Local anesthetics US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Local anesthetics. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Local anesthetics US Medical PG Question 1: During a nerve conduction study, which of the following ions is primarily responsible for the rapid upstroke of the action potential?
- A. Calcium
- B. Sodium (Correct Answer)
- C. Chloride
- D. Potassium
Local anesthetics Explanation: ***Sodium***
- The rapid upstroke of an **action potential** (depolarization) in nerves is primarily due to the rapid influx of **sodium ions** (Na+) into the cell.
- This influx occurs through **voltage-gated sodium channels** that open in response to a threshold stimulus.
*Calcium*
- **Calcium ions** (Ca2+) play a significant role in neurotransmitter release at the **synaptic terminals** and in cardiac and smooth muscle action potentials.
- However, they are not the primary ion responsible for the initial rapid **depolarization** in peripheral nerve conduction.
*Chloride*
- **Chloride ions** (Cl-) are generally involved in maintaining the resting membrane potential and mediating **inhibitory postsynaptic potentials** (IPSPs) by causing hyperpolarization or preventing depolarization.
- They do not contribute to the rapid upstroke of an **action potential**.
*Potassium*
- **Potassium ions** (K+) are primarily responsible for the **repolarization phase** of the action potential.
- The efflux of K+ through **voltage-gated potassium channels** causes the membrane potential to return to its resting state.
Local anesthetics US Medical PG Question 2: Two hours after undergoing elective cholecystectomy with general anesthesia, a 41-year-old woman is evaluated for decreased mental status. BMI is 36.6 kg/m2. Respirations are 18/min and blood pressure is 126/73 mm Hg. Physical examination shows the endotracheal tube in normal position. She does not respond to sternal rub and gag reflex is absent. Arterial blood gas analysis on room air shows normal PO2 and PCO2 levels. Which of the following anesthetic properties is the most likely cause of these findings?
- A. Low blood solubility
- B. High lipid solubility (Correct Answer)
- C. Low brain-blood partition coefficient
- D. High minimal alveolar concentration
- E. Low cytochrome P450 activity
Local anesthetics Explanation: ***High lipid solubility***
- Anesthetics with **high lipid solubility** accumulate in **adipose tissue** and are slowly released, prolonging their effect, especially in obese patients.
- The patient's **obesity (BMI 36.6 kg/m2)** contributes to a larger reservoir for lipid-soluble drugs, leading to delayed recovery and decreased mental status.
*Low blood solubility*
- **Low blood solubility** implies a rapid equilibrium between the lungs and the blood, leading to a **faster onset and offset** of anesthetic action.
- This property would result in a quicker recovery from anesthesia, which contradicts the patient's prolonged unconsciousness.
*Low brain-blood partition coefficient*
- A **low brain-blood partition coefficient** means the anesthetic does not accumulate significantly in brain tissue relative to blood.
- Agents with this property equilibrate quickly and leave the brain rapidly upon discontinuation, resulting in **fast recovery**, which is inconsistent with the patient's persistent decreased mental status.
*High minimal alveolar concentration*
- **High minimal alveolar concentration (MAC)** means that a higher concentration of the anesthetic gas is required to produce immobility in 50% of patients.
- A high MAC describes the **potency** of an anesthetic and does not directly explain prolonged recovery or decreased mental status in an obese patient, but rather indicates that a larger dose or concentration was needed to achieve anesthesia.
*Low cytochrome P450 activity*
- **Low cytochrome P450 activity** would lead to slower metabolism of drugs that are primarily cleared by this system, potentially prolonging their effects.
- While relevant for some drugs, the primary issue for inhaled anesthetics is their **physical distribution and elimination**, not typically metabolic clearance via Cytochrome P450 enzymes.
Local anesthetics US Medical PG Question 3: A group of researchers is studying various inhaled substances to determine their anesthetic properties. In particular, they are trying to identify an anesthetic with fast onset and quick recovery for use in emergencies. They determine the following data:
Inhalational anesthetic Blood-gas partition coefficient
A 0.15
B 0.92
C 5.42
Which of the following statements is accurate with regard to these inhaled anesthetic substances?
