Sodium channel blocking antiepileptics US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Sodium channel blocking antiepileptics. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Sodium channel blocking antiepileptics US Medical PG Question 1: A 7-year-old boy is brought to the physician because of spells of unresponsiveness and upward rolling of the eyes for 2 months. The episodes start abruptly and last a few seconds. During that time he does not hear anyone’s voice or make any purposeful movements. When the episodes end, he continues what he was doing before the spell. He does not lose his posture or fall to the ground. Episodes occur multiple times during the day. Physical examination shows no abnormal findings. An EEG following hyperventilation shows 3 Hz spike-and-slow-wave discharges. Which of the following is the most appropriate pharmacotherapy at this time?
- A. No pharmacotherapy at this time
- B. Ethosuximide (Correct Answer)
- C. Sodium valproate
- D. Oxcarbazepine
- E. Lamotrigine
Sodium channel blocking antiepileptics Explanation: ***Ethosuximide***
- The described clinical picture (brief unresponsiveness, eye-rolling, continuing activity afterward, frequent daily episodes, normal physical exam, and 3-Hz spike-and-slow-wave discharges on EEG during hyperventilation) is classic for **childhood absence epilepsy**.
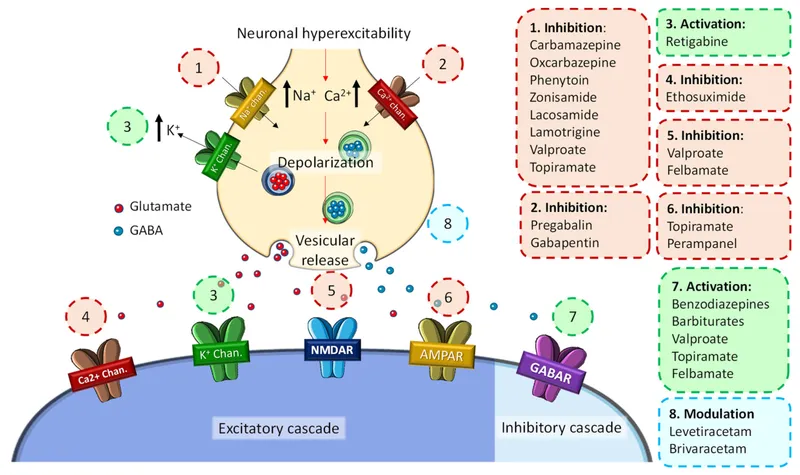
- **Ethosuximide** is the first-line and most effective treatment specifically for absence seizures due to its selective action on T-type calcium channels in the thalamus, which are implicated in the generation of absence seizures.
*No pharmacotherapy at this time*
- Leaving childhood absence epilepsy untreated can lead to significant impairments in learning, attention, and cognitive development due to the frequent, brief interruptions in consciousness.
- Given the clear diagnostic criteria including characteristic EEG findings and frequent episodes, initiating appropriate pharmacotherapy is medically indicated and crucial for the child's well-being.
*Sodium valproate*
- While **sodium valproate** is effective against absence seizures and has a broader spectrum of action against other seizure types, it is often considered a second-line agent for absence epilepsy due to potential side effects.
- Its use may be preferred if there are co-occurring generalized tonic-clonic seizures or if ethosuximide is not tolerated or effective, but for isolated absence seizures, ethosuximide has a better side effect profile.
*Oxcarbazepine*
- **Oxcarbazepine** is a sodium channel blocker primarily used for focal (partial onset) seizures and secondarily generalized tonic-clonic seizures.
- It is generally ineffective and can sometimes *worsen* absence seizures, making it an inappropriate choice for this diagnosis.
*Lamotrigine*
- **Lamotrigine** is a broad-spectrum antiepileptic drug effective for various seizure types, including focal, generalized tonic-clonic, and some forms of atypical absence seizures.
- While it can be used for absence seizures, it is generally considered a second-line or add-on therapy, especially when ethosuximide or valproate are ineffective or not tolerated, or if there are co-existing seizure types. It is not the most appropriate first-line choice for classic childhood absence epilepsy.
