GABA-enhancing antiepileptics US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for GABA-enhancing antiepileptics. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
GABA-enhancing antiepileptics US Medical PG Question 1: A 53-year-old woman is brought to the emergency department by her husband because of difficulty walking, slurred speech, and progressive drowsiness. The husband reports that his wife has appeared depressed over the past few days. She has a history of insomnia and social anxiety disorder. She appears lethargic. Her temperature is 36.2°C (97.1°F), pulse is 88/min, respirations are 12/min, and blood pressure is 110/80 mm Hg. Neurologic examination shows normal pupils. There is diffuse hypotonia and decreased deep tendon reflexes. Administration of a drug that acts as a competitive antagonist at which of the following receptors is most likely to reverse this patient's symptoms?
- A. D2 dopamine receptor
- B. Muscarinic acetylcholine receptor
- C. 5-hydroxytryptamine2 receptor
- D. GABAA receptor (Correct Answer)
- E. Ryanodine receptor
GABA-enhancing antiepileptics Explanation: ***GABAA receptor***
- The patient's symptoms of **sedation**, **slurred speech**, **ataxia** (difficulty walking), **diffuse hypotonia**, and **decreased deep tendon reflexes** are classic signs of **benzodiazepine overdose**.
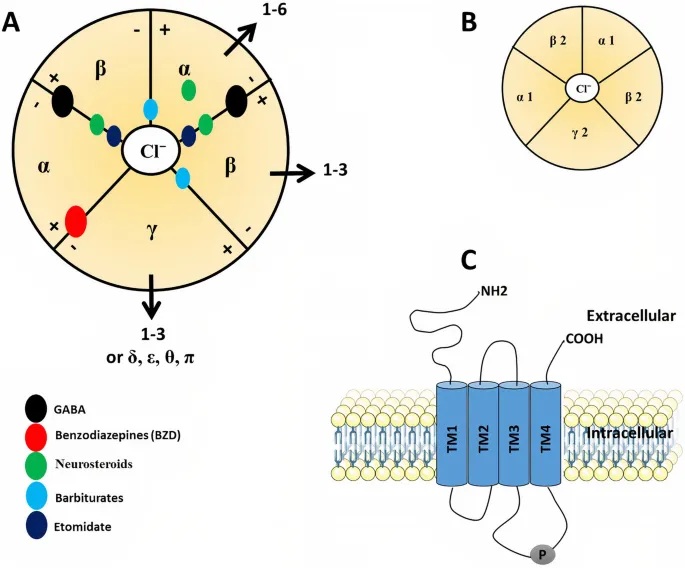
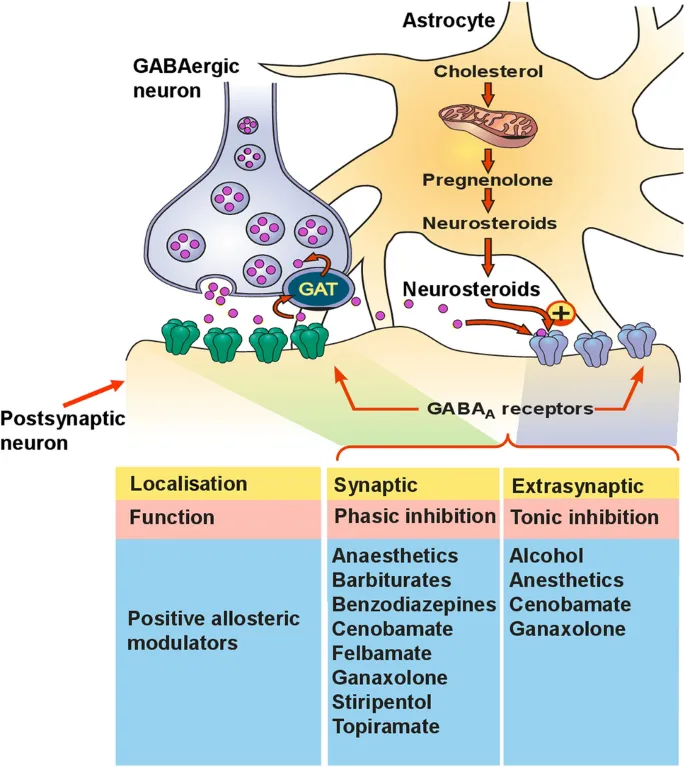
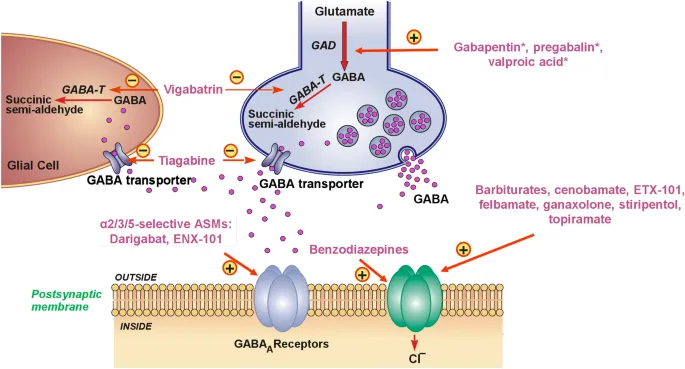
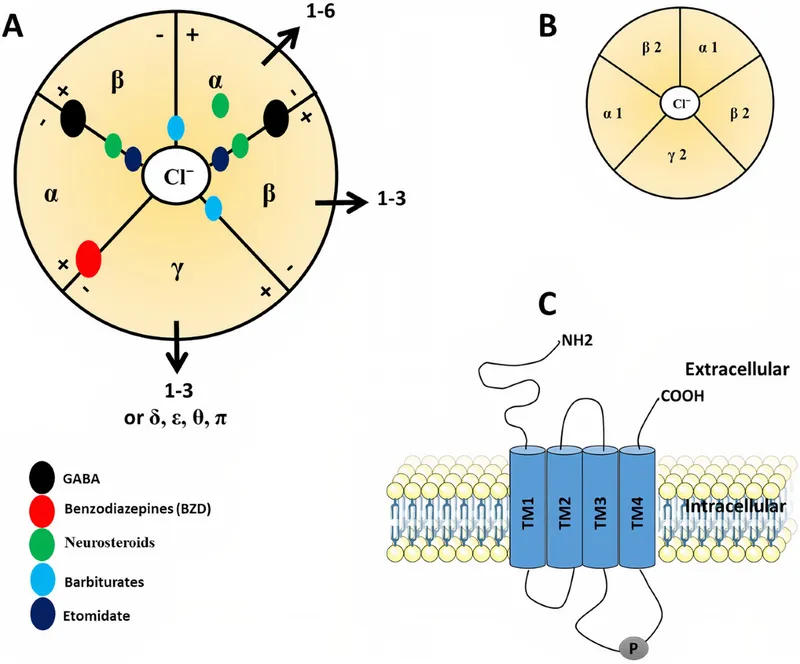