- A. Agent C has the fastest onset of action
- B. Agent A has the fastest onset of action (Correct Answer)
- C. Agent B is the most potent
- D. Agent B has the fastest onset of action
- E. Agent A is the most potent
Local anesthetics Explanation: ***Agent A has the fastest onset of action***
- **Agent A** has the lowest blood-gas partition coefficient (0.15), indicating very low solubility in blood.
- A **low blood-gas partition coefficient** means the anesthetic quickly equilibrates between the lungs and blood, leading to a rapid rise in partial pressure in the brain and thus **fast onset of action** and **quick recovery**.
*Agent C has the fastest onset of action*
- **Agent C** has the highest blood-gas partition coefficient (5.42), indicating high solubility in blood.
- High solubility means the anesthetic takes longer to saturate the blood and reach the brain, resulting in a **slow onset of action** and **slow recovery**.
*Agent B is the most potent*
- **Potency** of an inhaled anesthetic is inversely related to its **Minimum Alveolar Concentration (MAC)**, not directly to its blood-gas partition coefficient.
- While a higher blood-gas coefficient can sometimes correlate with other properties, it does not directly determine potency.
*Agent B has the fastest onset of action*
- **Agent B** has a blood-gas partition coefficient of 0.92, which is higher than Agent A (0.15).
- A higher blood-gas partition coefficient means the anesthetic is more soluble in blood, leading to a **slower onset of action** compared to Agent A.
*Agent A is the most potent*
- **Agent A** has the lowest blood-gas partition coefficient (0.15), which indicates **fast onset** and **rapid recovery**, but not necessarily high potency.
- **Potency** is determined by MAC (Minimum Alveolar Concentration), which is the concentration of anesthetic at 1 atmosphere that produces immobility in 50% of patients challenged with a surgical incision.
Local anesthetics US Medical PG Question 4: A 42-year-old man presents to his family physician for evaluation of oral pain. He states that he has increasing pain in a molar on the top left of his mouth. The pain started 1 week ago and has been progressively worsening since then. His medical history is significant for hypertension and type 2 diabetes mellitus, both of which are currently controlled with lifestyle modifications. His blood pressure is 124/86 mm Hg, heart rate is 86/min, and respiratory rate is 14/min. Physical examination is notable for a yellow-black discoloration of the second molar on his left upper mouth. The decision is made to refer him to a dentist for further management of this cavity. The patient has never had any dental procedures and is nervous about what type of sedation will be used. Which of the following forms of anesthesia utilizes solely an oral or intravenous anti-anxiety medication?
- A. Minimal Sedation (Correct Answer)
- B. Dissociation
- C. Regional anesthesia
- D. Epidural anesthesia
- E. Deep sedation
Local anesthetics Explanation: ***Minimal Sedation***
- This involves using **oral** or **intravenous anti-anxiety medications** to help a patient relax while remaining conscious and responsive.
- The patient can still respond to verbal commands but is in a state of decreased anxiety and awareness.
*Dissociation*
- This is a state induced by certain drugs, like **ketamine**, where the patient feels detached from their body and environment.
- While it can be achieved intravenously, it is not solely an anti-anxiety medication effect and involves a different neurological state.
*Regional anesthesia*
- This involves injecting a **local anesthetic** near nerves to numb a specific part of the body, such as a limb or a jaw section for dental procedures.
- It primarily provides pain relief by blocking nerve signals and does not typically involve anti-anxiety medication as its sole component for sedation.
*Epidural anesthesia*
- This form of regional anesthesia involves injecting a **local anesthetic** into the **epidural space** surrounding the spinal cord to block pain signals.
- It is used for pain control during surgery or childbirth and does not involve oral or intravenous anti-anxiety medication as the primary method of sedation.
*Deep sedation*
- This involves a more profound depression of consciousness than minimal sedation, where the patient may be difficult to arouse but still responds purposefully to repeated or painful stimulation.
- While it can use intravenous medications, it typically involves a combination of sedatives and analgesics to achieve a deeper state of unresponsiveness, beyond just anti-anxiety medication.
