Non-opioid analgesics US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Non-opioid analgesics. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Non-opioid analgesics US Medical PG Question 1: A 56-year-old postmenopausal woman comes to the physician because of a 6-month history of worsening pain and swelling in her left knee. She has a history of peptic ulcer disease for which she takes cimetidine. Examination shows palpable crepitus and limited range of motion of the left knee. Which of the following is the most appropriate pharmacotherapy for this patient’s symptoms?
- A. Acetylsalicylic acid
- B. Diclofenac
- C. Meloxicam
- D. Celecoxib (Correct Answer)
- E. Ketorolac
Non-opioid analgesics Explanation: ***Celecoxib***
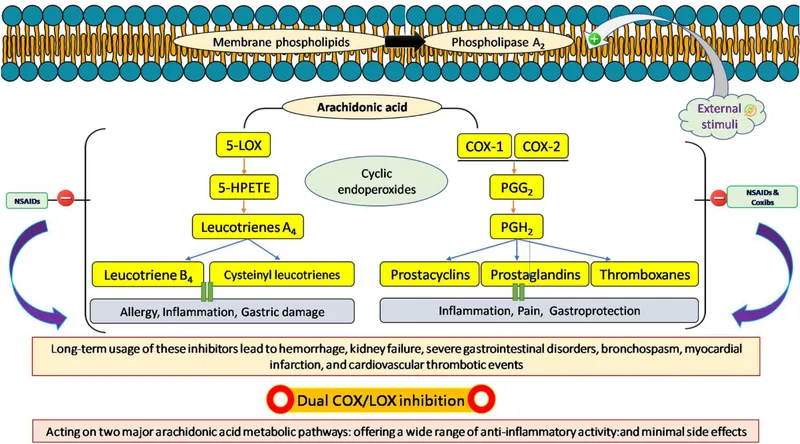
- This patient suffers from **osteoarthritis** (evidenced by her age, postmenopausal status, knee pain, crepitus, and limited range of motion) and has a history of **peptic ulcer disease (PUD)**. **Celecoxib** is a **COX-2 selective NSAID**, which reduces the risk of gastrointestinal side effects compared to non-selective NSAIDs.
- Given her history of PUD, a COX-2 selective NSAID is the most appropriate choice to manage her pain while minimizing the risk of a PUD exacerbation or bleed.
*Acetylsalicylic acid*
- **Aspirin** (acetylsalicylic acid) is a non-selective NSAID and would pose a significant risk of **gastrointestinal bleeding** or ulcer exacerbation in a patient with a history of **peptic ulcer disease**.
- While it has anti-inflammatory properties, its adverse effect profile makes it unsuitable for this patient's chronic pain management.
*Diclofenac*
- **Diclofenac** is a **non-selective NSAID**, meaning it inhibits both COX-1 and COX-2 enzymes.
- Due to its inhibition of COX-1, it carries an increased risk of **gastric ulcers** and bleeding, making it less safe for a patient with a history of **peptic ulcer disease**.
*Meloxicam*
- **Meloxicam** is a partially COX-2 selective NSAID, but it still has some affinity for COX-1 at higher doses, conferring a risk for **gastrointestinal adverse effects**.
- Although it may have a slightly better GI safety profile than non-selective NSAIDs, **celecoxib** offers superior GI protection.
*Ketorolac*
- **Ketorolac** is a potent **non-selective NSAID** primarily used for short-term management of moderate to severe acute pain, often administered parenterally.
- Its use is associated with a high risk of **gastrointestinal toxicity** and renal impairment, making it inappropriate for chronic pain management in a patient with **peptic ulcer disease**.
Non-opioid analgesics US Medical PG Question 2: A 17-year-old girl is brought to the emergency department 6 hours after she attempted suicide by consuming 16 tablets of acetaminophen (500 mg per tablet). At present, she does not have any complaints or symptoms. The patient is afebrile and vital signs are within normal limits. Physical examination is unremarkable. Laboratory findings show a serum acetaminophen level that is predictive of ‘probable hepatic toxicity’ on the Rumack-Matthew nomogram. Treatment is started with a drug, which is a precursor of glutathione and is a specific antidote for acetaminophen poisoning. Which of the following is an additional beneficial mechanism of action of this drug in this patient?
