Nicotinic antagonists US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Nicotinic antagonists. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Nicotinic antagonists US Medical PG Question 1: A 50-year-old male is brought to the dermatologist's office with complaints of a pigmented lesion. The lesion is uniformly dark with clean borders and no asymmetry and has been increasing in size over the past two weeks. He works in construction and spends large portions of his day outside. The dermatologist believes that this mole should be biopsied. To prepare the patient for the biopsy, the dermatologist injects a small amount of lidocaine into the skin around the lesion. Which of the following nerve functions would be the last to be blocked by the lidocaine?
- A. Pain
- B. Touch
- C. Temperature
- D. Sympathetic stimulation
- E. Pressure (Correct Answer)
Nicotinic antagonists Explanation: ***Pressure***
- **Pressure** sensation is mediated by **Aβ fibers**, which are relatively **larger** and **myelinated**, making them more resistant to local anesthetic blockade.
- Nerve fibers are blocked in a specific order, typically starting with smaller, unmyelinated fibers and ending with larger, myelinated fibers.
*Pain*
- **Pain** sensation is primarily carried by **unmyelinated C fibers** and **small myelinated Aδ fibers**, which are among the **first to be blocked** by local anesthetics.
- These fibers have a **high surface-to-volume ratio**, making them more susceptible to the action of lidocaine.
*Touch*
- **Touch** sensation is mediated by a mix of **Aβ and Aδ fibers**; light touch is typically blocked relatively early due to the involvement of smaller fibers.
- However, **crude touch** often persists longer than pain and temperature but is usually blocked before pressure.
*Temperature*
- **Temperature** sensation is primarily carried by **Aδ and C fibers**, making it one of the **earliest sensations to be blocked** by local anesthetic.
- These fibers are generally small and have high sensitivity to local anesthetic agents.
*Sympathetic stimulation*
- **Sympathetic nerve fibers** are typically **small, unmyelinated C fibers** and are generally the **first to be blocked** by local anesthetics.
- This early blockade can lead to **vasodilation** in the area due to the loss of sympathetic tone.
Nicotinic antagonists US Medical PG Question 2: Which receptor type mediates the slow phase of synaptic transmission in autonomic ganglia?
- A. Muscarinic (M3)
- B. Muscarinic (M2)
- C. Muscarinic (M1) (Correct Answer)
- D. Nicotinic (N2)
Nicotinic antagonists Explanation: ***Muscarinic (M1)***
- **M1 receptors** are **Gq-protein coupled receptors** that activate phospholipase C, leading to increased intracellular calcium and diacylglycerol, which mediates the slow excitatory postsynaptic potential in autonomic ganglia.
- This activation results in a **slow depolarization** that prolongs the excitability of ganglionic neurons after the initial fast synaptic transmission.
*Muscarinic (M3)*
- **M3 receptors** are primarily found on **smooth muscle**, glands, and endothelium, mediating contraction, secretion, and vasodilation, respectively.
- While also **Gq-protein coupled**, their role in autonomic ganglia is not the main mediator of the slow phase of synaptic transmission.
*Muscarinic (M2)*
- **M2 receptors** are **Gi-protein coupled receptors** mainly found in the heart, mediating decreased heart rate and contractility.
- In autonomic ganglia, M2 receptors could have a modulatory role, but they are not responsible for the slow excitatory phase of synaptic transmission.
*Nicotinic (N2)*
- **Nicotinic N2 receptors** (also known as **NN or neuronal nicotinic receptors**) mediate the **fast excitatory postsynaptic potential** (EPSP) in autonomic ganglia by opening ion channels.
- This leads to rapid depolarization and action potential generation, which is distinct from the **slower, prolonged phase** of transmission.
Nicotinic antagonists US Medical PG Question 3: A 37-year-old woman undergoes diagnostic laparoscopy under general anesthesia for evaluation of chronic pelvic pain. Postoperatively, the patient requires prolonged intubation. Neostigmine is administered. Results of acceleromyography during train-of-four ulnar nerve stimulation are shown. Which of the following drugs is most likely to have been used intraoperatively in this patient?
