Intravenous anesthetics US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Intravenous anesthetics. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Intravenous anesthetics US Medical PG Question 1: A 25-year-old female presents to the emergency room with a heart rate of 32 BPM and a blood pressure of 80/40. She was found by emergency medical services with an empty bottle of propranolol that was taken from her grandmother. Her vital signs do not improve despite IV fluids and oxygen. Which of the following is a first line treatment for overdose?
- A. Hemodialysis
- B. Adenosine
- C. Atropine
- D. Vagal maneuvers
- E. Glucagon (Correct Answer)
Intravenous anesthetics Explanation: ***Glucagon***
- **Glucagon** is the first-line antidote for severe beta-blocker overdose due to its ability to increase **intracellular cAMP** independently of beta-adrenergic receptors, thereby bypassing receptor blockade.
- This action leads to increased **heart rate** and **contractility**, improving hemodynamic stability.
*Hemodialysis*
- **Hemodialysis** is generally ineffective for propanolol overdose as it has a large volume of distribution and is highly protein-bound, making it difficult to clear from the body.
- It might be considered for other beta-blockers with different pharmacokinetic profiles but is not first-line for propanolol.
*Adenosine*
- **Adenosine** is contraindicated in beta-blocker overdose as it can worsen **bradycardia** and **hypotension** by directly inhibiting AV nodal conduction.
- Its action as an AV nodal blocker would exacerbate the patient's already compromised cardiac function.
*Atropine*
- **Atropine** may be used in beta-blocker overdose to counteract the **bradycardia** by blocking muscarinic receptors and increasing heart rate.
- However, it often provides only a partial or transient effect in severe beta-blocker toxicity and is not as effective as glucagon in restoring hemodynamic stability.
*Vagal maneuvers*
- **Vagal maneuvers** increase vagal tone, which would further slow the **heart rate** and worsen bradycardia in the context of beta-blocker overdose.
- They are used to terminate supraventricular tachycardias, not to treat bradycardia and hypotension from overdose.