- **Benzodiazepines** act as **positive allosteric modulators** at the GABA-A receptor, enhancing the effects of GABA and increasing chloride influx, leading to neuronal hyperpolarization and central nervous system depression. A **competitive antagonist** like **flumazenil** can reverse these effects.
*D2 dopamine receptor*
- Antagonism of **D2 dopamine receptors** is associated with **antipsychotic medications** and can lead to **extrapyramidal symptoms** or neuroleptic malignant syndrome, which do not match the patient's presentation.
- While dopamine receptors are involved in mood, their acute antagonism would not explain the rapid-onset, severe CNS depression described.
*Muscarinic acetylcholine receptor*
- **Muscarinic antagonists** (e.g., atropine, scopolamine) cause anticholinergic effects like **dry mouth**, **mydriasis**, **tachycardia**, and **delirium**, which are not observed in this patient.
- Reversal of these receptors would only be indicated in cases of anticholinergic toxicity, not the present signs of CNS depression.
*5-hydroxytryptamine2 receptor*
- **5-HT2 receptor antagonists** are used in some antipsychotics or for migraine prophylaxis, and their primary effects are not central nervous system depression of this nature.
- Overactivation or inhibition of these receptors does not typically manifest with the specific constellation of symptoms seen here (hypotonia, decreased reflexes, prominent sedation).
*Ryanodine receptor*
- **Ryanodine receptors** are primarily involved in **calcium release from the sarcoplasmic reticulum** in muscle cells, playing a role in muscle contraction.
- Drugs acting on these receptors (e.g., dantrolene for malignant hyperthermia) affect muscle tone and contractility, but not the broad CNS depression symptoms presented in this case.
