Neuromuscular blockers US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Neuromuscular blockers. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Neuromuscular blockers US Medical PG Question 1: During a nerve conduction study, which of the following ions is primarily responsible for the rapid upstroke of the action potential?
- A. Calcium
- B. Sodium (Correct Answer)
- C. Chloride
- D. Potassium
Neuromuscular blockers Explanation: ***Sodium***
- The rapid upstroke of an **action potential** (depolarization) in nerves is primarily due to the rapid influx of **sodium ions** (Na+) into the cell.
- This influx occurs through **voltage-gated sodium channels** that open in response to a threshold stimulus.
*Calcium*
- **Calcium ions** (Ca2+) play a significant role in neurotransmitter release at the **synaptic terminals** and in cardiac and smooth muscle action potentials.
- However, they are not the primary ion responsible for the initial rapid **depolarization** in peripheral nerve conduction.
*Chloride*
- **Chloride ions** (Cl-) are generally involved in maintaining the resting membrane potential and mediating **inhibitory postsynaptic potentials** (IPSPs) by causing hyperpolarization or preventing depolarization.
- They do not contribute to the rapid upstroke of an **action potential**.
*Potassium*
- **Potassium ions** (K+) are primarily responsible for the **repolarization phase** of the action potential.
- The efflux of K+ through **voltage-gated potassium channels** causes the membrane potential to return to its resting state.
Neuromuscular blockers US Medical PG Question 2: A 59-year-old woman is scheduled to undergo a right hip total arthroplasty for severe hip osteoarthritis that has failed conservative management. She has never had surgery before. She has a history of major depressive disorder and takes sertraline daily and ibuprofen occasionally for pain. Her mother died of breast cancer and her father died from a myocardial infarction. She has a brother who had an adverse reaction following anesthesia, but she does not know details of the event. In the operating room, the anesthesiologist administers isoflurane and succinylcholine. Two minutes later, the patient develops hypercarbia and hypertonicity of her bilateral upper and lower extremities. Her temperature is 103.7°F (39.8°C), blood pressure is 155/95 mmHg, pulse is 115/min, and respirations are 20/min.
A medication with which of the following mechanisms of action is most strongly indicated for this patient?
- A. Muscarinic antagonist
- B. Antihistamine
- C. Ryanodine receptor antagonist (Correct Answer)
- D. Cholinesterase inhibitor
- E. Dopamine receptor agonist
Neuromuscular blockers Explanation: ***Ryanodine receptor antagonist***
- The patient's presentation with **hyperthermia**, **hypercarbia**, and **muscle rigidity** after exposure to isoflurane and succinylcholine is highly indicative of **malignant hyperthermia (MH)**.
- **Dantrolene**, a **ryanodine receptor antagonist**, is the primary treatment for MH as it blocks the release of calcium from the sarcoplasmic reticulum, thereby reducing muscle contraction and heat production.
*Muscarinic antagonist*
- **Muscarinic antagonists** like atropine block the action of acetylcholine at muscarinic receptors and are used to treat **bradycardia** or reduce secretions.
- They would not address the underlying pathophysiology of malignant hyperthermia, which involves uncontrolled calcium release from the sarcoplasmic reticulum.
*Antihistamine*
- **Antihistamines** block histamine receptors and are used to treat **allergic reactions** or reduce nausea and vomiting.
- They have no role in the management of malignant hyperthermia, which is not an allergic response.
*Cholinesterase inhibitor*
- **Cholinesterase inhibitors** increase acetylcholine levels at the neuromuscular junction and are used to reverse **neuromuscular blockade** or treat **myasthenia gravis**.
- Administering a cholinesterase inhibitor would likely intensify muscle contraction and rigidity, worsening the patient's condition in malignant hyperthermia.
*Dopamine receptor agonist*
- **Dopamine receptor agonists** are primarily used to treat **Parkinson's disease** or as **vasopressors** in critical care.
- They have no direct therapeutic effect on the severe muscle rigidity and hypermetabolic state characteristic of malignant hyperthermia.
Neuromuscular blockers US Medical PG Question 3: A 46-year-old man presents after he accidentally got splashed with a liquid insecticide that was stored in a bucket in the storeroom one hour ago. He says that he can’t stop coughing and is having problems breathing. He also says he has a pain in his thighs which is unbearable, and his vision is blurry. His temperature is 36.7°C (98.1°F), the pulse is 130/min, the blood pressure is 144/92 mm Hg, and the respiratory rate is 20/min. On physical examination, the patient shows mild generalized pallor, moderate respiratory distress, excessive salivation, and diaphoresis. Cough is non-productive. Pupils are constricted (pinpoint). The cardiopulmonary exam reveals bilateral crepitus. The patient is administered atropine and pralidoxime, which help improve his symptoms. Which of the following is most likely to improve in this patient with the administration of atropine?