Sodium channel blocking antiepileptics US Medical PG Question 2: A 24-year-old man is brought to the emergency department because of violent jerky movements of his arms and legs that began 30 minutes ago. His father reports that the patient has a history of epilepsy. He is not responsive. Physical examination shows alternating tonic jerks and clonic episodes. There is blood in the mouth. Administration of intravenous lorazepam is begun. In addition, treatment with a second drug is started that alters the flow of sodium ions across neuronal membranes. The second agent administered was most likely which of the following drugs?
- A. Lamotrigine
- B. Phenobarbital
- C. Topiramate
- D. Carbamazepine
- E. Fosphenytoin (Correct Answer)
Sodium channel blocking antiepileptics Explanation: ***Fosphenytoin***
- This patient is experiencing **status epilepticus** as evidenced by prolonged tonic-clonic seizures. **Lorazepam** is the first-line short-acting benzodiazepine for acute seizure termination, but a second, longer-acting antiepileptic drug is needed for maintenance.
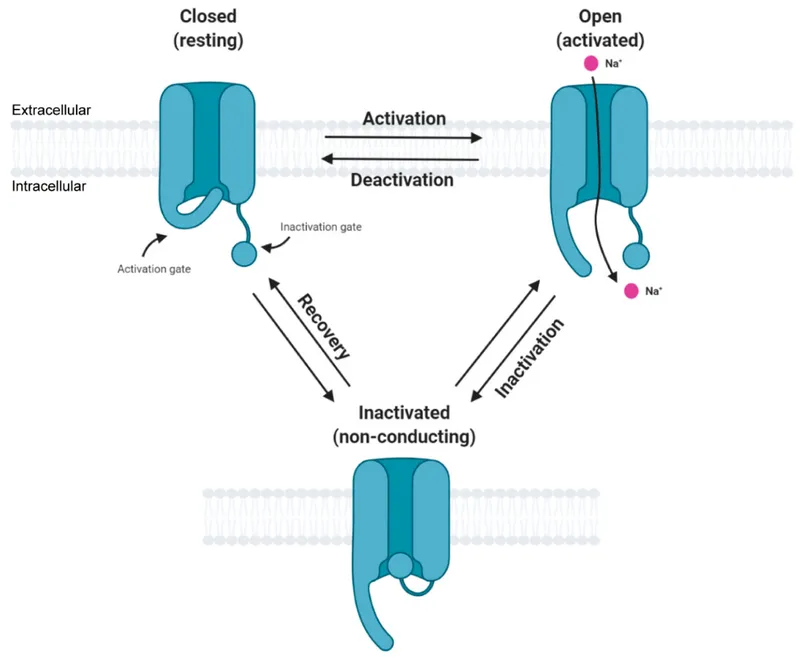
- **Fosphenytoin** is a prodrug of **phenytoin** that can be administered intravenously; **phenytoin** works by blocking **voltage-sensitive sodium channels**, thereby altering the flow of sodium ions and stabilizing neuronal membranes.
*Lamotrigine*
- While **lamotrigine** does block voltage-gated sodium channels, it is primarily used for **partial seizures** and **generalized tonic-clonic seizures** as a maintenance therapy, not typically as an acute treatment for status epilepticus.
- It requires **slow titration** due to the risk of severe skin reactions (e.g., Stevens-Johnson syndrome), making it unsuitable for immediate use in status epilepticus.
*Phenobarbital*
- **Phenobarbital** is an antiepileptic drug that enhances **GABAergic neurotransmission**, leading to neuronal hyperpolarization and reduced excitability. It is a very effective and older anticonvulsant.
- Although it can be used for status epilepticus, it acts primarily on GABA receptors, not directly on **sodium ion channels** as described in the question.
*Topiramate*
- **Topiramate** has multiple mechanisms of action, including blocking voltage-gated sodium channels and enhancing GABA activity, but it is typically used as a **maintenance therapy** for various seizure types.