Local anesthetics US Medical PG Question 5: A 28-year-old man comes to the emergency department for an injury sustained while doing construction. Physical examination shows a long, deep, irregular laceration on the lateral aspect of the left forearm with exposed fascia. Prior to surgical repair of the injury, a brachial plexus block is performed using a local anesthetic. Shortly after the nerve block is performed, he complains of dizziness and then loses consciousness. His radial pulse is faint and a continuous cardiac monitor shows a heart rate of 24/min. Which of the following is the most likely mechanism of action of the anesthetic that was administered?
- A. Activation of acetylcholine receptors
- B. Inactivation of ryanodine receptors
- C. Inactivation of sodium channels (Correct Answer)
- D. Activation of GABA receptors
- E. Inactivation of potassium channels
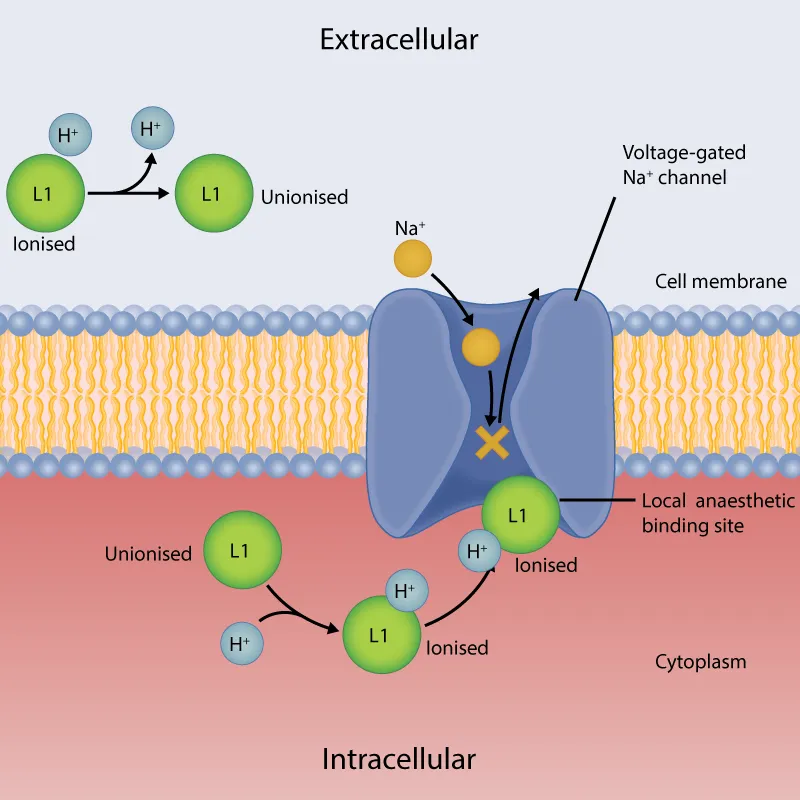
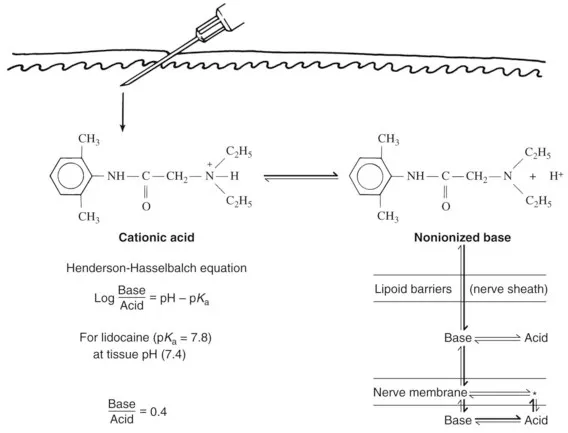
Local anesthetics Explanation: ***Inactivation of sodium channels***
- Local anesthetics primarily work by reversibly blocking **voltage-gated sodium channels** in nerves.
- This prevents the influx of sodium ions, inhibiting the generation and propagation of **action potentials**, thus blocking pain signals.