GABA-enhancing antiepileptics US Medical PG Question 2: A 7-year-old boy is brought to the physician because of spells of unresponsiveness and upward rolling of the eyes for 2 months. The episodes start abruptly and last a few seconds. During that time he does not hear anyone’s voice or make any purposeful movements. When the episodes end, he continues what he was doing before the spell. He does not lose his posture or fall to the ground. Episodes occur multiple times during the day. Physical examination shows no abnormal findings. An EEG following hyperventilation shows 3 Hz spike-and-slow-wave discharges. Which of the following is the most appropriate pharmacotherapy at this time?
- A. No pharmacotherapy at this time
- B. Ethosuximide (Correct Answer)
- C. Sodium valproate
- D. Oxcarbazepine
- E. Lamotrigine
GABA-enhancing antiepileptics Explanation: ***Ethosuximide***
- The described clinical picture (brief unresponsiveness, eye-rolling, continuing activity afterward, frequent daily episodes, normal physical exam, and 3-Hz spike-and-slow-wave discharges on EEG during hyperventilation) is classic for **childhood absence epilepsy**.
- **Ethosuximide** is the first-line and most effective treatment specifically for absence seizures due to its selective action on T-type calcium channels in the thalamus, which are implicated in the generation of absence seizures.
*No pharmacotherapy at this time*
- Leaving childhood absence epilepsy untreated can lead to significant impairments in learning, attention, and cognitive development due to the frequent, brief interruptions in consciousness.
- Given the clear diagnostic criteria including characteristic EEG findings and frequent episodes, initiating appropriate pharmacotherapy is medically indicated and crucial for the child's well-being.
*Sodium valproate*
- While **sodium valproate** is effective against absence seizures and has a broader spectrum of action against other seizure types, it is often considered a second-line agent for absence epilepsy due to potential side effects.
- Its use may be preferred if there are co-occurring generalized tonic-clonic seizures or if ethosuximide is not tolerated or effective, but for isolated absence seizures, ethosuximide has a better side effect profile.
*Oxcarbazepine*
- **Oxcarbazepine** is a sodium channel blocker primarily used for focal (partial onset) seizures and secondarily generalized tonic-clonic seizures.
- It is generally ineffective and can sometimes *worsen* absence seizures, making it an inappropriate choice for this diagnosis.
*Lamotrigine*
- **Lamotrigine** is a broad-spectrum antiepileptic drug effective for various seizure types, including focal, generalized tonic-clonic, and some forms of atypical absence seizures.
- While it can be used for absence seizures, it is generally considered a second-line or add-on therapy, especially when ethosuximide or valproate are ineffective or not tolerated, or if there are co-existing seizure types. It is not the most appropriate first-line choice for classic childhood absence epilepsy.
GABA-enhancing antiepileptics US Medical PG Question 3: A 24-year-old man is brought to the emergency department because of violent jerky movements of his arms and legs that began 30 minutes ago. His father reports that the patient has a history of epilepsy. He is not responsive. Physical examination shows alternating tonic jerks and clonic episodes. There is blood in the mouth. Administration of intravenous lorazepam is begun. In addition, treatment with a second drug is started that alters the flow of sodium ions across neuronal membranes. The second agent administered was most likely which of the following drugs?
- A. Lamotrigine
- B. Phenobarbital
- C. Topiramate
- D. Carbamazepine
- E. Fosphenytoin (Correct Answer)
GABA-enhancing antiepileptics Explanation: ***Fosphenytoin***
- This patient is experiencing **status epilepticus** as evidenced by prolonged tonic-clonic seizures. **Lorazepam** is the first-line short-acting benzodiazepine for acute seizure termination, but a second, longer-acting antiepileptic drug is needed for maintenance.
- **Fosphenytoin** is a prodrug of **phenytoin** that can be administered intravenously; **phenytoin** works by blocking **voltage-sensitive sodium channels**, thereby altering the flow of sodium ions and stabilizing neuronal membranes.
*Lamotrigine*
- While **lamotrigine** does block voltage-gated sodium channels, it is primarily used for **partial seizures** and **generalized tonic-clonic seizures** as a maintenance therapy, not typically as an acute treatment for status epilepticus.
- It requires **slow titration** due to the risk of severe skin reactions (e.g., Stevens-Johnson syndrome), making it unsuitable for immediate use in status epilepticus.
