Neuromuscular blocking agents US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Neuromuscular blocking agents. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Neuromuscular blocking agents US Medical PG Question 1: Which receptor type mediates the slow phase of synaptic transmission in autonomic ganglia?
- A. Muscarinic (M3)
- B. Muscarinic (M2)
- C. Muscarinic (M1) (Correct Answer)
- D. Nicotinic (N2)
Neuromuscular blocking agents Explanation: ***Muscarinic (M1)***
- **M1 receptors** are **Gq-protein coupled receptors** that activate phospholipase C, leading to increased intracellular calcium and diacylglycerol, which mediates the slow excitatory postsynaptic potential in autonomic ganglia.
- This activation results in a **slow depolarization** that prolongs the excitability of ganglionic neurons after the initial fast synaptic transmission.
*Muscarinic (M3)*
- **M3 receptors** are primarily found on **smooth muscle**, glands, and endothelium, mediating contraction, secretion, and vasodilation, respectively.
- While also **Gq-protein coupled**, their role in autonomic ganglia is not the main mediator of the slow phase of synaptic transmission.
*Muscarinic (M2)*
- **M2 receptors** are **Gi-protein coupled receptors** mainly found in the heart, mediating decreased heart rate and contractility.
- In autonomic ganglia, M2 receptors could have a modulatory role, but they are not responsible for the slow excitatory phase of synaptic transmission.
*Nicotinic (N2)*
- **Nicotinic N2 receptors** (also known as **NN or neuronal nicotinic receptors**) mediate the **fast excitatory postsynaptic potential** (EPSP) in autonomic ganglia by opening ion channels.
- This leads to rapid depolarization and action potential generation, which is distinct from the **slower, prolonged phase** of transmission.
Neuromuscular blocking agents US Medical PG Question 2: During a nerve conduction study, which of the following ions is primarily responsible for the rapid upstroke of the action potential?
- A. Calcium
- B. Sodium (Correct Answer)
- C. Chloride
- D. Potassium
Neuromuscular blocking agents Explanation: ***Sodium***
- The rapid upstroke of an **action potential** (depolarization) in nerves is primarily due to the rapid influx of **sodium ions** (Na+) into the cell.
- This influx occurs through **voltage-gated sodium channels** that open in response to a threshold stimulus.
*Calcium*
- **Calcium ions** (Ca2+) play a significant role in neurotransmitter release at the **synaptic terminals** and in cardiac and smooth muscle action potentials.
- However, they are not the primary ion responsible for the initial rapid **depolarization** in peripheral nerve conduction.
*Chloride*
- **Chloride ions** (Cl-) are generally involved in maintaining the resting membrane potential and mediating **inhibitory postsynaptic potentials** (IPSPs) by causing hyperpolarization or preventing depolarization.
- They do not contribute to the rapid upstroke of an **action potential**.
*Potassium*
- **Potassium ions** (K+) are primarily responsible for the **repolarization phase** of the action potential.
- The efflux of K+ through **voltage-gated potassium channels** causes the membrane potential to return to its resting state.
Neuromuscular blocking agents US Medical PG Question 3: A neurophysiologist describes the mechanism of a specific type of synaptic transmission to his students. While illustrating this, he points out that when the action potential reaches the presynaptic terminal of a chemical synapse, the voltage-gated Ca2+ channels open. Ca2+ ions trigger the release of neurotransmitters from vesicles in the presynaptic terminal. In this type of synaptic transmission, increased cytosolic Ca2+ levels cause the release of a neurotransmitter from small vesicles with dense cores. Which of the following neurotransmitters is most likely to be the one that is released into the synaptic cleft in this type of synapse?
- A. Epinephrine
- B. Glutamate
- C. Glycine
- D. GABA (γ-amino butyric acid)
- E. Norepinephrine (Correct Answer)
Neuromuscular blocking agents Explanation: ***Norepinephrine***
- **Norepinephrine** is the primary catecholamine neurotransmitter stored in **small vesicles with dense cores** (dense-core vesicles).
- It is released from **sympathetic postganglionic neurons** and central nervous system neurons, particularly from the **locus coeruleus**.