Intravenous anesthetics US Medical PG Question 2: A 38-year-old man presents with sudden onset abdominal pain and undergoes an emergent laparoscopic appendectomy. The procedure is performed quickly, without any complications, and the patient is transferred to the post-operative care unit. A little while later, the patient complains of seeing people in his room and hearing voices talking to him. The patient has no prior medical or psychiatric history and does not take any regular medications. What is the mechanism of action of the anesthetic most likely responsible for this patient’s symptoms?
- A. Stimulation of μ-opioid receptors
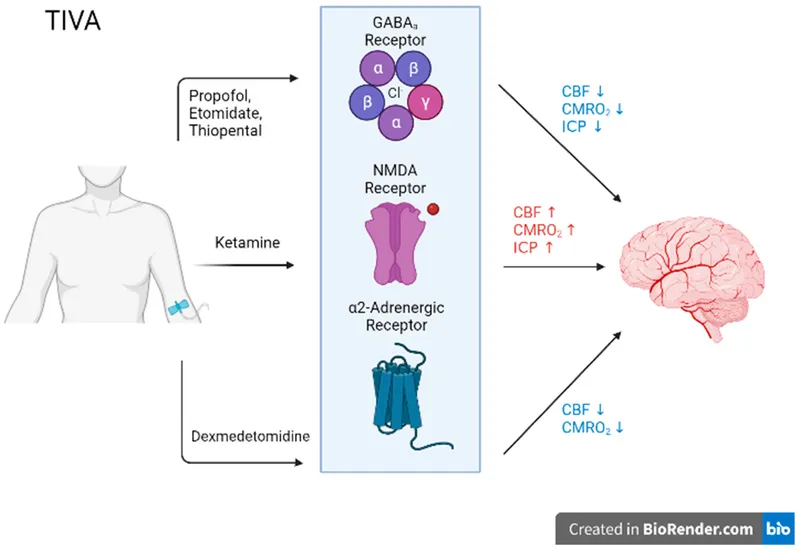
- B. N-methyl-D-aspartate receptor antagonism (Correct Answer)
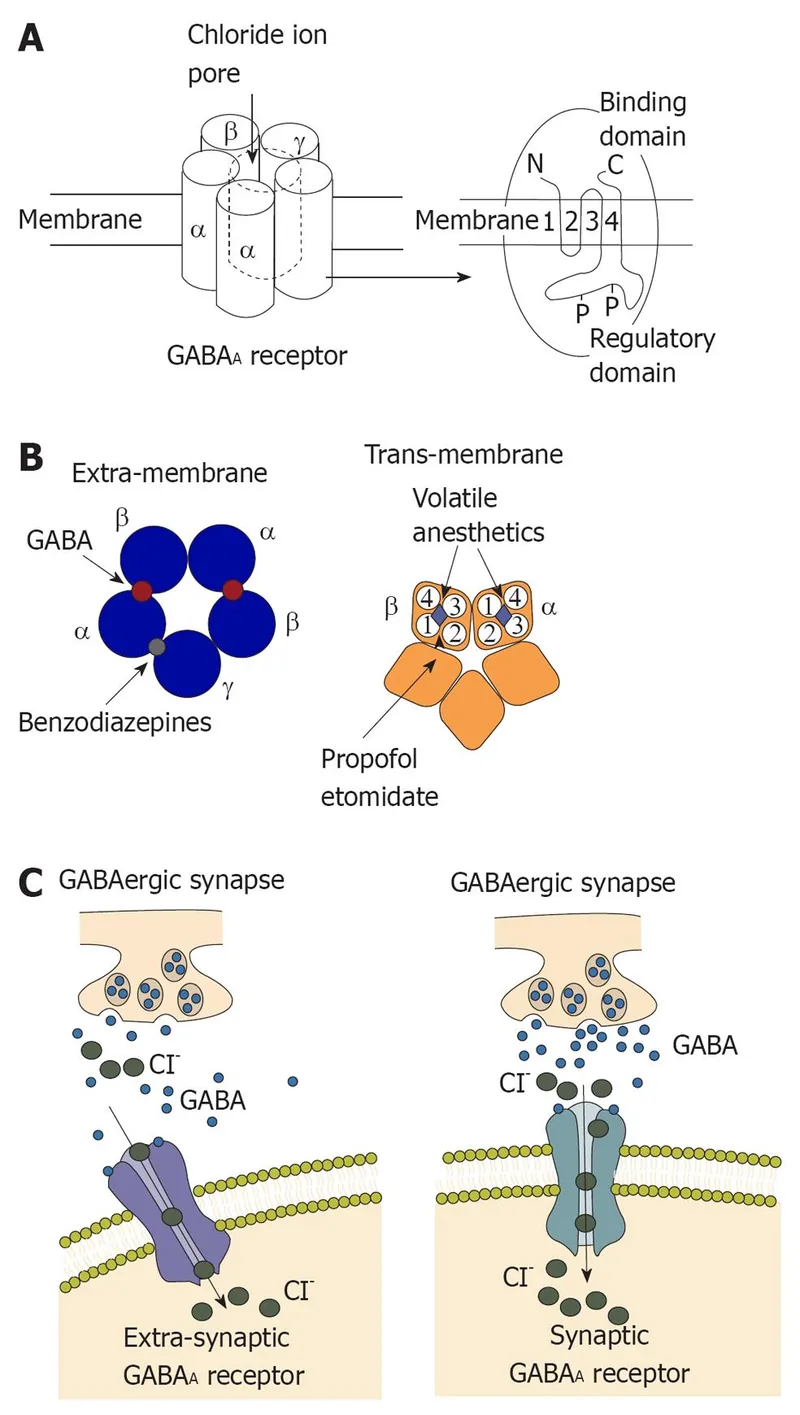
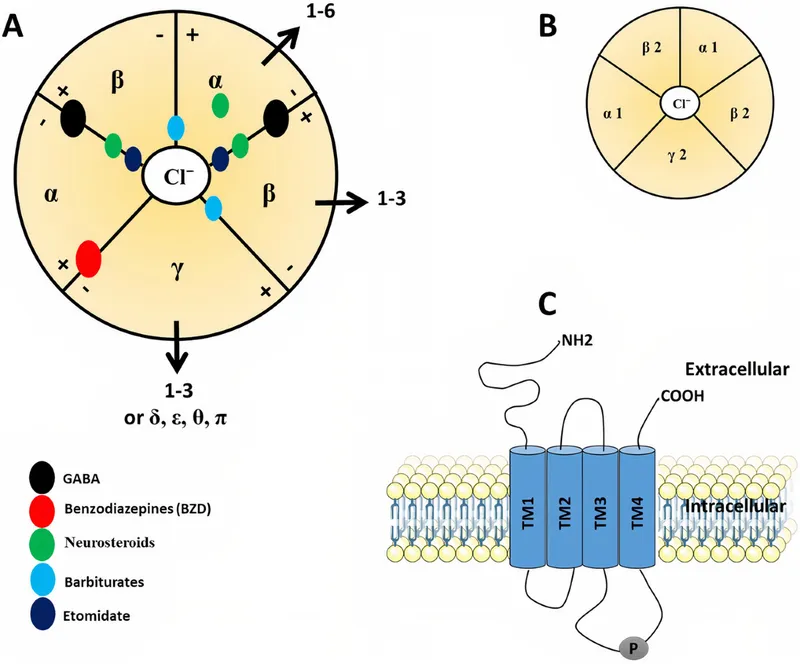
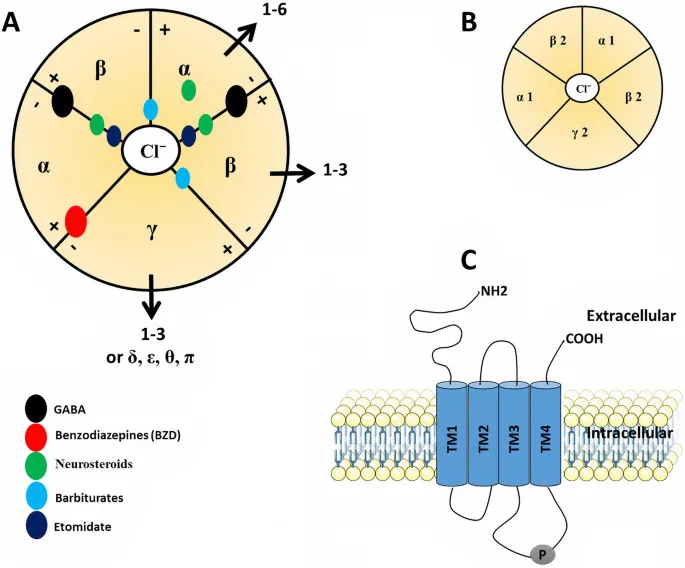
- C. Increased duration of GABA-gated chloride channel opening
- D. Blocking the fast voltage-gated Na+ channels
- E. Increased frequency of GABA-gated chloride channel opening
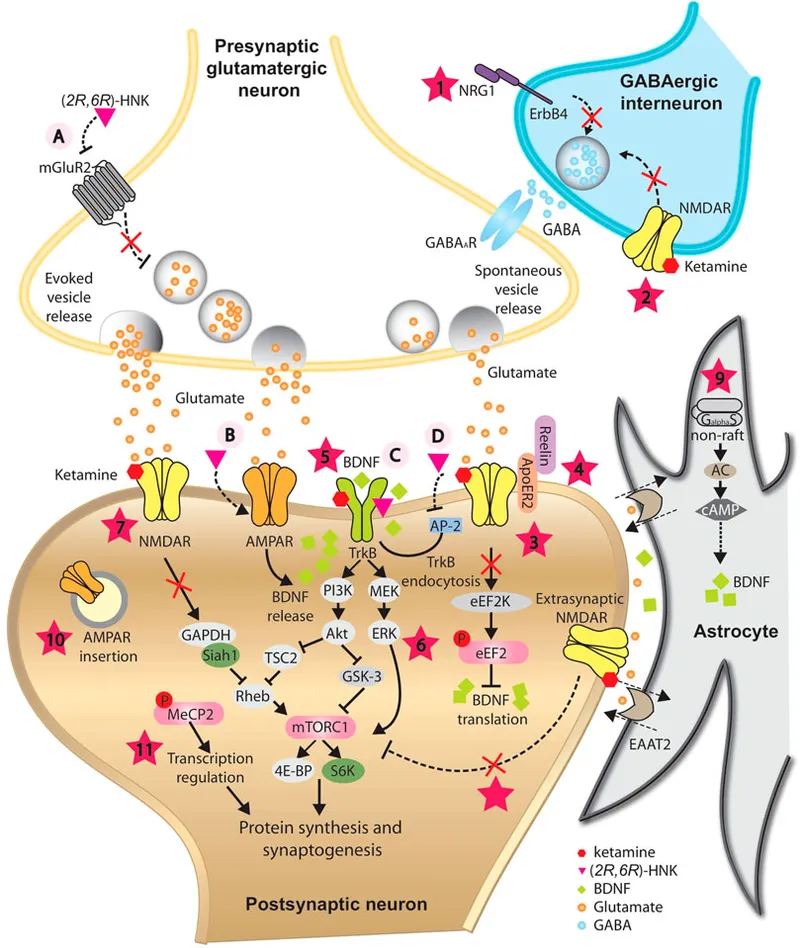
Intravenous anesthetics Explanation: ***N-methyl-D-aspartate receptor antagonism***
- The patient's symptoms of **hallucinations** and **auditory phenomena** post-anesthesia are characteristic of **emergence delirium**, often associated with **ketamine**.