- A. Tizanidine
- B. Clonazepam
- C. Ropivacaine
- D. Succinylcholine (Correct Answer)
- E. Rocuronium
Nicotinic antagonists Explanation: ***Succinylcholine***
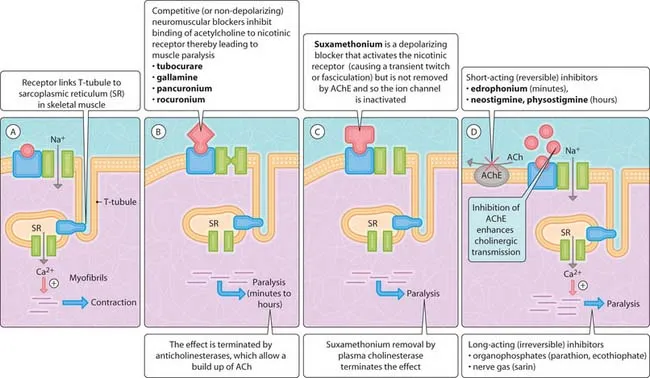
- The scenario describes a patient requiring **prolonged intubation** and the administration of **neostigmine** for neuromuscular blockade reversal, along with **acceleromyography** results.
- This constellation points to the use of a **depolarizing neuromuscular blocker** like succinylcholine, especially if the patient has atypical plasma **pseudocholinesterase activity**, leading to prolonged paralysis.
*Tizanidine*
- Tizanidine is an **alpha-2 adrenergic agonist** used as a centrally acting muscle relaxant.
- It does not cause neuromuscular blockade that requires reversal with **neostigmine** or monitoring with **acceleromyography** during general anesthesia.
*Clonazepam*
- Clonazepam is a **benzodiazepine** used as an anxiolytic and anticonvulsant.
- It acts on **GABA-A receptors** in the central nervous system and does not directly affect the neuromuscular junction.
*Ropivacaine*
- Ropivacaine is a **local anesthetic** that blocks voltage-gated sodium channels in nerve membranes.
- It is used for regional anesthesia or epidurals and does not cause generalized neuromuscular paralysis requiring such reversal.
*Rocuronium*
- Rocuronium is a **nondepolarizing neuromuscular blocker**, which would also cause neuromuscular blockade.
- However, the description of prolonged intubation followed by neostigmine (an anticholinesterase) could indicate **phase II block** from rocuronium, but the phrasing more strongly suggests **succinylcholine** given the potential for prolonged action due to pseudocholinesterase deficiency.
Nicotinic antagonists US Medical PG Question 4: A 16-year-old boy is brought to the emergency department by ambulance with a visible deformity of the upper thigh after being involved in a motor vehicle collision. He is informed that he will require surgery and is asked about his medical history. He mentions that he had surgery to remove his tonsils several years ago and at that time suffered a complication during the surgery. Specifically, shortly after the surgery began, he began to experience severe muscle contractions and an increased body temperature. Based on this information, a different class of muscle relaxants are chosen for use during the upcoming surgery. If these agents needed to be reversed, the reversal agent should be administered with which of the following to prevent off-target effects?