- It is not a first-line agent for acute management of **status epilepticus** and its primary mechanism mentioned isn't restricted to sodium channel modulation as explicitly as phenytoin.
*Carbamazepine*
- **Carbamazepine** is a sodium channel blocker, similar to phenytoin, and is effective for **partial** and **tonic-clonic seizures**.
- However, it is primarily an **oral medication** and its slow absorption makes it inappropriate for acute intravenous treatment of status epilepticus.
Sodium channel blocking antiepileptics US Medical PG Question 3: A 6-year-old boy is brought to the physician because of a 2-week history of frequent episodes of unresponsiveness. During these episodes, he stares blankly, rhythmically nods his head, and does not respond to verbal stimulation for several seconds. Hyperventilation for 30 seconds precipitates an episode of unresponsiveness and head nodding that lasts for 7 seconds. He regains consciousness immediately afterward. An electroencephalogram shows 3-Hz spikes and waves. Which of the following best describes the mechanism of action of the most appropriate pharmacotherapy for this patient's condition?
- A. Inhibition of GABA reuptake into presynaptic neurons
- B. Increased frequency of GABAA channel opening
- C. Irreversible inhibition of GABA transaminase
- D. Increased duration of GABAA channel opening
- E. Blockade of thalamic T-type calcium channels (Correct Answer)
Sodium channel blocking antiepileptics Explanation: ***Blockade of thalamic T-type calcium channels***
- The patient's presentation with **staring spells**, rhythmic head nodding, and precipitation by **hyperventilation** is classic for **absence epilepsy**. The EEG findings of **3-Hz spikes and waves** confirm this diagnosis.
- **Ethosuximide** is the first-line treatment for absence seizures. It works by selectively blocking **T-type calcium channels** in the thalamus, which are crucial for generating the 3-Hz spike-and-wave discharges.
*Inhibition of GABA reuptake into presynaptic neurons*
- This mechanism of action is characteristic of **tiagabine**, an antiepileptic drug primarily used as an add-on therapy for **focal seizures**.
- While GABAergic mechanisms are involved in epilepsy, tiagabine is not a primary treatment for absence seizures and does not target the specific thalamic pathways involved.
*Increased frequency of GABAA channel opening*
- This is the mechanism of action of **benzodiazepines**, such as **lorazepam** or **diazepam**, which enhance the inhibitory effects of GABA.
- Benzodiazepines are typically used for acute seizure management (e.g., **status epilepticus**) or as adjunct therapy, but not as first-line monotherapy for absence seizures due to sedation and tolerance issues.
*Irreversible inhibition of GABA transaminase*
- This mechanism describes **vigabatrin**, an antiepileptic drug that increases GABA levels by inhibiting its breakdown.
- Vigabatrin is primarily used for **infantile spasms** and **refractory focal seizures**, and it is associated with a risk of **visual field defects**, making it unsuitable for absence epilepsy.
*Increased duration of GABAA channel opening*
- This mechanism is characteristic of **barbiturates**, such as **phenobarbital**, which also enhance GABAergic inhibition like benzodiazepines but by increasing the duration of chloride channel opening.
- Barbiturates are older antiepileptic drugs with significant side effects (e.g., sedation) and are generally not preferred for absence seizures.
Sodium channel blocking antiepileptics US Medical PG Question 4: A 19-year-old man with a history of generalized tonic-clonic seizures comes to the physician for a routine health maintenance examination. He is a known user of intravenous cocaine. His vital signs are within normal limits. Physical examination shows multiple hyperpigmented lines along the forearms. Oral examination shows marked overgrowth of friable, ulcerated gingival mucosa. Which of the following is the most likely cause of this patient's oral examination findings?
- A. Cyclosporine
- B. Lacosamide
- C. Carbamazepine
- D. Phenytoin (Correct Answer)
- E. Lamotrigine
Sodium channel blocking antiepileptics Explanation: ***Phenytoin***
- **Phenytoin** is a common cause of **gingival hyperplasia**, presenting with marked overgrowth of friable, ulcerated gingival mucosa due to its effect on fibroblast proliferation and collagen production.