- Ketamine acts primarily as an **NMDA receptor antagonist**, which can lead to dissociative anesthesia and psychomimetic effects upon emergence.
*Stimulation of μ-opioid receptors*
- Opioids primarily cause **analgesia**, respiratory depression, and sedation by stimulating **μ-opioid receptors**.
- While opioids can cause some central nervous system effects like confusion or nightmares, the severe **hallucinations** described are not typical for this mechanism.
*Increased duration of GABA-gated chloride channel opening*
- This mechanism describes the action of **benzodiazepines** which potentiate GABAergic neurotransmission by increasing the **frequency** of chloride channel opening, while **barbiturates** increase the **duration**.
- These drugs typically cause **sedation** and **anxiolysis**, not acute psychosis or vivid hallucinations upon emergence.
*Blocking the fast voltage-gated Na+ channels*
- This is the primary mechanism of action for **local anesthetics** and certain **antiarrhythmic drugs**, leading to inhibition of nerve impulse conduction.
- While some systemic toxicity can occur with local anesthetics, it typically manifests as **seizures** or cardiovascular collapse, not dissociative emergence phenomena.
*Increased frequency of GABA-gated chloride channel opening*
- This is the mechanism of action for **benzodiazepines**, which enhance GABA's inhibitory effects by increasing the **frequency** of chloride channel opening.
- Similar to increased duration of opening, this leads to **sedation** and anxiolysis, not the vivid hallucinations seen in this patient.
Intravenous anesthetics US Medical PG Question 3: A 44-year-old male is brought to the emergency department by fire and rescue after he was the unrestrained driver in a motor vehicle accident. His wife notes that the patient’s only past medical history is recent development of severe episodes of headache accompanied by sweating and palpitations. She says that these episodes were diagnosed as atypical panic attacks by the patient’s primary care provider, and the patient was started on sertraline and alprazolam. In the trauma bay, the patient’s temperature is 97.6°F (36.4°C), blood pressure is 81/56 mmHg, pulse is 127/min, and respirations are 14/min. He has a Glascow Coma Score (GCS) of 10. He is extremely tender to palpation in the abdomen with rebound and guarding. His skin is cool and clammy, and he has thready peripheral pulses. The patient's Focused Assessment with Sonography for Trauma (FAST) exam reveals bleeding in the perisplenic space, and he is taken for emergency laparotomy. He is found to have a ruptured spleen, and his spleen is removed. During manipulation of the bowel, the patient’s temperature is 97.8°F (36.6°C), blood pressure is 246/124 mmHg, and pulse is 104/min. The patient is administered intravenous labetalol, but his blood pressure continues to worsen. The patient dies during the surgery.
Which of the following medications would most likely have prevented this outcome?
- A. Lorazepam
- B. Propylthiouracil
- C. Phenoxybenzamine (Correct Answer)
- D. Dantrolene
- E. Phentolamine
Intravenous anesthetics Explanation: ***Phenoxybenzamine***
- This patient likely had an undiagnosed **pheochromocytoma**, which is a **catecholamine-secreting tumor**. The severe labile hypertension during surgery, unresponsive to labetalol, is a classic sign of a catecholamine surge.
- **Phenoxybenzamine** is an **irreversible alpha-adrenergic blocker** that would have been used pre-operatively to control blood pressure and prevent such a hypertensive crisis by blocking the effects of excess catecholamines.
*Lorazepam*
- **Lorazepam** is a **benzodiazepine** used for anxiety and seizure control. While it might have helped to calm the patient or manage panic, it would not address the underlying physiological cause of the hypertensive crisis associated with an endocrine tumor.
- Its effects on blood pressure are generally mild and would not counteract the massive catecholamine release seen in a pheochromocytoma.
*Propylthiouracil*
- **Propylthiouracil** is an **antithyroid medication** used to treat **hyperthyroidism**. There is no indication of thyroid dysfunction in this patient's presentation.