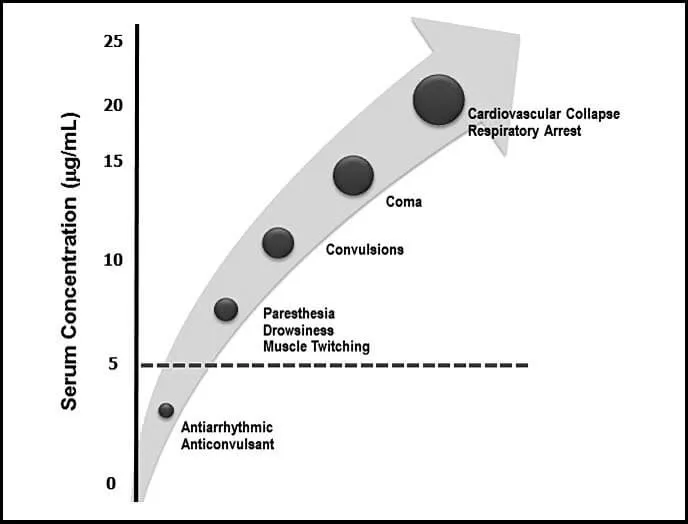
- The clinical presentation of dizziness, loss of consciousness, and bradycardia represents systemic toxicity from intravascular absorption of the local anesthetic.
*Activation of acetylcholine receptors*
- Activation of **nicotinic or muscarinic acetylcholine receptors** is the primary mechanism of action for neuromuscular stimulants or parasympathomimetics, not local anesthetics.
- This would typically lead to muscle contraction or increased parasympathetic activity rather than analgesia and local nerve block.
*Inactivation of ryanodine receptors*
- Inactivation of **ryanodine receptors** primarily affects calcium release from the sarcoplasmic reticulum in muscle cells, crucial for excitation-contraction coupling.
- This mechanism is associated with drugs like dantrolene used for malignant hyperthermia, not local anesthetics.
*Activation of GABA receptors*
- Activation of **GABA-A receptors** is the primary mechanism of action for benzodiazepines and barbiturates, leading to widespread CNS depression and sedation.
- While systemic absorption of local anesthetics can cause CNS effects (as seen in toxicity), their primary therapeutic mechanism for nerve block is sodium channel inactivation, not GABA receptor activation.
*Inactivation of potassium channels*
- Inactivation of **potassium channels** would typically prolong repolarization and increase neuronal excitability or cause arrhythmias, depending on the specific channel.
- This is not the mechanism of action for local anesthetics, which prevent depolarization by blocking sodium channel activation.
Local anesthetics US Medical PG Question 6: A 50-year-old male is brought to the dermatologist's office with complaints of a pigmented lesion. The lesion is uniformly dark with clean borders and no asymmetry and has been increasing in size over the past two weeks. He works in construction and spends large portions of his day outside. The dermatologist believes that this mole should be biopsied. To prepare the patient for the biopsy, the dermatologist injects a small amount of lidocaine into the skin around the lesion. Which of the following nerve functions would be the last to be blocked by the lidocaine?
- A. Pain
- B. Touch
- C. Temperature
- D. Sympathetic stimulation
- E. Pressure (Correct Answer)
Local anesthetics Explanation: ***Pressure***
- **Pressure** sensation is mediated by **Aβ fibers**, which are relatively **larger** and **myelinated**, making them more resistant to local anesthetic blockade.
- Nerve fibers are blocked in a specific order, typically starting with smaller, unmyelinated fibers and ending with larger, myelinated fibers.
*Pain*
- **Pain** sensation is primarily carried by **unmyelinated C fibers** and **small myelinated Aδ fibers**, which are among the **first to be blocked** by local anesthetics.
- These fibers have a **high surface-to-volume ratio**, making them more susceptible to the action of lidocaine.
*Touch*
- **Touch** sensation is mediated by a mix of **Aβ and Aδ fibers**; light touch is typically blocked relatively early due to the involvement of smaller fibers.
- However, **crude touch** often persists longer than pain and temperature but is usually blocked before pressure.
*Temperature*
- **Temperature** sensation is primarily carried by **Aδ and C fibers**, making it one of the **earliest sensations to be blocked** by local anesthetic.
- These fibers are generally small and have high sensitivity to local anesthetic agents.
*Sympathetic stimulation*
- **Sympathetic nerve fibers** are typically **small, unmyelinated C fibers** and are generally the **first to be blocked** by local anesthetics.
- This early blockade can lead to **vasodilation** in the area due to the loss of sympathetic tone.
