Beta-adrenergic agonists US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Beta-adrenergic agonists. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Beta-adrenergic agonists US Medical PG Question 1: A 23-year-old woman presents to the emergency department with acute onset of shortness of breath, wheezing, and chest tightness. This is her 4th visit for these symptoms in the last 5 years. She tells you she recently ran out of her normal "controller" medication. Concerned for an asthma exacerbation, you begin therapy with a short-acting beta2-agonist. What is the expected cellular response to your therapy?
- A. Gs protein coupled receptor activates adenylyl cyclase and increases intracellular cAMP (Correct Answer)
- B. Gq protein coupled receptor activates phospholipase C and increases intracellular calcium
- C. Gq protein coupled receptor activates adenylyl cyclase and increases intracellular cAMP
- D. Gs protein coupled receptor activates phospholipase C and increases intracellular calcium
- E. Gi protein coupled receptor inhibits adenylyl cyclase and decreases cAMP
Beta-adrenergic agonists Explanation: ***Gs protein coupled receptor activates adenylyl cyclase and increases intracellular cAMP***
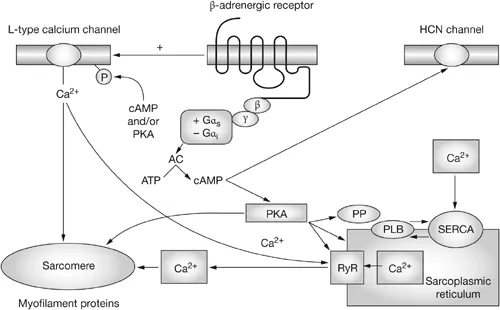
- **Short-acting beta2-agonists (SABAs)** like **albuterol** bind to **beta2-adrenergic receptors** on airway smooth muscle cells, which are **Gs protein-coupled receptors**.
- Activation of **Gs protein** stimulates **adenylyl cyclase**, leading to an increase in intracellular **cyclic AMP (cAMP)**, which triggers downstream relaxation of bronchial smooth muscle.
*Gq protein coupled receptor activates phospholipase C and increases intracellular calcium*
- **Gq protein-coupled receptors** are typically associated with **alpha1-adrenergic receptors** or **muscarinic M1/M3 receptors**, which, when activated, cause **bronchoconstriction** not bronchodilation.
- Activation of **Gq protein** leads to activation of **phospholipase C**, which generates **IP3** and **DAG**, ultimately increasing intracellular **calcium** and promoting contraction.
*Gq protein coupled receptor activates adenylyl cyclase and increases intracellular cAMP*
- This option incorrectly pairs **Gq protein** with the activation of **adenylyl cyclase** and an increase in **cAMP**.
- **Gq protein** signaling primarily involves the **phospholipase C pathway** and **calcium** mobilization, not direct adenylyl cyclase activation.
*Gs protein coupled receptor activates phospholipase C and increases intracellular calcium*
- This option incorrectly pairs **Gs protein** with the activation of **phospholipase C** and an increase in intracellular **calcium**.
- **Gs protein** is specifically coupled to the **adenylyl cyclase/cAMP pathway**, while **phospholipase C** and **calcium** are associated with **Gq protein** signaling.
*Gi protein coupled receptor inhibits adenylyl cyclase and decreases cAMP*
- **Gi protein-coupled receptors** inhibit **adenylyl cyclase** and decrease intracellular **cAMP**, which would lead to **bronchoconstriction**, not bronchodilation.
- This mechanism is associated with **M2 muscarinic receptors** on presynaptic terminals, which regulate acetylcholine release, or alpha2-adrenergic receptors, which are not the primary target for bronchodilation in asthma exacerbations.
Beta-adrenergic agonists US Medical PG Question 2: A patient presents with periods of severe headaches and flushing however every time they have come to the physician they have not experienced any symptoms. The only abnormal finding is a blood pressure of 175 mmHg/100 mmHg. It is determined that the optimal treatment for this patient is surgical. Prior to surgery which of the following noncompetitive inhibitors should be administered?
