Cholinergic agonists (direct and indirect) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cholinergic agonists (direct and indirect). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cholinergic agonists (direct and indirect) US Medical PG Question 1: Which receptor type mediates the slow phase of synaptic transmission in autonomic ganglia?
- A. Muscarinic (M3)
- B. Muscarinic (M2)
- C. Muscarinic (M1) (Correct Answer)
- D. Nicotinic (N2)
Cholinergic agonists (direct and indirect) Explanation: ***Muscarinic (M1)***
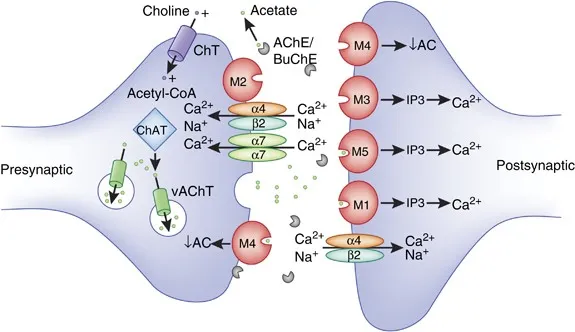
- **M1 receptors** are **Gq-protein coupled receptors** that activate phospholipase C, leading to increased intracellular calcium and diacylglycerol, which mediates the slow excitatory postsynaptic potential in autonomic ganglia.
- This activation results in a **slow depolarization** that prolongs the excitability of ganglionic neurons after the initial fast synaptic transmission.
*Muscarinic (M3)*
- **M3 receptors** are primarily found on **smooth muscle**, glands, and endothelium, mediating contraction, secretion, and vasodilation, respectively.
- While also **Gq-protein coupled**, their role in autonomic ganglia is not the main mediator of the slow phase of synaptic transmission.
*Muscarinic (M2)*
- **M2 receptors** are **Gi-protein coupled receptors** mainly found in the heart, mediating decreased heart rate and contractility.
- In autonomic ganglia, M2 receptors could have a modulatory role, but they are not responsible for the slow excitatory phase of synaptic transmission.
*Nicotinic (N2)*
- **Nicotinic N2 receptors** (also known as **NN or neuronal nicotinic receptors**) mediate the **fast excitatory postsynaptic potential** (EPSP) in autonomic ganglia by opening ion channels.
- This leads to rapid depolarization and action potential generation, which is distinct from the **slower, prolonged phase** of transmission.
Cholinergic agonists (direct and indirect) US Medical PG Question 2: In patients with chronic obstructive pulmonary disease, stimulation of muscarinic acetylcholine receptors results in an increase in mucus secretion, smooth muscle contraction and bronchoconstriction. The end result is an increase in airway resistance. Which of the following pharmacologic agents interferes directly with this pathway?
- A. Epinephrine
- B. Albuterol
- C. Theophylline
- D. Ipratropium (Correct Answer)
- E. Metoprolol
Cholinergic agonists (direct and indirect) Explanation: ***Ipratropium***
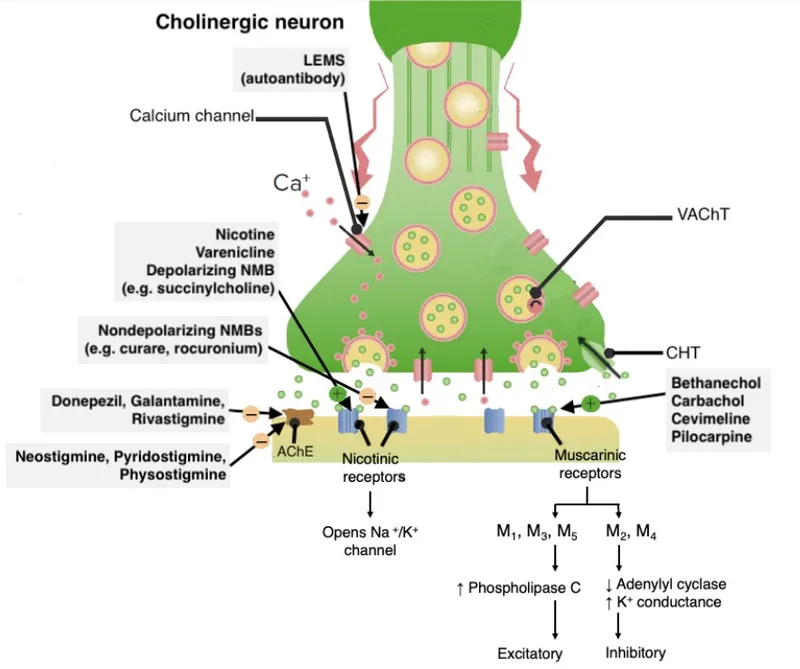
- **Ipratropium** is an **anticholinergic** agent that blocks muscarinic acetylcholine receptors.