- Dense-core vesicles are the hallmark of catecholaminergic neurons, and norepinephrine is the most abundant neuronal catecholamine.
- The description perfectly matches noradrenergic synaptic transmission.
*Epinephrine*
- While epinephrine is also a catecholamine stored in dense-core vesicles, it functions primarily as a **hormone** released from the **adrenal medulla** (not a neurotransmitter).
- Only a **very small number** of CNS neurons use epinephrine as a neurotransmitter (mainly in medullary regions).
- In the context of synaptic transmission, norepinephrine is far more common.
*Glutamate*
- **Glutamate** is the primary excitatory neurotransmitter in the CNS but is stored in **small, clear synaptic vesicles**, not dense-core vesicles.
- It does not fit the description of dense-core vesicle storage.
*Glycine*
- **Glycine** is an inhibitory neurotransmitter stored in **small, clear synaptic vesicles**.
- Found predominantly in the **spinal cord** and brainstem, not in dense-core vesicles.
*GABA (γ-amino butyric acid)*
- **GABA** is the main inhibitory neurotransmitter stored in **small, clear synaptic vesicles**.
- Not associated with dense-core vesicle storage.
Neuromuscular blocking agents US Medical PG Question 4: A 16-year-old boy is brought to the emergency department by ambulance with a visible deformity of the upper thigh after being involved in a motor vehicle collision. He is informed that he will require surgery and is asked about his medical history. He mentions that he had surgery to remove his tonsils several years ago and at that time suffered a complication during the surgery. Specifically, shortly after the surgery began, he began to experience severe muscle contractions and an increased body temperature. Based on this information, a different class of muscle relaxants are chosen for use during the upcoming surgery. If these agents needed to be reversed, the reversal agent should be administered with which of the following to prevent off-target effects?
- A. Atropine (Correct Answer)
- B. Epinephrine
- C. Echothiophate
- D. Methacholine
- E. Phentolamine
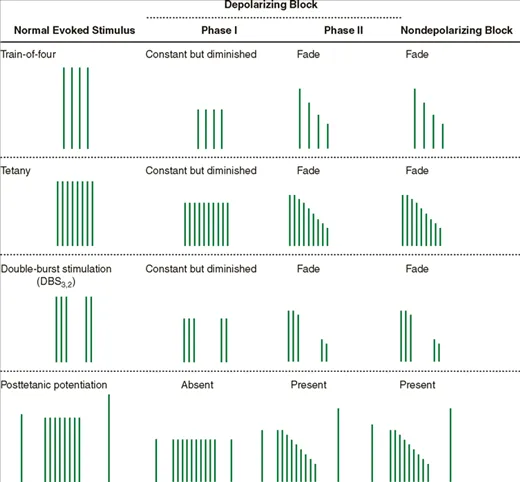
Neuromuscular blocking agents Explanation: **Atropine**
- The patient's history of **severe muscle contractions** and **increased body temperature** during prior surgery indicates **malignant hyperthermia**, a contraindication for succinylcholine
- Therefore, **nondepolarizing neuromuscular blockers** will be used instead and reversal is typically achieved with **neostigmine** (acetylcholinesterase inhibitor)
- Neostigmine increases acetylcholine at **both nicotinic and muscarinic receptors**, causing undesirable **muscarinic side effects** (bradycardia, salivation, bronchospasm, increased GI motility)
- **Atropine** or **glycopyrrolate** (muscarinic antagonists) must be co-administered to prevent these off-target muscarinic effects
*Epinephrine*
- Sympathomimetic acting on **alpha- and beta-adrenergic receptors** used for anaphylaxis, severe asthma, and cardiac arrest
- Not used to prevent muscarinic side effects of acetylcholinesterase inhibitors
*Echothiophate*
- **Irreversible acetylcholinesterase inhibitor** used for glaucoma treatment
- Would exacerbate rather than prevent cholinergic side effects when combined with neostigmine
*Methacholine*
- **Muscarinic cholinergic agonist** used in bronchial challenge tests for asthma diagnosis
- Would worsen muscarinic side effects rather than preventing them
*Phentolamine*
- **Alpha-adrenergic blocker** used for hypertensive crises from pheochromocytoma or vasopressor extravasation
- No role in managing muscarinic side effects of acetylcholinesterase inhibitors
Neuromuscular blocking agents US Medical PG Question 5: A 59-year-old woman is scheduled to undergo a right hip total arthroplasty for severe hip osteoarthritis that has failed conservative management. She has never had surgery before. She has a history of major depressive disorder and takes sertraline daily and ibuprofen occasionally for pain. Her mother died of breast cancer and her father died from a myocardial infarction. She has a brother who had an adverse reaction following anesthesia, but she does not know details of the event. In the operating room, the anesthesiologist administers isoflurane and succinylcholine. Two minutes later, the patient develops hypercarbia and hypertonicity of her bilateral upper and lower extremities. Her temperature is 103.7°F (39.8°C), blood pressure is 155/95 mmHg, pulse is 115/min, and respirations are 20/min.