- A. Muscle cramps
- B. Hypertension
- C. Tachycardia
- D. Bronchospasm (Correct Answer)
- E. Pallor
Neuromuscular blockers Explanation: ***Bronchospasm***
- The patient exhibits symptoms of **cholinergic crisis** due to organophosphate poisoning, including respiratory distress and excessive salivation. **Atropine** is a muscarinic antagonist that blocks the effects of acetylcholine at muscarinic receptors, thereby relieving **bronchospasm** and reducing secretions.
- Relief of bronchospasm will improve breathing difficulties, a prominent symptom in this patient.
*Muscle cramps*
- **Organophosphate poisoning** can cause **nicotinic effects** like muscle fasciculations and cramps due to excessive acetylcholine at the neuromuscular junction.
- **Atropine primarily targets muscarinic receptors** and has little to no effect on nicotinic receptors, so it would not significantly improve muscle cramps.
*Hypertension*
- **Organophosphate poisoning** typically causes **bradycardia and hypotension** in severe cases, although transient hypertension can occur due to sympathetic activation.
- While atropine can increase heart rate, its direct effect on blood pressure in this context is complex and primarily aimed at reversing muscarinic effects rather than directly treating hypertension.
*Tachycardia*
- The patient presents with **tachycardia (pulse 130/min)**, which is an expected finding in symptomatic organophosphate poisoning, often compensatory to hypotension or due to central nervous system effects.
- **Atropine** itself is a heart rate-elevating drug that blocks parasympathetic stimulation, so it would likely exacerbate or have no corrective effect on existing tachycardia.
*Pallor*
- Pallor can be a non-specific symptom, possibly related to poor circulation or anemia.
- **Atropine** directly addresses muscarinic effects of organophosphate poisoning (e.g., bronchorrhea, bradycardia) and would not be expected to directly improve **pallor**.
Neuromuscular blockers US Medical PG Question 4: A 25-year-old man is scheduled for an orthopedic surgery. His routine preoperative laboratory tests are within normal limits. An urticarial reaction occurs when a non-depolarizing neuromuscular blocking agent is injected for muscle relaxation and mechanical ventilation. The patient’s lungs are manually ventilated with 100% O2 by bag and mask and then through an endotracheal tube. After a few minutes, edema of the face and neck rapidly ensues and giant hives appear over most of his body. Which of the following neuromuscular blocking agents was most likely used in this operation?
- A. Ketamine
- B. Succinylcholine
- C. Nitrous oxide
- D. Neostigmine
- E. D-tubocurarine (Correct Answer)
Neuromuscular blockers Explanation: ***D-tubocurarine***
- The rapid onset of widespread **urticaria**, facial and neck **edema**, and giant hives immediately after injection of a **non-depolarizing neuromuscular blocking agent** strongly points to an **anaphylactic reaction**. d-Tubocurarine is a historical non-depolarizing neuromuscular blocker that is known for its propensity to cause **histamine release**, leading to severe hypersensitivity reactions including anaphylaxis and therefore is rarely used today.
- The symptoms described are classic signs of a severe allergic reaction, which is a known and significant side effect of d-tubocurarine due to its potent histamine-releasing properties.
*Ketamine*
- **Ketamine** is a dissociative anesthetic, not a neuromuscular blocking agent. It primarily affects the central nervous system, producing a trance-like state, pain relief, sedation, and amnesia.
- While it can cause some cardiovascular stimulation, it does not typically induce **histamine release** leading to anaphylactic-like reactions as described with neuromuscular blockers.
*Succinylcholine*
- **Succinylcholine** is a depolarizing neuromuscular blocker that can cause adverse effects like **hyperkalemia**, malignant hyperthermia, and muscle pain.
- Although it can rarely trigger an allergic reaction, it is not primarily known for causing widespread **histamine release** and anaphylaxis like d-tubocurarine.
*Nitrous oxide*
- **Nitrous oxide** is an inhalational anesthetic gas used for sedation and analgesia; it is not a neuromuscular blocking agent.
- Its adverse effects are generally related to its anesthetic properties, such as nausea and vomiting, and it does not cause **allergic reactions** of this nature.