- By blocking these receptors, it **reduces bronchoconstriction**, mucus secretion, and smooth muscle contraction, thus decreasing airway resistance.
*Epinephrine*
- **Epinephrine** is a non-selective **adrenergic agonist** that stimulates both alpha and beta receptors.
- Its effects in the airways are primarily mediated through **beta-2 agonism**, leading to bronchodilation, but it does not directly interfere with muscarinic pathways.
*Albuterol*
- **Albuterol** is a **short-acting beta-2 adrenergic agonist (SABA)**.
- It primarily causes bronchodilation by stimulating beta-2 receptors on airway smooth muscle, independent of the muscarinic pathway.
*Theophylline*
- **Theophylline** is a **methylxanthine** that primarily acts as a non-selective phosphodiesterase inhibitor.
- This leads to increased intracellular **cAMP** and bronchodilation, but it does not directly block muscarinic acetylcholine receptors.
*Metoprolol*
- **Metoprolol** is a **selective beta-1 adrenergic blocker** (beta-blocker).
- Its primary action is on the heart; it has minimal effect on airway beta-2 receptors at therapeutic doses due to its selectivity, and it does not interfere with the muscarinic pathway.
Cholinergic agonists (direct and indirect) US Medical PG Question 3: A forty-five-year-old farmer with past medical history of diabetes, hypertension, and possible narrow angles comes into your emergency room confused, diaphoretic, salivating, vomiting and shedding tears. He has pinpoint pupils. You conclude that he is showing effects of acute organophosphate poisoning. While administering the antidote, you should carefully monitor for which of the following side effects?
- A. Barotrauma to middle ear
- B. Bronchospasm
- C. Hyperkalemia
- D. Acute closed-angle glaucoma (Correct Answer)
- E. Tinnitus
Cholinergic agonists (direct and indirect) Explanation: ***Acute closed-angle glaucoma***
- **Atropine**, a common antidote for organophosphate poisoning, can dilate the pupils and **increase intraocular pressure**, precipitating acute closed-angle glaucoma in susceptible individuals.
- The patient's history of "possible narrow angles" indicates a predisposition to this condition, making careful monitoring essential during atropine administration.
*Barotrauma to middle ear*
- **Barotrauma** is typically associated with changes in **ambient pressure**, such as during air travel or diving.
- There is no direct physiological link between organophosphate poisoning treatment and middle ear barotrauma.
*Bronchospasm*
- **Organophosphate poisoning** *causes* bronchospasm due to excessive cholinergic stimulation, while atropine is used to *reverse* it.
- Therefore, bronchospasm would improve, not worsen, with appropriate antidote administration.
*Hyperkalemia*
- **Hyperkalemia** is not a direct side effect of atropine or a common complication of organophosphate poisoning treatment.
- While electrolyte imbalances can occur in critically ill patients, hyperkalemia is not specifically monitored for in this context.
*Tinnitus*
- **Tinnitus** is a perception of noise or ringing in the ears often associated with **auditory system damage** or certain medications.
- It is not a recognized side effect of atropine or a complication to specifically monitor for in organophosphate poisoning.