- A. Promotes glucuronidation of unmetabolized acetaminophen
- B. Promotes microcirculatory blood flow (Correct Answer)
- C. Promotes fecal excretion of unabsorbed acetaminophen
- D. Prevents gastrointestinal absorption of acetaminophen
- E. Promotes oxidation of N-acetyl-p-benzoquinoneimine (NAPQI)
Non-opioid analgesics Explanation: ***Promotes microcirculatory blood flow***
- **N-acetylcysteine** (NAC), the antidote for acetaminophen poisoning, acts as a **vasodilator** and **improves microcirculatory blood flow**, which can be beneficial in preventing and treating liver injury.
- This benefit is particularly relevant in cases of severe poisoning, where compromised hepatic perfusion can exacerbate damage.
*Promotes glucuronidation of unmetabolized acetaminophen*
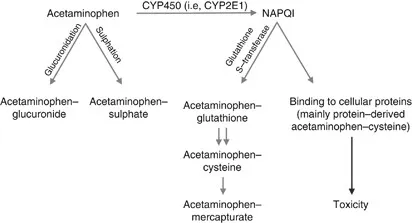
- NAC primarily works by replenishing **glutathione stores**, which are crucial for detoxifying the toxic metabolite **NAPQI**, not by enhancing glucuronidation.
- Glucuronidation is a separate metabolic pathway that conjugates acetaminophen for excretion and is not directly augmented by NAC.
*Promotes fecal excretion of unabsorbed acetaminophen*
- NAC is given systemically (orally or intravenously) to counteract absorbed acetaminophen and does not directly promote fecal excretion of unabsorbed drug.
- Activated charcoal is used to prevent absorption if given shortly after ingestion.
*Prevents gastrointestinal absorption of acetaminophen*
- NAC does not prevent the **Gastrointestinal absorption** of acetaminophen; it is administered after absorption has occurred and the drug is circulating in the body.
- Measures like activated charcoal or gastric lavage are used to prevent absorption if the patient presents early enough.
*Promotes oxidation of N-acetyl-p-benzoquinoneimine (NAPQI)*
- NAC works by **reducing** the toxic metabolite **NAPQI** back to acetaminophen and by replenishing **glutathione**, which then detoxifies NAPQI.
- It does not promote the *oxidation* of NAPQI; rather, it facilitates its *reduction* or conjugation to render it harmless.
Non-opioid analgesics US Medical PG Question 3: A 14-year-old boy is brought to the emergency department because of a 4-hour history of vomiting, lethargy, and confusion. Three days ago, he was treated with an over-the-counter medication for fever and runny nose. He is oriented only to person. His blood pressure is 100/70 mm Hg. Examination shows bilateral optic disc swelling and hepatomegaly. His blood glucose concentration is 65 mg/dL. Toxicology screening for serum acetaminophen is negative. The over-the-counter medication that was most likely used by this patient has which of the following additional effects?
- A. Increased partial thromboplastin time
- B. Decreased uric acid elimination
- C. Decreased expression of glycoprotein IIb/IIIa
- D. Irreversible inhibition of ATP synthase
- E. Irreversible inhibition of cyclooxygenase-1 (Correct Answer)
Non-opioid analgesics Explanation: ***Irreversible inhibition of cyclooxygenase-1***
- The patient's presentation is classic for **Reye syndrome** (vomiting, lethargy, confusion, cerebral edema with optic disc swelling, hepatomegaly, hypoglycemia) following recent viral illness treated with OTC medication
- **Aspirin** is strongly associated with Reye syndrome in children with viral infections and should be avoided in this population
- The "additional effect" of aspirin is its mechanism of action: **irreversible acetylation and inhibition of COX-1 and COX-2**
- This irreversible COX inhibition also explains aspirin's antiplatelet effects (via inhibition of thromboxane A2 synthesis) and anti-inflammatory properties
*Increased partial thromboplastin time*
- PTT measures the intrinsic and common coagulation pathways and is prolonged by **heparin** or clotting factor deficiencies
- Aspirin affects **platelet function** (prolonging bleeding time), not the coagulation cascade measured by PTT
- While Reye syndrome can cause coagulopathy from liver dysfunction, increased PTT is not a direct pharmacologic effect of aspirin
*Decreased uric acid elimination*
- **Low-dose aspirin** (<2 g/day) can decrease renal uric acid excretion and may precipitate gout
- While this is true, it is not the primary or most clinically relevant "additional effect" in this context
- High-dose aspirin actually increases uric acid excretion (uricosuric effect)
*Decreased expression of glycoprotein IIb/IIIa*
- This is the mechanism of **GP IIb/IIIa inhibitors** (abciximab, eptifibatide, tirofiban), not aspirin
- Aspirin inhibits platelet aggregation by preventing thromboxane A2 synthesis, not by affecting GP IIb/IIIa expression
- These are IV antiplatelet agents used in acute coronary syndromes, not OTC medications
*Irreversible inhibition of ATP synthase*
- This is not a mechanism of aspirin or other common OTC fever/cold medications
- While Reye syndrome involves mitochondrial dysfunction, aspirin does not directly inhibit ATP synthase
- The mitochondrial injury in Reye syndrome is likely multifactorial
Non-opioid analgesics US Medical PG Question 4: A 17-year-old female is brought to the emergency room by her parents shortly after a suicide attempt by aspirin overdose. Which of the following acid/base changes will occur FIRST in this patient?