*Neostigmine*
- **Neostigmine** is an acetylcholinesterase inhibitor used to **reverse the effects of non-depolarizing neuromuscular blockers**, not as a blocking agent itself.
- It increases acetylcholine levels at the neuromuscular junction; its side effects are typically cholinergic, such as bradycardia, salivation, and bronchospasm, and it does not cause anaphylaxis from histamine release.
Neuromuscular blockers US Medical PG Question 5: A neurophysiology expert is teaching his students the physiology of the neuromuscular junction. While describing the sequence of events that takes place at the neuromuscular junction, he mentions that as the action potential travels down the motor neuron, it causes depolarization of the presynaptic membrane. This results in the opening of voltage-gated calcium channels, which leads to an influx of calcium into the synapse of the motor neuron. Consequently, the cytosolic concentration of Ca2+ ions increases. Which of the following occurs at the neuromuscular junction as a result of this increase in cytosolic Ca2+?
- A. Generation of an end plate potential
- B. Exocytosis of acetylcholine from the synaptic vesicles (Correct Answer)
- C. Increased Na+ and K+ conductance of the motor end plate
- D. Binding of Ca2+ ions to NM receptors
- E. Release of Ca2+ ions into the synaptic cleft
Neuromuscular blockers Explanation: ***Exocytosis of acetylcholine from the synaptic vesicles***
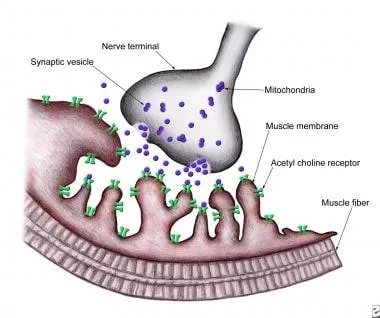
- The increase in **cytosolic Ca2+** within the presynaptic terminal is the primary trigger for the fusion of **synaptic vesicles** filled with **acetylcholine (ACh)** with the presynaptic membrane.
- This fusion process, known as **exocytosis**, releases ACh into the **synaptic cleft**, initiating synaptic transmission.
*Generation of an end plate potential*
- The **end plate potential (EPP)** is generated *after* acetylcholine (ACh) is released into the synaptic cleft and binds to receptors on the motor end plate.
- This event occurs *following* the Ca2+-induced release of neurotransmitter, not as a direct result of the Ca2+ increase itself.
*Increased Na+ and K+ conductance of the motor end plate*
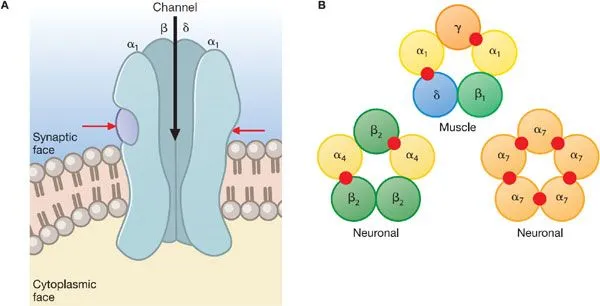
- Increased **Na+ and K+ conductance** across the motor end plate membrane is a direct consequence of acetylcholine binding to its receptors, which are **ligand-gated ion channels**.
- This change in conductance *generates the end plate potential*, occurring after ACh release.
*Binding of Ca2+ ions to NM receptors*
- **NM receptors** (nicotinic muscle receptors) are located on the **postsynaptic membrane** (motor end plate) and bind to **acetylcholine (ACh)**, not Ca2+ ions.
- Calcium's primary role in this context is presynaptic: triggering ACh release.
*Release of Ca2+ ions into the synaptic cleft*
- Calcium ions enter the **presynaptic terminal** from the synaptic cleft, and their increased cytosolic concentration within the presynaptic terminal drives neurotransmitter release.
- Calcium itself is not released *into* the synaptic cleft in this process; rather, it enters the presynaptic neuron from the cleft.
Neuromuscular blockers US Medical PG Question 6: A 23-year-old man is brought to the emergency department by ambulance following a motor vehicle accident. He was pinned between 2 cars for several hours. The patient has a history of asthma. He uses an albuterol inhaler intermittently. The patient was not the driver, and admits to having a few beers at a party prior to the accident. His vitals in the ambulance are stable. Upon presentation to the emergency department, the patient is immediately brought to the operating room for evaluation and surgical intervention. It is determined that the patient’s right leg has a Gustilo IIIC injury in the mid-shaft of the tibia with a severely comminuted fracture. The patient’s left leg suffered a similar injury but with damage to the peroneal nerve. The anesthesiologist begins to induce anesthesia. Which of the following agents would be contraindicated in this patient?