Cholinergic agonists (direct and indirect) US Medical PG Question 4: A 32-year-old farmer is brought to the emergency department by his wife. The patient was reportedly anxious, sweaty, and complaining of a headache and chest tightness before losing consciousness on route to the hospital. Which of the following is mechanistically responsible for this patient's symptoms?
- A. Reversible inhibition of acetylcholinesterase
- B. Competitive inhibition of acetylcholine at post-junctional effector sites
- C. Binding of acetylcholine agonists to post-junctional receptors
- D. Irreversible inhibition of acetylcholinesterase (Correct Answer)
- E. Inhibition of presynaptic exocytosis of acetylcholine vesicles
Cholinergic agonists (direct and indirect) Explanation: ***Irreversible inhibition of acetylcholinesterase***
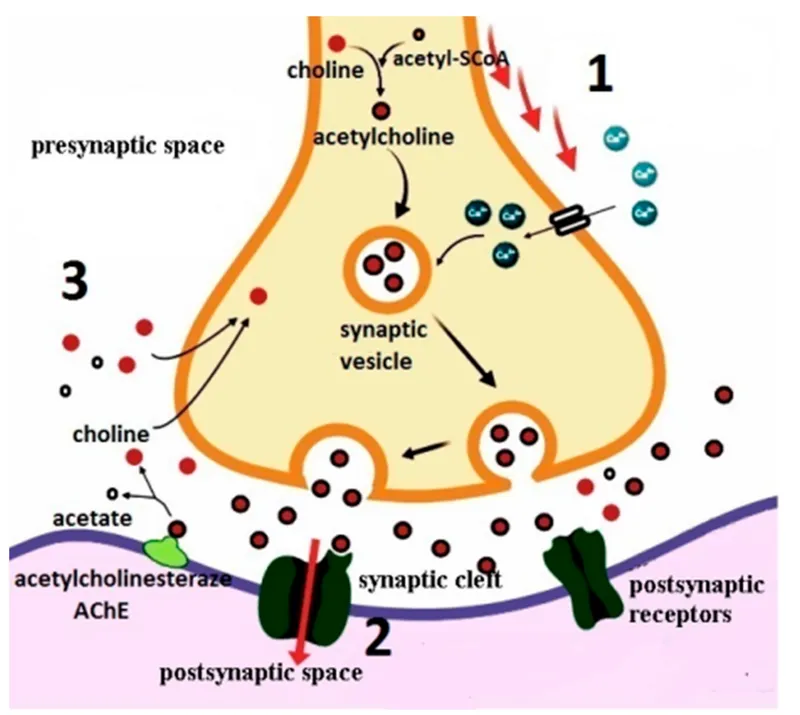
- The farmer's symptoms (anxiety, sweating, headache, chest tightness, loss of consciousness) are characteristic of **organophosphate poisoning**, which causes a cholinergic crisis due to accumulation of acetylcholine.
- Organophosphates are common in **pesticides** and act by irreversibly inhibiting **acetylcholinesterase**, leading to prolonged stimulation of cholinergic receptors.
*Reversible inhibition of acetylcholinesterase*
- Reversible acetylcholinesterase inhibitors, such as **physostigmine** or **neostigmine**, typically have a shorter duration of action and might cause similar symptoms but are less likely to lead to such severe, acute presentations in an accidental exposure scenario for a farmer.
- These agents are often used therapeutically and would not typically cause prolonged loss of consciousness in this context unless in very high intentional doses.
*Competitive inhibition of acetylcholine at post-junctional effector sites*
- This mechanism describes the action of **anticholinergic drugs** (e.g., atropine), which would block acetylcholine's effects and cause symptoms like dry mouth, dilated pupils, and tachycardia, opposite to what is observed here.
- Such agents would alleviate, not cause, the cholinergic symptoms seen in this patient.
*Binding of acetylcholine agonists to post-junctional receptors*
- While direct agonists (e.g., pilocarpine, methacholine) would mimic acetylcholine and cause cholinergic symptoms, organophosphate poisoning operates by preventing acetylcholine breakdown, rather than directly binding as an exogenous agonist.