- The symptoms of palpitations and sweating are common to both pheochromocytoma and hyperthyroidism, but the rapid, extreme hypertensive crisis points away from thyroid storm and towards a catecholamine-secreting tumor.
*Dantrolene*
- **Dantrolene** is a **skeletal muscle relaxant** primarily used to treat and prevent **malignant hyperthermia**.
- There is no evidence in the clinical presentation to suggest malignant hyperthermia as the cause of this patient's deterioration; the extreme hypertension is the primary issue.
*Phentolamine*
- **Phentolamine** is a **reversible alpha-adrenergic blocker** used to manage hypertensive crises, particularly those due to pheochromocytoma or monoamine oxidase inhibitor interactions.
- While phentolamine could be used during a crisis, **phenoxybenzamine** is preferred for *pre-operative preparation* due to its longer-acting and irreversible blockade, preventing the crisis more effectively when surgery is anticipated for pheochromocytoma.
Intravenous anesthetics US Medical PG Question 4: A 26-year-old woman presents with an 8-month history of insomnia and anxiety. She says that she has difficulty sleeping and has feelings of impending doom linked to her difficult financial situation. No significant family history and no current medications. The patient was prescribed an 8-week supply of medication. She follows up 4 weeks later saying that she has increased anxiety and needs a refill. She says that over the past month, due to increasing anxiety levels, she started taking extra doses of her medication to achieve an anxiolytic effect. Which of the following medications was most likely prescribed to this patient?
- A. Triazolam (Correct Answer)
- B. Hydroxyzine
- C. Zolpidem
- D. Buspirone
- E. Propranolol
Intravenous anesthetics Explanation: ***Triazolam***
- Triazolam is a **short-acting benzodiazepine** commonly prescribed for insomnia, but its rapid onset and short duration can lead to **rebound anxiety** and dependence with chronic use, as seen with the patient's increased anxiety and need for a refill.
- The patient's need to take "extra doses...to achieve an anxiolytic effect" suggests the development of **tolerance** and dependence, which is characteristic of benzodiazepine misuse.
*Hydroxyzine*
- Hydroxyzine is a **first-generation antihistamine** with sedative and anxiolytic properties, often used for anxiety and insomnia due to its relatively low abuse potential.
- It does not typically cause the **rapid tolerance** and withdrawal symptoms (like increased anxiety needing extra doses) seen with benzodiazepines.
*Zolpidem*
- Zolpidem is a **non-benzodiazepine hypnotic** (Z-drug) that acts on GABA-A receptors and is commonly prescribed for insomnia.
- While it has **lower dependence potential** than benzodiazepines, the patient's presentation with rapid tolerance development and dose escalation for anxiolytic effect is more characteristic of **benzodiazepine use** rather than zolpidem, which primarily provides sedation without strong anxiolytic effects.
*Buspirone*
- Buspirone is an **anxiolytic** that works on serotonin receptors and is used for generalized anxiety disorder, but it has a **delayed onset of action** (weeks) and lacks the immediate anxiolytic effect that would lead to acute dose escalation.
- It has a **low potential for abuse** or dependence, making it an unlikely choice for a patient rapidly escalating doses for an immediate effect.
*Propranolol*
- Propranolol is a **beta-blocker** used to manage the physical symptoms of anxiety (e.g., tremors, palpitations), but it does not directly treat the psychological symptoms of anxiety or insomnia.
- It is not associated with **tolerance, dependence**, or the need for dose escalation to achieve an anxiolytic effect.
Intravenous anesthetics US Medical PG Question 5: A 3-year-old boy is brought in by his parents to the emergency department for lethargy and vomiting. The patient was fine until this afternoon, when his parents found him in the garage with an unlabeled open bottle containing an odorless liquid. On exam, the patient is not alert or oriented, but is responsive to touch and pain. The patient is afebrile and pulse is 90/min, blood pressure is 100/60 mmHg, and respirations are 20/min. Which of the following is an antidote for the most likely cause of this patient’s presentation?
- A. Glucagon
- B. Epinephrine
- C. Fomepizole (Correct Answer)
- D. Succimer
- E. Sodium bicarbonate
Intravenous anesthetics Explanation: ***Fomepizole***
- The patient's presentation with **lethargy**, **vomiting**, and altered mental status after unsupervised access to an **unlabeled, odorless liquid** highly suggests **toxic alcohol ingestion** (e.g., ethylene glycol or methanol).
