Opioid analgesics US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Opioid analgesics. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Opioid analgesics US Medical PG Question 1: A 17-year-old male presents with altered mental status. He was recently admitted to the hospital due to a tibial fracture suffered while playing soccer. His nurse states that he is difficult to arouse. His temperature is 98.6 deg F (37 deg C), blood pressure is 130/80 mm Hg, pulse is 60/min, and respirations are 6/min. Exam is notable for pinpoint pupils and significant lethargy. Which of the following describes the mechanism of action of the drug likely causing this patient's altered mental status?
- A. Neuronal hyperpolarization due to sodium influx
- B. Neuronal depolarization due to sodium efflux
- C. Neuronal depolarization due to potassium influx
- D. Neuronal hyperpolarization due to potassium efflux (Correct Answer)
- E. Neuronal hyperpolarization due to chloride influx
Opioid analgesics Explanation: ***Neuronal hyperpolarization due to potassium efflux***
- The patient's symptoms of **altered mental status**, **pinpoint pupils**, and **respiratory depression** are classic for **opioid overdose**.
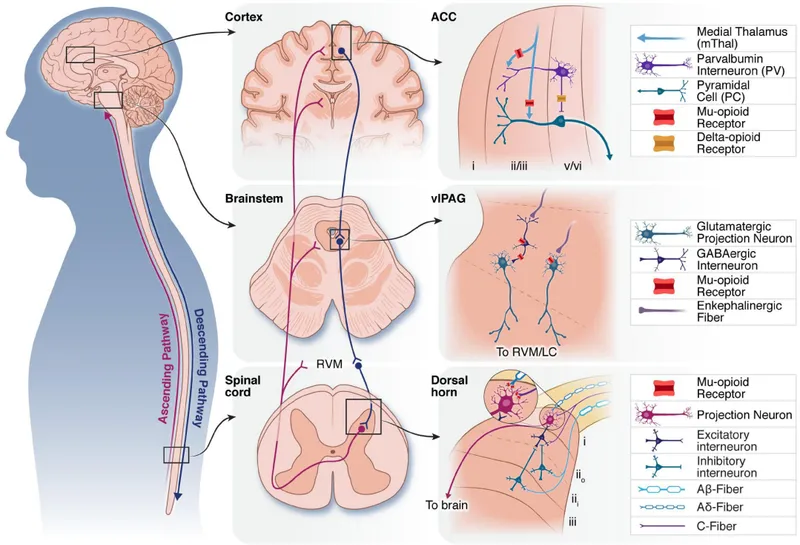
- Opioids act by binding to opioid receptors (mu, delta, kappa), which are **G-protein coupled receptors**. Activation of these receptors leads to **potassium efflux** and **calcium influx inhibition**, causing neuronal hyperpolarization and reduced neuronal excitability.
*Neuronal hyperpolarization due to sodium influx*
- **Sodium influx** typically causes depolarization, not hyperpolarization, making this option inconsistent with the mechanism of inducing neuronal inhibition.
- Hyperpolarization usually involves outward positive current (like potassium efflux) or inward negative current (like chloride influx).
*Neuronal depolarization due to sodium efflux*
- **Sodium efflux** (e.g., via the Na+/K+-ATPase) is crucial for maintaining resting membrane potential, but it does not directly lead to depolarization as described here.
- Depolarization is commonly associated with **sodium influx**, not efflux, causing the membrane potential to become more positive.
*Neuronal depolarization due to potassium influx*
- **Potassium influx** would make the cell less negative inside (depolarization), but this is not the primary mechanism of action for opioids.
- Opioids primarily cause **hyperpolarization** and reduced excitability, making this mechanism incorrect for the observed clinical picture caused by opioid overdose.
*Neuronal hyperpolarization due to chloride influx*
- While **chloride influx** does cause neuronal hyperpolarization (e.g., via GABA-A receptor activation by benzodiazepines), this is the mechanism for **GABAergic drugs**, not opioids.
- Opioids primarily achieve hyperpolarization through **potassium efflux**.