- The context of a farmer and sudden, severe symptoms points more strongly to pesticide exposure and acetylcholinesterase inhibition.
*Inhibition of presynaptic exocytosis of acetylcholine vesicles*
- This mechanism is characteristic of **botulinum toxin**, which blocks the release of acetylcholine from presynaptic terminals, leading to muscle paralysis and weakness.
- The patient's symptoms are those of cholinergic excess, not cholinergic blockade or deficiency at the neuromuscular junction.
Cholinergic agonists (direct and indirect) US Medical PG Question 5: A 63-year-old man comes to the physician for blurry vision and increased difficulty walking over the past month. He feels very fatigued after watering his garden but feels better after taking a nap. He has not had any recent illness. He has smoked one pack of cigarettes daily for 35 years. Examination shows drooping of the upper eyelids bilaterally and diminished motor strength in the upper extremities. Sensation to light touch and deep tendon reflexes are intact. An x-ray of the chest shows low lung volumes bilaterally. A drug with which of the following mechanisms of action is most appropriate for this patient?
- A. Inhibition of acetylcholinesterase (Correct Answer)
- B. Stimulation of D2 receptors
- C. Regeneration of acetylcholinesterase
- D. Inhibition of muscarinic ACh receptor
- E. Stimulation of β2 adrenergic receptors
Cholinergic agonists (direct and indirect) Explanation: ***Inhibition of acetylcholinesterase***
- The patient's symptoms (blurry vision, difficulty walking, fatigue improving with rest, ptosis, and proximal muscle weakness) are classic for **Lambert-Eaton myasthenic syndrome (LEMS)**, strongly associated with **small cell lung cancer** given his heavy smoking history and chest X-ray findings.
- LEMS is caused by **autoantibodies against presynaptic voltage-gated calcium channels** at the neuromuscular junction, which **reduce acetylcholine release**.
- While **3,4-diaminopyridine** (a potassium channel blocker that increases ACh release) is the preferred treatment for LEMS, it is not among the options; **acetylcholinesterase inhibitors** (e.g., pyridostigmine) can provide symptomatic benefit by increasing acetylcholine availability in the synaptic cleft, making this the best available option.
- Note: Acetylcholinesterase inhibitors are more effective in **myasthenia gravis** than in LEMS, but may still provide modest improvement.
*Incorrect: Stimulation of D2 receptors*
- **D2 receptor agonists** (e.g., pramipexole, ropinirole) are used to treat **Parkinson's disease**, which presents with **resting tremor, rigidity, bradykinesia, and postural instability**.
- The patient's fatigable weakness, ptosis, and improvement with rest are characteristic of a neuromuscular junction disorder, not a basal ganglia disorder.
*Incorrect: Regeneration of acetylcholinesterase*
- **Acetylcholinesterase reactivators** like **pralidoxime** are used to treat **organophosphate poisoning**, where acetylcholinesterase is irreversibly phosphorylated.
- This patient has no history of pesticide exposure or cholinergic crisis symptoms (salivation, lacrimation, miosis, bronchospasm).
*Incorrect: Inhibition of muscarinic ACh receptor*
- **Muscarinic antagonists** (e.g., atropine, scopolamine) block parasympathetic effects and would **worsen neuromuscular transmission** by reducing cholinergic activity.
- Blocking acetylcholine receptors would exacerbate the patient's muscle weakness and ptosis.
*Incorrect: Stimulation of β2 adrenergic receptors*
- **Beta-2 agonists** (e.g., albuterol, salmeterol) are bronchodilators used for **asthma and COPD**.
- While the patient has a significant smoking history, his presentation is dominated by neuromuscular symptoms, not respiratory distress or bronchospasm.