- A. Metabolic alkalosis
- B. Respiratory acidosis
- C. Anion gap metabolic acidosis
- D. Respiratory alkalosis (Correct Answer)
- E. Non-anion gap metabolic acidosis
Non-opioid analgesics Explanation: ***Respiratory alkalosis***
- **Aspirin overdose** initially causes direct stimulation of the **respiratory center in the medulla**, leading to **hyperventilation**.
- This increased rate and depth of breathing blows off CO2, resulting in a primary **respiratory alkalosis**.
*Metabolic alkalosis*
- This is an unlikely primary event in aspirin overdose, which typically causes acidosis.
- While aspirin can cause electrolyte disturbances, a direct metabolic alkalosis as the *first* change is not characteristic.
*Respiratory acidosis*
- Respiratory depression, leading to respiratory acidosis, can occur in *severe* and *late-stage* aspirin overdose due to central nervous system depression.
- However, the initial effect is stimulation of respiration, causing alkalosis.
*Anion gap metabolic acidosis*
- This is a significant acid-base disturbance that *does* occur in aspirin overdose, but it develops *later*.
- Salicylates uncouple oxidative phosphorylation and impair cellular metabolism, leading to the accumulation of organic acids (e.g., lactic acid), causing a high anion gap metabolic acidosis.
*Non-anion gap metabolic acidosis*
- This type of acidosis is characterized by a preservation of the anion gap and is often associated with conditions like diarrhea or renal tubular acidosis.
- It is not the expected initial or primary acid-base disturbance in aspirin overdose.
Non-opioid analgesics US Medical PG Question 5: A 25-year-old woman presents to the ED with nausea, vomiting, diarrhea, abdominal pain, and hematemesis after ingesting large quantities of a drug. Which of the following pairs a drug overdose with the correct antidote for this scenario?
- A. Iron; deferoxamine (Correct Answer)
- B. Organophosphate; physostigmine
- C. Atropine; fomepizole
- D. Aspirin; N-acetylcysteine
- E. Acetaminophen; naloxone
Non-opioid analgesics Explanation: ***Iron; deferoxamine***
- The symptoms of **nausea, vomiting, diarrhea, abdominal pain, and hematemesis** are classic signs of **iron overdose**, which causes direct corrosive injury to the GI mucosa.
- **Deferoxamine** is a **chelating agent** specifically used to bind iron ions and facilitate their excretion, thus reversing iron toxicity.
*Organophosphate; physostigmine*
- **Organophosphate poisoning** presents with a **cholinergic crisis** (SLUDGE: salivation, lacrimation, urination, defecation, GI upset, emesis, miosis), but **hematemesis** is not a primary feature.
- **Physostigmine** is an acetylcholinesterase inhibitor used for atropine overdose, not organophosphate poisoning; **atropine** and **pralidoxime** are the antidotes for organophosphate.
*Atropine; fomepizole*
- **Atropine overdose** causes **anticholinergic symptoms** (dry mouth, blurred vision, tachycardia, urinary retention, delirium), not GI irritation and hematemesis.
- **Fomepizole** is an antidote for **methanol** or **ethylene glycol poisoning**, not atropine.
*Aspirin; N-acetylcysteine*
- **Aspirin overdose** (salicylate toxicity) results in **tinnitus, hyperventilation, metabolic acidosis, and altered mental status**, but **hematemesis** is less common than with iron.
- **N-acetylcysteine** is the antidote for acetaminophen overdose, not aspirin; aspirin overdose is treated with **alkalinization of urine** and **hemodialysis**.
*Acetaminophen; naloxone*
- **Acetaminophen overdose** primarily causes **hepatic toxicity**, initially presenting with non-specific GI symptoms, but **hematemesis** is atypical, and the main concern is liver damage.
- **Naloxone** is an opioid antagonist used to reverse opioid overdose, not acetaminophen.