- A. Phentolamine
- B. Isoproterenol
- C. Atropine
- D. Propranolol
- E. Phenoxybenzamine (Correct Answer)
Beta-adrenergic agonists Explanation: ***Phenoxybenzamine***
- This patient likely has a **pheochromocytoma**, which explains the episodic headaches, flushing, and hypertension. **Phenoxybenzamine** is a **non-competitive, irreversible alpha-adrenergic blocker** that is crucial for preoperative preparation to prevent a **hypertensive crisis** during surgery.
- Its **irreversible binding** provides sustained alpha blockade, essential to control blood pressure and avoid catecholamine-induced surges during tumor manipulation.
*Phentolamine*
- **Phentolamine** is a **competitive alpha-adrenergic blocker** used to manage acute hypertensive episodes, but it has a shorter duration of action.
- It is not preferred for sustained preoperative alpha blockade due to its **reversible nature** and potential for drug washout during surgery, which could lead to catecholamine surges.
*Isoproterenol*
- **Isoproterenol** is a **beta-adrenergic agonist** that increases heart rate and contractility, and causes bronchodilation.
- It would be contraindicated in a patient with pheochromocytoma as it could worsen hypertension and cardiac symptoms by stimulating beta receptors that are already overly sensitive to endogenous catecholamines.
*Atropine*
- **Atropine** is a **muscarinic acetylcholine receptor antagonist** that blocks parasympathetic effects, like bradycardia and salivation.
- It has no role in managing hypertension or the catecholamine excess seen in pheochromocytoma.
*Propranolol*
- **Propranolol** is a **non-selective beta-adrenergic blocker** that can be used to control tachycardia and arrhythmias in pheochromocytoma, but only *after* adequate alpha-blockade has been established.
- Using **propranolol alone** or before alpha-blockade can lead to **unopposed alpha-adrenergic stimulation**, resulting in a severe, life-threatening hypertensive crisis.
Beta-adrenergic agonists US Medical PG Question 3: A 45-year-old unconscious man is brought to the emergency department by a friend who witnessed him collapse. They were working in a greenhouse spraying the vegetables when the man started to complain of blurred vision and nausea. On the way to the hospital, the man lost consciousness and lost bladder continence. The patient’s vital signs are as follows: blood pressure 95/60 mm Hg; heart rate 59/min; respiratory rate 22/min; and temperature 36.0℃ (96.8℉). On examination, he is unconscious with a GCS score of 7. His pupils are contracted and react poorly to light. Lung auscultation reveals diffuse wheezing. Cardiac auscultation is significant for bradycardia. Abdominal auscultation reveals increased bowel sounds. A cardiac monitor shows bradycardia with grade 2 AV-block. Which of the following leads to the cardiac manifestations seen in this patient?
- A. Activation of M1-cholinergic receptors
- B. Activation of β2-adrenergic receptors
- C. Activation of M2-cholinergic receptors (Correct Answer)
- D. Inhibition of β1-adrenergic receptors
- E. Inhibition of M2-cholinergic receptors
Beta-adrenergic agonists Explanation: ***Activation of M2-cholinergic receptors***
- The patient's symptoms (blurred vision, nausea, unconsciousness, incontinence, miosis, wheezing, bradycardia, increased bowel sounds) are classic for **organophosphate poisoning**, which involves excessive activation of the **parasympathetic nervous system**.