- **Fomepizole** is a competitive inhibitor of **alcohol dehydrogenase**, preventing the metabolism of toxic alcohols into their highly toxic acid metabolites (oxalic acid, formic acid), thus reducing organ damage.
*Glucagon*
- **Glucagon** is primarily used to treat severe **hypoglycemia**, especially in patients who cannot tolerate oral glucose or if intravenous access is difficult.
- It is also indicated in the management of **beta-blocker overdose** to bypass beta-adrenergic receptors and increase cardiac contractility.
*Epinephrine*
- **Epinephrine** is a potent **vasopressor** and bronchodilator used in emergencies such as **anaphylaxis**, **cardiac arrest**, and severe asthma exacerbations.
- It works by stimulating alpha- and beta-adrenergic receptors, leading to vasoconstriction, increased heart rate, and bronchodilation.
*Succimer*
- **Succimer** is a **chelating agent** primarily used in the treatment of **lead poisoning** in children with blood lead levels above a certain threshold.
- It binds to lead ions, forming a stable complex that can be excreted in the urine.
*Sodium bicarbonate*
- **Sodium bicarbonate** is used to correct **metabolic acidosis**, which can occur in various conditions, including severe sepsis, diabetic ketoacidosis, and certain poisonings (e.g., salicylates, tricyclic antidepressants).
- While toxic alcohol ingestion can cause metabolic acidosis, sodium bicarbonate addresses the acidosis itself, not the underlying toxic alcohol metabolism, for which fomepizole is the specific antidote.
Intravenous anesthetics US Medical PG Question 6: A 28-year-old man comes to the emergency department for an injury sustained while doing construction. Physical examination shows a long, deep, irregular laceration on the lateral aspect of the left forearm with exposed fascia. Prior to surgical repair of the injury, a brachial plexus block is performed using a local anesthetic. Shortly after the nerve block is performed, he complains of dizziness and then loses consciousness. His radial pulse is faint and a continuous cardiac monitor shows a heart rate of 24/min. Which of the following is the most likely mechanism of action of the anesthetic that was administered?
- A. Activation of acetylcholine receptors
- B. Inactivation of ryanodine receptors
- C. Inactivation of sodium channels (Correct Answer)
- D. Activation of GABA receptors
- E. Inactivation of potassium channels
Intravenous anesthetics Explanation: ***Inactivation of sodium channels***
- Local anesthetics primarily work by reversibly blocking **voltage-gated sodium channels** in nerves.
- This prevents the influx of sodium ions, inhibiting the generation and propagation of **action potentials**, thus blocking pain signals.
- The clinical presentation of dizziness, loss of consciousness, and bradycardia represents systemic toxicity from intravascular absorption of the local anesthetic.
*Activation of acetylcholine receptors*
- Activation of **nicotinic or muscarinic acetylcholine receptors** is the primary mechanism of action for neuromuscular stimulants or parasympathomimetics, not local anesthetics.
- This would typically lead to muscle contraction or increased parasympathetic activity rather than analgesia and local nerve block.
*Inactivation of ryanodine receptors*
- Inactivation of **ryanodine receptors** primarily affects calcium release from the sarcoplasmic reticulum in muscle cells, crucial for excitation-contraction coupling.
- This mechanism is associated with drugs like dantrolene used for malignant hyperthermia, not local anesthetics.
*Activation of GABA receptors*
- Activation of **GABA-A receptors** is the primary mechanism of action for benzodiazepines and barbiturates, leading to widespread CNS depression and sedation.
- While systemic absorption of local anesthetics can cause CNS effects (as seen in toxicity), their primary therapeutic mechanism for nerve block is sodium channel inactivation, not GABA receptor activation.
*Inactivation of potassium channels*
- Inactivation of **potassium channels** would typically prolong repolarization and increase neuronal excitability or cause arrhythmias, depending on the specific channel.
- This is not the mechanism of action for local anesthetics, which prevent depolarization by blocking sodium channel activation.
Intravenous anesthetics US Medical PG Question 7: Which of the following statements regarding the patch shown in the figure is correct?
- A. It is an equal mixture of local anesthetics.
- B. Excessive use can result in methemoglobinemia. (Correct Answer)
- C. 5 ml of a 5 percent mixture contains 50 mg of lignocaine.
- D. It contains lignocaine and ropivacaine in a ratio of 50 percent each.
- E. It should be applied for at least 2 hours before minor procedures.
