Alpha-adrenergic antagonists US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Alpha-adrenergic antagonists. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Alpha-adrenergic antagonists US Medical PG Question 1: A 68-year-old man with hypertension comes to the physician because of fatigue and difficulty initiating urination. He wakes up several times a night to urinate. He does not take any medications. His blood pressure is 166/82 mm Hg. Digital rectal examination shows a firm, non-tender, and uniformly enlarged prostate. Which of the following is the most appropriate pharmacotherapy?
- A. Finasteride
- B. α-Methyldopa
- C. Phenoxybenzamine
- D. Terazosin (Correct Answer)
- E. Tamsulosin
Alpha-adrenergic antagonists Explanation: ***Terazosin***
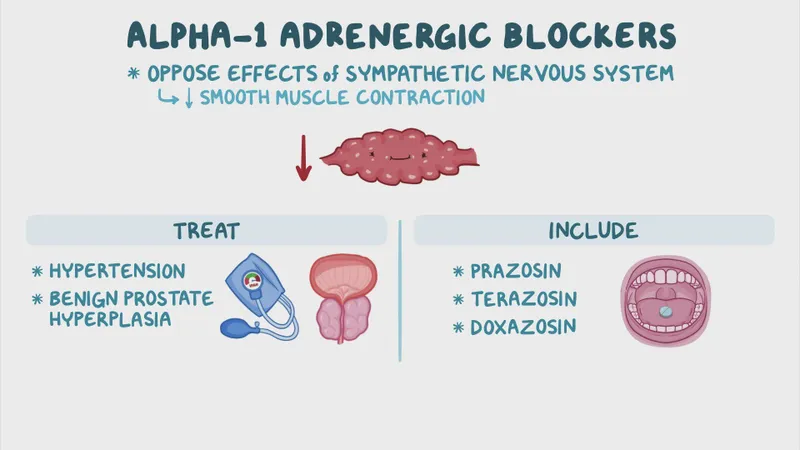
- **Terazosin** is an alpha-1 blocker that relaxes the smooth muscles in the prostate and bladder neck, improving urine flow and relieving symptoms of **benign prostatic hyperplasia (BPH)**.
- It also has the added benefit of lowering blood pressure, making it suitable for this patient with both **BPH** and **hypertension**.
*Finasteride*
- **Finasteride** is a 5-alpha reductase inhibitor that reduces prostate volume by inhibiting the conversion of testosterone to **dihydrotestosterone (DHT)**.
- While effective for **BPH**, it takes longer to show benefits (6-12 months) and does not address the patient's **hypertension**.
*α-Methyldopa*
- **α-Methyldopa** is a centrally acting alpha-2 adrenergic agonist used to treat **hypertension**, particularly in pregnancy.
- It does not have a direct effect on prostate smooth muscle and would not alleviate the patient's urinary symptoms.
*Phenoxybenzamine*
- **Phenoxybenzamine** is a non-selective, irreversible alpha-adrenergic blocker primarily used for **pheochromocytoma** to control blood pressure.
- Its non-selective nature and side effect profile make it less suitable for chronic management of **BPH** and **hypertension** compared to selective alpha-1 blockers.
*Tamsulosin*
- **Tamsulosin** is a selective alpha-1A adrenergic blocker that specifically targets the prostate, rapidly improving **BPH** symptoms with less effect on blood pressure.
- While it effectively treats **BPH**, unlike terazosin, it does not offer the additional advantage of lowering the patient's elevated blood pressure.
Alpha-adrenergic antagonists US Medical PG Question 2: A patient presents with periods of severe headaches and flushing however every time they have come to the physician they have not experienced any symptoms. The only abnormal finding is a blood pressure of 175 mmHg/100 mmHg. It is determined that the optimal treatment for this patient is surgical. Prior to surgery which of the following noncompetitive inhibitors should be administered?
- A. Phentolamine
- B. Isoproterenol
- C. Atropine
- D. Propranolol
- E. Phenoxybenzamine (Correct Answer)
Alpha-adrenergic antagonists Explanation: ***Phenoxybenzamine***
- This patient likely has a **pheochromocytoma**, which explains the episodic headaches, flushing, and hypertension. **Phenoxybenzamine** is a **non-competitive, irreversible alpha-adrenergic blocker** that is crucial for preoperative preparation to prevent a **hypertensive crisis** during surgery.