Opioid analgesics US Medical PG Question 2: A 32-year-old homeless woman is brought to the emergency department by ambulance 30 minutes after the police found her on the sidewalk. On arrival, she is unresponsive. Her pulse is 76/min, respirations are 6/min, and blood pressure is 110/78 mm Hg. Examination shows cool, dry skin. The pupils are pinpoint and react sluggishly to light. Intravenous administration of a drug is initiated. Two minutes after treatment is started, the patient regains consciousness and her respirations increase to 12/min. The drug that was administered has the strongest effect on which of the following receptors?
- A. Ryanodine receptor
- B. 5-HT2A receptor
- C. M1 receptor
- D. GABAA receptor
- E. μ-receptor (Correct Answer)
Opioid analgesics Explanation: ***μ-receptor***
- The patient's presentation with **unresponsiveness, pinpoint pupils, and respiratory depression** is classic for an **opioid overdose**.
- The rapid reversal of symptoms after drug administration indicates that the drug was an **opioid antagonist** like **naloxone**, which primarily acts on **μ-opioid receptors**.
*Ryanodine receptor*
- These receptors are primarily involved in **calcium release** from the sarcoplasmic reticulum in muscle cells, crucial for muscle contraction.
- They are targeted by drugs used in conditions like **malignant hyperthermia**, which is not indicated here.
*5-HT2A receptor*
- This receptor is a subtype of **serotonin receptors** and is a target for **antipsychotics** and some **hallucinogens**.
- While serotonin syndrome can cause altered mental status, it typically presents with **hyperthermia, myoclonus, and hypertension**, which are not seen in this patient.
*M1 receptor*
- These are **muscarinic acetylcholine receptors** found in the central nervous system and autonomic ganglia.
- Drugs acting on M1 receptors are involved in conditions like **Alzheimer's disease** (cholinesterase inhibitors) or **motion sickness** (anticholinergics), and are not relevant to opioid overdose.
*GABAA receptor*
- This receptor is the primary target for **benzodiazepines** and **barbiturates**, which cause central nervous system depression.
- While these drugs can cause respiratory depression and unresponsiveness, they typically do not cause **pinpoint pupils**, a hallmark of opioid overdose.
Opioid analgesics US Medical PG Question 3: A 35-year-old male is picked up by paramedics presenting with respiratory depression, pupillary constriction, and seizures. Within a few minutes, the male dies. On autopsy, fresh tracks marks are seen on both arms. Administration of which of the following medications would have been appropriate for this patient?
- A. Methadone
- B. Flumazenil
- C. Bupropion
- D. Naloxone (Correct Answer)
- E. Diazepam
Opioid analgesics Explanation: ***Naloxone***
- The patient's presentation with **respiratory depression**, **pupillary constriction**, and **fresh track marks** is highly indicative of an **opioid overdose**.
- **Naloxone** is a potent **opioid receptor antagonist** that rapidly reverses the effects of opioid overdose, including respiratory depression.
*Methadone*
- **Methadone** is a **long-acting opioid agonist** used for pain management and **opioid dependence treatment**.
- Administering methadone would worsen an opioid overdose by increasing the opioid effect, potentially deepening respiratory depression.
*Flumazenil*
- **Flumazenil** is an **antidote for benzodiazepine overdose**, acting as a competitive antagonist at the GABA-A receptor.
- It would not be effective in reversing an opioid overdose, as the patient's symptoms are not consistent with benzodiazepine intoxication.
*Bupropion*
- **Bupropion** is an **antidepressant** and **smoking cessation aid** that works by inhibiting the reuptake of norepinephrine and dopamine.
- It has no role in the acute management of opioid overdose and would not address the life-threatening respiratory depression.
*Diazepam*
- **Diazepam** is a **benzodiazepine** that has sedative, anxiolytic, anticonvulsant, and muscle relaxant properties.
- While it could address seizures, it would exacerbate the underlying respiratory depression in an opioid overdose.
Opioid analgesics US Medical PG Question 4: A 42-year-old man is discovered unconscious by local police while patrolling in a park. He is unresponsive to stimulation. Syringes were found scattered around him. His heart rate is 70/min and respiratory rate is 6/min. Physical examination reveals a disheveled man with track marks on both arms. His glasgow coma scale is 8. Pupillary examination reveals miosis. An ambulance is called and a reversing agent is administered. Which of the following is most accurate regarding the reversal agent most likely administered to this patient?