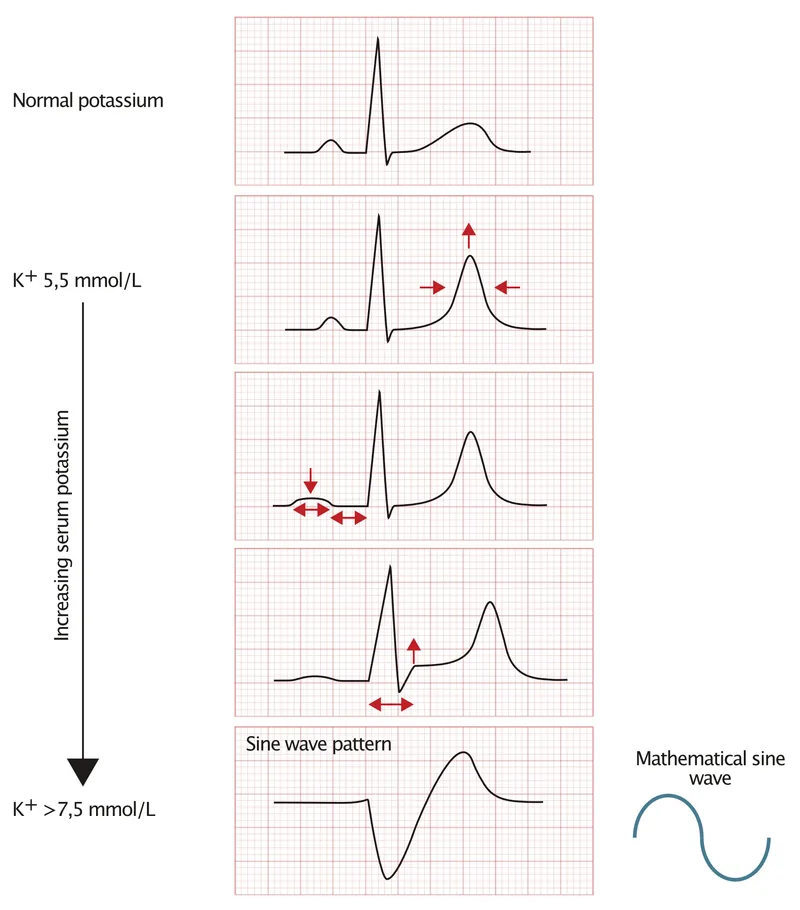
- **M2 receptors** are primarily located in the heart and, when activated by acetylcholine, lead to slowed heart rate (bradycardia) and decreased conduction (AV block), characteristic of the cardiac manifestations observed.
*Activation of M1-cholinergic receptors*
- **M1 receptors** are primarily found in neural tissue and glands, contributing to increased GI motility and glandular secretions but not directly to cardiac slowing.
- Their activation does not directly cause the observed **bradycardia** and **AV block**.
*Activation of β2-adrenergic receptors*
- **β2-adrenergic receptors** are part of the sympathetic nervous system and are present in the smooth muscle of the bronchioles and blood vessels.
- Their activation typically causes **bronchodilation** and **vasodilation**, which would counteract the patient's wheezing and hypotension, and are not involved in bradycardia.
*Inhibition of β1-adrenergic receptors*
- **β1-adrenergic receptors** are found in the heart and their inhibition would lead to bradycardia, but organophosphate poisoning causes **cholinergic excess**, not adrenergic inhibition.
- This mechanism would not explain the other widespread **parasympathetic activation** symptoms like miosis, wheezing, and increased GI motility.
*Inhibition of M2-cholinergic receptors*
- **Inhibition of M2-cholinergic receptors** would lead to an increase in heart rate and improved AV conduction, rather than the severe **bradycardia** and **AV block** observed.
- This mechanism is characteristic of **anticholinergic toxidrome**, which presents with opposing symptoms.
Beta-adrenergic agonists US Medical PG Question 4: A 55-year-old woman comes to the physician because of involuntary hand movements that improve with alcohol consumption. Physical examination shows bilateral hand tremors that worsen when the patient is asked to extend her arms out in front of her. The physician prescribes a medication that is associated with an increased risk of bronchospasms. This drug has which of the following immediate effects on the cardiovascular system?
