Pharmacodynamic interaction mechanisms US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pharmacodynamic interaction mechanisms. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pharmacodynamic interaction mechanisms US Medical PG Question 1: A 50-year-old woman presents with acute onset fever and chills for the past hour. She mentions earlier in the day she felt blue, so she took some St. John’s wort because she was told by a friend that it helps with depression. Past medical history is significant for hypertension, diabetes mellitus, and depression managed medically with captopril, metformin, and fluoxetine. She has no history of allergies. Her pulse is 130/min, the respiratory rate is 18/min, the blood pressure is 176/92 mm Hg, and the temperature is 38.5°C (101.3°F). On physical examination, the patient is profusely diaphoretic and extremely irritable when asked questions. Oriented x 3. The abdomen is soft and nontender with no hepatosplenomegaly. Increased bowel sounds are heard in the abdomen. Deep tendon reflexes are 3+ bilaterally and clonus is elicited. The sensation is decreased in the feet bilaterally. Mydriasis is present. Fingerstick glucose is 140 mg/dL. An ECG shows sinus tachycardia but is otherwise normal. Which of the following is the most likely cause of this patient’s condition?
- A. Sepsis
- B. Anaphylactic reaction
- C. Diabetic ketoacidosis
- D. Neuroleptic malignant syndrome
- E. Serotonin syndrome (Correct Answer)
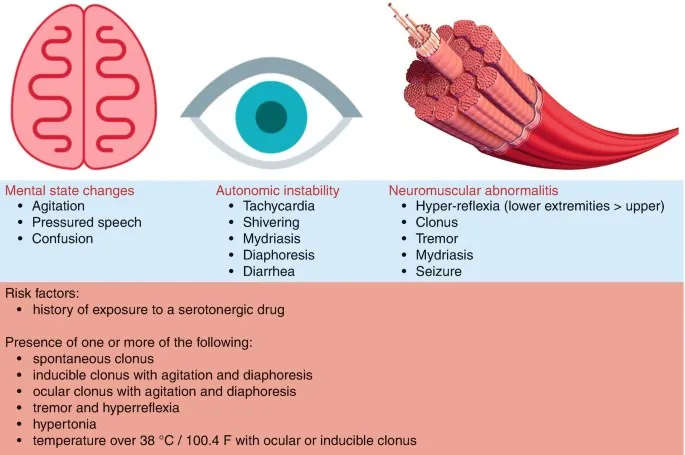
Pharmacodynamic interaction mechanisms Explanation: ***Serotonin syndrome***
- The patient's presentation with **fever, diaphoresis, hypertension, tachycardia, hyperreflexia, clonus, mydriasis**, and **agitation** after combining an **SSRI (fluoxetine)** with **St. John's wort** (a serotonin-enhancing herbal supplement) is highly characteristic of serotonin syndrome.
- This condition results from excessive serotonergic activity in the central and peripheral nervous system.
*Sepsis*
- While **fever, chills, and tachycardia** can be indicators of sepsis, the presence of specific neurological and neuromuscular signs like **hyperreflexia, clonus, and mydriasis** points away from it.
- The patient's **irritable state and normal mental orientation** is less typical for severe sepsis, which often involves altered mental status.
*Anaphylactic reaction*
- **Anaphylaxis** presents with rapid onset of symptoms such as **urticaria, angioedema, bronchospasm, and hypotension**, which are not observed in this patient.
- There is no history of allergen exposure, and the prominent neurological symptoms are not typical of anaphylaxis.
*Diabetic ketoacidosis*
- **DKA** is characterized by **hyperglycemia, metabolic acidosis, and ketonemia**, often presenting with Kussmaul respirations and fruity breath odor.
- The patient's **fingerstick glucose (140 mg/dL)** is not significantly elevated, and there is no mention of deep, rapid breathing or other DKA-specific symptoms.
*Neuroleptic malignant syndrome*
- **NMS** is typically associated with exposure to **dopamine antagonists (antipsychotics)** and is characterized by **severe muscle rigidity, hyperthermia, altered mental status, and autonomic instability.**
- While some symptoms overlap, this patient's history of St. John's wort and fluoxetine points to increased serotonin, and the specific neuromuscular findings like clonus are more indicative of serotonin syndrome.