Cholinergic agonists (direct and indirect) US Medical PG Question 6: A 16 year-old female is being evaluated for shortness of breath. For the last year she has had shortness of breath and subjective wheezing with exercise and intermittent coughing at night. She reports waking up from sleep coughing 1-2 times per month. She now skips gym class because of her symptoms. She denies any coughing, chest tightness, or shortness of breath on the day of her visit. On exam, her lungs are clear to auscultation bilaterally, with normal inspiratory to expiratory duration ratio. Her pulmonary function tests (PFTs) show normal FEV1 and FVC based on her age, gender, and height. She is told to inhale a medication, and her PFTs are repeated, now showing a FEV1 79% of her previous reading. The patient is diagnosed with asthma. Which of the following medications was used to diagnose the patient?
- A. Pilocarpine
- B. Carbachol
- C. Methacholine (Correct Answer)
- D. Bethanechol
- E. Physostigmine
Cholinergic agonists (direct and indirect) Explanation: ***Methacholine***
- **Methacholine** is a muscarinic cholinergic agonist that, when inhaled, causes **bronchoconstriction** in susceptible individuals, leading to a decrease in FEV1.
- A significant drop in FEV1 (typically 20% or more) after methacholine challenge is diagnostic for **asthma**, especially when baseline PFTs are normal.
*Pilocarpine*
- **Pilocarpine** is a muscarinic agonist primarily used to treat **glaucoma** (by causing miosis and reducing intraocular pressure) and **dry mouth/eyes**.
- It is not used for the diagnosis of asthma through bronchial challenge testing.
*Carbachol*
- **Carbachol** is a cholinergic agonist with both muscarinic and nicotinic activity, used mainly in ophthalmology to induce **miosis** during surgery.
- It is not a standard agent for bronchial provocation testing in asthma diagnosis.
*Bethanechol*
- **Bethanechol** is a muscarinic agonist used to treat **urinary retention** and reduce symptoms of **gastroesophageal reflux disease (GERD)**.
- It is not used for asthma diagnosis.
*Physostigmine*
- **Physostigmine** is an acetylcholinesterase inhibitor that indirectly increases acetylcholine levels, used as an **antidote for anticholinergic poisoning**.
- It is not used as a direct broncho-constrictor for asthma diagnosis.
Cholinergic agonists (direct and indirect) US Medical PG Question 7: A 30-year-old woman is undergoing work up for progressive weakness. She reports that at the end of the work day, her "eyelids droop" and her "eyes cross," but in the morning she feels "ok." She reports that her legs feel heavy when she climbs the stairs of her house to go to sleep at night. As part of her work up, the physician has her hold her gaze toward the ceiling, and after a minute, her lids become ptotic. She is given an IV medication and her symptoms resolve, but return 10 minutes later. Which of the following medications was used in the diagnostic test performed for this patient?
- A. Neostigmine
- B. Pyridostigmine
- C. Physostigmine
- D. Edrophonium (Correct Answer)
- E. Echothiophate
Cholinergic agonists (direct and indirect) Explanation: ***Edrophonium***
* The clinical picture strongly suggests **myasthenia gravis**, characterized by fluctuating muscle weakness that worsens with activity and improves with rest, exemplified by the patient's symptoms at the end of the day.
* **Edrophonium** is an **ultrashort-acting acetylcholinesterase inhibitor** used in the **Tensilon test** to diagnose myasthenia gravis. Its rapid onset and brief duration of action (symptoms resolve briefly then return) match the scenario described.
*Neostigmine*
* While **neostigmine** is an acetylcholinesterase inhibitor, it has a **longer duration of action** compared to edrophonium and is typically used for the *treatment* of myasthenia gravis, not primarily for the rapid diagnostic test.
* It is also used to reverse the effects of non-depolarizing neuromuscular blockers.
*Pyridostigmine*
* **Pyridostigmine** is a commonly used, **intermediate-acting acetylcholinesterase inhibitor** used for the *chronic management* of myasthenia gravis due to its longer duration (3-6 hours).
* It would not produce the rapid, transient improvement and return of symptoms seen in the diagnostic test described.