- A. Works on dopamine receptors
- B. Has a short half-life
- C. Can be given per oral
- D. Results in acute withdrawal (Correct Answer)
- E. Is a non-competitive inhibitor
Opioid analgesics Explanation: ***Results in acute withdrawal***
- The patient's presentation (unconscious, track marks, miosis, bradypnea) is characteristic of **opioid overdose**. The reversal agent, **naloxone**, rapidly displaces opioids from their receptors, leading to an abrupt onset of withdrawal symptoms.
- **Acute opioid withdrawal** can manifest with symptoms like nausea, vomiting, diarrhea, muscle cramps, and agitation, as the body suddenly lacks the opioid-induced suppression.
- This is the **most clinically significant** characteristic of naloxone in the acute overdose setting, as it explains the immediate physiological response patients experience.
*Works on dopamine receptors*
- **Naloxone** primarily acts as an **opioid receptor antagonist**, particularly at the mu-opioid receptor.
- It does not significantly interact with or exert its primary effects through **dopamine receptors**.
*Has a short half-life*
- While this statement is **factually true** (naloxone has a half-life of 30-81 minutes), it describes a **pharmacokinetic property** rather than a characteristic of its reversal mechanism.
- The question asks about the reversal agent in the context of immediate administration, where the **acute precipitation of withdrawal** is the most defining and immediate clinical consequence.
- The short half-life is clinically relevant for monitoring (patients may re-sedate), but it is not the most accurate statement regarding what happens when the reversal agent is administered.
*Can be given per oral*
- Although **naloxone** can be administered orally, its **bioavailability via the oral route is very low** (less than 3%) due to extensive first-pass metabolism.
- For acute overdose reversal, it is typically administered via intravenous, intramuscular, subcutaneous, or intranasal routes for rapid and effective absorption.
*Is a non-competitive inhibitor*
- **Naloxone** is a **competitive antagonist** of opioid receptors, meaning it competes with opioids for binding sites.
- It does not bind to an allosteric site to reduce the opioid's efficiency (non-competitive inhibition); rather, it directly blocks the receptor.
Opioid analgesics US Medical PG Question 5: A 25-year-old man comes to the physician because of an 8-hour history of painful leg cramping, runny nose, chills, diarrhea, and abdominal pain. Examination shows cool, damp skin with piloerection. The pupils are 7 mm in diameter and equal in size. Deep tendon reflexes are 3+ bilaterally. The diagnosis of opioid withdrawal is made. After the patient is stabilized, the physician initiates a withdrawal regimen with methadone. Which of the following characteristics makes this drug a suitable substance for the treatment of this patient's addiction?
- A. Rapid onset of action
- B. Low tolerance potential
- C. Long elimination half-life (Correct Answer)
- D. Low dependence risk
- E. Limited potency
Opioid analgesics Explanation: ***Long elimination half-life***
- **Methadone's long half-life** allows for steady drug levels, preventing the rapid fluctuations that trigger severe withdrawal symptoms.
- This characteristic enables **once-daily dosing**, simplifying treatment and reducing the likelihood of illicit drug-seeking behavior.
*Rapid onset of action*
- While methadone does have a relatively quick onset, it's not its primary advantage in **opioid addiction treatment**.
- **Buprenorphine** often has a faster onset and is used in a different capacity for induction of treatment.
*Low tolerance potential*
- **Methadone** is an opioid agonist and, like other opioids, patients can develop **tolerance** to its effects over time.
- Its utility in addiction treatment comes from its ability to stabilize opioid receptors, not from a lack of tolerance development.
*Low dependence risk*
- **Methadone** is an opioid and carries a significant risk of **physical dependence**.
- The goal of methadone maintenance is to manage this dependence in a controlled medical setting, reducing harm associated with illicit opioid use.
*Limited potency*
- **Methadone** is a potent opioid, similar in potency to morphine, which contributes to its effectiveness in managing severe withdrawal symptoms and cravings.
- Its high potency is a key factor in its therapeutic benefit, not a limitation.
Opioid analgesics US Medical PG Question 6: A 27-year-old homeless man presents to the emergency department with abdominal pain and vomiting. He has a known history of intravenous drug use and has been admitted to the hospital several times before. On physical examination his temperature is 99°F (37.2°C), blood pressure is 130/85 mmHg, pulse is 90/min, respirations are 19/min, and pulse oximetry is 99% on room air. The patient is in obvious discomfort. There is increased salivation and lacrimation. Pupils are reactive to light and 5 mm bilaterally. Cardiopulmonary exam is unremarkable. There is diffuse abdominal tenderness to palpation with no rebound or guarding. Which of the following interventions would have prevented this patient’s current condition?