Pharmacodynamic interaction mechanisms US Medical PG Question 2: A 59-year-old man is brought to the emergency department one hour after developing shortness of breath and “squeezing” chest pain that began while he was mowing the lawn. He has asthma, hypertension, and erectile dysfunction. Current medications include salmeterol, amlodipine, lisinopril, and vardenafil. His pulse is 110/min and blood pressure is 122/70 mm Hg. Physical examination shows diaphoresis. An ECG shows sinus tachycardia. Sublingual nitroglycerin is administered. Five minutes later, his pulse is 137/min and his blood pressure is 78/40 mm Hg. Which of the following is the most likely mechanism of this patient's hypotension?
- A. Bradykinin accumulation
- B. Cyclic GMP elevation (Correct Answer)
- C. Decreased nitric oxide production
- D. Calcium channel antagonism
- E. Alpha-1 receptor antagonism
Pharmacodynamic interaction mechanisms Explanation: ***Cyclic GMP elevation***
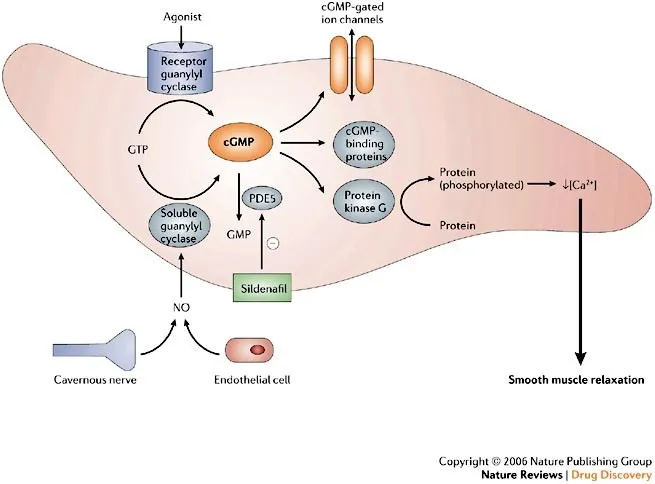
- The patient's severe hypotension after nitroglycerin administration is likely due to an interaction with **vardenafil**, a **phosphodiesterase-5 (PDE5) inhibitor**.
- Both nitroglycerin and vardenafil increase levels of **cyclic guanosine monophosphate (cGMP)**, leading to excessive systemic vasodilation and profound hypotension.
*Bradykinin accumulation*
- This is a well-known side effect of **ACE inhibitors (e.g., lisinopril)**, manifesting primarily as a dry cough or angioedema.
- While the patient is on lisinopril, bradykinin accumulation does not immediately cause severe hypotension following nitroglycerin administration in this manner.
*Decreased nitric oxide production*
- Nitric oxide (NO) is a **vasodilator**; decreased production would typically lead to vasoconstriction and *increased* blood pressure, not hypotension.
- Nitroglycerin, in fact, works by **increasing NO production** or release to induce vasodilation.
*Calcium channel antagonism*
- **Amlodipine** is a calcium channel blocker, which can cause vasodilation and lower blood pressure.
- However, the sudden and severe drop in blood pressure observed *after* nitroglycerin is not primarily due to an additive effect of amlodipine in the way PDE5 inhibitors interact.
*Alpha-1 receptor antagonism*
- Alpha-1 receptor antagonists (e.g., prazosin, doxazosin) cause **vasodilation** by blocking norepinephrine's action on blood vessels.
- While they can cause orthostatic hypotension, the patient is not on such a medication, and this mechanism does not explain the acute, severe drop seen after nitroglycerin.
Pharmacodynamic interaction mechanisms US Medical PG Question 3: A 71-year-old man presents to his oncologist with nausea. He recently underwent chemotherapy for pancreatic cancer and has developed severe intractable nausea over the past week. He vomits several times a day. His past medical history is notable for gout, osteoarthritis, and major depressive disorder. He takes allopurinol and sertraline. He has a 15-pack-year smoking history and drinks 1 glass of wine per day. His temperature is 98.6°F (37°C), blood pressure is 148/88 mmHg, pulse is 106/min, and respirations are 22/min. On exam, he is lethargic but able to answer questions appropriately. He has decreased skin turgor and dry mucous membranes. He is started on a medication to treat nausea. However, 3 days later he presents to the emergency room with fever, agitation, hypertonia, and clonus. What is the most likely mechanism of action of the drug this patient was prescribed?