*Physostigmine*
* **Physostigmine** is an acetylcholinesterase inhibitor that can cross the **blood-brain barrier** and is primarily used to treat central anticholinergic toxicity.
* It is not used for the diagnosis of myasthenia gravis due to its central effects and different clinical indications.
*Echothiophate*
* **Echothiophate** is an **irreversible acetylcholinesterase inhibitor** used topically for glaucoma.
* Its irreversible nature and long duration of action make it unsuitable for a diagnostic test like the one described, as the effects would not resolve quickly.
Cholinergic agonists (direct and indirect) US Medical PG Question 8: A researcher is studying receptors that respond to epinephrine in the body and discovers a particular subset that is expressed in presynaptic adrenergic nerve terminals. She discovers that upon activation, these receptors will lead to decreased sympathetic nervous system activity. She then studies the intracellular second messenger changes that occur when this receptor is activated. She records these changes and begins searching for analogous receptor pathways. Which of the following receptors would cause the most similar set of intracellular second messenger changes?
- A. Muscarinic cholinoreceptors in the gastrointestinal tract
- B. Growth hormone receptors in the musculoskeletal system
- C. Vasopressin receptors in the kidney
- D. Dopamine receptors in the brain (Correct Answer)
- E. Aldosterone receptors in the kidney
Cholinergic agonists (direct and indirect) Explanation: ***Dopamine receptors in the brain***
- The described presynaptic receptors for epinephrine that decrease sympathetic activity are **alpha-2 adrenergic receptors**, which are **G inhibitory protein (Gi)-coupled receptors**.
- Gi-coupled receptors **inhibit adenylyl cyclase**, leading to a **decrease in intracellular cAMP**, a signaling pathway shared by **D2 dopamine receptors**.
*Muscarinic cholinoreceptors in the gastrointestinal tract*
- Most muscarinic receptors (M1 and M3) in the GI tract are **Gq-coupled**, leading to an **increase in phospholipase C (PLC) activity**, ultimately increasing intracellular **IP3 and DAG** and promoting smooth muscle contraction.
- This mechanism is distinct from the **Gi-mediated inhibition of cAMP** described for the presynaptic adrenergic receptor.
*Growth hormone receptors in the musculoskeletal system*
- Growth hormone receptors are **tyrosine kinase-associated receptors** (specifically, they are linked to **JAK/STAT pathways**), not G protein-coupled receptors.
- Their intracellular signaling involves **protein phosphorylation cascades**, which are fundamentally different from second messenger changes involving cAMP.
*Vasopressin receptors in the kidney*
- Vasopressin (ADH) acts on **V2 receptors** in the kidney, which are **G stimulatory protein (Gs)-coupled receptors**.
- Activation of V2 receptors leads to an **increase in adenylyl cyclase activity** and thus an **increase in intracellular cAMP**, the opposite effect of the described Gi-coupled receptor.
*Aldosterone receptors in the kidney*
- Aldosterone receptors are **intracellular steroid hormone receptors** that directly bind to DNA and regulate gene transcription.
- They do not engage in rapid intracellular second messenger changes like G protein-coupled receptors, but rather alter **protein synthesis** over hours to days.
Cholinergic agonists (direct and indirect) US Medical PG Question 9: A 64-year-old man is brought to the emergency department by his wife with a 2-hour history of diarrhea and vomiting. He says that he felt fine in the morning, but noticed that he was salivating, sweating, and feeling nauseated on the way home from his work as a landscaper. The diarrhea and vomiting then started about 10 minutes after he got home. His past medical history is significant for depression and drug abuse. His wife says that he has also been more confused lately and is afraid he may have ingested something unusual. Physical exam reveals miosis, rhinorrhea, wheezing, and tongue fasciculations. Which of the following treatments would most likely be effective for this patient?