- Its **irreversible binding** provides sustained alpha blockade, essential to control blood pressure and avoid catecholamine-induced surges during tumor manipulation.
*Phentolamine*
- **Phentolamine** is a **competitive alpha-adrenergic blocker** used to manage acute hypertensive episodes, but it has a shorter duration of action.
- It is not preferred for sustained preoperative alpha blockade due to its **reversible nature** and potential for drug washout during surgery, which could lead to catecholamine surges.
*Isoproterenol*
- **Isoproterenol** is a **beta-adrenergic agonist** that increases heart rate and contractility, and causes bronchodilation.
- It would be contraindicated in a patient with pheochromocytoma as it could worsen hypertension and cardiac symptoms by stimulating beta receptors that are already overly sensitive to endogenous catecholamines.
*Atropine*
- **Atropine** is a **muscarinic acetylcholine receptor antagonist** that blocks parasympathetic effects, like bradycardia and salivation.
- It has no role in managing hypertension or the catecholamine excess seen in pheochromocytoma.
*Propranolol*
- **Propranolol** is a **non-selective beta-adrenergic blocker** that can be used to control tachycardia and arrhythmias in pheochromocytoma, but only *after* adequate alpha-blockade has been established.
- Using **propranolol alone** or before alpha-blockade can lead to **unopposed alpha-adrenergic stimulation**, resulting in a severe, life-threatening hypertensive crisis.
Alpha-adrenergic antagonists US Medical PG Question 3: A 53-year-old man presents to the office for a routine examination. The medical history is significant for diabetes mellitus, for which he is taking metformin. The medical records show blood pressure readings from three separate visits to fall in the 130–160 mm Hg range for systolic and 90–100 mm Hg range for diastolic. Prazosin is prescribed. Which of the following are effects of this drug?
- A. Vasodilation, decreased heart rate, bronchial constriction
- B. Vasodilation, increased peristalsis, bronchial dilation
- C. Vasoconstriction, bladder sphincter constriction, mydriasis
- D. Vasoconstriction, increase in AV conduction rate, bronchial dilation
- E. Vasodilation, bladder sphincter relaxation (Correct Answer)
Alpha-adrenergic antagonists Explanation: ***Vasodilation, bladder sphincter relaxation***
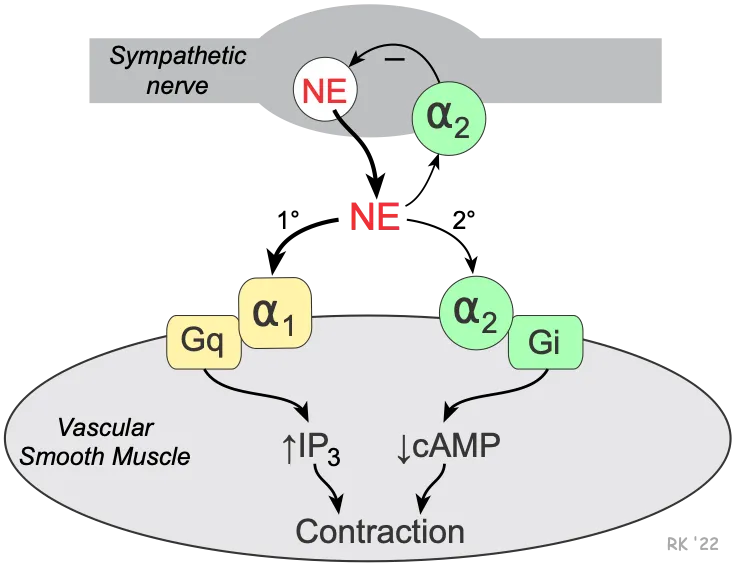
- **Prazosin** is an **alpha-1 adrenergic receptor antagonist**, which blocks the effects of norepinephrine on vascular smooth muscle, leading to **vasodilation** and decreased blood pressure.
- Blocking alpha-1 receptors in the bladder neck and prostate causes **bladder sphincter relaxation**, which can improve urine flow and is also useful in benign prostatic hyperplasia (BPH).
- These are the two primary clinically relevant effects of alpha-1 blockade with prazosin.
*Vasodilation, decreased heart rate, bronchial constriction*
- While prazosin causes **vasodilation**, it does not typically decrease heart rate directly; alpha-1 blockade can lead to **reflex tachycardia** due to decreased blood pressure.