- A. 5-HT3 receptor antagonist (Correct Answer)
- B. M1 receptor antagonist
- C. Opiate receptor agonist
- D. D2 receptor antagonist
- E. H1 receptor antagonist
Pharmacodynamic interaction mechanisms Explanation: ***5-HT3 receptor antagonist***
- The patient's symptoms of **fever**, **agitation**, **hypertonia**, and **clonus** after starting an antiemetic strongly suggest **serotonin syndrome**.
- **Ondansetron**, a common 5-HT3 receptor antagonist used for chemotherapy-induced nausea, can precipitate serotonin syndrome, especially when used with **SSRIs** like **sertraline**.
*M1 receptor antagonist*
- **M1 receptor antagonists** (e.g., scopolamine, atropine) are anticholinergic agents that can cause dry mouth, blurred vision, urinary retention, and constipation.
- They are not typically associated with the severe neuromuscular and autonomic hyperactivity seen in **serotonin syndrome**.
*Opiate receptor agonist*
- **Opiate receptor agonists** (e.g., morphine, fentanyl) primarily cause CNS depression, respiratory depression, constipation, and miosis.
- They do not cause features like clonus, agitation, or hypertonia characteristic of **serotonin syndrome**.
*D2 receptor antagonist*
- **D2 receptor antagonists** (e.g., metoclopramide, prochlorperazine) can cause **extrapyramidal symptoms** (dystonia, akathisia) and **neuroleptic malignant syndrome** (NMS).
- NMS also presents with fever and rigidity but lacks hyperreflexia and clonus, which are prominent in **serotonin syndrome**.
*H1 receptor antagonist*
- **H1 receptor antagonists** (e.g., promethazine, diphenhydramine) are used for nausea due to their sedative and anticholinergic effects.
- Their side effects include sedation, dizziness, and anticholinergic effects, but not the specific constellation of symptoms indicative of **serotonin syndrome**.
Pharmacodynamic interaction mechanisms US Medical PG Question 4: A 14-year-old boy is brought to the emergency department because of a 4-hour history of vomiting, lethargy, and confusion. Three days ago, he was treated with an over-the-counter medication for fever and runny nose. He is oriented only to person. His blood pressure is 100/70 mm Hg. Examination shows bilateral optic disc swelling and hepatomegaly. His blood glucose concentration is 65 mg/dL. Toxicology screening for serum acetaminophen is negative. The over-the-counter medication that was most likely used by this patient has which of the following additional effects?
- A. Increased partial thromboplastin time
- B. Decreased uric acid elimination
- C. Decreased expression of glycoprotein IIb/IIIa
- D. Irreversible inhibition of ATP synthase
- E. Irreversible inhibition of cyclooxygenase-1 (Correct Answer)
Pharmacodynamic interaction mechanisms Explanation: ***Irreversible inhibition of cyclooxygenase-1***
- The patient's presentation is classic for **Reye syndrome** (vomiting, lethargy, confusion, cerebral edema with optic disc swelling, hepatomegaly, hypoglycemia) following recent viral illness treated with OTC medication
- **Aspirin** is strongly associated with Reye syndrome in children with viral infections and should be avoided in this population
- The "additional effect" of aspirin is its mechanism of action: **irreversible acetylation and inhibition of COX-1 and COX-2**
- This irreversible COX inhibition also explains aspirin's antiplatelet effects (via inhibition of thromboxane A2 synthesis) and anti-inflammatory properties
*Increased partial thromboplastin time*
- PTT measures the intrinsic and common coagulation pathways and is prolonged by **heparin** or clotting factor deficiencies
- Aspirin affects **platelet function** (prolonging bleeding time), not the coagulation cascade measured by PTT
- While Reye syndrome can cause coagulopathy from liver dysfunction, increased PTT is not a direct pharmacologic effect of aspirin
*Decreased uric acid elimination*
- **Low-dose aspirin** (<2 g/day) can decrease renal uric acid excretion and may precipitate gout
- While this is true, it is not the primary or most clinically relevant "additional effect" in this context
- High-dose aspirin actually increases uric acid excretion (uricosuric effect)
*Decreased expression of glycoprotein IIb/IIIa*
- This is the mechanism of **GP IIb/IIIa inhibitors** (abciximab, eptifibatide, tirofiban), not aspirin
- Aspirin inhibits platelet aggregation by preventing thromboxane A2 synthesis, not by affecting GP IIb/IIIa expression
- These are IV antiplatelet agents used in acute coronary syndromes, not OTC medications
*Irreversible inhibition of ATP synthase*
- This is not a mechanism of aspirin or other common OTC fever/cold medications
- While Reye syndrome involves mitochondrial dysfunction, aspirin does not directly inhibit ATP synthase
- The mitochondrial injury in Reye syndrome is likely multifactorial
Pharmacodynamic interaction mechanisms US Medical PG Question 5: A 25-year-old woman presents to the ED with nausea, vomiting, diarrhea, abdominal pain, and hematemesis after ingesting large quantities of a drug. Which of the following pairs a drug overdose with the correct antidote for this scenario?
