Muscarinic antagonists US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Muscarinic antagonists. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Muscarinic antagonists US Medical PG Question 1: An 18-year-old boy presents to the clinic with shortness of breath and fever for the last 2 days. He also has a cough for the same duration. He is asthmatic and uses inhaled albuterol for symptom relief when required. He used albuterol today 3 times at 10-minute intervals but has not had relief of his symptoms. On physical examination, his temperature is 38.3°C (101.0°F), pulse is 130/min, blood pressure is 116/80 mm Hg, and respirations are 28/min. Auscultation of the chest reveals bilateral crackles. Considering that he has already taken inhaled albuterol and has tachycardia, the physician nebulizes him with inhaled ipratropium bromide, which significantly improves his symptoms. Which of the following is the mechanism of action of this drug?
- A. Inhibition of vagally-mediated contraction of bronchial smooth muscles (Correct Answer)
- B. Inhibition of degranulation of mast cells
- C. Inhibition of phosphodiesterase-4, leading to prevention of release of cytokines and chemokines
- D. Inhibition of adenosine receptors in the respiratory tract
- E. Stimulation of β2-adrenergic receptors in bronchial smooth muscle
Muscarinic antagonists Explanation: ***Inhibition of vagally-mediated contraction of bronchial smooth muscles***
- Ipratropium bromide is a **short-acting muscarinic antagonist (SAMA)** that blocks M3 muscarinic receptors on bronchial smooth muscle
- This action **inhibits acetylcholine's effect**, leading to bronchodilation by preventing vagally-mediated bronchoconstriction
- Particularly useful as an **adjunct to β2-agonists** in acute asthma exacerbations and COPD
*Inhibition of degranulation of mast cells*
- This is the mechanism of action of **mast cell stabilizers** like cromolyn sodium and nedocromil
- These drugs are used for **asthma prophylaxis**, not acute symptom relief
- They prevent the release of inflammatory mediators like histamine from mast cells
*Inhibition of phosphodiesterase-4, leading to prevention of release of cytokines and chemokines*
- This is the mechanism of action of **phosphodiesterase-4 (PDE4) inhibitors** such as roflumilast
- Primarily used in **severe COPD** to reduce inflammation
- PDE4 inhibition increases intracellular cAMP, which has anti-inflammatory effects
*Inhibition of adenosine receptors in the respiratory tract*
- This is the mechanism of action of **methylxanthines** like theophylline and aminophylline
- Blocking adenosine receptors provides bronchodilation and reduces inflammation
- Now considered **second-line therapy** due to narrow therapeutic index
*Stimulation of β2-adrenergic receptors in bronchial smooth muscle*
- This is the mechanism of action of **β2-agonists** like albuterol (already used by this patient)
- Not the mechanism of ipratropium, which is an **anticholinergic** agent
- The patient had already received albuterol without adequate relief, prompting the addition of ipratropium
Muscarinic antagonists US Medical PG Question 2: A forty-five-year-old farmer with past medical history of diabetes, hypertension, and possible narrow angles comes into your emergency room confused, diaphoretic, salivating, vomiting and shedding tears. He has pinpoint pupils. You conclude that he is showing effects of acute organophosphate poisoning. While administering the antidote, you should carefully monitor for which of the following side effects?
- A. Barotrauma to middle ear
- B. Bronchospasm
- C. Hyperkalemia
- D. Acute closed-angle glaucoma (Correct Answer)
- E. Tinnitus
Muscarinic antagonists Explanation: ***Acute closed-angle glaucoma***
- **Atropine**, a common antidote for organophosphate poisoning, can dilate the pupils and **increase intraocular pressure**, precipitating acute closed-angle glaucoma in susceptible individuals.
- The patient's history of "possible narrow angles" indicates a predisposition to this condition, making careful monitoring essential during atropine administration.
*Barotrauma to middle ear*
- **Barotrauma** is typically associated with changes in **ambient pressure**, such as during air travel or diving.
- There is no direct physiological link between organophosphate poisoning treatment and middle ear barotrauma.