- A. Halothane
- B. Propofol
- C. Etomidate
- D. Succinylcholine (Correct Answer)
- E. Neostigmine
Neuromuscular blockers Explanation: ***Succinylcholine***
- Given the history of the patient being pinned between two cars for several hours, there is a significant risk of **rhabdomyolysis** and subsequent hyperkalemia.
- **Succinylcholine**, a depolarizing neuromuscular blocker, can cause a sudden and significant release of potassium from muscle cells, leading to **life-threatening hyperkalemia** in patients with rhabdomyolysis or crush injuries.
*Halothane*
- While **halothane** has been associated with **malignant hyperthermia**, the patient's history does not directly suggest an increased risk for this condition here.
- It also has a bronchodilating effect, which could be beneficial for a patient with a history of **asthma**.
*Propofol*
- **Propofol** is a commonly used intravenous anesthetic for induction and maintenance, providing rapid onset and recovery.
- There are generally no specific contraindications for propofol in a patient with a crush injury or asthma.
*Etomidate*
- **Etomidate** is an intravenous anesthetic agent known for its **cardiovascular stability**, making it a good choice for hemodynamically unstable patients.
- It can cause adrenal suppression, but this is usually a concern with prolonged infusions, not a single induction dose.
*Neostigmine*
- **Neostigmine** is an acetylcholinesterase inhibitor used to reverse the effects of non-depolarizing neuromuscular blockers.
- It is not an induction agent and would not be used at the beginning of anesthesia induction.
Neuromuscular blockers US Medical PG Question 7: A 1-year-old boy presents to the emergency department with weakness and a change in his behavior. His parents state that they first noticed the change in his behavior this morning and it has been getting worse. They noticed the patient was initially weak in his upper body and arms, but now he won’t move his legs with as much strength or vigor as he used to. Physical exam is notable for bilateral ptosis with a sluggish pupillary response, a very weak sucking and gag reflex, and shallow respirations. The patient is currently drooling and his diaper is dry. The parents state he has not had a bowel movement in over 1 day. Which of the following is the pathophysiology of this patient’s condition?
- A. Lower motor neuron destruction in the anterior horn
- B. Antibodies against postsynaptic nicotinic cholinergic ion channels
- C. Blockade of presynaptic acetylcholine release at the neuromuscular junction (Correct Answer)
- D. Autoantibodies against the presynaptic voltage-gated calcium channels
- E. Autoimmune demyelination of peripheral nerves
Neuromuscular blockers Explanation: ***Blockade of presynaptic acetylcholine release at the neuromuscular junction***
- The patient's symptoms, including **descending flaccid paralysis** (starting in the upper body and progressing downwards), **ptosis**, **sluggish pupillary response**, **weak suck/gag reflex**, **shallow respirations**, **drooling**, and **constipation**, are classic for **infant botulism**.
- **Infant botulism** is caused by the **botulinum toxin** produced by *Clostridium botulinum*, which **inhibits acetylcholine exocytosis** at the neuromuscular junction.
*Lower motor neuron destruction in the anterior horn*
- This describes conditions like **poliomyelitis**, which causes **asymmetric flaccid paralysis** and spares extraocular and bulbar muscles.
- The patient's presentation of **symmetric, descending paralysis** with prominent **bulbar involvement** (ptosis, weak suck/gag, sluggish pupils) is inconsistent with anterior horn cell destruction.
*Antibodies against postsynaptic nicotinic cholinergic ion channels*
- This is the pathophysiology of **myasthenia gravis**, which causes fluctuating muscle weakness that **worsens with activity** and improves with rest.
- While it can cause ptosis and bulbar weakness, it typically does not present with the rapid, progressive descending paralysis, absent gag reflex, or pupillary sluggishness seen in this infant.
*Autoantibodies against the presynaptic voltage-gated calcium channels*
- This is characteristic of **Lambert-Eaton Myasthenic Syndrome (LEMS)**, which causes proximal muscle weakness and often improves with repeated muscle activation (unlike myasthenia gravis).
- LEMS is rare in infants and typically associated with malignancy in adults; the patient's symptoms are more consistent with a neurotoxin.
*Autoimmune demyelination of peripheral nerves*
- This is the hallmark of **Guillain-Barré Syndrome (GBS)**, which typically presents with **ascending paralysis** (weakness starting in the legs and moving upwards) and **areflexia**.