- A. Iron; deferoxamine (Correct Answer)
- B. Organophosphate; physostigmine
- C. Atropine; fomepizole
- D. Aspirin; N-acetylcysteine
- E. Acetaminophen; naloxone
Pharmacodynamic interaction mechanisms Explanation: ***Iron; deferoxamine***
- The symptoms of **nausea, vomiting, diarrhea, abdominal pain, and hematemesis** are classic signs of **iron overdose**, which causes direct corrosive injury to the GI mucosa.
- **Deferoxamine** is a **chelating agent** specifically used to bind iron ions and facilitate their excretion, thus reversing iron toxicity.
*Organophosphate; physostigmine*
- **Organophosphate poisoning** presents with a **cholinergic crisis** (SLUDGE: salivation, lacrimation, urination, defecation, GI upset, emesis, miosis), but **hematemesis** is not a primary feature.
- **Physostigmine** is an acetylcholinesterase inhibitor used for atropine overdose, not organophosphate poisoning; **atropine** and **pralidoxime** are the antidotes for organophosphate.
*Atropine; fomepizole*
- **Atropine overdose** causes **anticholinergic symptoms** (dry mouth, blurred vision, tachycardia, urinary retention, delirium), not GI irritation and hematemesis.
- **Fomepizole** is an antidote for **methanol** or **ethylene glycol poisoning**, not atropine.
*Aspirin; N-acetylcysteine*
- **Aspirin overdose** (salicylate toxicity) results in **tinnitus, hyperventilation, metabolic acidosis, and altered mental status**, but **hematemesis** is less common than with iron.
- **N-acetylcysteine** is the antidote for acetaminophen overdose, not aspirin; aspirin overdose is treated with **alkalinization of urine** and **hemodialysis**.
*Acetaminophen; naloxone*
- **Acetaminophen overdose** primarily causes **hepatic toxicity**, initially presenting with non-specific GI symptoms, but **hematemesis** is atypical, and the main concern is liver damage.
- **Naloxone** is an opioid antagonist used to reverse opioid overdose, not acetaminophen.
Pharmacodynamic interaction mechanisms US Medical PG Question 6: A 52-year-old man with a history of hypertension and hyperlipidemia comes to the physician because of a 10-month history of substernal chest pain on exertion that is relieved with rest. His pulse is 82/min and blood pressure is 145/82 mm Hg. He is prescribed a drug that acts by forming free radical nitric oxide. The patient is most likely to experience which of the following adverse effects as a result of this drug?
- A. Pulsating headaches (Correct Answer)
- B. Erectile dysfunction
- C. Hypertensive urgency
- D. Lower extremity edema
- E. Nonproductive cough
Pharmacodynamic interaction mechanisms Explanation: ***Pulsating headaches***
- The drug described is likely **nitroglycerin** or another **nitrate**, which acts by releasing **nitric oxide (NO)** to cause **vasodilation**.
- **Vasodilation** in the cerebral vasculature is a common side effect of nitrates and can lead to **pulsating headaches**.
*Erectile dysfunction*
- **Erectile dysfunction** is not a direct adverse effect of nitrates; in fact, nitrates can be used to treat it, though their use with PDE5 inhibitors is contraindicated.
- This condition is more commonly associated with the underlying cardiovascular disease rather than the medication used to treat angina.