Stroke volume | Heart rate | Peripheral vascular resistance
- A. ↓ ↓ ↓
- B. ↓ ↓ ↑ (Correct Answer)
- C. ↓ ↑ ↑
- D. ↑ ↑ ↑
- E. ↑ ↑ ↓
Beta-adrenergic agonists Explanation: ***↓ ↓ ↑***
- This patient likely has **essential tremor**, which is characterized by **bilateral hand tremors** that improve with alcohol and worsen with intention (postural tremor). The prescribed medication is a **beta-blocker** (e.g., propranolol), which is associated with an increased risk of bronchospasms due to blocking **beta-2 receptors** in the airways.
- Beta-blockers **decrease heart rate** (negative chronotropic effect) and **stroke volume** (negative inotropic effect) by blocking beta-1 receptors in the heart, reducing cardiac output.
- **Peripheral vascular resistance increases** acutely due to: (1) **unopposed alpha-1 adrenergic tone** in blood vessels (loss of beta-2 mediated vasodilation), and (2) baroreceptor-mediated reflex vasoconstriction in response to decreased cardiac output. This helps maintain blood pressure despite reduced cardiac output.
*↓ ↓ ↓*
- While beta-blockers decrease **heart rate** and **stroke volume**, peripheral vascular resistance does not decrease acutely. A decrease in all three parameters would cause severe hypotension.
- The loss of beta-2 receptor-mediated vasodilation and baroreceptor reflexes lead to increased, not decreased, peripheral vascular resistance.
*↓ ↑ ↑*
- Beta-blockers **decrease heart rate** through beta-1 blockade, not increase it. This is their primary cardiac mechanism of action.
- An increase in heart rate would be expected with sympathomimetic drugs or anticholinergics, not beta-blockers.
*↑ ↑ ↑*
- This combination indicates increased cardiovascular activity, which is the opposite effect of **beta-blockers**.
- Beta-blockers reduce heart rate and stroke volume by blocking beta-1 receptors; they do not increase these parameters.
- This pattern would suggest sympathetic activation or administration of an adrenergic agonist.
*↑ ↑ ↓*
- Beta-blockers **decrease** (not increase) both heart rate and stroke volume through beta-1 receptor blockade.
- While decreased peripheral vascular resistance occurs with vasodilators, beta-blockers acutely **increase** PVR due to unopposed alpha-adrenergic tone.
Beta-adrenergic agonists US Medical PG Question 5: A 53-year-old woman presents to a physician for a regular check-up. She has no complaints, but notes that she has been anxious and easily irritable for no particular reason over the past year. Six months ago, she was diagnosed with grade I arterial hypertension and prescribed lifestyle modification and weight loss to control her blood pressure. She currently takes aspirin (81 mg) and rosuvastatin (10 mg) daily. The vital signs are as follows: blood pressure 145/80 mm Hg, heart rate 81/min, respiratory rate 14/min, and temperature 36.6℃ (97.9℉). She weighs 91 kg (213.8 lb), the height is 167 cm (5.5 ft), and the BMI is 32.6 kg/m2. The physical examination is unremarkable. Blood testing was performed, and the results are shown below.
Plasma glucose 109.9 mg/dL (6.1 mmol/L)
Plasma triglycerides 185.8 mg/dL (2.1 mmol/L)
Na+ 141 mEq/L
K+ 4.2 mEq/L
The patient was prescribed atenolol. If the medication alone affects the patient’s measurements, which laboratory finding would you expect to note several weeks after the treatment is initiated?
- A. Plasma glucose 54 mg/dL (3.0 mmol/L)
- B. Plasma triglycerides 150.4 mg/dL (1.7 mmol/L) (Correct Answer)
- C. Na+ 137 mEq/L
- D. Na+ 148 mEq/L
- E. K+ 2.6 mEq/L
Beta-adrenergic agonists Explanation: ***Plasma triglycerides 150.4 mg/dL (1.7 mmol/L)***
- Beta-blockers, including atenolol, can cause **modest increases in triglycerides** (typically 10-20%) and **decreases in HDL cholesterol**.
- However, a **decrease in triglycerides** from 185.8 to 150.4 mg/dL would be **unexpected and beneficial** if it occurred, but is **not a typical effect** of beta-blockers.