*Bronchospasm*
- **Organophosphate poisoning** *causes* bronchospasm due to excessive cholinergic stimulation, while atropine is used to *reverse* it.
- Therefore, bronchospasm would improve, not worsen, with appropriate antidote administration.
*Hyperkalemia*
- **Hyperkalemia** is not a direct side effect of atropine or a common complication of organophosphate poisoning treatment.
- While electrolyte imbalances can occur in critically ill patients, hyperkalemia is not specifically monitored for in this context.
*Tinnitus*
- **Tinnitus** is a perception of noise or ringing in the ears often associated with **auditory system damage** or certain medications.
- It is not a recognized side effect of atropine or a complication to specifically monitor for in organophosphate poisoning.
Muscarinic antagonists US Medical PG Question 3: A 43-year-old man is brought to the emergency department by his wife because of a 1-hour history of confusion and strange behavior. She reports that he started behaving in an agitated manner shortly after eating some wild berries that they had picked during their camping trip. His temperature is 38.7°C (101.7°F). Physical examination shows warm, dry skin and dry mucous membranes. His pupils are dilated and minimally reactive to light. His bowel sounds are decreased. The patient is admitted and pharmacotherapy is initiated with a drug that eventually results in complete resolution of all of his symptoms. This patient was most likely administered which of the following drugs?
- A. Rivastigmine
- B. Atropine
- C. Scopolamine
- D. Physostigmine (Correct Answer)
- E. Neostigmine
Muscarinic antagonists Explanation: ***Physostigmine***
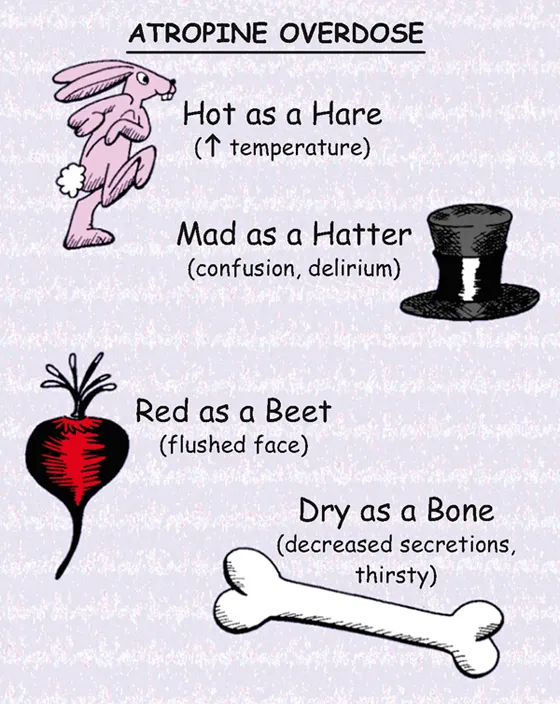
- The patient's symptoms (confusion, agitation, dilated pupils, warm/dry skin, decreased bowel sounds, fever) are characteristic of **anticholinergic toxicity**, often caused by ingestion of plants like Jimson weed or deadly nightshade (containing atropine-like alkaloids).
- **Physostigmine** is a **reversible acetylcholinesterase inhibitor** that can cross the **blood-brain barrier** and reverse both central (confusion, agitation) and peripheral (dilated pupils, dry skin, decreased bowel sounds) anticholinergic effects.
*Rivastigmine*
- **Rivastigmine** is an acetylcholinesterase inhibitor primarily used to treat **Alzheimer's disease** and Parkinson's disease dementia.
- While it inhibits acetylcholinesterase, its primary clinical use and efficacy profile do not align with rapid reversal of acute, severe anticholinergic poisoning.
*Atropine*
- **Atropine** is a **muscarinic anticholinergic agent** that would *exacerbate* the patient's symptoms, as the presentation is consistent with anticholinergic poisoning.
- It works by blocking acetylcholine receptors, leading to effects like dilated pupils, dry mouth, and decreased gastrointestinal motility.
*Scopolamine*
- **Scopolamine** is another potent **muscarinic anticholinergic agent** that causes similar symptoms to atropine, particularly confusion and delirium due to its central nervous system effects.