Local anesthetics US Medical PG Question 7: A 45-year-old homeless man presents to the emergency department with a 1-week history of an intensely pruritic, red rash on his hands, wrists, and finger webs. The itching is worse at night. Physical examination reveals small, erythematous papules and burrows. A topical drug with which of the following mechanisms of action is most likely to be effective in treating this condition?
- A. Increase in keratinocyte turnover
- B. Inhibition of histamine-1 receptors
- C. Decrease in peptidoglycan synthesis
- D. Inhibition of nuclear factor-κB
- E. Binding to sodium channels (Correct Answer)
Local anesthetics Explanation: ***Binding to sodium channels***
- The clinical presentation of **intensely pruritic rash**, especially worse at night, with **burrows** on hands, wrists, and finger webs, is highly suggestive of **scabies**.
- Scabies is caused by the mite *Sarcoptes scabiei*, and treatment often involves **permethrin**, which acts by **binding to sodium channels** in the mite's nervous system, leading to paralysis and death.
*Increase in keratinocyte turnover*
- This mechanism of action is characteristic of drugs used to treat conditions like **psoriasis**, where the goal is to reduce rapid skin cell proliferation.
- It is not relevant for parasitic infestations like scabies, which require an agent to directly kill the mites.
*Inhibition of histamine-1 receptors*
- Antihistamines, which block H1 receptors, are used to alleviate **pruritus** associated with allergic reactions or other inflammatory skin conditions.
- While they can help with the *symptom* of itching, they do not address the underlying *cause* of scabies (the mite infestation itself).
*Decrease in peptidoglycan synthesis*
- This mechanism is characteristic of **antibiotics** like **penicillins** and **cephalosporins**, which target the bacterial cell wall.
- It is effective against bacterial infections but has no utility in treating parasitic infestations like scabies, which are caused by arthropods, not bacteria.
*Inhibition of nuclear factor-κB*
- **NF-κB** is a protein complex that controls **transcription of DNA**, cytokine production, and cell survival, and its inhibition is often targeted in **inflammatory diseases** or cancers.
- This mechanism is not directly involved in the eradication of scabies mites.
Local anesthetics US Medical PG Question 8: Which of the following statements regarding the patch shown in the figure is correct?
- A. It is an equal mixture of local anesthetics.
- B. Excessive use can result in methemoglobinemia. (Correct Answer)
- C. 5 ml of a 5 percent mixture contains 50 mg of lignocaine.
- D. It contains lignocaine and ropivacaine in a ratio of 50 percent each.
- E. It should be applied for at least 2 hours before minor procedures.
Local anesthetics Explanation: ***Excessive use can result in methemoglobinemia.***
- The patch shown is likely an **EMLA patch**, which contains **lidocaine** and **prilocaine**. Excessive absorption of prilocaine, especially with large doses or prolonged application, can lead to the formation of **methemoglobinemia**.
- **Prilocaine** is metabolized into **ortho-toluidine**, which is an oxidizing agent that can convert hemoglobin to methemoglobin, reducing the blood's oxygen-carrying capacity.
*It is an equal mixture of local anesthetics.*
- The EMLA patch is a 1:1 mixture of **lidocaine** and **prilocaine**, but the claim that it contains "an equal mixture of local anesthetics" is vague and could imply other compositions not specific to EMLA.
- While it's an equal ratio of two specific local anesthetics, the option's wording is not precise enough to be the *most correct* statement.
*5 ml of a 5 percent mixture contains 50 mg of lignocaine.*
- A 5% solution means 5 grams (5000 mg) per 100 ml. Therefore, 1 ml contains 50 mg of lignocaine.
- Thus, 5 ml of a 5% mixture would contain 250 mg of **lignocaine**, not 50 mg. This statement is mathematically incorrect.
*It contains lignocaine and ropivacaine in a ratio of 50 percent each.*
- **EMLA patches** contain **lidocaine** (lignocaine) and **prilocaine**, not ropivacaine.
- While it is a 50% concentration for each active ingredient, the specific combination of local anesthetics mentioned in this option is incorrect.
*It should be applied for at least 2 hours before minor procedures.*
- For most minor procedures, **EMLA cream** typically requires **30-60 minutes** of application time to achieve adequate topical anesthesia.