- A. Atropine (Correct Answer)
- B. Epinephrine
- C. Echothiophate
- D. Methacholine
- E. Phentolamine
Nicotinic antagonists Explanation: **Atropine**
- The patient's history of **severe muscle contractions** and **increased body temperature** during prior surgery indicates **malignant hyperthermia**, a contraindication for succinylcholine
- Therefore, **nondepolarizing neuromuscular blockers** will be used instead and reversal is typically achieved with **neostigmine** (acetylcholinesterase inhibitor)
- Neostigmine increases acetylcholine at **both nicotinic and muscarinic receptors**, causing undesirable **muscarinic side effects** (bradycardia, salivation, bronchospasm, increased GI motility)
- **Atropine** or **glycopyrrolate** (muscarinic antagonists) must be co-administered to prevent these off-target muscarinic effects
*Epinephrine*
- Sympathomimetic acting on **alpha- and beta-adrenergic receptors** used for anaphylaxis, severe asthma, and cardiac arrest
- Not used to prevent muscarinic side effects of acetylcholinesterase inhibitors
*Echothiophate*
- **Irreversible acetylcholinesterase inhibitor** used for glaucoma treatment
- Would exacerbate rather than prevent cholinergic side effects when combined with neostigmine
*Methacholine*
- **Muscarinic cholinergic agonist** used in bronchial challenge tests for asthma diagnosis
- Would worsen muscarinic side effects rather than preventing them
*Phentolamine*
- **Alpha-adrenergic blocker** used for hypertensive crises from pheochromocytoma or vasopressor extravasation
- No role in managing muscarinic side effects of acetylcholinesterase inhibitors
Nicotinic antagonists US Medical PG Question 5: A 25-year-old man is scheduled for an orthopedic surgery. His routine preoperative laboratory tests are within normal limits. An urticarial reaction occurs when a non-depolarizing neuromuscular blocking agent is injected for muscle relaxation and mechanical ventilation. The patient’s lungs are manually ventilated with 100% O2 by bag and mask and then through an endotracheal tube. After a few minutes, edema of the face and neck rapidly ensues and giant hives appear over most of his body. Which of the following neuromuscular blocking agents was most likely used in this operation?
- A. Ketamine
- B. Succinylcholine
- C. Nitrous oxide
- D. Neostigmine
- E. D-tubocurarine (Correct Answer)
Nicotinic antagonists Explanation: ***D-tubocurarine***
- The rapid onset of widespread **urticaria**, facial and neck **edema**, and giant hives immediately after injection of a **non-depolarizing neuromuscular blocking agent** strongly points to an **anaphylactic reaction**. d-Tubocurarine is a historical non-depolarizing neuromuscular blocker that is known for its propensity to cause **histamine release**, leading to severe hypersensitivity reactions including anaphylaxis and therefore is rarely used today.
- The symptoms described are classic signs of a severe allergic reaction, which is a known and significant side effect of d-tubocurarine due to its potent histamine-releasing properties.
*Ketamine*
- **Ketamine** is a dissociative anesthetic, not a neuromuscular blocking agent. It primarily affects the central nervous system, producing a trance-like state, pain relief, sedation, and amnesia.
- While it can cause some cardiovascular stimulation, it does not typically induce **histamine release** leading to anaphylactic-like reactions as described with neuromuscular blockers.
*Succinylcholine*
- **Succinylcholine** is a depolarizing neuromuscular blocker that can cause adverse effects like **hyperkalemia**, malignant hyperthermia, and muscle pain.
- Although it can rarely trigger an allergic reaction, it is not primarily known for causing widespread **histamine release** and anaphylaxis like d-tubocurarine.
*Nitrous oxide*
- **Nitrous oxide** is an inhalational anesthetic gas used for sedation and analgesia; it is not a neuromuscular blocking agent.
- Its adverse effects are generally related to its anesthetic properties, such as nausea and vomiting, and it does not cause **allergic reactions** of this nature.
*Neostigmine*
- **Neostigmine** is an acetylcholinesterase inhibitor used to **reverse the effects of non-depolarizing neuromuscular blockers**, not as a blocking agent itself.
- It increases acetylcholine levels at the neuromuscular junction; its side effects are typically cholinergic, such as bradycardia, salivation, and bronchospasm, and it does not cause anaphylaxis from histamine release.