- Among the options provided, this represents the **least implausible change**, though it goes in the opposite direction of the expected effect.
- Note: The patient is already on rosuvastatin, which affects lipids, but the question specifies "medication alone" referring to atenolol.
*Plasma glucose 54 mg/dL (3.0 mmol/L)*
- While beta-blockers can **mask hypoglycemia symptoms** and slightly impair glucose tolerance, atenolol as a β1-selective agent has **minimal effect on glucose metabolism** in non-diabetic patients.
- Severe hypoglycemia (54 mg/dL) would **not be expected** in a non-diabetic patient taking atenolol alone.
*Na+ 137 mEq/L*
- Beta-blockers are **not associated with hyponatremia** or significant changes in serum sodium.
- A decrease from 141 to 137 mEq/L is within normal variation and **not a recognized pharmacological effect** of atenolol.
*Na+ 148 mEq/L*
- Beta-blockers do **not cause hypernatremia**.
- An increase to 148 mEq/L would suggest **dehydration or other causes**, not atenolol therapy.
*K+ 2.6 mEq/L*
- Beta-blockers can cause **mild hyperkalemia** (increased potassium), not hypokalemia, by inhibiting β2-receptor-mediated cellular potassium uptake and reducing renin-aldosterone activity.
- **Hypokalemia (2.6 mEq/L) is the opposite** of what would be expected and would suggest other causes such as diuretic use or GI losses.
Beta-adrenergic agonists US Medical PG Question 6: An epidemiologist is evaluating the efficacy of Noxbinle in preventing HCC deaths at the population level. A clinical trial shows that over 5 years, the mortality rate from HCC was 25% in the control group and 15% in patients treated with Noxbinle 100 mg daily. Based on this data, how many patients need to be treated with Noxbinle 100 mg to prevent, on average, one death from HCC?
- A. 20
- B. 73
- C. 10 (Correct Answer)
- D. 50
- E. 100
Beta-adrenergic agonists Explanation: ***10***
- The **number needed to treat (NNT)** is calculated by first finding the **absolute risk reduction (ARR)**.
- **ARR** = Risk in control group - Risk in treatment group = 25% - 15% = **10%** (or 0.10).
- **NNT = 1 / ARR** = 1 / 0.10 = **10 patients**.
- This means that **10 patients must be treated with Noxbinle to prevent one death from HCC** over 5 years.
*20*
- This would result from an ARR of 5% (1/0.05 = 20), which is not supported by the data.
- May arise from miscalculating the risk difference or incorrectly halving the actual ARR.
*73*
- This value does not correspond to any standard calculation of NNT from the given mortality rates.
- May result from confusion with other epidemiological measures or calculation error.
*50*
- This would correspond to an ARR of 2% (1/0.02 = 50), which significantly underestimates the actual risk reduction.
- Could result from incorrectly calculating the difference as a proportion rather than absolute percentage points.
*100*
- This would correspond to an ARR of 1% (1/0.01 = 100), grossly underestimating the treatment benefit.
- May result from confusing ARR with relative risk reduction or other calculation errors.
Beta-adrenergic agonists US Medical PG Question 7: A 70-year-old male presents for an annual exam. His past medical history is notable for shortness of breath when he sleeps, and upon exertion. Recently he has experienced dyspnea and lower extremity edema that seems to be worsening. Both of these symptoms have resolved since he was started on several medications and instructed to weigh himself daily. Which of the following is most likely a component of his medical management?
- A. Lidocaine
- B. Verapamil
- C. Carvedilol (Correct Answer)
- D. Aspirin
- E. Ibutilide
Beta-adrenergic agonists Explanation: ***Carvedilol***
- The patient exhibits classic symptoms of **heart failure**, such as **dyspnea on exertion**, **orthopnea** (shortness of breath when he sleeps), and **lower extremity edema**.
- **Beta-blockers** like carvedilol are essential for managing **chronic heart failure** by reducing myocardial oxygen demand and improving cardiac function.