*Hypertensive urgency*
- **Nitrates** cause **vasodilation** and typically **lower blood pressure**, making **hypotension** (not hypertension) a potential side effect.
- **Hypertensive urgency** would indicate a sudden, severe elevation in blood pressure, which is antithetical to the drug's mechanism of action.
*Lower extremity edema*
- **Lower extremity edema** is generally not a direct side effect of nitrates; it is more commonly associated with conditions like **heart failure**, certain **calcium channel blockers**, or **venous insufficiency**.
- While vasodilation can sometimes lead to fluid shifts, edema is not a prominent or expected adverse effect of this class of drugs.
*Nonproductive cough*
- A **nonproductive cough** is a common side effect of **ACE inhibitors** (e.g., lisinopril), which act on the **renin-angiotensin-aldosterone system**.
- This symptom is not associated with **nitrates** because their mechanism of action is primarily through nitric oxide-mediated vasodilation, unrelated to the respiratory irritation seen with ACE inhibitors.
Pharmacodynamic interaction mechanisms US Medical PG Question 7: Scientists are developing a new non-steroidal anti-inflammatory drug for osteoarthritis. Their hope is that the new drug will have a higher potency but the same efficacy as ibuprofen in the hope of minimizing gastrointestinal side effects. If ibuprofen is curve C in the figure provided, which of the following would be the curve for the new drug based on the scientists’ specifications? The desired therapeutic effect in patients is represented by the dashed line Y.
- A. Curve B
- B. Curve D
- C. Curve C
- D. Curve E
- E. Curve A (Correct Answer)
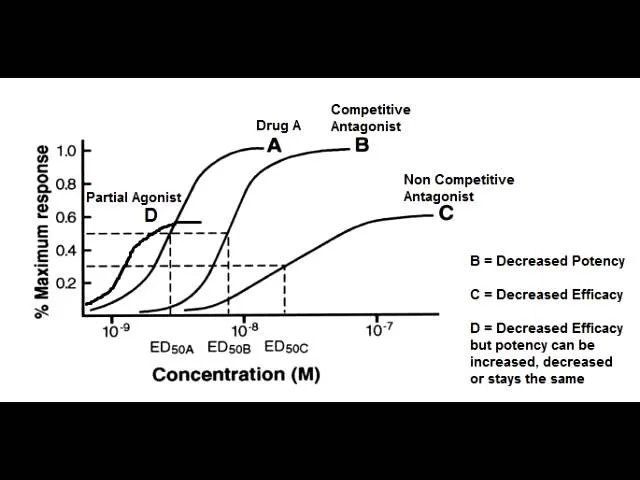
Pharmacodynamic interaction mechanisms Explanation: ***Curve A***
- A drug with **higher potency** will achieve its maximal effect at a lower concentration, shifting the curve to the **left** (from C to A).
- **Same efficacy** means the drug reaches the **same maximal effect** (height on the y-axis) as ibuprofen (curve C), which curve A does.
*Curve B*
- This curve represents a drug with **lower potency** than ibuprofen, as it requires a higher concentration to achieve its maximal effect, shifting the curve to the right.
- While it has the same efficacy, it does not meet the requirement of higher potency.
*Curve D*
- Curve D shows a drug with **higher potency** (shifted left) but **lower efficacy** (lower maximal effect) compared to ibuprofen.
- The scientists are looking for the same efficacy, not lower efficacy.
*Curve E*
- Curve E represents a drug with **lower efficacy** (lower maximal effect) than ibuprofen.
- It also appears to have lower potency as the curve is shifted to the right, failing both criteria.
*Curve C*
- This curve is ibuprofen itself, meaning there is no change in potency or efficacy.
- The new drug needs to have higher potency while maintaining the same efficacy as ibuprofen.
Pharmacodynamic interaction mechanisms US Medical PG Question 8: A 22-year-old woman presents to the emergency department because of agitation and sweating. History shows she is currently being treated for depression with citalopram. She also takes tramadol for back pain. Her temperature is 38.6°C (101.5°F), the pulse is 108/min, the respirations are 18/min, and the blood pressure is 165/110 mm Hg. Physical examination shows hyperreflexia and mild tremors in all 4 extremities. Which of the following should be used in the next step of management for this patient?