- Administering scopolamine would worsen the patient's existing anticholinergic toxidrome.
*Neostigmine*
- **Neostigmine** is a **reversible acetylcholinesterase inhibitor** used for conditions like myasthenia gravis and reversal of neuromuscular blockade.
- However, **neostigmine does not cross the blood-brain barrier** effectively, meaning it would not reverse the central nervous system symptoms (confusion, agitation) prominent in this anticholinergic poisoning case.
Muscarinic antagonists US Medical PG Question 4: A 78-year-old man suffers a fall in a nursing home and is brought to the emergency room. A right hip fracture is diagnosed, and he is treated with a closed reduction with internal fixation under spinal anesthesia. On the second postoperative day, the patient complains of pain in the lower abdomen and states that he has not urinated since the surgery. An ultrasound shows increased bladder size and volume. Which of the following is the mechanism of action of the drug which is most commonly used to treat this patient’s condition?
- A. Alpha-blocker
- B. Parasympathetic antagonist
- C. Sympathetic agonist
- D. Beta-blocker
- E. Parasympathetic agonist (Correct Answer)
Muscarinic antagonists Explanation: ***Parasympathetic agonist***
- The patient presents with **postoperative urinary retention (POUR)**, commonly treated with **bethanechol**, a muscarinic cholinergic agonist.
- Bethanechol acts as a **parasympathetic agonist**, stimulating **muscarinic receptors** on the **detrusor muscle** of the bladder, causing it to contract and facilitating urination.
*Alpha-blocker*
- **Alpha-blockers** (e.g., tamsulosin) relax the **smooth muscle** of the prostatic urethra and bladder neck, often used for **benign prostatic hyperplasia (BPH)**.
- While they can improve urinary flow, they do not directly stimulate **detrusor contraction** and are not the primary treatment for acute POUR.
*Parasympathetic antagonist*
- **Parasympathetic antagonists** (e.g., oxybutynin) block muscarinic receptors, leading to **detrusor relaxation**.
- These drugs are used to treat conditions like **overactive bladder** or **urge incontinence**, which involve excessive bladder contraction, and would worsen urinary retention.
*Sympathetic agonist*
- **Sympathetic agonists** (e.g., norepinephrine) primarily cause vasoconstriction and cardiac stimulation.
- They tend to **relax the detrusor muscle** and contract the internal urethral sphincter via **beta-3 and alpha-1 receptors**, respectively, which would exacerbate urinary retention.
*Beta-blocker*
- **Beta-blockers** (e.g., propranolol) primarily affect the heart and blood vessels, slowing heart rate and lowering blood pressure.
- They have **no direct primary role** in the treatment of acute urinary retention as they do not directly act on bladder contractility.
Muscarinic antagonists US Medical PG Question 5: An 83-year-old man with advanced-stage prostate cancer comes to the physician because of a 1-week history of worsening lower back and hip pain. The patient's analgesic regimen includes oxycodone, ibuprofen, and alendronic acid. Physical examination shows localized tenderness over the lumbar spine and right hip. His current pain management requires opioid dose escalation. Which of the following opioid side effects is most likely to remain unaffected by the mechanism underlying this patient's need for a higher drug dose?
- A. Pruritus
- B. Constipation (Correct Answer)
- C. Mydriasis
- D. Respiratory depression
- E. Nausea
Muscarinic antagonists Explanation: ***Constipation***
- **Opioid-induced constipation** is mediated by direct opioid receptor activation in the **enteric nervous system**, reducing gut motility.
- Unlike most other opioid side effects, the body generally does not develop **tolerance** to this effect, meaning it persists even with chronic use and dose escalation.
*Pruritus*
- **Opioid-induced pruritus** is often due to **histamine release** from mast cells, which is a common side effect of opioid administration.
- **Tolerance** can develop to pruritus over time, meaning it may lessen or resolve with chronic opioid use or dose escalation as the body adapts.
*Mydriasis*
- **Mydriasis** (pupil dilation) is not a typical opioid side effect; rather, **miosis** (pinpoint pupils) is characteristic of opioid use.