- This medication is frequently used to manage **tonic-clonic seizures**, consistent with the patient's history.
*Cyclosporine*
- While **cyclosporine** can cause **gingival hyperplasia**, it is an **immunosuppressant** primarily used in organ transplantation or autoimmune conditions, which is not indicated in the patient's seizure history.
- The patient's presentation does not suggest any condition for which cyclosporine would be prescribed.
*Lacosamide*
- **Lacosamide** is an anticonvulsant that stabilizes hyperexcitable neuronal membranes, but it is **not typically associated with gingival hyperplasia**.
- Its known side effects are primarily neurological, such as dizziness, headache, and nausea.
*Carbamazepine*
- **Carbamazepine** is an anticonvulsant effective for focal and tonic-clonic seizures, but **gingival hyperplasia is a rare side effect** with this medication.
- More common side effects include dizziness, drowsiness, and bone marrow suppression.
*Lamotrigine*
- **Lamotrigine** is an anticonvulsant used for various seizure types, but **gingival hyperplasia is not a recognized side effect**.
- It is more commonly associated with skin rashes, including severe reactions like **Stevens-Johnson syndrome**.
Sodium channel blocking antiepileptics US Medical PG Question 5: A 30-year-old female with a history of epilepsy becomes pregnant. Her epilepsy has been well controlled by taking a medication that inhibits GABA transaminase and blocks voltage-gated sodium and calcium channels. Her obstetrician informs her that her epilepsy medication has been shown to have teratogenic effects. Of the following, which teratogenic effect is this woman's medication most likely to cause?
- A. Limb defects
- B. Neural tube defect (Correct Answer)
- C. Renal damage
- D. Ebstein's anomaly
- E. Discolored teeth
Sodium channel blocking antiepileptics Explanation: ***Neural tube defect***
- The medication described, which **inhibits GABA transaminase** and has multiple mechanisms including effects on voltage-gated channels, is **valproic acid** (valproate).
- **Valproic acid** is the antiepileptic drug with the **highest risk of neural tube defects** (e.g., spina bifida), with an incidence of approximately 1-2% when taken during pregnancy.
- This teratogenic effect occurs primarily during the first trimester and is believed to be due to interference with **folate metabolism** and **histone deacetylase inhibition**, which are crucial for proper neural tube closure.
- Folic acid supplementation is recommended for women of childbearing age taking valproate.
*Limb defects*
- **Limb defects** (e.g., phocomelia, limb reduction defects) are classically associated with **thalidomide** exposure during early pregnancy.
- While **phenytoin** (fetal hydantoin syndrome) can cause limb abnormalities including hypoplastic nails and distal phalanges, this is not the primary teratogenic concern with valproic acid.
*Renal damage*
- **Fetal renal damage** can be caused by medications such as **ACE inhibitors**, **ARBs**, and **NSAIDs** when taken during pregnancy.
- This is not a characteristic teratogenic effect of valproic acid or other antiepileptic medications.
*Ebstein's anomaly*
- **Ebstein's anomaly**, a congenital heart defect characterized by apical displacement of the tricuspid valve, is most notably associated with **lithium exposure** during the first trimester of pregnancy.
- This cardiac anomaly is not typically linked to valproic acid or other anticonvulsant medications.
*Discolored teeth*
- **Discolored teeth** (yellow-brown staining) and enamel hypoplasia are classic adverse effects of **tetracycline antibiotics** when administered during pregnancy (second and third trimesters) or early childhood.
- This effect is not associated with antiepileptic medications.
Sodium channel blocking antiepileptics US Medical PG Question 6: A neuroscientist is delivering a lecture on the electrophysiology of the brain. He talks about neuroreceptors which act as ion channels in the neurons. He mentions a specific receptor, which is both voltage-gated and ligand-gated ion channel. Which of the following receptors is most likely to be the one mentioned by the neuroscientist?