*Phenobarbital*
- **Phenobarbital** is an antiepileptic drug that enhances **GABAergic neurotransmission**, leading to neuronal hyperpolarization and reduced excitability. It is a very effective and older anticonvulsant.
- Although it can be used for status epilepticus, it acts primarily on GABA receptors, not directly on **sodium ion channels** as described in the question.
*Topiramate*
- **Topiramate** has multiple mechanisms of action, including blocking voltage-gated sodium channels and enhancing GABA activity, but it is typically used as a **maintenance therapy** for various seizure types.
- It is not a first-line agent for acute management of **status epilepticus** and its primary mechanism mentioned isn't restricted to sodium channel modulation as explicitly as phenytoin.
*Carbamazepine*
- **Carbamazepine** is a sodium channel blocker, similar to phenytoin, and is effective for **partial** and **tonic-clonic seizures**.
- However, it is primarily an **oral medication** and its slow absorption makes it inappropriate for acute intravenous treatment of status epilepticus.
GABA-enhancing antiepileptics US Medical PG Question 4: A 16-year-old boy with history of seizure disorder is rushed to the Emergency Department with multiple generalized tonic-clonic seizures that have spanned more than 30 minutes in duration. He has not regained consciousness between these episodes. In addition to taking measures to ensure that he maintains adequate respiration, which of the following is appropriate for initial pharmacological therapy?
- A. Carbamazepine
- B. Gabapentin
- C. Lorazepam (Correct Answer)
- D. Valproic acid
- E. Phenytoin
GABA-enhancing antiepileptics Explanation: ***Lorazepam***
- This patient is experiencing **status epilepticus**, defined by continuous seizures lasting over 5 minutes or recurrent seizures without regaining consciousness. **Intravenous benzodiazepines**, like lorazepam, are the first-line treatment due to their rapid onset of action on GABA receptors.
- **Lorazepam** is preferred over other benzodiazepines in this setting due to its relatively **longer duration of action** and availability as an intravenous formulation, effectively terminating the acute seizure.
*Carbamazepine*
- **Carbamazepine** is an oral **anti-epileptic drug** used for long-term control of focal seizures, but it is not suitable for acute management of status epilepticus due to its **slow onset of action** and lack of intravenous formulation for rapid effect.
- It works by blocking **voltage-gated sodium channels**, which is not the primary mechanism for immediate seizure termination in an emergency.
*Gabapentin*
- **Gabapentin** is an anti-epileptic medication primarily used for focal seizures and neuropathic pain, and is **not effective** in treating acute generalized tonic-clonic seizures or status epilepticus.
- Its mechanism of action involves modulation of **calcium channels** and GABA, but it has a **slow onset** and limited efficacy in acute seizure termination.
*Valproic acid*
- **Valproic acid** can be used in the long-term management of various seizure types, including generalized tonic-clonic seizures, and has an intravenous formulation, but it is **not the first-line choice for immediate termination** of status epilepticus.
- Benzodiazepines are typically administered first, and if they fail, valproic acid can be considered as a **second-line agent** along with other antiepileptics.
*Phenytoin*
- **Phenytoin** is a classic anti-epileptic drug that can be used intravenously as a **second-line agent** for status epilepticus if benzodiazepines are unsuccessful.
- It has a slower onset of action compared to benzodiazepines and carries risks such as **cardiac arrhythmias** and **hypotension** with rapid infusion, making it less ideal for initial therapy.
GABA-enhancing antiepileptics US Medical PG Question 5: A 21-year-old female is brought by her brother to the emergency department after having a generalized tonic-clonic seizure one hour ago. She is slightly confused and has no recollection of her seizure. Her brother relayed that the patient has a history of severe anxiety for which she takes medication. For the past several days, he noticed that his sister exhibited body tremors, appeared to be agitated with quick mood changes, and, at times, was delirious. He states his sister recently ran out of her medications while visiting from out of town. Which of the following would best treat the patient's condition?
- A. Varenicline
- B. Naloxone
- C. Methadone
- D. Diazepam (Correct Answer)
- E. Flumazenil
GABA-enhancing antiepileptics Explanation: ***Diazepam***
- The patient's presentation suggests **benzodiazepine withdrawal**, characterized by anxiety, tremors, agitation, mood swings, delirium, and seizures. **Diazepam**, a long-acting benzodiazepine, is the most appropriate treatment to reverse these withdrawal symptoms.