- A. Diazepam
- B. Chlorpromazine
- C. Cyproheptadine
- D. Selegiline
- E. Discontinue tramadol and citalopram (Correct Answer)
Pharmacodynamic interaction mechanisms Explanation: ***Discontinue tramadol and citalopram***
- This patient presents with symptoms highly suggestive of **serotonin syndrome**, characterized by **agitation, sweating, hyperthermia, tachycardia, hypertension, hyperreflexia, and tremors**, stemming from the concomitant use of **citalopram (SSRI)** and **tramadol (serotonergic properties)**.
- The immediate priority in managing serotonin syndrome is to **discontinue all serotonergic agents** definitively, as continued exposure can worsen symptoms and lead to severe complications.
*Diazepam*
- While **benzodiazepines** like diazepam are often used to manage agitation and hyperreflexia in serotonin syndrome, they are **symptomatic treatments** and do not address the underlying cause.
- Their use would be **adjunctive to discontinuing the causative agents**, not the primary next step.
*Chlorpromazine*
- **Chlorpromazine** is an antipsychotic with **dopamine-blocking effects** and anticholinergic properties; it is **not indicated** for the treatment of serotonin syndrome.
- In fact, its use could **exacerbate certain symptoms** or lead to adverse effects due to its other pharmacological actions.
*Cyproheptadine*
- **Cyproheptadine** is a **serotonin antagonist** that can be used in some cases of severe serotonin syndrome to counteract the excessive serotonin activity.
- However, the **initial and most critical step** is to discontinue the offending medications before considering pharmacologic interventions like cyproheptadine, which is typically reserved for moderate to severe cases after initial drug cessation.
*Selegiline*
- **Selegiline** is a **monoamine oxidase B (MAO-B) inhibitor** that increases dopamine levels and, at higher doses, can also inhibit MAO-A, leading to increased serotonin.
- Administering another serotonergic agent would be **contraindicated** and potentially fatal in a patient experiencing serotonin syndrome.
Pharmacodynamic interaction mechanisms US Medical PG Question 9: An investigator is studying the effects of different drugs on the contraction of cardiomyocytes. The myocytes are able to achieve maximal contractility with the administration of drug A. The subsequent administration of drug B produces the response depicted in the graph shown. Which of the following drugs is most likely to produce a response similar to that of drug B?
- A. Albuterol
- B. Phenoxybenzamine
- C. Pindolol (Correct Answer)
- D. Isoproterenol
- E. Propranolol
Pharmacodynamic interaction mechanisms Explanation: ***Pindolol***
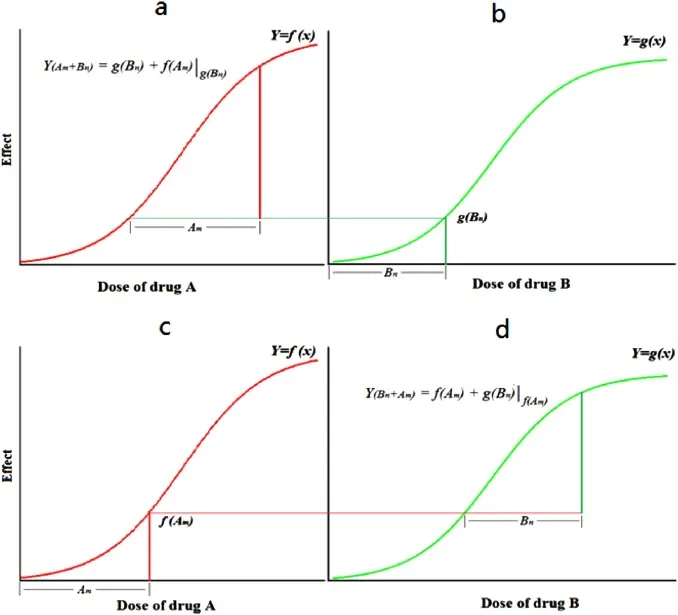
- The graph shows drug B reducing the maximal contractility achieved by drug A, suggesting it is a **partial agonist** or a **competitive antagonist** that can exert some intrinsic activity. Pindolol is a **beta-blocker** with **intrinsic sympathomimetic activity (ISA)**, meaning it can partially stimulate beta-receptors while blocking full agonists.