- A. NMDA receptor (Correct Answer)
- B. GABAA receptor
- C. AMPA receptor
- D. Nicotinic acetylcholine receptor
- E. Glycine receptor
Sodium channel blocking antiepileptics Explanation: ***NMDA receptor***
- The **NMDA receptor** is unique among ionotropic glutamate receptors as it functions as both a **ligand-gated** and **voltage-gated** ion channel.
- It requires both the binding of an excitatory neurotransmitter (like **glutamate**) and a sufficient **depolarization** of the postsynaptic membrane to remove a **magnesium ion (Mg2+) block** from its pore.
*GABAA receptor*
- The **GABAA receptor** is a **ligand-gated ion channel** that opens upon binding of the neurotransmitter **GABA**, leading to an influx of chloride ions and neuronal hyperpolarization.
- It is primarily responsible for **inhibitory synaptic transmission** in the central nervous system.
*AMPA receptor*
- The **AMPA receptor** is an ionotropic glutamate receptor that is primarily **ligand-gated**, opening swiftly upon binding of **glutamate** to allow sodium and potassium ion flow.
- While it contributes to depolarization, it is generally not considered to have a significant **voltage-gating** mechanism like the NMDA receptor.
*Nicotinic acetylcholine receptor*
- The **nicotinic acetylcholine receptor** is a **ligand-gated ion channel** that opens in response to the binding of **acetylcholine**, initiating fast excitatory synaptic transmission.
- It is **not voltage-gated** in the same manner as the NMDA receptor; its opening is primarily dependent on neurotransmitter binding.
*Glycine receptor*
- The **glycine receptor** is a **ligand-gated chloride channel** that mediates fast inhibitory synaptic transmission in the spinal cord and brainstem.
- Its activation by **glycine** leads to an influx of chloride ions, causing hyperpolarization, and it does not exhibit significant voltage-gating properties.
Sodium channel blocking antiepileptics US Medical PG Question 7: A 20-year-old woman presents to the emergency department with painful abdominal cramping. She states she has missed her menstrual period for 5 months, which her primary care physician attributes to her obesity. She has a history of a seizure disorder treated with valproic acid; however, she has not had a seizure in over 10 years and is no longer taking medications for her condition. She has also been diagnosed with pseudoseizures for which she takes fluoxetine and clonazepam. Her temperature is 98.0°F (36.7°C), blood pressure is 174/104 mmHg, pulse is 88/min, respirations are 19/min, and oxygen saturation is 98% on room air. Neurologic exam is unremarkable. Abdominal exam is notable for a morbidly obese and distended abdomen that is nontender. Laboratory studies are ordered as seen below.
Serum:
hCG: 100,000 mIU/mL
Urine:
Color: Amber
hCG: Positive
Protein: Positive
During the patient's evaluation, she experiences 1 episode of tonic-clonic motions which persist for 5 minutes. Which of the following treatments is most appropriate for this patient?
- A. Phenobarbital
- B. Magnesium (Correct Answer)
- C. Phenytoin
- D. Propofol
- E. Lorazepam
Sodium channel blocking antiepileptics Explanation: ***Magnesium***
- The patient's presentation with **painful abdominal cramping**, **elevated blood pressure (174/104 mmHg)**, **proteinuria**, a **positive hCG** (100,000 mIU/mL), and a **new-onset tonic-clonic seizure** strongly indicates **eclampsia**.
- **Magnesium sulfate** is the first-line treatment for seizure prophylaxis and management in patients with preeclampsia and eclampsia.
*Phenobarbital*
- While effective for seizure control, **phenobarbital** is a less preferred agent for eclampsia compared to magnesium sulfate.
- Its use in eclampsia is typically reserved for cases refractory to magnesium sulfate.
*Phenytoin*
- **Phenytoin** is not recommended as a first-line agent for eclamptic seizures, as magnesium sulfate has demonstrated superior efficacy.