*Lidocaine*
- **Lidocaine** is primarily an **antiarrhythmic drug** used for acute treatment of **ventricular arrhythmias**, not for chronic heart failure management.
- It works by blocking sodium channels and has no direct benefit in addressing the underlying pathophysiology of heart failure.
*Verapamil*
- **Verapamil** is a **non-dihydropyridine calcium channel blocker** typically used for hypertension, angina, and supraventricular tachyarrhythmias.
- It can have **negative inotropic effects**, which are generally contraindicated or used with extreme caution in patients with **systolic heart failure** due to its potential to worsen cardiac function.
*Aspirin*
- **Aspirin** is an **antiplatelet agent** used for primary or secondary prevention of **atherosclerotic cardiovascular disease** (e.g., in patients with coronary artery disease).
- It does not directly manage the symptoms or pathophysiology of **heart failure** unless there is a coexisting ischemic etiology.
*Ibutilide*
- **Ibutilide** is an **antiarrhythmic drug** specifically used for the rapid conversion of **atrial flutter and atrial fibrillation** of recent onset to sinus rhythm.
- It is not a medication used for the long-term management of **heart failure** symptoms described in the patient.
Beta-adrenergic agonists US Medical PG Question 8: You are currently employed as a clinical researcher working on clinical trials of a new drug to be used for the treatment of Parkinson's disease. Currently, you have already determined the safe clinical dose of the drug in a healthy patient. You are in the phase of drug development where the drug is studied in patients with the target disease to determine its efficacy. Which of the following phases is this new drug currently in?
- A. Phase 4
- B. Phase 1
- C. Phase 2 (Correct Answer)
- D. Phase 0
- E. Phase 3
Beta-adrenergic agonists Explanation: ***Phase 2***
- **Phase 2 trials** involve studying the drug in patients with the target disease to assess its **efficacy** and further evaluate safety, typically involving a few hundred patients.
- The question describes a stage after safe dosing in healthy patients (Phase 1) and before large-scale efficacy confirmation (Phase 3), focusing on efficacy in the target population.
*Phase 4*
- **Phase 4 trials** occur **after a drug has been approved** and marketed, monitoring long-term effects, optimal use, and rare side effects in a diverse patient population.
- This phase is conducted post-market approval, whereas the question describes a drug still in development prior to approval.
*Phase 1*
- **Phase 1 trials** primarily focus on determining the **safety and dosage** of a new drug in a **small group of healthy volunteers** (or sometimes patients with advanced disease if the drug is highly toxic).
- The question states that the safe clinical dose in a healthy patient has already been determined, indicating that Phase 1 has been completed.
*Phase 0*
- **Phase 0 trials** are exploratory, very early-stage studies designed to confirm that the drug reaches the target and acts as intended, typically involving a very small number of doses and participants.
- These trials are conducted much earlier in the development process, preceding the determination of safe clinical doses and large-scale efficacy studies.
*Phase 3*
- **Phase 3 trials** are large-scale studies involving hundreds to thousands of patients to confirm **efficacy**, monitor side effects, compare it to commonly used treatments, and collect information that will allow the drug to be used safely.
- While Phase 3 does assess efficacy, it follows Phase 2 and is typically conducted on a much larger scale before submitting for regulatory approval.
Beta-adrenergic agonists US Medical PG Question 9: A 48-year-old man presents to the emergency department with complaints of substernal chest pain for the past 1 hour. The pain is crushing in nature and radiates to his neck and left arm. He rates the pain as 7/10. He gives a history of similar episodes in the past that resolved with rest. He is a non-smoker and drinks alcohol occasionally. On physical examination, the temperature is 37.0°C (98.6°F), the pulse rate is 130/min and irregular, the blood pressure is 148/92 mm Hg, and the respiratory rate is 18/min. The physician immediately orders an electrocardiogram, the findings of which are consistent with an acute Q-wave myocardial infarction (MI). After appropriate emergency management, he is admitted to the medical floor. He develops atrial fibrillation on the second day of admission. He is given a β-adrenergic blocking agent for the arrhythmia. On discharge, he is advised to continue the medication for at least 2 years. Which of the following β-adrenergic blocking agents was most likely prescribed to this patient?