- Prazosin has no significant effect on bronchial smooth muscle and does not cause **bronchial constriction**; bronchial effects are primarily mediated by beta-2 receptors or muscarinic (M3) receptors.
*Vasodilation, increased peristalsis, bronchial dilation*
- Prazosin does cause **vasodilation** but does not directly cause **increased peristalsis**; gastrointestinal motility is mainly regulated by the autonomic nervous system via muscarinic receptors and the enteric nervous system.
- Prazosin does not cause **bronchial dilation**; this effect is mediated by beta-2 adrenergic receptor stimulation.
*Vasoconstriction, bladder sphincter constriction, mydriasis*
- Prazosin is an alpha-1 antagonist, meaning it *blocks* **vasoconstriction** and instead causes vasodilation.
- Similarly, it causes **bladder sphincter relaxation**, not constriction.
- Prazosin has minimal effects on pupil size; mydriasis would be caused by alpha-1 agonists or muscarinic antagonists, not alpha-1 antagonists.
*Vasoconstriction, increase in AV conduction rate, bronchial dilation*
- Prazosin causes **vasodilation**, not vasoconstriction.
- It does not significantly affect **AV conduction rate** or directly cause **bronchial dilation**.
Alpha-adrenergic antagonists US Medical PG Question 4: A 55-year-old man comes to the physician because of intermittent palpitations that occur when he is stressed, exercising, or when he drinks alcohol. Physical examination shows an irregularly irregular pulse. An ECG shows irregular QRS complexes without any discrete P waves. Pharmacotherapy with carvedilol is initiated for his condition. Compared to treatment with propranolol, which of the following adverse effects is most likely?
- A. Bradycardia
- B. Bronchospasm
- C. Hyperkalemia
- D. Hypotension (Correct Answer)
- E. Hyperglycemia
Alpha-adrenergic antagonists Explanation: ***Hypotension***
- **Carvedilol** is a non-selective beta-blocker with additional **alpha-1 adrenergic receptor blocking activity**, which leads to peripheral vasodilation and a greater potential for **hypotension** compared to propranolol (a pure beta-blocker).
- The **alpha-1 blockade** causes a reduction in peripheral vascular resistance, leading to a more pronounced decrease in blood pressure.
*Bradycardia*
- Both carvedilol and propranolol are beta-blockers and can cause **bradycardia** by reducing heart rate.
- However, the question asks for an adverse effect **more likely** with carvedilol compared to propranolol, and while both can cause bradycardia, carvedilol's additional alpha-blocking activity makes hypotension more distinguishing.
*Bronchospasm*
- Both carvedilol and propranolol are **non-selective beta-blockers** (blocking both beta-1 and beta-2 receptors) and can cause **bronchospasm** by blocking beta-2 receptors in the bronchi.
- Therefore, this adverse effect is common to both and not more likely with carvedilol specifically in comparison to propranolol.
*Hyperkalemia*
- Neither carvedilol nor propranolol is directly associated with causing **hyperkalemia** as a primary adverse effect.
- Beta-blockers can sometimes lead to minor shifts in potassium, but it's not a common or more significant side effect compared to others listed.
*Hyperglycemia*
- **Non-selective beta-blockers** like propranolol can impair the recovery from **hypoglycemia** and mask its symptoms.
- While beta-blockers can have some metabolic effects, **hyperglycemia** is not a generally recognized or more prominent adverse effect of carvedilol compared to propranolol.
Alpha-adrenergic antagonists US Medical PG Question 5: A 78-year-old man suffers a fall in a nursing home and is brought to the emergency room. A right hip fracture is diagnosed, and he is treated with a closed reduction with internal fixation under spinal anesthesia. On the second postoperative day, the patient complains of pain in the lower abdomen and states that he has not urinated since the surgery. An ultrasound shows increased bladder size and volume. Which of the following is the mechanism of action of the drug which is most commonly used to treat this patient’s condition?
- A. Alpha-blocker
- B. Parasympathetic antagonist
- C. Sympathetic agonist
- D. Beta-blocker
- E. Parasympathetic agonist (Correct Answer)
Alpha-adrenergic antagonists Explanation: ***Parasympathetic agonist***
- The patient presents with **postoperative urinary retention (POUR)**, commonly treated with **bethanechol**, a muscarinic cholinergic agonist.