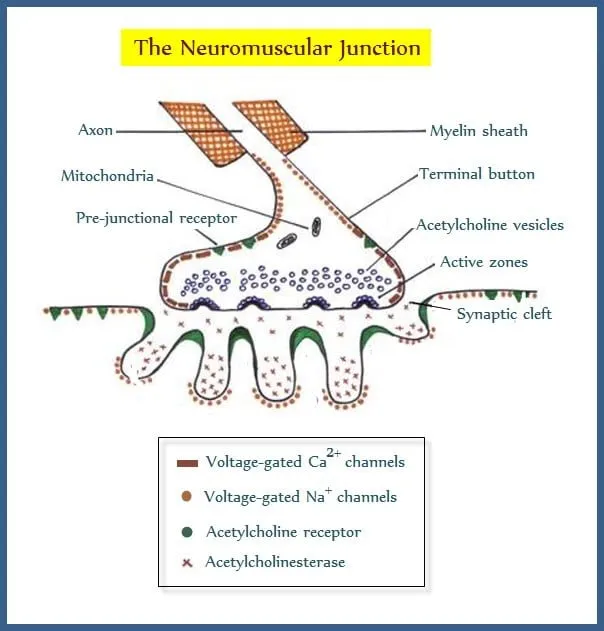
Nicotinic antagonists US Medical PG Question 6: A neurophysiology expert is teaching his students the physiology of the neuromuscular junction. While describing the sequence of events that takes place at the neuromuscular junction, he mentions that as the action potential travels down the motor neuron, it causes depolarization of the presynaptic membrane. This results in the opening of voltage-gated calcium channels, which leads to an influx of calcium into the synapse of the motor neuron. Consequently, the cytosolic concentration of Ca2+ ions increases. Which of the following occurs at the neuromuscular junction as a result of this increase in cytosolic Ca2+?
- A. Generation of an end plate potential
- B. Exocytosis of acetylcholine from the synaptic vesicles (Correct Answer)
- C. Increased Na+ and K+ conductance of the motor end plate
- D. Binding of Ca2+ ions to NM receptors
- E. Release of Ca2+ ions into the synaptic cleft
Nicotinic antagonists Explanation: ***Exocytosis of acetylcholine from the synaptic vesicles***
- The increase in **cytosolic Ca2+** within the presynaptic terminal is the primary trigger for the fusion of **synaptic vesicles** filled with **acetylcholine (ACh)** with the presynaptic membrane.
- This fusion process, known as **exocytosis**, releases ACh into the **synaptic cleft**, initiating synaptic transmission.
*Generation of an end plate potential*
- The **end plate potential (EPP)** is generated *after* acetylcholine (ACh) is released into the synaptic cleft and binds to receptors on the motor end plate.
- This event occurs *following* the Ca2+-induced release of neurotransmitter, not as a direct result of the Ca2+ increase itself.
*Increased Na+ and K+ conductance of the motor end plate*
- Increased **Na+ and K+ conductance** across the motor end plate membrane is a direct consequence of acetylcholine binding to its receptors, which are **ligand-gated ion channels**.
- This change in conductance *generates the end plate potential*, occurring after ACh release.
*Binding of Ca2+ ions to NM receptors*
- **NM receptors** (nicotinic muscle receptors) are located on the **postsynaptic membrane** (motor end plate) and bind to **acetylcholine (ACh)**, not Ca2+ ions.
- Calcium's primary role in this context is presynaptic: triggering ACh release.
*Release of Ca2+ ions into the synaptic cleft*
- Calcium ions enter the **presynaptic terminal** from the synaptic cleft, and their increased cytosolic concentration within the presynaptic terminal drives neurotransmitter release.
- Calcium itself is not released *into* the synaptic cleft in this process; rather, it enters the presynaptic neuron from the cleft.
Nicotinic antagonists US Medical PG Question 7: A 23-year-old man is brought to the emergency department by ambulance following a motor vehicle accident. He was pinned between 2 cars for several hours. The patient has a history of asthma. He uses an albuterol inhaler intermittently. The patient was not the driver, and admits to having a few beers at a party prior to the accident. His vitals in the ambulance are stable. Upon presentation to the emergency department, the patient is immediately brought to the operating room for evaluation and surgical intervention. It is determined that the patient’s right leg has a Gustilo IIIC injury in the mid-shaft of the tibia with a severely comminuted fracture. The patient’s left leg suffered a similar injury but with damage to the peroneal nerve. The anesthesiologist begins to induce anesthesia. Which of the following agents would be contraindicated in this patient?
- A. Halothane
- B. Propofol
- C. Etomidate
- D. Succinylcholine (Correct Answer)
- E. Neostigmine
Nicotinic antagonists Explanation: ***Succinylcholine***
- Given the history of the patient being pinned between two cars for several hours, there is a significant risk of **rhabdomyolysis** and subsequent hyperkalemia.