Intravenous anesthetics Explanation: ***Excessive use can result in methemoglobinemia.***
- The patch shown is likely an **EMLA patch**, which contains **lidocaine** and **prilocaine**. Excessive absorption of prilocaine, especially with large doses or prolonged application, can lead to the formation of **methemoglobinemia**.
- **Prilocaine** is metabolized into **ortho-toluidine**, which is an oxidizing agent that can convert hemoglobin to methemoglobin, reducing the blood's oxygen-carrying capacity.
*It is an equal mixture of local anesthetics.*
- The EMLA patch is a 1:1 mixture of **lidocaine** and **prilocaine**, but the claim that it contains "an equal mixture of local anesthetics" is vague and could imply other compositions not specific to EMLA.
- While it's an equal ratio of two specific local anesthetics, the option's wording is not precise enough to be the *most correct* statement.
*5 ml of a 5 percent mixture contains 50 mg of lignocaine.*
- A 5% solution means 5 grams (5000 mg) per 100 ml. Therefore, 1 ml contains 50 mg of lignocaine.
- Thus, 5 ml of a 5% mixture would contain 250 mg of **lignocaine**, not 50 mg. This statement is mathematically incorrect.
*It contains lignocaine and ropivacaine in a ratio of 50 percent each.*
- **EMLA patches** contain **lidocaine** (lignocaine) and **prilocaine**, not ropivacaine.
- While it is a 50% concentration for each active ingredient, the specific combination of local anesthetics mentioned in this option is incorrect.
*It should be applied for at least 2 hours before minor procedures.*
- For most minor procedures, **EMLA cream** typically requires **30-60 minutes** of application time to achieve adequate topical anesthesia.
- While longer application times (up to 2 hours) may enhance depth of anesthesia for certain procedures, stating that it "should be applied for at least 2 hours" is excessive and not a standard recommendation for minor procedures.
Intravenous anesthetics US Medical PG Question 8: You are a resident on an anesthesiology service and are considering using nitrous oxide to assist in placing a laryngeal mask airway (LMA) in your patient, who is about to undergo a minor surgical procedure. You remember that nitrous oxide has a very high minimal alveolar concentration (MAC) compared to other anesthetics. This means that nitrous oxide has:
- A. no effect on lipid solubility or potency
- B. decreased lipid solubility and decreased potency (Correct Answer)
- C. decreased lipid solubility and increased potency
- D. increased lipid solubility and increased potency
- E. increased lipid solubility and decreased potency
Intravenous anesthetics Explanation: ***Decreased lipid solubility and decreased potency***
- A **very high MAC** indicates that a large concentration of the anesthetic agent is required to produce immobility in 50% of patients, signifying **low potency**.
- According to the **Meyer-Overton rule**, anesthetic potency is directly correlated with lipid solubility; therefore, low potency implies **decreased lipid solubility**.
*No effect on lipid solubility or potency*
- This statement is incorrect as MAC is a direct measure of potency, and potency is linked to lipid solubility by the **Meyer-Overton rule**.
- A high MAC unequivocally indicates **low potency**, and indirectly, low lipid solubility.
*Decreased lipid solubility and increased potency*
- This is incorrect because **increased potency** would be associated with a **low MAC**.
- Potency and lipid solubility are positively correlated, so decreased lipid solubility would lead to **decreased potency**.
*Increased lipid solubility and increased potency*
- This is incorrect; while **increased lipid solubility** is associated with **increased potency**, increased potency would manifest as a **low MAC**, not a high one.
- The given information states a **very high MAC**, which signifies low potency.
*Increased lipid solubility and decreased potency*
- This statement contradicts the **Meyer-Overton rule**, which establishes a direct relationship between lipid solubility and anesthetic potency.
- Therefore, **increased lipid solubility** should correspond to **increased potency**, not decreased potency.
Intravenous anesthetics US Medical PG Question 9: A 5-year-old boy undergoes MRI neuroimaging for the evaluation of worsening headaches and intermittent nausea upon awakening. He receives a bolus of intravenous thiopental for sedation during the procedure. Ten minutes after the MRI, the patient is awake and responsive. Which of the following pharmacological properties is most likely responsible for this patient's rapid recovery from this anesthetic agent?
- A. First-pass metabolism
- B. Redistribution (Correct Answer)
- C. Zero-order elimination
- D. Ion trapping
- E. Cytochrome P450 oxidation
Intravenous anesthetics Explanation: ***Redistribution***
- Thiopental is a highly **lipid-soluble** drug that rapidly crosses the **blood-brain barrier**, leading to quick onset of action.