- Bethanechol acts as a **parasympathetic agonist**, stimulating **muscarinic receptors** on the **detrusor muscle** of the bladder, causing it to contract and facilitating urination.
*Alpha-blocker*
- **Alpha-blockers** (e.g., tamsulosin) relax the **smooth muscle** of the prostatic urethra and bladder neck, often used for **benign prostatic hyperplasia (BPH)**.
- While they can improve urinary flow, they do not directly stimulate **detrusor contraction** and are not the primary treatment for acute POUR.
*Parasympathetic antagonist*
- **Parasympathetic antagonists** (e.g., oxybutynin) block muscarinic receptors, leading to **detrusor relaxation**.
- These drugs are used to treat conditions like **overactive bladder** or **urge incontinence**, which involve excessive bladder contraction, and would worsen urinary retention.
*Sympathetic agonist*
- **Sympathetic agonists** (e.g., norepinephrine) primarily cause vasoconstriction and cardiac stimulation.
- They tend to **relax the detrusor muscle** and contract the internal urethral sphincter via **beta-3 and alpha-1 receptors**, respectively, which would exacerbate urinary retention.
*Beta-blocker*
- **Beta-blockers** (e.g., propranolol) primarily affect the heart and blood vessels, slowing heart rate and lowering blood pressure.
- They have **no direct primary role** in the treatment of acute urinary retention as they do not directly act on bladder contractility.
Alpha-adrenergic antagonists US Medical PG Question 6: A 72-year-old male presents to his primary care physician complaining of increased urinary frequency and a weakened urinary stream. He has a history of gout, obesity, diabetes mellitus, and hyperlipidemia. He currently takes allopurinol, metformin, glyburide, and rosuvastatin. His temperature is 98.6°F (37°C), blood pressure is 130/85 mmHg, pulse is 90/min, and respirations are 18/min. Physical examination reveals an enlarged, non-tender prostate without nodules or masses. An ultrasound reveals a uniformly enlarged prostate that is 40mL in size. His physician starts him on a new medication. After taking the first dose, the patient experiences lightheadedness upon standing and has a syncopal event. Which of the following mechanisms of action is most consistent with the medication in question?
- A. Dihydropyridine calcium channel blocker
- B. Selective muscarinic agonist
- C. Alpha-2-adrenergic receptor agonist
- D. Alpha-1-adrenergic receptor antagonist (Correct Answer)
- E. Non-selective alpha receptor antagonist
Alpha-adrenergic antagonists Explanation: ***Alpha-1-adrenergic receptor antagonist***
- The patient's symptoms of **increased urinary frequency** and **weakened urinary stream** are consistent with **benign prostatic hyperplasia (BPH)**. The physical exam and ultrasound findings of an **enlarged, non-tender prostate** confirm this.
- The medication caused **lightheadedness upon standing** and a **syncopal event** after the first dose, which is indicative of **first-dose orthostatic hypotension**. This adverse effect is characteristic of **alpha-1-adrenergic receptor antagonists**, which relax smooth muscles in the prostate and bladder neck but can also cause vasodilation.
*Dihydropyridine calcium channel blocker*
- These drugs primarily relax **vascular smooth muscle**, leading to vasodilation and can cause **hypotension**, but **orthostatic hypotension** and syncope as a "first-dose effect" are less common compared to alpha-1 blockers.
- They are used to treat **hypertension** and **angina**, not directly for BPH symptoms.
*Selective muscarinic agonist*
- **Muscarinic agonists** (e.g., bethanechol) would **increase bladder contraction** and could worsen urinary outflow obstruction in BPH, not improve it.
- Their primary side effects include **diarrhea**, **nausea**, and **bradycardia**, not orthostatic hypotension and syncope.
*Alpha-2-adrenergic receptor agonist*
- **Alpha-2 agonists** (e.g., clonidine) typically **lower blood pressure** by reducing sympathetic outflow from the central nervous system, but they primarily cause **sedation** and **dry mouth**, and are not used for BPH.
- While they can cause hypotension, the specific presentation of first-dose syncope in the context of BPH treatment points away from this class.
*Non-selective alpha receptor antagonist*
- Although non-selective alpha antagonists can also cause **orthostatic hypotension** due to vasodilation, **selective alpha-1 antagonists** are the preferred choice for BPH due to their more targeted action on the prostate and bladder neck, and the question describes a direct therapy for BPH.