- **Succinylcholine**, a depolarizing neuromuscular blocker, can cause a sudden and significant release of potassium from muscle cells, leading to **life-threatening hyperkalemia** in patients with rhabdomyolysis or crush injuries.
*Halothane*
- While **halothane** has been associated with **malignant hyperthermia**, the patient's history does not directly suggest an increased risk for this condition here.
- It also has a bronchodilating effect, which could be beneficial for a patient with a history of **asthma**.
*Propofol*
- **Propofol** is a commonly used intravenous anesthetic for induction and maintenance, providing rapid onset and recovery.
- There are generally no specific contraindications for propofol in a patient with a crush injury or asthma.
*Etomidate*
- **Etomidate** is an intravenous anesthetic agent known for its **cardiovascular stability**, making it a good choice for hemodynamically unstable patients.
- It can cause adrenal suppression, but this is usually a concern with prolonged infusions, not a single induction dose.
*Neostigmine*
- **Neostigmine** is an acetylcholinesterase inhibitor used to reverse the effects of non-depolarizing neuromuscular blockers.
- It is not an induction agent and would not be used at the beginning of anesthesia induction.
Nicotinic antagonists US Medical PG Question 8: Which of the following statements is correct regarding the given graph?
- A. Drug 1 represents agonist and drug 2 represents inverse agonist
- B. Drug 3 represents agonist and drug 4 represents inverse agonist
- C. Drug 2 represents partial agonist and drug 3 represents inverse agonist
- D. Drug 1 represents agonist and drug 4 represents inverse agonist (Correct Answer)
Nicotinic antagonists Explanation: ***Drug 1 represents agonist and drug 4 represent inverse agonist***
- **Drug 1** demonstrates maximal efficacy, producing a **supraphysiologic response** above the baseline (100%), characteristic of an **agonist**.
- **Drug 4** produces a response **below the baseline** (100%), indicating inhibition of constitutive receptor activity, which is the definition of an **inverse agonist**.
*Drug 1 represents agonist and drug 2 represents inverse agonist*
- While **Drug 1** is correctly identified as an **agonist** due to its maximal effect above baseline, **Drug 2** is a **partial agonist**, as it produces a submaximal effect above baseline but does not reach the full agonist's efficacy.
- **Drug 2** does not reduce the baseline response, so it cannot be an inverse agonist.
*Drug 3 represents agonist and drug 4 represents inverse agonist*
- **Drug 3** maintains the **baseline response** (at 100%) regardless of concentration, indicating it is a **neutral antagonist** or has no effect, not an agonist.
- **Drug 4** is correctly identified as an **inverse agonist** because it reduces the baseline receptor activity.
*Drug 2 represents partial agonist and drug 3 represents inverse agonist*
- **Drug 2** is correctly identified as a **partial agonist** as it produces an effect above baseline but less than a full agonist.
- **Drug 3** is incorrect; it shows no change from baseline (100%), reflecting a **neutral antagonist** or inactive substance, not an inverse agonist which would decrease the baseline response.
Nicotinic antagonists US Medical PG Question 9: Which of the following is true regarding nicotine substitution therapy?
- A. Preferably given by gastrointestinal route.
- B. Varenicline comes with a black box warning of cardiovascular death
- C. There should be a 15-minute gap between nicotine gum and coffee/soda/acidic food as they decrease its absorption (Correct Answer)
- D. Nicotine chewing gum is better for constant use as it gives 25% higher blood level than lozenges
Nicotinic antagonists Explanation: ***There should be a 15-minute gap between nicotine gum and coffee/soda/acidic food as they decrease its absorption***
- **Acidic beverages** like coffee, soda, and fruit juices can alter the pH of the mouth and stomach, which significantly **reduces the absorption of nicotine** from gum.
- This recommendation ensures optimal **nicotine delivery** and effectiveness of the therapy in reducing withdrawal symptoms.
*Preferably given by gastrointestinal route*
- Nicotine has poor bioavailability when taken orally due to **extensive first-pass metabolism** in the liver.