- This **partial agonism** allows pindolol to reduce the effect of a stronger agonist (like drug A, if it's a full beta-agonist) but still provide some baseline stimulation, thus decreasing the maximal response rather than completely abolishing it.
*Albuterol*
- Albuterol is a **selective beta-2 adrenergic agonist** primarily used as a bronchodilator.
- It would increase contractility if beta-2 receptors were present and acted upon, but it would not reduce the maximal contraction from an existing strong agonist.
*Phenoxybenzamine*
- Phenoxybenzamine is an **irreversible alpha-adrenergic antagonist**.
- It would not directly affect cardiac contractility which is primarily mediated by beta-adrenergic receptors, nor would it produce the depicted effect on contractility.
*Isoproterenol*
- Isoproterenol is a **non-selective beta-adrenergic agonist**.
- As a full agonist, it would increase contractility and could even be drug A if drug A is a beta-agonist, but it would not reduce the maximal response of an established agonist.
*Propranolol*
- Propranolol is a **non-selective beta-adrenergic antagonist** without intrinsic sympathomimetic activity (ISA).
- It would act as a **full competitive antagonist**, completely blocking the effects of drug A if drug A is a beta-agonist, thus reducing contractility much more significantly than depicted, potentially to baseline or below.
Pharmacodynamic interaction mechanisms US Medical PG Question 10: A 64-year-old man presents to the emergency department with acute onset of chest pain. He says the pain is substernal and radiates to his left arm. He has a history of hypertension, diabetes mellitus, erectile dysfunction, benign prostate hyperplasia, and panic disorder. He takes aspirin, lisinopril, metformin, sildenafil, prazosin, and citalopram. An electrocardiogram shows new ST-elevations in the lateral leads. He undergoes catherization, which reveals a complete blockage of the left circumflex artery. A stent is placed, and the patient is discharged with clopidogrel and isosorbide mononitrate. Five days later the patient presents to the emergency department complaining of fainting spells. The patient’s temperature is 97°F (37.2°C), blood pressure is 89/53 mmHg, and pulse is 90/min. Physical examination is unremarkable. An electrocardiogram reveals lateral Q waves without ST or T wave abnormalities. Which of the following is the most likely cause of the patient’s presentation?
- A. Stent thrombosis
- B. Fibrinous pericarditis
- C. Myocardial wall rupture
- D. Papillary muscle rupture
- E. Medication interaction (Correct Answer)
Pharmacodynamic interaction mechanisms Explanation: ***Medication interaction***
- The patient experienced **hypotension and fainting spells** after being prescribed **isosorbide mononitrate** (a nitrate) following his myocardial infarction. The patient also takes **sildenafil** (a PDE5 inhibitor) for erectile dysfunction, which when combined with nitrates can lead to severe and prolonged hypotension.
- Both **nitrates and sildenafil mediate nitric oxide (NO)-induced vasodilation**, leading to a synergistic effect on blood pressure reduction which caused his syncopal episodes.
*Stent thrombosis*
- This would typically present with a **recurrence of acute chest pain, ST-elevations, and signs of myocardial ischemia** due to re-occlusion of the stented artery.
- The patient's symptoms are primarily **fainting spells and hypotension**, without signs of recurrent ischemia on ECG (lateral Q waves indicate prior infarction, but no acute changes).
*Fibrinous pericarditis*
- This complication typically occurs **2-4 days post-MI** and presents with **pleuritic chest pain that is positional** (worse when lying flat, better when leaning forward) and can be associated with a pericardial friction rub.
- The patient's primary complaint is fainting spells and hypotension, not pleuritic chest pain.
*Myocardial wall rupture*
- A myocardial wall rupture is a catastrophic complication that typically presents with **sudden severe chest pain, profound hypotension, and often rapid death** due to cardiac tamponade.
- The patient's presentation of fainting spells without acute severe chest pain or immediate life-threatening collapse makes complete myocardial wall rupture less likely.
*Papillary muscle rupture*
- This complication primarily presents with acute onset of **severe mitral regurgitation**, leading to **acute pulmonary edema, dyspnea, and cardiogenic shock**.
- While hypotension can be present, the dominant symptoms are usually respiratory distress and signs of heart failure, which are not described in this patient's fainting spells.
More Pharmacodynamic interaction mechanisms US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.