but less severely than cisapride.
*Erythromycin*
- Erythromycin is a **macrolide antibiotic** that acts as a **motilin receptor agonist**, significantly increasing gastric emptying.
- It's a useful prokinetic for gastroparesis, although long-term use can be limited by antibiotic resistance and potential for **QT prolongation**, though less severe than cisapride.
*Promethazine*
- Promethazine is an **antihistamine** with antiemetic properties, often used for nausea and vomiting, but it is **not a prokinetic agent**.
- It would address the nausea symptomatically but would not improve gastric emptying in a patient with gastroparesis.
QT prolongation and torsades de pointes US Medical PG Question 7: A 54-year-old man with a past medical history significant for hypertension, type 2 diabetes, and chronic obstructive pulmonary disease presents with complaints of nausea and abdominal pain for the past month. The pain is located in the epigastric region and is described as “burning” in quality, often following food intake. The patient denies any changes in bowel movements, fever, or significant weight loss. Medications include metformin, lisinopril, hydrochlorothiazide, albuterol inhaler, and fluconazole for a recent fungal infection. Physical examination was unremarkable except for a mildly distended abdomen that is diffusely tender to palpation and decreased sensation at lower extremities bilaterally. A medication was started for the symptoms. Two days later, the patient reports heart palpitations. An EKG is shown below. Which of the following is the medication most likely prescribed?
- A. Aspirin
- B. Metformin
- C. Omeprazole
- D. Ranitidine
- E. Erythromycin (Correct Answer)
QT prolongation and torsades de pointes Explanation: ***Erythromycin***
- The EKG shows **QT prolongation** (long QT interval), which can lead to **torsades de pointes** and palpitations. Erythromycin is a macrolide antibiotic known to cause QT prolongation.
- **Critical drug interaction:** The patient is taking **fluconazole**, a strong **CYP3A4 inhibitor**, which increases erythromycin levels (a CYP3A4 substrate), significantly enhancing the risk of QT prolongation and cardiac arrhythmias.
- Given the patient's complaints of burning epigastric pain following food intake and diabetic neuropathy, a diagnosis of **diabetic gastroparesis** is suggested. Erythromycin can be used as a **prokinetic agent** for gastroparesis due to its agonistic effect on motilin receptors, thus explaining its prescription.
*Aspirin*
- Aspirin is a **non-steroidal anti-inflammatory drug (NSAID)** and an antiplatelet agent. While it can cause epigastric pain and is often used in cardiovascular disease patients, it does not typically cause QT prolongation or palpitations.
- It is unlikely to be prescribed for the patient's symptoms of nausea and burning epigastric pain, as it can **exacerbate gastric irritation**.
*Metformin*
- Metformin is an oral hypoglycemic agent already listed in the patient's current medication list and used for type 2 diabetes. Its primary side effects relate to **gastrointestinal upset** (e.g., nausea, diarrhea) but it doesn't cause QT prolongation.
- The question implies a *new* medication was started, and metformin is an existing medication *for diabetes*, not specifically for the new burning epigastric pain.
*Omeprazole*
- Omeprazole is a **proton pump inhibitor (PPI)** commonly prescribed for acid reflux and peptic ulcer disease, which might align with the burning epigastric pain.
- However, PPIs are generally not associated with **QT prolongation** or palpitations.
*Ranitidine*
- Ranitidine is an **H2 receptor antagonist** used to reduce stomach acid, similar to omeprazole, and could be prescribed for the epigastric pain.
- Like omeprazole, ranitidine is not known to cause **QT prolongation** or cardiac arrhythmias like palpitations.
QT prolongation and torsades de pointes US Medical PG Question 8: A 72-year-old man with congestive heart failure is brought to the emergency department because of chest pain, shortness of breath, dizziness, and palpitations for 30 minutes. An ECG shows a wide complex tachycardia with a P-wave rate of 105/min, an R-wave rate of 130/min, and no apparent relation between the two. Intravenous pharmacotherapy is initiated with a drug that prolongs the QRS and QT intervals. The patient was most likely treated with which of the following drugs?
- A. Carvedilol
- B. Verapamil
- C. Flecainide
- D. Quinidine (Correct Answer)
- E. Sotalol
QT prolongation and torsades de pointes Explanation: **Quinidine**
- Quinidine is a **Class IA antiarrhythmic** that blocks fast sodium channels, prolonging both the **QRS complex** (due to slowed conduction) and the **QT interval** (due to prolonged repolarization).
- The ECG findings of **wide-complex tachycardia** and **AV dissociation** (P-wave rate different from R-wave rate without apparent relation) are consistent with ventricular tachycardia, which Class IA drugs can treat.
*Carvedilol*
- Carvedilol is a **beta-blocker** (Class II antiarrhythmic) that primarily slows heart rate and AV nodal conduction, generally **shortening the QT interval** or having no effect, and would not widen the QRS complex.
- Beta-blockers are typically contraindicated in **decompensated heart failure** and **wide-complex tachycardia** due to their negative inotropic effects and risk of worsening decompensation.
*Verapamil*
- Verapamil is a **non-dihydropyridine calcium channel blocker** (Class IV antiarrhythmic) that mainly slows AV nodal conduction. It would not cause QRS widening and can shorten the QT interval.
- Verapamil is generally contraindicated in **wide-complex tachycardias** of unknown origin as it can precipitate cardiovascular collapse if the arrhythmia is ventricular.