- Benzodiazepines work by enhancing the effect of **GABA** (gamma-aminobutyric acid), an inhibitory neurotransmitter, and withdrawal leads to a state of neuronal hyperexcitability.
*Varenicline*
- **Varenicline** is a medication used for **smoking cessation**.
- It acts as a partial agonist at nicotinic acetylcholine receptors and is not indicated for benzodiazepine withdrawal.
*Naloxone*
- **Naloxone** is an **opioid antagonist** used to reverse opioid overdose.
- It has no role in the management of benzodiazepine withdrawal.
*Methadone*
- **Methadone** is a long-acting opioid agonist primarily used for **opioid dependence treatment** and chronic pain management.
- It is not indicated for treating benzodiazepine withdrawal symptoms.
*Flumazenil*
- **Flumazenil** is a **benzodiazepine receptor antagonist** (competitive antagonist at the benzodiazepine binding site on the GABA-A receptor) used to reverse benzodiazepine overdose.
- Administering **flumazenil** in a patient with benzodiazepine dependence can precipitate or worsen withdrawal symptoms, including seizures, and is therefore contraindicated.
GABA-enhancing antiepileptics US Medical PG Question 6: A neuroscientist is delivering a lecture on the electrophysiology of the brain. He talks about neuroreceptors which act as ion channels in the neurons. He mentions a specific receptor, which is both voltage-gated and ligand-gated ion channel. Which of the following receptors is most likely to be the one mentioned by the neuroscientist?
- A. NMDA receptor (Correct Answer)
- B. GABAA receptor
- C. AMPA receptor
- D. Nicotinic acetylcholine receptor
- E. Glycine receptor
GABA-enhancing antiepileptics Explanation: ***NMDA receptor***
- The **NMDA receptor** is unique among ionotropic glutamate receptors as it functions as both a **ligand-gated** and **voltage-gated** ion channel.
- It requires both the binding of an excitatory neurotransmitter (like **glutamate**) and a sufficient **depolarization** of the postsynaptic membrane to remove a **magnesium ion (Mg2+) block** from its pore.
*GABAA receptor*
- The **GABAA receptor** is a **ligand-gated ion channel** that opens upon binding of the neurotransmitter **GABA**, leading to an influx of chloride ions and neuronal hyperpolarization.
- It is primarily responsible for **inhibitory synaptic transmission** in the central nervous system.
*AMPA receptor*
- The **AMPA receptor** is an ionotropic glutamate receptor that is primarily **ligand-gated**, opening swiftly upon binding of **glutamate** to allow sodium and potassium ion flow.
- While it contributes to depolarization, it is generally not considered to have a significant **voltage-gating** mechanism like the NMDA receptor.
*Nicotinic acetylcholine receptor*
- The **nicotinic acetylcholine receptor** is a **ligand-gated ion channel** that opens in response to the binding of **acetylcholine**, initiating fast excitatory synaptic transmission.
- It is **not voltage-gated** in the same manner as the NMDA receptor; its opening is primarily dependent on neurotransmitter binding.
*Glycine receptor*
- The **glycine receptor** is a **ligand-gated chloride channel** that mediates fast inhibitory synaptic transmission in the spinal cord and brainstem.
- Its activation by **glycine** leads to an influx of chloride ions, causing hyperpolarization, and it does not exhibit significant voltage-gating properties.
GABA-enhancing antiepileptics US Medical PG Question 7: A 34-year-old woman is brought to the emergency department by fire and rescue after an apparent suicide attempt. She reports ingesting several pills 6 hours prior to presentation but cannot recall what they were. No pills were found on the scene. She complains of severe malaise, ringing in her ears, and anxiety. Her past medical history is notable for bipolar disorder, generalized anxiety disorder, rheumatoid arthritis, obesity, and diabetes. She takes lithium, methotrexate, metformin, and glyburide. She has a reported history of benzodiazepine and prescription opioid abuse. Her temperature is 102.2°F (39°C), blood pressure is 135/85 mmHg, pulse is 110/min, and respirations are 26/min. On exam, she appears diaphoretic and pale. Results from an arterial blood gas are shown:
pH: 7.48
PaCO2: 32 mmHg
HCO3-: 23 mEq/L
This patient should be treated with which of the following?