- Furthermore, **miosis** itself can exhibit some degree of **tolerance** with chronic opioid use, though it is often one of the more persistent effects.
*Respiratory depression*
- **Respiratory depression** is a serious and dose-dependent opioid side effect caused by decreased sensitivity of the respiratory center in the brainstem to CO2.
- While it is a dangerous effect, **tolerance** can develop to respiratory depression with chronic opioid use, reducing its severity over time.
*Nausea*
- **Opioid-induced nausea** is thought to be mediated by the **chemoreceptor trigger zone (CTZ)** in the brain and slowed gastric emptying.
- The body often develops **tolerance** to opioid-induced nausea within a few days to weeks of consistent opioid use.
Muscarinic antagonists US Medical PG Question 6: A 67-year-old man presents to the emergency department acutely confused. The patient's wife found him mumbling incoherently in the kitchen this morning as they were preparing for a hike. The patient was previously healthy and only had a history of mild forgetfulness, depression, asthma, and seasonal allergies. His temperature is 98.5°F (36.9°C), blood pressure is 122/62 mmHg, pulse is 119/min, and oxygen saturation is 98% on room air. The patient is answering questions inappropriately and seems confused. Physical exam is notable for warm, flushed, and dry skin. The patient's pupils are dilated. Which of the following is also likely to be found in this patient?
- A. Hypoventilation
- B. QRS widening
- C. Coronary artery vasospasm
- D. Increased bronchial secretions
- E. Urinary retention (Correct Answer)
Muscarinic antagonists Explanation: ***Urinary retention***
- The patient's symptoms (dilated pupils, warm/flushed/dry skin, confusion, tachycardia) are consistent with **anticholinergic toxidrome**.
- **Urinary retention** is a common manifestation of anticholinergic toxicity due to the paralysis of the detrusor muscle and contraction of the urethral sphincter.
*Hypoventilation*
- Anticholinergic toxicity typically causes **tachycardia** and may lead to tachypnea, not hypoventilation.
- Respiratory depression is more characteristic of **opioid** or **sedative-hypnotic** overdose.
*QRS widening*
- **QRS widening** is characteristic of **sodium channel blockade**, as seen with tricyclic antidepressant overdose, which can have anticholinergic effects but primarily causes cardiac toxicity via sodium channel blockade.
- While anticholinergics can cause arrhythmias, QRS widening specific to this mechanism isn't a primary feature of pure anticholinergic toxidrome.
*Coronary artery vasospasm*
- **Coronary artery vasospasm** is not a direct effect of anticholinergic toxicity.
- It is more commonly associated with drug use such as **cocaine**, or certain medications like **5-fluorouracil**.
*Increased bronchial secretions*
- Anticholinergic agents **decrease bronchial secretions** by blocking muscarinic receptors in the airway smooth muscle and glands.
- Increased bronchial secretions are characteristic of **cholinergic overdose**.
Muscarinic antagonists US Medical PG Question 7: A 33-year-old man comes to the emergency department because of a dry mouth and blurred vision for the past 30 minutes. Prior to this, he was on a road trip and started to feel nauseous, dizzy, and fatigued, so his friend gave him a drug that had helped in the past. Physical examination shows dry mucous membranes and dilated pupils. The remainder of the examination shows no abnormalities. Administration of which of the following drugs is most likely to cause a similar adverse reaction in this patient?
- A. Loratadine
- B. Phenylephrine
- C. Oxycodone
- D. Oxybutynin (Correct Answer)
- E. Pilocarpine
Muscarinic antagonists Explanation: ***Oxybutynin***
- Oxybutynin is an **anticholinergic** drug primarily used to treat overactive bladder.
- Its adverse effects, such as **dry mouth** (xerostomia), blurred vision (due to cycloplegia and mydriasis), nausea, dizziness, and fatigue, are directly related to its **muscarinic receptor blockade**.
*Loratadine*
- Loratadine is a **second-generation antihistamine** that is largely non-sedating and has minimal anticholinergic effects.
- While it can cause dry mouth in rare cases, it is much less likely to cause the constellation of severe anticholinergic symptoms seen here, especially **blurred vision due to mydriasis**.