- A. Naltrexone
- B. Buprenorphine (Correct Answer)
- C. Lorazepam
- D. Naloxone
- E. Bupropion
Opioid analgesics Explanation: ***Buprenorphine***
- This patient is presenting with symptoms consistent with **opioid withdrawal** (abdominal pain, vomiting, increased salivation, lacrimation). **Buprenorphine** is used for **opioid dependence treatment** as it's a **partial opioid agonist** that helps manage withdrawal symptoms and cravings, thus preventing acute withdrawal episodes.
- By stabilizing opioid receptors, buprenorphine, often combined with naloxone (Suboxone), reduces the risk of relapse and prevents the cycle of **intravenous drug use** that leads to withdrawal.
*Naltrexone*
- **Naltrexone** is an **opioid antagonist** used to prevent relapse in individuals who have achieved abstinence from opioids. It blocks the effects of opioids.
- However, administering naltrexone to someone actively using opioids or in withdrawal would precipitate or worsen withdrawal symptoms, making it unsuitable for preventing this acute presentation.
*Lorazepam*
- **Lorazepam** is a **benzodiazepine** primarily used to treat **anxiety**, **insomnia**, and **seizures**, and it is often used in **alcohol withdrawal**.
- While it can help manage some anxiety associated with opioid withdrawal, it does not address the underlying opioid dependence or prevent the physical symptoms of withdrawal itself, nor does it prevent the underlying cause of withdrawal which is abstinence from opioids.
*Naloxone*
- **Naloxone** is a potent, short-acting **opioid antagonist** used to **reverse opioid overdose** by rapidly displacing opioids from receptors.
- It would not prevent withdrawal; in fact, administering naloxone to an opioid-dependent individual would acutely precipitate severe withdrawal.
*Bupropion*
- **Bupropion** is an **antidepressant** that also aids in **smoking cessation**. It works by inhibiting the reuptake of norepinephrine and dopamine.
- It has no role in the prevention or treatment of opioid withdrawal and would not have altered this patient's current condition.
Opioid analgesics US Medical PG Question 7: 2 hours after being admitted to the hospital because of a fracture of the right ankle, a 75-year-old man continues to complain of pain despite treatment with acetaminophen and ibuprofen. He has a history of dementia and cannot recall his medical history. The presence of which of the following features would most likely be a reason to avoid treatment with morphine in this patient?
- A. Severe hypertension
- B. Persistent cough
- C. Biliary tract dysfunction
- D. Tachypnea (Correct Answer)
- E. Watery diarrhea
Opioid analgesics Explanation: ***Tachypnea***
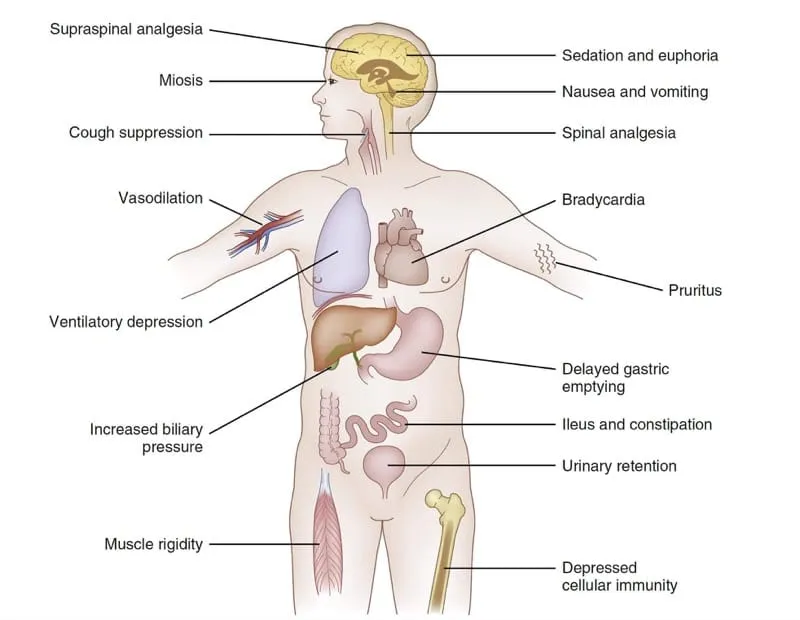
- **Tachypnea** (increased respiratory rate) can indicate underlying **respiratory compromise**, making morphine use risky due to its potential for **respiratory depression**.