A medication with which of the following mechanisms of action is most strongly indicated for this patient?
- A. Muscarinic antagonist
- B. Antihistamine
- C. Ryanodine receptor antagonist (Correct Answer)
- D. Cholinesterase inhibitor
- E. Dopamine receptor agonist
Neuromuscular blocking agents Explanation: ***Ryanodine receptor antagonist***
- The patient's presentation with **hyperthermia**, **hypercarbia**, and **muscle rigidity** after exposure to isoflurane and succinylcholine is highly indicative of **malignant hyperthermia (MH)**.
- **Dantrolene**, a **ryanodine receptor antagonist**, is the primary treatment for MH as it blocks the release of calcium from the sarcoplasmic reticulum, thereby reducing muscle contraction and heat production.
*Muscarinic antagonist*
- **Muscarinic antagonists** like atropine block the action of acetylcholine at muscarinic receptors and are used to treat **bradycardia** or reduce secretions.
- They would not address the underlying pathophysiology of malignant hyperthermia, which involves uncontrolled calcium release from the sarcoplasmic reticulum.
*Antihistamine*
- **Antihistamines** block histamine receptors and are used to treat **allergic reactions** or reduce nausea and vomiting.
- They have no role in the management of malignant hyperthermia, which is not an allergic response.
*Cholinesterase inhibitor*
- **Cholinesterase inhibitors** increase acetylcholine levels at the neuromuscular junction and are used to reverse **neuromuscular blockade** or treat **myasthenia gravis**.
- Administering a cholinesterase inhibitor would likely intensify muscle contraction and rigidity, worsening the patient's condition in malignant hyperthermia.
*Dopamine receptor agonist*
- **Dopamine receptor agonists** are primarily used to treat **Parkinson's disease** or as **vasopressors** in critical care.
- They have no direct therapeutic effect on the severe muscle rigidity and hypermetabolic state characteristic of malignant hyperthermia.
Neuromuscular blocking agents US Medical PG Question 6: A 71-year-old male is brought to the emergency room by his caretaker and presents with difficulty breathing, muscle rigidity in the face, neck, back and upper extremities, and profuse sweating. The intern notes a large wound on his head near the back of his right ear which his caretaker had bandaged up. The caretaker explains that the wound was the result of a fall while walking in his backyard. The intern performs a quick physical exam and observes increased reflexes. The patient was intubated to assist in his breathing and was given diazepam, metronidazole, and an immunoglobulin after the blood work came back. Which of the following neurotransmitters is affected in this patient?
- A. Glycine (Correct Answer)
- B. Acetylcholine
- C. Serotonin
- D. Dopamine
- E. Epinephrine
Neuromuscular blocking agents Explanation: ***Glycine***
- The patient's symptoms (muscle rigidity, profuse sweating, increased reflexes, and difficulty breathing) are classic signs of **tetanus**, caused by *Clostridium tetani* toxin (tetanospasmin). The toxin inhibits the release of **both glycine and GABA**, which are inhibitory neurotransmitters in the spinal cord. Specifically, it blocks release from Renshaw cells and other inhibitory interneurons, leading to disinhibition of motor neurons and resulting in uncontrolled muscle spasms and rigidity.