- A. Ammonium chloride
- B. Atropine
- C. Sodium bicarbonate (Correct Answer)
- D. Flumazenil
- E. Physostigmine
GABA-enhancing antiepileptics Explanation: ***Sodium bicarbonate***
- This patient presents with symptoms highly suggestive of **salicylate (aspirin) overdose**: tinnitus, tachypnea, hyperthermia, altered mental status, and **respiratory alkalosis** on ABG.
- **Sodium bicarbonate** is the treatment of choice to **alkalinize the urine** (target pH 7.5-8.0), which increases renal excretion of salicylates by trapping the ionized form in the urine.
- Salicylate toxicity initially causes **respiratory alkalosis** (direct stimulation of the respiratory center), and can progress to **metabolic acidosis** in severe cases due to uncoupling of oxidative phosphorylation.
*Ammonium chloride*
- **Ammonium chloride** is an acidifying agent and would be **contraindicated** in salicylate toxicity.
- Acidifying the urine would increase reabsorption of salicylate and worsen toxicity.
- It has limited use in toxicology for enhancing excretion of basic drugs, but not applicable here.
*Atropine*
- **Atropine** is an anticholinergic agent used to treat bradycardia or organophosphate/cholinergic poisoning.
- It is not indicated for salicylate toxicity and would not address the patient's acid-base disturbance or enhance drug elimination.
*Flumazenil*
- **Flumazenil** is a benzodiazepine receptor antagonist used to reverse **benzodiazepine overdose**.
- While the patient has a history of benzodiazepine abuse, her presentation (tinnitus, hyperthermia, tachypnea, respiratory alkalosis) is classic for **salicylate toxicity**, not benzodiazepine overdose.
- Flumazenil also carries risk of precipitating seizures in patients with chronic benzodiazepine use.
*Physostigmine*
- **Physostigmine** is a cholinesterase inhibitor used to treat **anticholinergic toxicity** (e.g., from antihistamines, TCAs).
- The patient's symptoms are inconsistent with anticholinergic poisoning (which would present with hyperthermia, dry skin, mydriasis, urinary retention, altered mental status).
- This patient has diaphoresis and tachypnea, more consistent with salicylate toxicity.
GABA-enhancing antiepileptics US Medical PG Question 8: A 75-year-old man with a seizure disorder is brought to the emergency department by a friend because of progressive confusion over the past two weeks. He is unable to provide any history. His vital signs are within normal limits. He appears lethargic and is only oriented to person. Oral mucosa is moist. There is no jugular venous distention. A basic metabolic panel shows a serum sodium concentration of 115 mEq/L but is otherwise normal. Serum osmolality is low and antidiuretic hormone level is elevated. X-ray of the chest shows no abnormalities. Which of the following is the most likely cause of this patient’s hyponatremia?
- A. Aldosterone deficiency
- B. Medication effect (Correct Answer)
- C. Low cardiac output
- D. Insulin deficiency
- E. Excess cortisol
GABA-enhancing antiepileptics Explanation: ***Medication effect***
- This patient's **hyponatremia** with **appropriately low serum osmolality** and **elevated antidiuretic hormone (ADH)** levels, in the absence of signs of hypovolemia or fluid overload, points to the **syndrome of inappropriate ADH secretion (SIADH)**.
- Many medications, including anti-epileptic drugs like carbamazepine or oxcarbazepine (commonly used for seizure disorders), as well as selective serotonin reuptake inhibitors (SSRIs), can cause SIADH.
*Aldosterone deficiency*
- **Aldosterone deficiency** would likely lead to **hyperkalemia** and metabolic acidosis, which are not mentioned in the basic metabolic panel as being abnormal.
- While it can cause hyponatremia due to inability to retain sodium, the elevated ADH level with normal volume status points away from primary aldosterone deficiency.
*Low cardiac output*
- **Low cardiac output** can lead to hyponatremia by decreased renal perfusion and activation of the renin-angiotensin-aldosterone system and ADH release.
- However, this patient has **normal vital signs** and **no jugular venous distention**, making significant low cardiac output and resultant hypovolemia less likely.
*Insulin deficiency*
- **Insulin deficiency** (as seen in uncontrolled diabetes) typically leads to **hyperglycemia** and can cause a **pseudohyponatremia** due to osmotic effects, or true hyponatremia due to polyuria and volume depletion.