- The patient's **descending paralysis** and prominent **bulbar/autonomic symptoms** (pupil changes, constipation) are not typical for GBS.
Neuromuscular blockers US Medical PG Question 8: A 16-year-old girl is brought to the emergency department by her friends who say that she took a whole bottle of her mom’s medication. They do not know which medication it was she ingested. The patient is slipping in and out of consciousness and is unable to offer any history. Her temperature is 39.6°C (103.2°F), the heart rate is 135/min, the blood pressure is 178/98 mm Hg, and the respiratory rate is 16/min. On physical examination, there is significant muscle rigidity without tremor or clonus. Which of the following is the best course of treatment for this patient?
- A. Cyproheptadine
- B. Dantrolene (Correct Answer)
- C. Flumazenil
- D. Fenoldopam
- E. Naloxone
Neuromuscular blockers Explanation: ***Dantrolene***
- The patient's presentation with **hyperthermia**, **tachycardia**, **hypertension**, and **severe muscle rigidity without tremor or clonus** is highly suggestive of **neuroleptic malignant syndrome (NMS)** or **malignant hyperthermia**.
- **Dantrolene** is a direct-acting **skeletal muscle relaxant** that reduces calcium release from the sarcoplasmic reticulum, effectively treating the muscle rigidity and hyperthermia in these conditions.
*Cyproheptadine*
- **Cyproheptadine** is an **antihistamine with serotonin antagonist properties** used to treat **serotonin syndrome**, which typically presents with **clonus** and **hyperreflexia**, not the rigidity seen here.
- While both NMS and serotonin syndrome involve hyperthermia, the distinct absence of clonus and presence of severe rigidity points away from serotonin syndrome.
*Flumazenil*
- **Flumazenil** is a **benzodiazepine receptor antagonist** used to reverse **benzodiazepine overdose**.
- Benzodiazepine overdose typically causes **CNS depression** (hypotension, bradycardia, respiratory depression), which is opposite to the patient's hyperdynamic state.
*Fenoldopam*
- **Fenoldopam** is a **D1 dopamine receptor agonist** used intravenously to treat **severe hypertension** and **hypertensive emergencies**.
- Although the patient has hypertension, fenoldopam would not address the underlying pathology of hyperthermia and muscle rigidity, which are the primary life-threatening issues.
*Naloxone*
- **Naloxone** is a **mu-opioid receptor antagonist** used to reverse **opioid overdose**.
- Opioid overdose typically causes **respiratory depression**, **miosis**, and **CNS depression**, which are not consistent with this patient's presentation.
Neuromuscular blockers US Medical PG Question 9: A 50-year-old woman presents with acute onset fever and chills for the past hour. She mentions earlier in the day she felt blue, so she took some St. John’s wort because she was told by a friend that it helps with depression. Past medical history is significant for hypertension, diabetes mellitus, and depression managed medically with captopril, metformin, and fluoxetine. She has no history of allergies. Her pulse is 130/min, the respiratory rate is 18/min, the blood pressure is 176/92 mm Hg, and the temperature is 38.5°C (101.3°F). On physical examination, the patient is profusely diaphoretic and extremely irritable when asked questions. Oriented x 3. The abdomen is soft and nontender with no hepatosplenomegaly. Increased bowel sounds are heard in the abdomen. Deep tendon reflexes are 3+ bilaterally and clonus is elicited. The sensation is decreased in the feet bilaterally. Mydriasis is present. Fingerstick glucose is 140 mg/dL. An ECG shows sinus tachycardia but is otherwise normal. Which of the following is the most likely cause of this patient’s condition?
- A. Sepsis
- B. Anaphylactic reaction
- C. Diabetic ketoacidosis
- D. Neuroleptic malignant syndrome
- E. Serotonin syndrome (Correct Answer)
Neuromuscular blockers Explanation: ***Serotonin syndrome***
- The patient's presentation with **fever, diaphoresis, hypertension, tachycardia, hyperreflexia, clonus, mydriasis**, and **agitation** after combining an **SSRI (fluoxetine)** with **St. John's wort** (a serotonin-enhancing herbal supplement) is highly characteristic of serotonin syndrome.
- This condition results from excessive serotonergic activity in the central and peripheral nervous system.
*Sepsis*
- While **fever, chills, and tachycardia** can be indicators of sepsis, the presence of specific neurological and neuromuscular signs like **hyperreflexia, clonus, and mydriasis** points away from it.