- While longer application times (up to 2 hours) may enhance depth of anesthesia for certain procedures, stating that it "should be applied for at least 2 hours" is excessive and not a standard recommendation for minor procedures.
Local anesthetics US Medical PG Question 9: A 4-year-old boy presents to the Emergency Department with wheezing and shortness of breath after playing with the new family pet. Which of the following immunological factors is most involved in generating the antibodies necessary for mast cell Fc-receptor cross-linking and degranulation?
- A. IL-5
- B. IL-13
- C. IL-2
- D. IL-4 (Correct Answer)
- E. IL-10
Local anesthetics Explanation: **IL-4**
- **IL-4** is a primary cytokine responsible for promoting **Th2 differentiation** and inducing **B cell class switching to IgE**, which is critical for allergic reactions.
- The IgE antibodies then bind to **Fc receptors on mast cells**, leading to cross-linking and degranulation upon re-exposure to the allergen.
*IL-5*
- **IL-5** is primarily involved in the growth, differentiation, and activation of **eosinophils**, which are important in late-phase allergic reactions and parasitic infections.
- While it plays a role in allergic inflammation, it does not directly drive the production of IgE antibodies crucial for initial mast cell sensitization.
*IL-13*
- **IL-13** shares many functions with IL-4, including promoting **IgE production** and contributing to airway hyperresponsiveness and mucus secretion in asthma.
- However, **IL-4** is considered the foundational cytokine for initial IgE class switching, even though IL-13 can synergize or contribute later.
*IL-2*
- **IL-2** is primarily known for its role in the **proliferation and differentiation of T cells**, including regulatory T cells, and general immune activation.
- It does not directly promote B cell class switching to IgE or directly induce allergic antibody production.
*IL-10*
- **IL-10** is an **immunosuppressive cytokine** that *inhibits* the production of pro-inflammatory cytokines and can downregulate immune responses.
- Its role is generally to *suppress* allergic responses rather than generate the antibodies (IgE) necessary for mast cell degranulation.
Local anesthetics US Medical PG Question 10: A 20-year-old woman presents to the emergency department after developing a widespread rash when she was playing in the park. She states she feels somewhat light-headed. She is otherwise healthy and has no significant past medical history. Her temperature is 97.0°F (36.1°C), blood pressure is 84/54 mmHg, pulse is 130/min, respirations are 22/min, and oxygen saturation is 95% on room air. Physical exam is notable for bilateral wheezing and a diffuse urticarial rash. Which of the following is the next best step in management?
- A. Normal saline
- B. Continuous monitoring
- C. Diphenhydramine
- D. Albuterol
- E. Epinephrine (Correct Answer)
Local anesthetics Explanation: ***Epinephrine***
- The patient presents with classic signs of **anaphylaxis**, including a widespread urticarial rash, wheezing, hypotension, and lightheadedness. **Epinephrine** is the first-line treatment for anaphylaxis due to its alpha-1 agonist effects (increasing blood pressure and reducing angioedema) and beta-2 agonist effects (bronchodilation).
- Delaying administration of **epinephrine** can lead to rapid progression of symptoms and potentially fatal outcomes.
*Normal saline*
- While **intravenous fluids** like normal saline may be indicated later to help manage hypotension in anaphylaxis, they are not the immediate priority.
- **Epinephrine** addresses the underlying pathophysiological processes of anaphylaxis more directly and quickly than fluid resuscitation alone.
*Continuous monitoring*
- While continuous monitoring is always important in unstable patients, it is not an intervention.
- The patient's vital signs and clinical presentation require immediate therapeutic intervention, not just observation.
*Diphenhydramine*
- **Diphenhydramine**, an H1 antihistamine, can help alleviate cutaneous symptoms like urticaria and pruritus.
- However, it does not address the life-threatening aspects of anaphylaxis, such as hypotension, bronchospasm, or upper airway edema, and should only be used as an adjunct to epinephrine.
*Albuterol*
- **Albuterol** is a beta-2 adrenergic agonist that can help with bronchospasm and wheezing.
- While it may be a useful adjunct, it does not address the cardiovascular collapse (hypotension) or the generalized systemic reaction of anaphylaxis, making epinephrine the more comprehensive and life-saving initial treatment.
More Local anesthetics US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.