- Alpha-2 blockade is less relevant to BPH and can cause additional side effects.
Alpha-adrenergic antagonists US Medical PG Question 7: A 72-year-old man of Asian descent seeks evaluation at your medical office and is frustrated about the frequency he wakes up at night to urinate. He comments that he has stopped drinking liquids at night, but the symptoms have progressively worsened. The physical examination is unremarkable, except for an enlarged, symmetric prostate free of nodules. Which of the following should you prescribe based on the main factor that contributes to the underlying pathogenesis?
- A. Prazosin
- B. Tamsulosin
- C. Leuprolide
- D. Phenylephrine
- E. Finasteride (Correct Answer)
Alpha-adrenergic antagonists Explanation: ***Finasteride***
- This medication is a **5-alpha reductase inhibitor** that reduces the size of the prostate by decreasing the conversion of testosterone to **dihydrotestosterone (DHT)**, the primary androgen responsible for prostate growth.
- Given the patient's enlarged prostate and symptoms of **nocturia** that have progressively worsened despite behavioral changes, addressing the underlying stromal and epithelial proliferation of **benign prostatic hyperplasia (BPH)** is key.
*Prazosin*
- **Prazosin** is an **alpha-1 adrenergic antagonist** that works by relaxing the smooth muscle in the prostate and bladder neck, which can improve urine flow but does not address the underlying prostatic hypertrophy.
- While it can alleviate symptoms of BPH, it does not treat the **main pathogenic factor** (prostate enlargement due to DHT) that contributes to the worsening condition.
*Tamsulosin*
- **Tamsulosin** is a selective **alpha-1A adrenergic blocker** that primarily relaxes smooth muscle in the prostate and bladder neck, improving urinary flow with fewer cardiovascular side effects compared to non-selective alpha blockers.
- Like prazosin, it helps with symptom relief but does not target the **hormone-driven growth** of the prostate, which is the underlying cause of the worsening condition.
*Leuprolide*
- **Leuprolide** is a **GnRH agonist** mainly used in advanced prostate cancer or endometriosis; it suppresses gonadotropin release and, consequently, testosterone production.
- It is not indicated for the management of **benign prostatic hyperplasia (BPH)**, which is the more likely diagnosis given the patient's presentation and symmetrical, non-nodular prostate.
*Phenylephrine*
- **Phenylephrine** is an **alpha-1 adrenergic agonist** that causes vasoconstriction and can contract the smooth muscle of the bladder neck, leading to increased outflow resistance.
- This would **worsen rather than improve** the patient's symptoms of urinary obstruction and is contraindicated in BPH.
Alpha-adrenergic antagonists US Medical PG Question 8: Match the following:
Column A:
a. Beta 1
b. Beta 2
c. Beta 3
Column B:
1. Mirabegron
2. Betaxolol
3. Salbutamol
- A. a-2, b-3 ,c-1 (Correct Answer)
- B. a-2, b-1, c-3
- C. a-3, b-2, c-1
- D. a-3, b-1, c-2
Alpha-adrenergic antagonists Explanation: ***a-2, b-3, c-1***
- This pairing correctly matches **Betaxolol** with **Beta 1 selective** antagonism, **Salbutamol** with **Beta 2 selective** agonism, and **Mirabegron** with **Beta 3 selective** agonism.
- **Betaxolol** is a beta-1 selective adrenergic receptor antagonist, primarily used in ophthalmology to reduce intraocular pressure and as an antihypertensive. **Salbutamol** is a selective beta-2 adrenergic agonist used as a bronchodilator in asthma and COPD, causing relaxation of bronchial smooth muscle. **Mirabegron** is a selective beta-3 adrenergic agonist used to treat overactive bladder by relaxing the detrusor muscle.
*a-2, b-1, c-3*
- This option incorrectly assigns **Mirabegron** to Beta 2. Mirabegron is a **Beta 3 selective agonist**.
- It also incorrectly assigns **Salbutamol** to Beta 3. Salbutamol is a **Beta 2 selective agonist**.
*a-3, b-2, c-1*
- This option incorrectly assigns **Salbutamol** to Beta 1. Salbutamol is a **Beta 2 selective agonist**.
- It also incorrectly assigns **Betaxolol** to Beta 2. Betaxolol is a **Beta 1 selective antagonist**.