- A. Atenolol (Correct Answer)
- B. Penbutolol
- C. Acebutolol
- D. Pindolol
- E. Celiprolol
Beta-adrenergic agonists Explanation: ***Atenolol***
- **Atenolol** is a **cardioselective β1-blocker** that is commonly prescribed for atrial fibrillation, especially post-MI, due to its efficacy in reducing heart rate and improving survival.
- It lacks **intrinsic sympathomimetic activity (ISA)**, which is crucial for the post-MI setting to ensure adequate beta-blockade and prevent adverse cardiac events.
*Penbutolol*
- **Penbutolol** is a **non-selective β-blocker** with **intrinsic sympathomimetic activity (ISA)**.
- Beta-blockers with ISA are generally **contraindicated or not preferred** in post-MI patients because their partial agonist activity might negate the protective effects of beta-blockade on myocardial oxygen demand and arrhythmogenesis.
*Acebutolol*
- **Acebutolol** is a **cardioselective β1-blocker** with **intrinsic sympathomimetic activity (ISA)**.
- Like other beta-blockers with ISA, acebutolol is **not typically recommended** for long-term use after myocardial infarction due to concerns about reduced cardioprotective benefits.
*Pindolol*
- **Pindolol** is a **non-selective β-blocker** with **intrinsic sympathomimetic activity (ISA)**.
- Its partial agonist activity can lead to **less reduction in heart rate and myocardial contractility** compared to beta-blockers without ISA, making it an unsuitable choice for post-MI management.
*Celiprolol*
- **Celiprolol** is a **cardioselective β1-blocker** that also has **β2-agonist properties** and **intrinsic sympathomimetic activity (ISA)**.
- Its β2-agonist and ISA effects make it **less desirable post-MI** as it may not provide the full cardioprotective benefits of a pure β-blocker.
Beta-adrenergic agonists US Medical PG Question 10: Match the following:
Column A:
a. Beta 1
b. Beta 2
c. Beta 3
Column B:
1. Mirabegron
2. Betaxolol
3. Salbutamol
- A. a-2, b-3 ,c-1 (Correct Answer)
- B. a-2, b-1, c-3
- C. a-3, b-2, c-1
- D. a-3, b-1, c-2
Beta-adrenergic agonists Explanation: ***a-2, b-3, c-1***
- This pairing correctly matches **Betaxolol** with **Beta 1 selective** antagonism, **Salbutamol** with **Beta 2 selective** agonism, and **Mirabegron** with **Beta 3 selective** agonism.
- **Betaxolol** is a beta-1 selective adrenergic receptor antagonist, primarily used in ophthalmology to reduce intraocular pressure and as an antihypertensive. **Salbutamol** is a selective beta-2 adrenergic agonist used as a bronchodilator in asthma and COPD, causing relaxation of bronchial smooth muscle. **Mirabegron** is a selective beta-3 adrenergic agonist used to treat overactive bladder by relaxing the detrusor muscle.
*a-2, b-1, c-3*
- This option incorrectly assigns **Mirabegron** to Beta 2. Mirabegron is a **Beta 3 selective agonist**.
- It also incorrectly assigns **Salbutamol** to Beta 3. Salbutamol is a **Beta 2 selective agonist**.
*a-3, b-2, c-1*
- This option incorrectly assigns **Salbutamol** to Beta 1. Salbutamol is a **Beta 2 selective agonist**.
- It also incorrectly assigns **Betaxolol** to Beta 2. Betaxolol is a **Beta 1 selective antagonist**.
*a-3, b-1, c-2*
- This option incorrectly assigns **Salbutamol** to Beta 1 and **Betaxolol** to Beta 3.
- **Salbutamol** is a Beta 2 selective agonist, and **Betaxolol** is a Beta 1 selective antagonist.
More Beta-adrenergic agonists US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.