- In a 75-year-old with a fracture and possible underlying health issues, exacerbating respiratory distress with opioids could be dangerous.
*Severe hypertension*
- While morphine can cause **hypotension** due to vasodilation, it is not typically contraindicated in severe hypertension.
- In fact, the hypotensive effect of morphine can sometimes be beneficial in conditions like **acute pulmonary edema** associated with hypertension.
*Persistent cough*
- Morphine is known to have **antitussive effects**, meaning it can help suppress a cough.
- Therefore, a persistent cough would more likely be a reason *to use* morphine, rather than avoid it, especially if the cough is non-productive and distressing.
*Biliary tract dysfunction*
- Morphine can cause **spasm of the sphincter of Oddi**, leading to increased pressure in the biliary tract and potentially exacerbating pain in patients with biliary dysfunction.
- However, this is usually a concern for patients with pre-existing biliary colic or pancreatitis, and not a primary contraindication in acute pain management unless other safer alternatives are available.
*Watery diarrhea*
- Opioids like morphine are well-known to cause **constipation** by slowing gut motility, due to their action on mu-opioid receptors in the enteric nervous system.
- Therefore, watery diarrhea would not be a reason to avoid morphine; in some cases, the constipating effect could even be considered beneficial.
Opioid analgesics US Medical PG Question 8: A 21-year-old man with a recent history of traumatic right femur fracture status post open reduction and internal fixation presents for follow-up. The patient says his pain is controlled with the oxycodone but he says he has been severely constipated the past 4 days. No other past medical history. Current medications are oxycodone and ibuprofen. The patient is afebrile and vital signs are within normal limits. On physical examination, surgical incision is healing well. Which of the following is correct regarding the likely role of opiates in this patient’s constipation?
- A. Opiates decrease the sympathetic activity of the gut wall
- B. Opiates increase the production and secretion of pancreatic digestive enzymes
- C. Opiates increase fluid absorption from the lumen leading to hard stools (Correct Answer)
- D. Opiates cause rapid gastrointestinal transit
- E. Opiates activate the excitatory neural pathways in the gut
Opioid analgesics Explanation: ***Opiates increase fluid absorption from the lumen leading to hard stools***
- Opiates act on **opioid receptors** in the GI tract, increasing **fluid absorption** and decreasing secretion, which makes stools drier and harder.
- This effect contributes significantly to **opioid-induced constipation** (OIC) by slowing stool transit and making defecation difficult.
*Opiates decrease the sympathetic activity of the gut wall*
- Opiates primarily affect the **parasympathetic nervous system** and enteric nervous system, rather than directly decreasing sympathetic activity.
- Their main impact on motility is to **decrease acetylcholine release**, which reduces gut contractions.
*Opiates increase the production and secretion of pancreatic digestive enzymes*
- Opiates are known to **decrease pancreatic enzyme secretion**, not increase it.
- This effect is not a primary mechanism for opioid-induced constipation.
*Opiates cause rapid gastrointestinal transit*
- Opiates actually **slow down gastrointestinal transit** by disrupting propulsive contractions and increasing non-propulsive segmental contractions.
- This delayed transit time is a major contributor to constipation.
*Opiates activate the excitatory neural pathways in the gut*
- Opiates typically **inhibit excitatory neural pathways** in the gut, particularly those mediated by acetylcholine, which reduces smooth muscle contractions.
- Their action leads to reduced peristalsis and overall decreased gut motility.
Opioid analgesics US Medical PG Question 9: A 40-year-old woman with a recent history of carcinoma of the breast status post mastectomy and adjuvant chemotherapy one week ago presents for follow-up. She reports adequate pain control managed with the analgesic drug she was prescribed. Past medical history is significant for hepatitis C and major depressive disorder. The patient denies any history of smoking or alcohol use but says she is currently using intravenous heroin and has been for the past 10 years. However, she reports that she has been using much less heroin since she started taking the pain medication, which is confirmed by the toxicology screen. Which of the following is the primary mechanism of action of the analgesic drug she was most likely prescribed?