- It carries a risk of adverse effects such as **cardiac arrhythmias** and **hypotension**, especially with rapid administration.
*Propofol*
- **Propofol** is an anesthetic and sedative used for continuous seizure control, often in status epilepticus, but is not the primary treatment for eclampsia.
- Its use can lead to significant **respiratory depression** and **hypotension**, requiring close monitoring and intubation.
*Lorazepam*
- Although **lorazepam** is a benzodiazepine used to acutely stop seizures, it is not the preferred agent for eclampsia.
- Benzodiazepines may cause **sedation** and **respiratory depression**, and their efficacy in eclampsia is inferior to magnesium sulfate.
Sodium channel blocking antiepileptics US Medical PG Question 8: A 45-year-old homeless man presents to the emergency department with a 1-week history of an intensely pruritic, red rash on his hands, wrists, and finger webs. The itching is worse at night. Physical examination reveals small, erythematous papules and burrows. A topical drug with which of the following mechanisms of action is most likely to be effective in treating this condition?
- A. Increase in keratinocyte turnover
- B. Inhibition of histamine-1 receptors
- C. Decrease in peptidoglycan synthesis
- D. Inhibition of nuclear factor-κB
- E. Binding to sodium channels (Correct Answer)
Sodium channel blocking antiepileptics Explanation: ***Binding to sodium channels***
- The clinical presentation of **intensely pruritic rash**, especially worse at night, with **burrows** on hands, wrists, and finger webs, is highly suggestive of **scabies**.
- Scabies is caused by the mite *Sarcoptes scabiei*, and treatment often involves **permethrin**, which acts by **binding to sodium channels** in the mite's nervous system, leading to paralysis and death.
*Increase in keratinocyte turnover*
- This mechanism of action is characteristic of drugs used to treat conditions like **psoriasis**, where the goal is to reduce rapid skin cell proliferation.
- It is not relevant for parasitic infestations like scabies, which require an agent to directly kill the mites.
*Inhibition of histamine-1 receptors*
- Antihistamines, which block H1 receptors, are used to alleviate **pruritus** associated with allergic reactions or other inflammatory skin conditions.
- While they can help with the *symptom* of itching, they do not address the underlying *cause* of scabies (the mite infestation itself).
*Decrease in peptidoglycan synthesis*
- This mechanism is characteristic of **antibiotics** like **penicillins** and **cephalosporins**, which target the bacterial cell wall.
- It is effective against bacterial infections but has no utility in treating parasitic infestations like scabies, which are caused by arthropods, not bacteria.
*Inhibition of nuclear factor-κB*
- **NF-κB** is a protein complex that controls **transcription of DNA**, cytokine production, and cell survival, and its inhibition is often targeted in **inflammatory diseases** or cancers.
- This mechanism is not directly involved in the eradication of scabies mites.
Sodium channel blocking antiepileptics US Medical PG Question 9: A 56-year-old man comes to the physician for a follow-up examination. One month ago, he was diagnosed with a focal seizure and treatment with a drug that blocks voltage-gated sodium channels was begun. Today, he reports that he has not had any abnormal body movements, but he has noticed occasional double vision. His serum sodium is 132 mEq/L, alanine aminotransferase is 49 U/L, and aspartate aminotransferase is 46 U/L. This patient has most likely been taking which of the following drugs?
- A. Carbamazepine (Correct Answer)
- B. Topiramate
- C. Lamotrigine
- D. Gabapentin
- E. Levetiracetam
Sodium channel blocking antiepileptics Explanation: ***Carbamazepine***
- This patient's symptoms of **double vision (diplopia)**, **hyponatremia** (serum sodium 132 mEq/L), and mild elevation in **liver enzymes** (ALT 49 U/L, AST 46 U/L) are classic side effects of carbamazepine.
- Carbamazepine blocks **voltage-gated sodium channels**, which is consistent with the initial treatment description for focal seizures.