*Phenylephrine*
- Phenylephrine is an **alpha-1 adrenergic agonist** used as a decongestant or to increase blood pressure.
- Its primary effects are vasoconstriction; it does not typically cause dry mouth, blurred vision, or the other anticholinergic symptoms described.
*Oxycodone*
- Oxycodone is an **opioid analgesic** that primarily acts on mu-opioid receptors.
- Common side effects include constipation, nausea, sedation, and respiratory depression, but not dry mouth or blurred vision as a prominent anticholinergic effect.
*Pilocarpine*
- Pilocarpine is a **muscarinic agonist** used to treat dry mouth or glaucoma.
- It would cause symptoms directly opposite to those observed, such as increased salivation and miosis, rather than dry mouth and dilated pupils.
Muscarinic antagonists US Medical PG Question 8: Choose the correctly matched pairs regarding the drugs used in schizophrenia:
1. D2 antagonism: Reduces positive symptoms
2. 5HT2A antagonism: Reduces negative symptoms
3. 5HT1A agonism: Weight loss
4. Muscarinic antagonism: Reduces extrapyramidal symptoms
- A. 1,4
- B. 1,2,4
- C. 1,2,3,4
- D. 1,2 (Correct Answer)
Muscarinic antagonists Explanation: ***1,2***
- **D2 antagonism** is the primary mechanism by which antipsychotics reduce **positive symptoms** of schizophrenia, such as hallucinations and delusions.
- **5HT2A antagonism** is a key mechanism of atypical antipsychotics contributing to the reduction of **negative symptoms** (e.g., apathy, anhedonia, flat affect) and cognitive deficits, while also reducing the risk of extrapyramidal symptoms.
*1,2,3,4*
- This option is incorrect because **5HT1A agonism** is not associated with **weight loss**. While 5HT1A partial agonism (as seen with aripiprazole and brexpiprazole) may improve negative symptoms, anxiety, and cognitive function, it does not directly cause weight loss.
- Additionally, **muscarinic antagonism** does not reduce extrapyramidal symptoms as a primary mechanism. Rather, anticholinergic (muscarinic antagonist) drugs like benztropine are used to **treat** EPS after it occurs. The reduction of EPS in atypical antipsychotics primarily comes from 5HT2A antagonism and lower D2 binding affinity.
*1,2,4*
- This option is incorrect because **muscarinic antagonism** is not a mechanism that reduces EPS. Anticholinergic agents are used therapeutically to counteract EPS caused by dopamine blockade, but anticholinergic effects themselves do not prevent or reduce EPS.
- The reduction of EPS with atypical antipsychotics is mainly due to **5HT2A antagonism** balancing dopaminergic blockade, selective limbic over striatal binding, and fast D2 dissociation kinetics.
*1,4*
- This option is incorrect because it omits **5HT2A antagonism**, which is crucial for reducing **negative symptoms** in schizophrenia.
- It also incorrectly includes muscarinic antagonism as a mechanism that reduces EPS, when in reality anticholinergics are used to treat EPS rather than prevent it.
Muscarinic antagonists US Medical PG Question 9: A 26-year-old man is brought to the hospital by his wife who complains that her husband has been behaving oddly for the past few hours. The patient’s wife says that she has known him for only 4 months. The wife is unable to give any past medical history. The patient’s speech is difficult to follow, and he seems very distracted. After 15 minutes, he becomes agitated and starts to bang his head on a nearby pillar. He is admitted to the psychiatric ward and is given an emergency medication, after which he calms down. In the next 2 days, he continues to become agitated at times and required 2 more doses of the same drug. On the 4th day of admission, he appears very weak, confused, and does not respond to questions appropriately. His vital signs include: temperature 40.0°C (104.0°F), blood pressure 160/95 mm Hg, and pulse 114/min. On physical examination, he is profusely diaphoretic. He is unable to stand upright or even get up from his bed. Which of the following is the mechanism of action of the drug which most likely caused this patient’s current condition?