- Nicotine substitution therapies are therefore preferentially administered via **transdermal**, **buccal** (gum, lozenges), or **nasal routes** to bypass first-pass metabolism and achieve therapeutic blood levels more effectively.
*Varenicline comes with a black box warning of cardiovascular death*
- Varenicline (Chantix) previously had a black box warning for **neuropsychiatric side effects**, including suicidal ideation and depression, which has since been removed due to further studies.
- It does not carry a black box warning specifically for **cardiovascular death**, though cardiovascular events have been a subject of study, particularly in patients with pre-existing cardiovascular conditions.
*Nicotine chewing gum is better for constant use as it gives 25% higher blood level than lozenges*
- While both nicotine gum and lozenges are effective, the **blood levels achieved are comparable**, and the choice often depends on patient preference and proper technique.
- Nicotine gum is best used with a **"chew and park" technique** to allow buccal absorption, and constant chewing can lead to excessive swallowing of nicotine, causing gastrointestinal upset.
Nicotinic antagonists US Medical PG Question 10: A 26-year-old man is brought to the hospital by his wife who complains that her husband has been behaving oddly for the past few hours. The patient’s wife says that she has known him for only 4 months. The wife is unable to give any past medical history. The patient’s speech is difficult to follow, and he seems very distracted. After 15 minutes, he becomes agitated and starts to bang his head on a nearby pillar. He is admitted to the psychiatric ward and is given an emergency medication, after which he calms down. In the next 2 days, he continues to become agitated at times and required 2 more doses of the same drug. On the 4th day of admission, he appears very weak, confused, and does not respond to questions appropriately. His vital signs include: temperature 40.0°C (104.0°F), blood pressure 160/95 mm Hg, and pulse 114/min. On physical examination, he is profusely diaphoretic. He is unable to stand upright or even get up from his bed. Which of the following is the mechanism of action of the drug which most likely caused this patient’s current condition?
- A. Skeletal muscle relaxation
- B. Agonistic effect on dopamine receptors
- C. Serotonin reuptake inhibition
- D. Histamine H2 receptor blocking
- E. Dopamine receptor blocking (Correct Answer)
Nicotinic antagonists Explanation: ***Dopamine receptor blocking***
- The patient's presentation with **fever, altered mental status, muscle rigidity**, and **autonomic instability** (tachycardia, hypertension, diaphoresis) after receiving antipsychotic medication strongly suggests **neuroleptic malignant syndrome (NMS)**.
- NMS is caused by a severe decrease in **dopaminergic activity**, primarily due to the blockade of **D2 dopamine receptors** in the basal ganglia and hypothalamus by antipsychotics.
- The classic tetrad of NMS includes: **hyperthermia, muscle rigidity, altered mental status**, and **autonomic instability**.
*Skeletal muscle relaxation*
- While agitation might be treated with benzodiazepines, which cause muscle relaxation, this mechanism does not explain the **severe rigidity, hyperthermia**, and **autonomic dysfunction** seen in the patient.
- **Muscle rigidity** (lead-pipe rigidity) is a hallmark of the patient's current condition, contradicting the idea of muscle relaxation.
*Agonistic effect on dopamine receptors*
- An agonistic effect on dopamine receptors would typically lead to symptoms similar to **psychosis** or **mania**, not the severe rigidity and hypodopaminergic state observed in NMS.
- This mechanism would counteract the effects of antipsychotics and would not cause NMS.
*Serotonin reuptake inhibition*
- This is the mechanism of action for **SSRIs**, and an excess of serotonin can lead to **serotonin syndrome**, which shares some features with NMS but typically includes **hyperreflexia** and **myoclonus**, rather than lead-pipe rigidity.
- The context of treating acute psychosis with an emergency medication points more towards an antipsychotic, not an antidepressant.
*Histamine H2 receptor blocking*
- **Histamine H2 receptor blockers** are used to treat conditions like **acid reflux** and **peptic ulcers**; they have no direct neurological effects that would cause NMS.
- This mechanism is entirely irrelevant to the patient's psychiatric symptoms and subsequent severe adverse reaction.
More Nicotinic antagonists US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.