- Hyponatremia occurs due to **SIADH (syndrome of inappropriate antidiuretic hormone secretion)**, a well-known adverse effect.
*Topiramate*
- Common side effects include **cognitive slowing**, **paresthesias**, and **kidney stones**, which are not reported by the patient.
- While it can cause weight loss and metabolic acidosis, **diplopia** and **hyponatremia** are not typical adverse effects.
*Lamotrigine*
- Also blocks voltage-gated sodium channels but has a different side effect profile.
- The most significant and potentially life-threatening side effect is a severe skin rash known as **Stevens-Johnson syndrome (SJS)** or toxic epidermal necrolysis (TEN).
- It does not commonly cause **diplopia** or significant **hyponatremia**.
*Gabapentin*
- Primarily acts by binding to the **α2δ subunit of voltage-gated calcium channels** and is NOT a sodium channel blocker.
- Side effects typically include **dizziness**, **somnolence**, and peripheral edema, not the constellation of symptoms presented.
*Levetiracetam*
- Its mechanism of action involves binding to the **synaptic vesicle protein 2A (SV2A)**, a unique target, and it is NOT a voltage-gated sodium channel blocker.
- Common side effects include behavioral changes (**irritability**, **aggression**) and **somnolence**, but not diplopia or hyponatremia.
Sodium channel blocking antiepileptics US Medical PG Question 10: A 75-year-old man with a seizure disorder is brought to the emergency department by a friend because of progressive confusion over the past two weeks. He is unable to provide any history. His vital signs are within normal limits. He appears lethargic and is only oriented to person. Oral mucosa is moist. There is no jugular venous distention. A basic metabolic panel shows a serum sodium concentration of 115 mEq/L but is otherwise normal. Serum osmolality is low and antidiuretic hormone level is elevated. X-ray of the chest shows no abnormalities. Which of the following is the most likely cause of this patient’s hyponatremia?
- A. Aldosterone deficiency
- B. Medication effect (Correct Answer)
- C. Low cardiac output
- D. Insulin deficiency
- E. Excess cortisol
Sodium channel blocking antiepileptics Explanation: ***Medication effect***
- This patient's **hyponatremia** with **appropriately low serum osmolality** and **elevated antidiuretic hormone (ADH)** levels, in the absence of signs of hypovolemia or fluid overload, points to the **syndrome of inappropriate ADH secretion (SIADH)**.
- Many medications, including anti-epileptic drugs like carbamazepine or oxcarbazepine (commonly used for seizure disorders), as well as selective serotonin reuptake inhibitors (SSRIs), can cause SIADH.
*Aldosterone deficiency*
- **Aldosterone deficiency** would likely lead to **hyperkalemia** and metabolic acidosis, which are not mentioned in the basic metabolic panel as being abnormal.
- While it can cause hyponatremia due to inability to retain sodium, the elevated ADH level with normal volume status points away from primary aldosterone deficiency.
*Low cardiac output*
- **Low cardiac output** can lead to hyponatremia by decreased renal perfusion and activation of the renin-angiotensin-aldosterone system and ADH release.
- However, this patient has **normal vital signs** and **no jugular venous distention**, making significant low cardiac output and resultant hypovolemia less likely.
*Insulin deficiency*
- **Insulin deficiency** (as seen in uncontrolled diabetes) typically leads to **hyperglycemia** and can cause a **pseudohyponatremia** due to osmotic effects, or true hyponatremia due to polyuria and volume depletion.
- The basic metabolic panel is otherwise normal, suggesting no significant hyperglycemia or electrolyte abnormalities consistent with insulin deficiency.
*Excess cortisol*
- **Excess cortisol** (Cushing's syndrome) typically leads to **hyperglycemia**, hypertension, and features of fat redistribution, muscular weakness, and thin skin, none of which are detailed here.
- It does not directly cause hyponatremia; conversely, cortisol has some mineralocorticoid effects and typically opposes ADH action, so severe excess would more likely cause hypernatremia or normal sodium levels.
More Sodium channel blocking antiepileptics US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.