- The patient's **irritable state and normal mental orientation** is less typical for severe sepsis, which often involves altered mental status.
*Anaphylactic reaction*
- **Anaphylaxis** presents with rapid onset of symptoms such as **urticaria, angioedema, bronchospasm, and hypotension**, which are not observed in this patient.
- There is no history of allergen exposure, and the prominent neurological symptoms are not typical of anaphylaxis.
*Diabetic ketoacidosis*
- **DKA** is characterized by **hyperglycemia, metabolic acidosis, and ketonemia**, often presenting with Kussmaul respirations and fruity breath odor.
- The patient's **fingerstick glucose (140 mg/dL)** is not significantly elevated, and there is no mention of deep, rapid breathing or other DKA-specific symptoms.
*Neuroleptic malignant syndrome*
- **NMS** is typically associated with exposure to **dopamine antagonists (antipsychotics)** and is characterized by **severe muscle rigidity, hyperthermia, altered mental status, and autonomic instability.**
- While some symptoms overlap, this patient's history of St. John's wort and fluoxetine points to increased serotonin, and the specific neuromuscular findings like clonus are more indicative of serotonin syndrome.
Neuromuscular blockers US Medical PG Question 10: A 32-year-old woman is admitted to the hospital after undergoing an open cholecystectomy under general anesthesia. Preoperatively, the patient was administered a single dose of intravenous ceftriaxone. Now, the anesthetic effects have worn off, and her pain is well managed. The patient has a prior medical history of hypertension which has been well-controlled by captopril for 2 years. Her vitals currently show: blood pressure 134/82 mm Hg, heart rate 84/min, and respiratory rate 16/min. Postoperative laboratory findings are significant for the following:
Serum glucose (random) 174 mg/dL
Serum electrolytes
Sodium 142 mEq/L
Potassium 3.9 mEq/L
Chloride 101 mEq/L
Serum creatinine 0.9 mg/dL
Blood urea nitrogen 10 mg/dL
Alanine aminotransferase (ALT) 150 U/L
Aspartate aminotransferase (AST) 172 U/L
Serum bilirubin (total) 0.9 mg/dL
Preoperative labs were all within normal limits. Which of the following drugs is most likely responsible for this patient’s abnormal laboratory findings?
- A. Captopril
- B. Propofol
- C. Nitrous oxide
- D. Sevoflurane (Correct Answer)
- E. Ceftriaxone
Neuromuscular blockers Explanation: ***Sevoflurane***
- **Sevoflurane** is a volatile halogenated anesthetic that can rarely cause **postoperative hepatotoxicity** (halogenated anesthetic hepatitis)
- This presents with **elevated transaminases** (ALT and AST) within 2-14 days post-surgery
- Sevoflurane can also cause **transient hyperglycemia** through stress response and insulin resistance during and after anesthesia
- While less hepatotoxic than halothane, sevoflurane metabolism produces trifluoroacetic acid derivatives that can trigger immune-mediated liver injury in susceptible individuals
- Renal function remains normal, distinguishing this from fluoride-induced nephrotoxicity
*Captopril*
- **Captopril** is an ACE inhibitor that can rarely cause **cholestatic hepatitis** with chronic use
- However, the patient has been on captopril for 2 years with normal preoperative labs, making it an unlikely cause of acute postoperative transaminase elevation
- Does not explain the hyperglycemia observed
*Propofol*
- **Propofol** is an intravenous anesthetic that can cause **propofol infusion syndrome** with prolonged high-dose infusions (typically >48 hours)
- While propofol can cause metabolic derangements, acute transaminase elevation is not a typical feature of short-term use for routine surgery
- The degree of liver enzyme elevation seen here is more consistent with volatile anesthetic hepatotoxicity
*Nitrous oxide*
- **Nitrous oxide** inactivates **vitamin B12** (methionine synthase inhibition), leading to megaloblastic anemia and neurological complications with prolonged or repeated exposure
- Does not cause acute hepatotoxicity or explain the elevated transaminases and glucose seen in this case
*Ceftriaxone*
- **Ceftriaxone** can cause **cholestatic hepatitis** and hyperbilirubinemia, particularly with prolonged use
- However, this patient received only a **single preoperative dose**, making ceftriaxone an unlikely cause
- The patient's bilirubin is normal (0.9 mg/dL), which would be elevated in ceftriaxone-induced cholestasis
- Does not explain the hyperglycemia
More Neuromuscular blockers US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.