*Flecainide*
- Flecainide is a **Class IC antiarrhythmic** that primarily blocks fast sodium channels, causing significant **QRS widening** but has **minimal effect on the QT interval**, which is contrary to the case description.
- Class IC agents are also generally avoided in patients with **structural heart disease** like congestive heart failure due to increased mortality risk.
*Sotalol*
- Sotalol is a **Class III antiarrhythmic** (beta-blocker with potassium channel blockade) that primarily prolongs the **QT interval** by blocking potassium channels. While it prolongs the QT, it does **not significantly widen the QRS complex**.
- Its beta-blocking effects could exacerbate **decompensated heart failure** in this patient, similar to carvedilol.
QT prolongation and torsades de pointes US Medical PG Question 9: Match the following drugs in Column A with their contraindications in Column B.
| Column A | Column B |
| :-- | :-- |
| 1. Morphine | 1. QT prolongation |
| 2. Amiodarone | 2. Thromboembolism |
| 3. Vigabatrin | 3. Pregnancy |
| 4. Estrogen preparations | 4. Head injury |
- A. A-1, B-3, C-2, D-4
- B. A-4, B-1, C-3, D-2 (Correct Answer)
- C. A-3, B-2, C-4, D-1
- D. A-2, B-4, C-1, D-3
QT prolongation and torsades de pointes Explanation: ***A-4, B-1, C-3, D-2***
- **Morphine** is contraindicated in **head injury** as it can increase intracranial pressure and mask neurological symptoms.
- **Amiodarone** is contraindicated in patients with **QT prolongation** due to its risk of inducing more severe arrhythmias like Torsades de Pointes.
- **Vigabatrin** is contraindicated during **pregnancy** due to its potential for teratogenicity and adverse effects on fetal development.
- **Estrogen preparations** are contraindicated in patients with a history of **thromboembolism** due to their increased risk of blood clot formation.
*A-1, B-3, C-2, D-4*
- This option incorrectly matches **Morphine** with QT prolongation and **Estrogen preparations** with head injury, which are not their primary contraindications.
- It also incorrectly links **Vigabatrin** with thromboembolism and **Amiodarone** with pregnancy.
*A-3, B-2, C-4, D-1*
- This choice incorrectly associates **Morphine** with pregnancy and **Vigabatrin** with head injury, which are not the most critical or direct contraindications.
- It also misaligns **Amiodarone** with thromboembolism and **Estrogen preparations** with QT prolongation.
*A-2, B-4, C-1, D-3*
- This option incorrectly matches **Morphine** with thromboembolism and **Amiodarone** with head injury, which are not their most significant contraindications.
- It also incorrectly links **Vigabatrin** with QT prolongation and **Estrogen preparations** with pregnancy.
QT prolongation and torsades de pointes US Medical PG Question 10: A 70-year-old male immigrant from Asia is brought to the emergency room with complaints of palpitations and light-headedness for 1 hour. The patient was sitting in his chair watching television when he felt his heart racing and became dizzy. He was unable to stand up from his chair because of weakness and light-headedness. His past medical history is notable for mitral stenosis secondary to rheumatic fever as a child. On arrival to the emergency department, the patient's temperature is 99.7°F (37.6°C), blood pressure is 110/55 mmHg, pulse is 140/min, and respirations are 15/min. The patient appears comfortable but anxious. Electrocardiogram shows atrial fibrillation with rapid ventricular response. The patient is started on dofetilide. Which of the following would be expected in this patient’s cardiac action potential as a result of this drug?
- A. Decreased conduction velocity
- B. Increased QT interval (Correct Answer)
- C. Decreased calcium current
- D. Decreased slope of phase 0
- E. Decreased slope of phase 4
QT prolongation and torsades de pointes Explanation: ***Increased QT interval***
- **Dofetilide** is a **Class III antiarrhythmic** drug that primarily blocks the delayed rectifier **potassium channels (Ik)** in cardiomyocytes.
- Blocking potassium efflux prolongs repolarization, which is reflected as a **prolonged action potential duration (APD)** and a lengthened **QT interval** on the electrocardiogram.
*Decreased conduction velocity*
- This effect is primarily associated with **Class I antiarrhythmic drugs** (e.g., flecainide, procainamide) which block **sodium channels**, thereby slowing the depolarization (Phase 0) and subsequent conduction velocity.
- **Dofetilide**, a Class III agent, does not directly impact sodium channels or significantly decrease conduction velocity.
*Decreased calcium current*
- A decreased calcium current (Phase 2) is characteristic of **Class IV antiarrhythmic drugs** (**calcium channel blockers** like verapamil and diltiazem).
- These drugs primarily act on nodal tissue to slow AV nodal conduction and heart rate, which is not the primary mechanism of action for **dofetilide**.
*Decreased slope of phase 0*
- The slope of **Phase 0 (depolarization)** is determined by the rapid influx of **sodium ions** into the cell.
- A decreased slope of Phase 0 would be expected with **Class I antiarrhythmic drugs** (sodium channel blockers), not with **dofetilide**, which targets potassium channels.
*Decreased slope of phase 4*
- The slope of **Phase 4 (spontaneous depolarization)** in pacemaker cells is primarily influenced by the "funny current" (If) and calcium currents.
- A decreased slope of Phase 4 is characteristic of **beta-blockers** (Class II antiarrhythmics) or **calcium channel blockers** that reduce the rate of spontaneous depolarization in nodal cells, thereby lowering heart rate. **Dofetilide** does not have this primary effect.
More QT prolongation and torsades de pointes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.