- The treatment with **metronidazole** (to kill *C. tetani*), **immunoglobulin** (to neutralize unbound toxin), and **diazepam** (a GABA agonist to reduce muscle spasms) further supports a diagnosis of tetanus, where **glycine's** inhibitory function is critically impaired.
*Acetylcholine*
- **Acetylcholine** is a primary excitatory neurotransmitter at the neuromuscular junction, responsible for muscle contraction. The pathology in tetanus is not an excess of acetylcholine, but rather a lack of inhibition by other neurotransmitters.
- While muscle contraction is a symptom, the underlying defect isn't directly related to acetylcholine synthesis or release, but rather the loss of inhibitory input onto motor neurons.
*Serotonin*
- **Serotonin** primarily regulates mood, sleep, appetite, and pain perception in the central nervous system.
- Dysregulation of serotonin is associated with conditions like depression and anxiety, not the severe muscle rigidity and spasms seen in this patient.
*Dopamine*
- **Dopamine** is involved in reward, motivation, motor control, and hormone release. Its deficiency is characteristic of Parkinson's disease, leading to bradykinesia and tremors.
- Excess dopamine can be linked to psychotic disorders, but it does not cause the generalized muscle rigidity and hyperexcitability observed here.
*Epinephrine*
- **Epinephrine** (adrenaline) is a crucial neurotransmitter and hormone involved in the "fight or flight" response, increasing heart rate, blood pressure, and blood flow to muscles.
- While profuse sweating suggests autonomic dysregulation, epinephrine's primary role is not in directly mediating the muscle rigidity and increased reflexes characteristic of tetanus.
Neuromuscular blocking agents US Medical PG Question 7: You are currently employed as a clinical researcher working on clinical trials of a new drug to be used for the treatment of Parkinson's disease. Currently, you have already determined the safe clinical dose of the drug in a healthy patient. You are in the phase of drug development where the drug is studied in patients with the target disease to determine its efficacy. Which of the following phases is this new drug currently in?
- A. Phase 4
- B. Phase 1
- C. Phase 2 (Correct Answer)
- D. Phase 0
- E. Phase 3
Neuromuscular blocking agents Explanation: ***Phase 2***
- **Phase 2 trials** involve studying the drug in patients with the target disease to assess its **efficacy** and further evaluate safety, typically involving a few hundred patients.
- The question describes a stage after safe dosing in healthy patients (Phase 1) and before large-scale efficacy confirmation (Phase 3), focusing on efficacy in the target population.
*Phase 4*
- **Phase 4 trials** occur **after a drug has been approved** and marketed, monitoring long-term effects, optimal use, and rare side effects in a diverse patient population.
- This phase is conducted post-market approval, whereas the question describes a drug still in development prior to approval.
*Phase 1*
- **Phase 1 trials** primarily focus on determining the **safety and dosage** of a new drug in a **small group of healthy volunteers** (or sometimes patients with advanced disease if the drug is highly toxic).
- The question states that the safe clinical dose in a healthy patient has already been determined, indicating that Phase 1 has been completed.
*Phase 0*
- **Phase 0 trials** are exploratory, very early-stage studies designed to confirm that the drug reaches the target and acts as intended, typically involving a very small number of doses and participants.
- These trials are conducted much earlier in the development process, preceding the determination of safe clinical doses and large-scale efficacy studies.
*Phase 3*
- **Phase 3 trials** are large-scale studies involving hundreds to thousands of patients to confirm **efficacy**, monitor side effects, compare it to commonly used treatments, and collect information that will allow the drug to be used safely.
- While Phase 3 does assess efficacy, it follows Phase 2 and is typically conducted on a much larger scale before submitting for regulatory approval.