- A. Sodium bicarbonate
- B. Naloxone
- C. Atropine (Correct Answer)
- D. Fomepizole
- E. Ammonium chloride
Cholinergic agonists (direct and indirect) Explanation: ***Atropine***
- This patient displays classic signs of **organophosphate poisoning**, characterized by **cholinergic crisis** (salivation, sweating, nausea, vomiting, diarrhea, miosis, rhinorrhea, wheezing, fasciculations). **Atropine** is a competitive antagonist of acetylcholine at muscarinic receptors and is the primary antidote, reversing most of these symptoms.
- The patient's profession as a **landscaper** increases his exposure risk, and the acute onset of symptoms supports a toxic exposure rather than an infection.
*Sodium bicarbonate*
- **Sodium bicarbonate** is primarily used to treat **metabolic acidosis**, such as in aspirin overdose or tricyclic antidepressant poisoning, or to alkalinize urine in certain toxic exposures.
- While metabolic acidosis can occur in severe organophosphate poisoning, it is not the primary treatment for the **cholinergic symptoms** themselves.
*Naloxone*
- **Naloxone** is an opioid antagonist used to reverse the effects of **opioid overdose**, characterized by respiratory depression, miosis, and central nervous system depression.
- The patient's symptoms of excessive secretions, gastrointestinal distress, and muscle fasciculations are inconsistent with opioid overdose.
*Fomepizole*
- **Fomepizole** is an alcohol dehydrogenase inhibitor used to treat **methanol and ethylene glycol poisoning**.
- These poisonings present with severe metabolic acidosis, visual disturbances (methanol), or renal failure (ethylene glycol), which are not the primary features described in this patient.
*Ammonium chloride*
- **Ammonium chloride** is an acidifying agent used to treat severe **metabolic alkalosis** or to increase the excretion of basic drugs.
- It is not indicated for the treatment of organophosphate poisoning and would likely exacerbate any existing acidosis.
Cholinergic agonists (direct and indirect) US Medical PG Question 10: A 67-year-old man presents to the emergency department acutely confused. The patient's wife found him mumbling incoherently in the kitchen this morning as they were preparing for a hike. The patient was previously healthy and only had a history of mild forgetfulness, depression, asthma, and seasonal allergies. His temperature is 98.5°F (36.9°C), blood pressure is 122/62 mmHg, pulse is 119/min, and oxygen saturation is 98% on room air. The patient is answering questions inappropriately and seems confused. Physical exam is notable for warm, flushed, and dry skin. The patient's pupils are dilated. Which of the following is also likely to be found in this patient?
- A. Hypoventilation
- B. QRS widening
- C. Coronary artery vasospasm
- D. Increased bronchial secretions
- E. Urinary retention (Correct Answer)
Cholinergic agonists (direct and indirect) Explanation: ***Urinary retention***
- The patient's symptoms (dilated pupils, warm/flushed/dry skin, confusion, tachycardia) are consistent with **anticholinergic toxidrome**.
- **Urinary retention** is a common manifestation of anticholinergic toxicity due to the paralysis of the detrusor muscle and contraction of the urethral sphincter.
*Hypoventilation*
- Anticholinergic toxicity typically causes **tachycardia** and may lead to tachypnea, not hypoventilation.
- Respiratory depression is more characteristic of **opioid** or **sedative-hypnotic** overdose.
*QRS widening*
- **QRS widening** is characteristic of **sodium channel blockade**, as seen with tricyclic antidepressant overdose, which can have anticholinergic effects but primarily causes cardiac toxicity via sodium channel blockade.
- While anticholinergics can cause arrhythmias, QRS widening specific to this mechanism isn't a primary feature of pure anticholinergic toxidrome.
*Coronary artery vasospasm*
- **Coronary artery vasospasm** is not a direct effect of anticholinergic toxicity.
- It is more commonly associated with drug use such as **cocaine**, or certain medications like **5-fluorouracil**.
*Increased bronchial secretions*
- Anticholinergic agents **decrease bronchial secretions** by blocking muscarinic receptors in the airway smooth muscle and glands.
- Increased bronchial secretions are characteristic of **cholinergic overdose**.
More Cholinergic agonists (direct and indirect) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.