- The drug then rapidly **redistributes** from the brain to other highly perfused tissues (e.g., muscle, fat) and then less perfused tissues, causing a rapid decrease in drug concentration at the site of action and thus termination of the anesthetic effect.
*First-pass metabolism*
- This refers to the **metabolism of a drug** before it reaches systemic circulation, typically after oral administration, and does not explain the termination of action for an intravenously administered drug like thiopental.
- While thiopental is ultimately metabolized by the liver, this process is slower than redistribution and does not account for the **rapid awakening**.
*Zero-order elimination*
- **Zero-order elimination** occurs when a constant amount of drug is eliminated per unit of time, regardless of the drug's concentration, often seen with drug saturation of elimination pathways.
- Thiopental elimination follows **first-order kinetics** at therapeutic doses, meaning a constant fraction of the drug is eliminated per unit time, and this describes slower, overall elimination, not rapid recovery.
*Ion trapping*
- **Ion trapping** occurs when a drug accumulates in a compartment due to differences in pH across a membrane and the drug's pKa, leading to ionization and reduced ability to diffuse back.
- This mechanism is important for drug excretion or distribution into specific compartments (e.g., accumulation of basic drugs in acidic urine) but does not explain the **rapid termination of CNS effects** via redistribution.
*Cytochrome P450 oxidation*
- **Cytochrome P450 (CYP450) oxidation** is a major pathway for drug metabolism in the liver, which is responsible for the eventual elimination of thiopental from the body.
- While important for overall drug clearance, the rate of CYP450 oxidation is too slow to account for the **rapid awakening** seen after a single bolus dose of thiopental; redistribution is the primary factor for rapid recovery.
Intravenous anesthetics US Medical PG Question 10: A 42-year-old man is brought in to the emergency department by his daughter. She reports that her father drank heavily for the last 16 years, but he stopped 4 days ago after he decided to quit drinking on his birthday. She also reports that he has been talking about seeing cats running in his room since this morning, although there were no cats. There is no history of any known medical problems or any other substance use. On physical examination, his temperature is 38.4ºC (101.2ºF), heart rate is 116/min, blood pressure is 160/94 mm Hg, and respiratory rate is 22/min. He is severely agitated and is not oriented to his name, time, or place. On physical examination, profuse perspiration and tremors are present. Which of the following best describes the pathophysiologic mechanism underlying his condition?
- A. Increased influx of chloride ions
- B. Increased inhibition of norepinephrine
- C. Functional increase in GABA
- D. Increased activity of NMDA receptors (Correct Answer)
- E. Increased inhibition of glutamate
Intravenous anesthetics Explanation: ***Increased activity of NMDA receptors***
- Chronic alcohol use leads to **downregulation of GABA receptors** and **upregulation of NMDA receptors** to compensate for alcohol's inhibitory effects.
- When alcohol is withdrawn, the unopposed upregulation of NMDA receptors (and decreased GABA activity) causes a state of **neuronal hyperexcitability**, leading to symptoms like agitation, hallucinations, and autonomic hyperactivity seen in **delirium tremens**.
*Increased influx of chloride ions*
- This describes the mechanism of action of **GABA-A agonists** (like benzodiazepines), which enhance GABA's inhibitory effects by increasing chloride influx and hyperpolarizing neurons.
- In alcohol withdrawal, there is a **functional decrease in GABAergic activity**, not an increase in chloride ion influx.
*Increased inhibition of norepinephrine*
- **Norepinephrine** is a neurotransmitter associated with wakefulness, alertness, and autonomic responses; increased activity is seen in alcohol withdrawal, contributing to sympathetic overdrive.
- Increased inhibition of norepinephrine would lead to sedation and reduced autonomic activity, which is the opposite of the patient's presentation.
*Functional increase in GABA*
- **GABA** (gamma-aminobutyric acid) is the primary inhibitory neurotransmitter in the brain; alcohol enhances GABAergic activity.
- In alcohol withdrawal, there is a **functional decrease in GABAergic activity**, contributing to neuronal hyperexcitability and withdrawal symptoms.
*Increased inhibition of glutamate*
- **Glutamate** is the primary excitatory neurotransmitter, and its receptors (like NMDA) are implicated in alcohol withdrawal.
- Alcohol withdrawal is characterized by **increased excitatory activity**, including increased glutamate release and NMDA receptor activation, not increased inhibition of glutamate.
More Intravenous anesthetics US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.