- A. Skeletal muscle relaxation
- B. Agonistic effect on dopamine receptors
- C. Serotonin reuptake inhibition
- D. Histamine H2 receptor blocking
- E. Dopamine receptor blocking (Correct Answer)
Muscarinic antagonists Explanation: ***Dopamine receptor blocking***
- The patient's presentation with **fever, altered mental status, muscle rigidity**, and **autonomic instability** (tachycardia, hypertension, diaphoresis) after receiving antipsychotic medication strongly suggests **neuroleptic malignant syndrome (NMS)**.
- NMS is caused by a severe decrease in **dopaminergic activity**, primarily due to the blockade of **D2 dopamine receptors** in the basal ganglia and hypothalamus by antipsychotics.
- The classic tetrad of NMS includes: **hyperthermia, muscle rigidity, altered mental status**, and **autonomic instability**.
*Skeletal muscle relaxation*
- While agitation might be treated with benzodiazepines, which cause muscle relaxation, this mechanism does not explain the **severe rigidity, hyperthermia**, and **autonomic dysfunction** seen in the patient.
- **Muscle rigidity** (lead-pipe rigidity) is a hallmark of the patient's current condition, contradicting the idea of muscle relaxation.
*Agonistic effect on dopamine receptors*
- An agonistic effect on dopamine receptors would typically lead to symptoms similar to **psychosis** or **mania**, not the severe rigidity and hypodopaminergic state observed in NMS.
- This mechanism would counteract the effects of antipsychotics and would not cause NMS.
*Serotonin reuptake inhibition*
- This is the mechanism of action for **SSRIs**, and an excess of serotonin can lead to **serotonin syndrome**, which shares some features with NMS but typically includes **hyperreflexia** and **myoclonus**, rather than lead-pipe rigidity.
- The context of treating acute psychosis with an emergency medication points more towards an antipsychotic, not an antidepressant.
*Histamine H2 receptor blocking*
- **Histamine H2 receptor blockers** are used to treat conditions like **acid reflux** and **peptic ulcers**; they have no direct neurological effects that would cause NMS.
- This mechanism is entirely irrelevant to the patient's psychiatric symptoms and subsequent severe adverse reaction.
Muscarinic antagonists US Medical PG Question 10: A 28-year-old man is brought to the emergency department after his girlfriend found him twitching and jerking in the yard while gardening. Shortly after he became obtunded, emergency medical services reported 1 episode of emesis during transport. His blood pressure is 85/50 mmHg, pulse is 55/min, and respirations are irregular. Physical examination demonstrates marks on his left forearm, pinpoint pupils, diaphoresis, and fasciculations of his left calf. Following initial stabilization and respiratory support, what is the best next step?
- A. Atropine
- B. Naltrexone
- C. Atropine and pralidoxime (Correct Answer)
- D. Lamotrigine
- E. Naloxone
Muscarinic antagonists Explanation: ***Atropine and pralidoxime***
* This patient presents with a classic picture of **organophosphate poisoning**, characterized by profuse secretions, bradycardia, hypotension, pinpoint pupils, and fasciculations.
* **Atropine** is given to block the muscarinic effects, and **pralidoxime** (2-PAM) is used to reactivate acetylcholinesterase, reversing both muscarinic and nicotinic effects.
* *Atropine*
* While essential for managing the **muscarinic effects** like bradycardia and profuse secretions, atropine alone does not address the nicotinic effects, such as muscle fasciculations and weakness.
* Without pralidoxime, the underlying cause of acetylcholinesterase inhibition is not treated, potentially leading to continued nicotinic toxicity.
* *Naltrexone*
* **Naltrexone** is an opioid receptor antagonist used for opioid dependence and alcohol use disorder.
* It has no role in the management of organophosphate poisoning, which involves cholinergic overstimulation.
* *Lamotrigine*
* **Lamotrigine** is an anticonvulsant medication used to treat epilepsy and bipolar disorder.
* The patient's seizures are secondary to organophosphate poisoning and would not be primarily managed with lamotrigine.
* *Naloxone*
* **Naloxone** is an opioid antagonist used to reverse opioid overdose.
* The patient's symptoms are inconsistent with opioid overdose and point strongly towards cholinergic crisis.
More Muscarinic antagonists US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.