Neuromuscular blocking agents US Medical PG Question 8: A 36-year-old man presents to a psychiatrist for management of nicotine dependence. He has been a heavy smoker for the past 20 years. He has unsuccessfully attempted to quit smoking many times. He has seen multiple physicians for nicotine dependence. They prescribed nicotine replacement therapy and varenicline. He has also taken two antidepressants and participated in talk therapy. He asks the psychiatrist whether there are other alternatives. The psychiatrist explains that nicotine replacement therapy, non-nicotine pharmacotherapy, and talk therapy are the best options for the management of nicotine dependence. He tells the patient he can take a second-line medication for non-nicotine pharmacotherapy because the first-line medication failed. Which of the following medications would the psychiatrist most likely use to manage this patient’s nicotine dependence?
- A. Topiramate
- B. Methadone
- C. Clonidine (Correct Answer)
- D. Buprenorphine
- E. Lorazepam
Neuromuscular blocking agents Explanation: ***Clonidine***
- **Clonidine** is a **second-line agent** for smoking cessation, particularly effective for managing **withdrawal symptoms** like anxiety, irritability, and restlessness.
- It works as an **alpha-2 adrenergic agonist**, reducing sympathetic outflow and alleviating the somatic symptoms of nicotine withdrawal.
*Topiramate*
- **Topiramate** is an anticonvulsant sometimes used off-label for **alcohol dependence** or **weight management**; it is not a primary or secondary treatment for nicotine dependence.
- Its mechanism of action involves GABAergic and glutamatergic modulation, which is not directly targeted at nicotine withdrawal.
*Methadone*
- **Methadone** is an **opioid agonist** primarily used in the treatment of **opioid use disorder** to prevent withdrawal symptoms and reduce cravings.
- It has no established role in the direct management of nicotine dependence or smoking cessation.
*Buprenorphine*
- **Buprenorphine** is a **partial opioid agonist** used in the treatment of **opioid use disorder**, often combined with naloxone.
- Similar to methadone, it is not indicated for the treatment of nicotine dependence.
*Lorazepam*
- **Lorazepam** is a **benzodiazepine** used to treat **anxiety, insomnia**, and **seizures** due to its sedative and anxiolytic properties.
- While it could help with anxiety associated with nicotine withdrawal, it is not a direct treatment for nicotine dependence and carries risks of dependence itself.
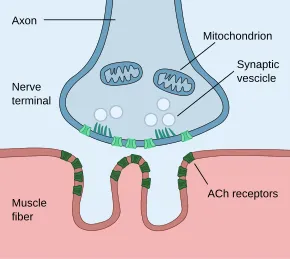
Neuromuscular blocking agents US Medical PG Question 9: A neurophysiology expert is teaching his students the physiology of the neuromuscular junction. While describing the sequence of events that takes place at the neuromuscular junction, he mentions that as the action potential travels down the motor neuron, it causes depolarization of the presynaptic membrane. This results in the opening of voltage-gated calcium channels, which leads to an influx of calcium into the synapse of the motor neuron. Consequently, the cytosolic concentration of Ca2+ ions increases. Which of the following occurs at the neuromuscular junction as a result of this increase in cytosolic Ca2+?
- A. Generation of an end plate potential
- B. Exocytosis of acetylcholine from the synaptic vesicles (Correct Answer)
- C. Increased Na+ and K+ conductance of the motor end plate
- D. Binding of Ca2+ ions to NM receptors
- E. Release of Ca2+ ions into the synaptic cleft
Neuromuscular blocking agents Explanation: ***Exocytosis of acetylcholine from the synaptic vesicles***
- The increase in **cytosolic Ca2+** within the presynaptic terminal is the primary trigger for the fusion of **synaptic vesicles** filled with **acetylcholine (ACh)** with the presynaptic membrane.
- This fusion process, known as **exocytosis**, releases ACh into the **synaptic cleft**, initiating synaptic transmission.
*Generation of an end plate potential*
- The **end plate potential (EPP)** is generated *after* acetylcholine (ACh) is released into the synaptic cleft and binds to receptors on the motor end plate.
- This event occurs *following* the Ca2+-induced release of neurotransmitter, not as a direct result of the Ca2+ increase itself.
*Increased Na+ and K+ conductance of the motor end plate*
- Increased **Na+ and K+ conductance** across the motor end plate membrane is a direct consequence of acetylcholine binding to its receptors, which are **ligand-gated ion channels**.
- This change in conductance *generates the end plate potential*, occurring after ACh release.