Non-opioid analgesics US Medical PG Question 6: A 56-year-old woman presents with fatigue and joint pain in her fingers and wrists for the last 6 months. She says the pain is present in both hands, and her wrists are also swollen. Furthermore, she describes morning stiffness in her joints lasting about 2 hours, which improves with use. She has been taking acetaminophen, which provided minimal relief, but the swelling has gotten progressively worse. She also feels increasingly tired. Her past medical history reveals she has been successfully treated for Helicobacter pylori (H. pylori) related ulcers last year but still takes omeprazole for her mild gastroesophageal reflux. The patient denies any smoking history and stopped drinking when her gastric symptoms started. Which of the following analgesic drugs is the best choice to use in this patient?
- A. Indomethacin
- B. Naproxen
- C. Diclofenac
- D. Aspirin
- E. Celecoxib (Correct Answer)
Non-opioid analgesics Explanation: ***Celecoxib***
- This patient presents with symptoms highly suggestive of **rheumatoid arthritis**, characterized by **symmetric polyarticular joint pain**, swelling, and prolonged morning stiffness, along with fatigue. Given her history of **H. pylori-related ulcers** and current omeprazole use for GERD, she is at increased risk for **gastrointestinal complications** from traditional NSAIDs.
- **Celecoxib** is a **selective COX-2 inhibitor**, which preferentially inhibits the COX-2 enzyme responsible for inflammation and pain, while sparing COX-1, which protects the gastric mucosa. This makes it a safer choice for patients with a **history of GI ulcers** or at high risk for ulcer development.
*Indomethacin*
- Indomethacin is a **non-selective NSAID** that inhibits both COX-1 and COX-2. Given the patient's history of H. pylori ulcers and current omeprazole use, it carries a **high risk of causing gastric irritation** and ulcer recurrence.
- Its use would counteract the protective effects of omeprazole and potentially lead to further gastrointestinal complications.
*Naproxen*
- Naproxen is also a **non-selective NSAID** and thus carries a **significant risk of gastrointestinal adverse effects**, including gastric ulcers and bleeding, especially in a patient with a history of H. pylori ulcers.
- Using naproxen would be inappropriate due to the increased risk of exacerbating her pre-existing gastric issues.
*Diclofenac*
- Diclofenac is another **non-selective NSAID** with a considerable risk of **gastrointestinal complications**, similar to indomethacin and naproxen.
- Its use is not recommended given the patient's vulnerable gastric history, making it an unsafe option for long-term pain management in this case.
*Aspirin*
- **Regular-dose aspirin** is a **non-selective NSAID** and is particularly known for its strong inhibition of COX-1, leading to a high risk of **gastrointestinal bleeding** and ulcer formation.
- While low-dose aspirin is used for cardiovascular protection, high-dose aspirin for pain and inflammation is contraindicated in patients with a history of ulcers.
Non-opioid analgesics US Medical PG Question 7: A 61-year-old woman comes to the physician because of a 6-month history of left knee pain and stiffness. Examination of the left knee shows tenderness to palpation along the joint line; there is crepitus with full flexion and extension. An x-ray of the knee shows osteophytes with joint-space narrowing. Arthrocentesis of the knee joint yields clear fluid with a leukocyte count of 120/mm3. Treatment with ibuprofen during the next week significantly improves her condition. The beneficial effect of this drug is most likely due to inhibition of which of the following?
- A. Conversion of hypoxanthine to urate
- B. Conversion of phospholipids to arachidonic acid
- C. Conversion of prostaglandin H2 to thromboxane A2
- D. Conversion of arachidonic acid to prostaglandin G2 (Correct Answer)
- E. Conversion of dihydroorotate to orotate
Non-opioid analgesics Explanation: ***Conversion of arachidonic acid to prostaglandin G2***
- This patient presents with symptoms and signs consistent with **osteoarthritis**, characterized by joint pain, stiffness, crepitus, and radiographic findings like **osteophytes** and **joint-space narrowing**.
- **Ibuprofen is a non-selective NSAID** that inhibits **cyclooxygenase (COX-1 and COX-2) enzymes**, which catalyze the conversion of **arachidonic acid to prostaglandin G2 (PGG2)**, the first committed step in prostaglandin synthesis.
- By blocking prostaglandin production, ibuprofen reduces inflammation and pain associated with osteoarthritis.
*Conversion of hypoxanthine to urate*
- This process is catalyzed by **xanthine oxidase** and is inhibited by medications like **allopurinol**, used in the treatment of **gout** to reduce uric acid levels.