- The basic metabolic panel is otherwise normal, suggesting no significant hyperglycemia or electrolyte abnormalities consistent with insulin deficiency.
*Excess cortisol*
- **Excess cortisol** (Cushing's syndrome) typically leads to **hyperglycemia**, hypertension, and features of fat redistribution, muscular weakness, and thin skin, none of which are detailed here.
- It does not directly cause hyponatremia; conversely, cortisol has some mineralocorticoid effects and typically opposes ADH action, so severe excess would more likely cause hypernatremia or normal sodium levels.
GABA-enhancing antiepileptics US Medical PG Question 9: A patient on SSRI sertraline was also prescribed amitriptyline and subsequently developed serotonin toxicity. What is the likely treatment for serotonin toxicity?
- A. Flumazenil
- B. Cyproheptadine (Correct Answer)
- C. L-Carnitine
- D. Leucovorin
- E. Naloxone
GABA-enhancing antiepileptics Explanation: ***Cyproheptadine***
- **Cyproheptadine** is a serotonin antagonist that can help reverse the effects of excessive serotonin in the central nervous system.
- It works by blocking **serotonin 5-HT2A receptors**, which are implicated in the pathophysiology of serotonin toxicity.
*Flumazenil*
- **Flumazenil** is a benzodiazepine receptor antagonist used to reverse the effects of benzodiazepine overdose.
- It has no role in the treatment of **serotonin toxicity**, as it does not affect serotonin pathways.
*L-Carnitine*
- **L-Carnitine** is a mitochondrial co-factor used in fatty acid metabolism, sometimes supplemented for certain metabolic disorders or muscle pain.
- It does not have any direct action on **serotonin receptors** or the serotonin system, making it ineffective for serotonin toxicity.
*Leucovorin*
- **Leucovorin** (folinic acid) is used to counteract the effects of methotrexate toxicity or to enhance the effects of fluorouracil in chemotherapy.
- It is not involved in modulating **neurotransmitter levels** or reversing the symptoms of serotonin toxicity.
*Naloxone*
- **Naloxone** is an opioid receptor antagonist used to reverse opioid overdose.
- It has no effect on **serotonin receptors** or serotonergic pathways, making it ineffective for treating serotonin toxicity.
GABA-enhancing antiepileptics US Medical PG Question 10: A 34-year-old woman with a history of depression is brought to the emergency department by her husband 45 minutes after ingesting an unknown amount of a termite poison in a suicide attempt. She has abdominal pain, nausea, and vomiting. Her husband reports that she has had two episodes of watery diarrhea on the way to the emergency department. A distinct, garlic-like odor on the breath is noted on examination. An ECG shows sinus tachycardia and QTc prolongation. Administration of which of the following is most appropriate?
- A. Deferoxamine
- B. Dimercaprol (Correct Answer)
- C. Fomepizole
- D. N-acetylcysteine
- E. Physostigmine
GABA-enhancing antiepileptics Explanation: ***Dimercaprol***
- The patient's symptoms (abdominal pain, nausea, vomiting, watery diarrhea, garlic-like odor on breath, QTc prolongation, and ingestion of termite poison) are highly suggestive of **acute arsenic poisoning**.
- **Dimercaprol** (BAL) is a chelating agent indicated for severe arsenic poisoning by forming stable renally excreted complexes with arsenic.
*Deferoxamine*
- Is a chelating agent primarily used for **iron overdose** by binding to free iron in the bloodstream.
- It is not effective for arsenic poisoning and would not address the patient's specific symptoms.
*Fomepizole*
- Is an **alcohol dehydrogenase inhibitor** used in cases of **methanol** or **ethylene glycol poisoning** to prevent the formation of toxic metabolites.
- It has no role in the management of arsenic poisoning due to a different mechanism of toxicity.
*N-acetylcysteine*
- Is an antidote primarily used for **acetaminophen overdose** by replenishing glutathione stores, and as a mucolytic.
- It is not indicated for arsenic poisoning and would not mitigate the toxic effects of arsenic.
*Physostigmine*
- Is an **acetylcholinesterase inhibitor** used to reverse anticholinergic toxicity.
- The patient's symptoms are not consistent with anticholinergic poisoning, and physostigmine would be inappropriate and potentially harmful.
More GABA-enhancing antiepileptics US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.