- A. Pure antagonist at opioid receptors
- B. Pure agonist at the µ-opioid receptor (Correct Answer)
- C. Inhibits prostaglandin synthesis
- D. Mixed agonist-antagonist at opioid receptors
- E. Central action via blockade of serotonin reuptake
Opioid analgesics Explanation: ***Pure agonist at the µ-opioid receptor***
- Opioid analgesics, commonly prescribed for **post-mastectomy pain** and cancer-related pain, primarily exert their effects by acting as **pure agonists at the µ-opioid receptor**.
- This activation leads to profound **analgesia** by modulating pain perception and emotional response to pain in the central nervous system.
*Pure antagonist at opioid receptors*
- A **pure antagonist** would block opioid receptors and **reverse** the effects of opioid agonists, not provide analgesia.
- Such drugs are used to treat **opioid overdose** (e.g., naloxone) or to manage addiction by preventing opioid effects.
*Inhibits prostaglandin synthesis*
- This is the mechanism of action for **NSAIDs** (non-steroidal anti-inflammatory drugs), which primarily treat **mild to moderate pain** and inflammation.
- NSAIDs are generally insufficient for severe **post-surgical** or **cancer pain** of the magnitude experienced by this patient.
*Mixed agonist-antagonist at opioid receptors*
- Mixed agonist-antagonists provide analgesia by acting as agonists at some opioid receptors while acting as antagonists at others (e.g., **buprenorphine**).
- While they can provide pain relief, their use in acute severe pain is often limited, and they can sometimes **precipitate withdrawal** in patients chronically using full opioid agonists.
*Central action via blockade of serotonin reuptake*
- This is the primary mechanism of action for **antidepressants** (SSRIs) and some drugs used for **neuropathic pain** (e.g., tramadol with additional opioid action).
- While some antidepressants have analgesic properties, this mechanism alone is not typically the primary one for the potent pain relief needed post-mastectomy, which usually requires an **opioid**.
Opioid analgesics US Medical PG Question 10: A 36-year-old man is admitted to the hospital for treatment of burn wounds on his upper extremities. Analgesic therapy with an opioid drug is begun. Shortly after, the patient develops chills, diaphoresis, nausea, and abdominal pain. On further questioning, the patient reports that he has been smoking opium at home to help him ""deal with the depression and pain.” This patient was most likely given which of the following opioid drugs?
- A. Butorphanol (Correct Answer)
- B. Oxycodone
- C. Morphine
- D. Fentanyl
- E. Hydrocodone
Opioid analgesics Explanation: ***Butorphanol***
- **Butorphanol** is a **mixed opioid agonist-antagonist** that acts as a **kappa (κ) receptor agonist** and **mu (μ) receptor antagonist/partial agonist**.
- In opioid-dependent patients who use **mu receptor agonists** (like opium), butorphanol can precipitate **acute opioid withdrawal** by displacing full agonists from mu receptors and blocking their effects.
- The patient's symptoms of chills, diaphoresis, nausea, and abdominal pain are classic signs of **acute opioid withdrawal syndrome**.
*Oxycodone*
- **Oxycodone** is a **full mu opioid receptor agonist** and would not precipitate withdrawal in an opioid-dependent patient.
- Administering oxycodone would provide continued mu receptor stimulation, potentially alleviating withdrawal symptoms or maintaining the patient's opioid dependence.
*Morphine*
- **Morphine** is a **full mu opioid receptor agonist** and would not cause withdrawal in an opioid-dependent individual.
- It would continue to stimulate mu opioid receptors, providing analgesia and preventing withdrawal symptoms.
*Fentanyl*
- **Fentanyl** is a potent **full mu opioid receptor agonist** and would provide continued opioid receptor stimulation.
- Its administration would prevent withdrawal and provide effective analgesia in an opioid-tolerant patient.
*Hydrocodone*
- **Hydrocodone** is a **full mu opioid receptor agonist** and would not induce withdrawal symptoms.
- Like other full agonists, it would continue mu receptor activation, providing analgesia without precipitating withdrawal.
More Opioid analgesics US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.