- Gout typically presents with acute, severe joint pain with signs of inflammation and monosodium urate crystals on joint aspiration, which are not characteristic of this patient's presentation.
*Conversion of phospholipids to arachidonic acid*
- This step is catalyzed by **phospholipase A2**, which is inhibited by **glucocorticoids** (via lipocortin induction).
- While glucocorticoids have potent anti-inflammatory effects by working upstream of the arachidonic acid cascade, ibuprofen has a different mechanism targeting the COX enzymes downstream.
*Conversion of prostaglandin H2 to thromboxane A2*
- This reaction is catalyzed by **thromboxane synthase**, primarily important in platelet aggregation and vasoconstriction.
- NSAIDs like ibuprofen do not specifically inhibit thromboxane synthase; rather, they inhibit COX enzymes upstream, which reduces production of both prostaglandins and thromboxanes.
- Low-dose aspirin preferentially inhibits COX-1 in platelets, reducing thromboxane A2 for cardioprotection, but this is not ibuprofen's primary therapeutic mechanism in osteoarthritis.
*Conversion of dihydroorotate to orotate*
- This is a step in **pyrimidine synthesis**, inhibited by **leflunomide**, a disease-modifying antirheumatic drug (DMARD) used in rheumatoid arthritis.
- This mechanism is unrelated to the action of NSAIDs or the treatment of osteoarthritis.
Non-opioid analgesics US Medical PG Question 8: A 40-year-old woman with a recent history of carcinoma of the breast status post mastectomy and adjuvant chemotherapy one week ago presents for follow-up. She reports adequate pain control managed with the analgesic drug she was prescribed. Past medical history is significant for hepatitis C and major depressive disorder. The patient denies any history of smoking or alcohol use but says she is currently using intravenous heroin and has been for the past 10 years. However, she reports that she has been using much less heroin since she started taking the pain medication, which is confirmed by the toxicology screen. Which of the following is the primary mechanism of action of the analgesic drug she was most likely prescribed?
- A. Pure antagonist at opioid receptors
- B. Pure agonist at the µ-opioid receptor (Correct Answer)
- C. Inhibits prostaglandin synthesis
- D. Mixed agonist-antagonist at opioid receptors
- E. Central action via blockade of serotonin reuptake
Non-opioid analgesics Explanation: ***Pure agonist at the µ-opioid receptor***
- Opioid analgesics, commonly prescribed for **post-mastectomy pain** and cancer-related pain, primarily exert their effects by acting as **pure agonists at the µ-opioid receptor**.
- This activation leads to profound **analgesia** by modulating pain perception and emotional response to pain in the central nervous system.
*Pure antagonist at opioid receptors*
- A **pure antagonist** would block opioid receptors and **reverse** the effects of opioid agonists, not provide analgesia.
- Such drugs are used to treat **opioid overdose** (e.g., naloxone) or to manage addiction by preventing opioid effects.
*Inhibits prostaglandin synthesis*
- This is the mechanism of action for **NSAIDs** (non-steroidal anti-inflammatory drugs), which primarily treat **mild to moderate pain** and inflammation.
- NSAIDs are generally insufficient for severe **post-surgical** or **cancer pain** of the magnitude experienced by this patient.
*Mixed agonist-antagonist at opioid receptors*
- Mixed agonist-antagonists provide analgesia by acting as agonists at some opioid receptors while acting as antagonists at others (e.g., **buprenorphine**).
- While they can provide pain relief, their use in acute severe pain is often limited, and they can sometimes **precipitate withdrawal** in patients chronically using full opioid agonists.
*Central action via blockade of serotonin reuptake*
- This is the primary mechanism of action for **antidepressants** (SSRIs) and some drugs used for **neuropathic pain** (e.g., tramadol with additional opioid action).
- While some antidepressants have analgesic properties, this mechanism alone is not typically the primary one for the potent pain relief needed post-mastectomy, which usually requires an **opioid**.
Non-opioid analgesics US Medical PG Question 9: A previously healthy 61-year-old man comes to the physician because of bilateral knee pain for the past year. The pain is worse with movement and is relieved with rest. Physical examination shows crepitus, pain, and decreased range of motion with complete flexion and extension of both knees. There is no warmth, redness, or swelling. X-rays of both knees show irregular joint space narrowing, osteophytes, and subchondral cysts. Which of the following is the most appropriate pharmacotherapy?