*Binding of Ca2+ ions to NM receptors*
- **NM receptors** (nicotinic muscle receptors) are located on the **postsynaptic membrane** (motor end plate) and bind to **acetylcholine (ACh)**, not Ca2+ ions.
- Calcium's primary role in this context is presynaptic: triggering ACh release.
*Release of Ca2+ ions into the synaptic cleft*
- Calcium ions enter the **presynaptic terminal** from the synaptic cleft, and their increased cytosolic concentration within the presynaptic terminal drives neurotransmitter release.
- Calcium itself is not released *into* the synaptic cleft in this process; rather, it enters the presynaptic neuron from the cleft.
Neuromuscular blocking agents US Medical PG Question 10: A 26-year-old man is brought to the emergency department by his friends because of blurred vision and slurred speech for the past 6 hours. He had some difficulty swallowing his food during lunch and has weakness in both arms. Two weeks ago, he had an upper respiratory infection that resolved spontaneously. He lives independently and returned from his grandparents' farm 2 days ago. He commonly consumes canned vegetables and fruits. He is alert and oriented to person, place, and time. His temperature is 37°C (98.6°F), pulse is 88/min, respirations are 10/min and labored, and blood pressure is 110/70 mm Hg. Examination shows bilateral nystagmus and ptosis. The pupils are dilated and not reactive to light. Muscle strength of the facial muscles and bilateral upper extremities is decreased. Upper extremity deep tendon reflexes are 1+ bilaterally. Cardiopulmonary examination shows no abnormalities. Which of the following is the most likely cause for this patient's symptoms?
- A. Autoantibodies against myelin
- B. Chemical that inhibits acetylcholinesterase
- C. Autoantibodies against ACh receptors
- D. Toxin that inhibits ACh release (Correct Answer)
- E. Cell-mediated focal demyelination
Neuromuscular blocking agents Explanation: **Toxin that inhibits ACh release**
- The patient's symptoms, including **blurred vision, ptosis, fixed dilated pupils, slurred speech, dysphagia, and descending flaccid paralysis** (weakness in arms before legs, with reduced reflexes), are highly characteristic of **botulism**.
- **Clostridium botulinum toxin** inhibits the release of **acetylcholine (ACh)** at the neuromuscular junction and parasympathetic synapses, leading to these symptoms. The history of consuming **canned foods** and returning from a farm suggests a potential exposure source.
*Autoantibodies against myelin*
- This mechanism describes **Guillain-Barré syndrome (GBS)**, which typically presents with **ascending paralysis** and areflexia, often following an infection.
- While GBS can cause some cranial nerve involvement, the prominent **fixed dilated pupils (pupil-sparing paralysis is typical in GBS)** and the **descending pattern of weakness** in this patient are inconsistent with GBS.
*Chemical that inhibits acetylcholinesterase*
- This mechanism is associated with **organophosphate poisoning**, which presents with a **cholinergic crisis**.
- Symptoms include **miosis**, increased salivation, lacrimation, urination, defecation, gastrointestinal upset, emesis (**SLUDGE** syndrome), bradycardia, and muscle fasciculations, none of which are noted in this patient.
*Autoantibodies against ACh receptors*
- This is the underlying mechanism of **myasthenia gravis**, an autoimmune disorder characterized by **fluctuating muscle weakness** that worsens with activity and improves with rest.
- Key features often include **ptosis and diplopia**, but pupils are typically **spared**. The weakness in myasthenia gravis is not typically descending with fixed dilated pupils, and it does not usually present acutely with such severe widespread involvement.
*Cell-mediated focal demyelination*
- This describes the pathology of **multiple sclerosis (MS)**, a chronic inflammatory demyelinating disease of the central nervous system.
- MS typically presents with **diverse neurological symptoms** that can be relapsing-remitting or progressive, often including sensory disturbances, motor weakness, visual changes (e.g., optic neuritis), and bladder dysfunction. It does not typically cause acute, rapidly progressive flaccid paralysis with fixed dilated pupils and bulbar symptoms as seen here.
More Neuromuscular blocking agents US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.