- A. Allopurinol
- B. Naproxen (Correct Answer)
- C. Celecoxib
- D. Infliximab
- E. Prednisone
Non-opioid analgesics Explanation: ***Naproxen***
- The patient's presentation with **bilateral knee pain worse with movement**, relief with rest, crepitus, and characteristic X-ray findings (joint space narrowing, osteophytes, subchondral cysts) is classic for **osteoarthritis (OA)** [3].
- **NSAIDs** like naproxen are **first-line pharmacotherapy** for managing pain and inflammation in osteoarthritis that is not adequately controlled by acetaminophen or topical agents [1].
- As a **non-selective NSAID**, naproxen is an appropriate initial choice for a patient without specified risk factors for GI complications or cardiovascular disease [2].
*Allopurinol*
- **Allopurinol** is a xanthine oxidase inhibitor used to reduce **urate production in hyperuricemia** and prevent gout attacks.
- The patient's symptoms are not consistent with gout, as there is **no acute inflammatory arthritis, redness, warmth, or swelling**.
*Celecoxib*
- **Celecoxib** is a **COX-2 selective NSAID** that can be used for osteoarthritis pain.
- It is generally preferred in patients with **documented GI risk factors** (history of peptic ulcer, concurrent anticoagulation, or advanced age with other risk factors).
- While this 61-year-old patient has age as a consideration, in the absence of other specified GI risk factors, either non-selective or COX-2 selective NSAIDs are reasonable; **naproxen is acceptable as initial therapy** and is more cost-effective.
*Infliximab*
- **Infliximab** is a **biologic disease-modifying antirheumatic drug (DMARD)**, specifically a TNF-alpha inhibitor, used to treat inflammatory arthritides like rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis.
- It is **not indicated for osteoarthritis**, which is a degenerative joint disease rather than an autoimmune inflammatory process.
*Prednisone*
- **Prednisone** is a corticosteroid used to **reduce inflammation** in various conditions, including inflammatory arthritides and acute pain flares.
- While it can provide symptomatic relief, it is **not a first-line or long-term pharmacotherapy for osteoarthritis** due to significant **side effects** with chronic use (weight gain, hyperglycemia, osteoporosis, immunosuppression) [1].
Non-opioid analgesics US Medical PG Question 10: A 43-year-old Caucasian female with a long history of uncontrolled migraines presents to general medical clinic with painless hematuria. She is quite concerned because she has never had symptoms like this before. Vital signs are stable, and her physical examination is benign. She denies any groin pain, flank pain, or costovertebral angle tenderness. She denies any recent urinary tract infections or dysuria. Urinary analysis confirms hematuria and a serum creatinine returns at 3.0. A renal biopsy reveals papillary necrosis and a tubulointerstitial infiltrate. What is the most likely diagnosis?
- A. Analgesic nephropathy (Correct Answer)
- B. Kidney cancer
- C. Sickle cell disease
- D. Bladder cancer
- E. Kidney stone
Non-opioid analgesics Explanation: ***Analgesic nephropathy***
- The patient's history of **uncontrolled migraines** suggests chronic use of analgesic medications, which can lead to **papillary necrosis** and chronic **tubulointerstitial nephritis**.
- **Painless hematuria** and elevated creatinine with biopsy-confirmed papillary necrosis and tubulointerstitial infiltrate are classic manifestations of analgesic nephropathy.
*Kidney cancer*
- While kidney cancer can cause **painless hematuria**, it typically presents with a **mass on imaging** and often results in symptoms like flank pain or palpable mass with progression.
- The specific renal biopsy findings of **papillary necrosis** and **tubulointerstitial infiltrate** are not characteristic of kidney cancer.
*Sickle cell disease*
- **Sickle cell nephropathy** can cause papillary necrosis and hematuria, but this patient is a **Caucasian female** and has no history or symptoms indicative of sickle cell disease.
- The disease is primarily seen in individuals of African, Mediterranean, or South Asian descent.
*Bladder cancer*
- **Bladder cancer** can cause painless hematuria, but it typically presents with **bladder lesions** on cystoscopy and biopsies show malignancy, not papillary necrosis or tubulointerstitial infiltrate.
- The renal pathology here points to a problem originating in the kidneys, not the bladder.
*Kidney stone*
- **Kidney stones** usually present with **severe flank pain** (renal colic), and often hematuria, but the pain would be a prominent symptom.
- A biopsy would show evidence of stone formation or obstruction, not tubulointerstitial infiltrate or papillary necrosis unless complicated by infection or obstruction.
More Non-opioid analgesics US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.