*a-3, b-1, c-2*
- This option incorrectly assigns **Salbutamol** to Beta 1 and **Betaxolol** to Beta 3.
- **Salbutamol** is a Beta 2 selective agonist, and **Betaxolol** is a Beta 1 selective antagonist.
Alpha-adrenergic antagonists US Medical PG Question 9: A 29-year-old man is outside his home doing yard work when a bee stings him in the right arm. Within 10 minutes, he reports breathlessness and multiple, circular, pruritic rashes over his right arm. He drives to his family physician’s office for evaluation. His past medical history is significant for hypertension and he takes lisinopril. Known allergies include latex, Hymenoptera, and aspirin. His blood pressure is 118/68 mm Hg; heart rate is 104/min and regular; respiratory rate is 22/min; temperature is 37.7°C (99.8°F). There is non-pitting edema but erythema with raised wheels are present in the region of the right arm. Auscultation of the lungs reveals mild wheezing at the lung bases. Which of the following is the best course of action in the management of this patient?
- A. Go to the emergency department
- B. Methylprednisolone and go to the emergency department
- C. Diphenhydramine and go to the emergency department
- D. Epinephrine and go to the emergency department (Correct Answer)
- E. Albuterol and go to the emergency department
Alpha-adrenergic antagonists Explanation: ***Epinephrine and go to the emergency department***
- This patient is experiencing **anaphylaxis**, indicated by breathlessness, generalized urticaria, and a known bee sting allergy, which requires immediate treatment with **epinephrine**.
- **Epinephrine** is the first-line and most critical treatment for anaphylaxis as it reverses bronchoconstriction, stabilizes mast cells, and increases blood pressure. After administering epinephrine, prompt transfer to the **emergency department** is essential for monitoring and further management.
*Go to the emergency department*
- While going to the emergency department is necessary, it is not sufficient as the **initial and most critical treatment (epinephrine)** is missing.
- Delaying the administration of epinephrine for anaphylaxis can lead to rapid deterioration and life-threatening complications.
*Methylprednisolone and go to the emergency department*
- **Methylprednisolone (corticosteroids)** can help prevent biphasic anaphylaxis and reduce inflammation but are **not a first-line treatment for acute anaphylaxis** and do not provide immediate relief from bronchospasm or hypotension.
- The immediate priority is addressing the acute symptoms with epinephrine, followed by transport to the emergency department, where corticosteroids may be administered.
*Diphenhydramine and go to the emergency department*
- **Diphenhydramine (an antihistamine)** can help alleviate mild cutaneous symptoms like pruritus and urticaria, but it **does not treat the life-threatening respiratory or cardiovascular symptoms** of anaphylaxis.
- It should not be used as the sole or primary treatment for anaphylaxis, especially in the presence of breathlessness.
*Albuterol and go to the emergency department*
- **Albuterol (a bronchodilator)** can help relieve bronchospasm and breathlessness, but it **does not address other critical aspects of anaphylaxis** such as vasodilation or mast cell stabilization.
- While useful as an adjunct, it is not a substitute for epinephrine in the management of systemic anaphylaxis.
Alpha-adrenergic antagonists US Medical PG Question 10: A 65-year-old woman is transferred to the intensive care unit after she underwent coronary stenting for a posterior-inferior STEMI. She is known to have allergies to amiodarone and captopril. A few hours after the transfer, she suddenly loses consciousness. The monitor shows ventricular fibrillation. CPR is initiated. After 3 consecutive shocks with a defibrillator, the monitor shows ventricular fibrillation. Which of the following medications should be administered next?
- A. Adrenaline and lidocaine (Correct Answer)
- B. Lidocaine and sotalol
- C. Adrenaline and verapamil
- D. Adrenaline and amiodarone
- E. Amiodarone and lidocaine
Alpha-adrenergic antagonists Explanation: ***Adrenaline and lidocaine***
- **Adrenaline (epinephrine)** is the standard vasopressor in ACLS for cardiac arrest, given at 1 mg IV/IO every 3-5 minutes to increase coronary and cerebral perfusion pressures, improving the chances of return of spontaneous circulation (ROSC).
- **Lidocaine** is the recommended alternative antiarrhythmic for refractory ventricular fibrillation when **amiodarone is contraindicated** (as in this patient with documented amiodarone allergy).
- Per **ACLS guidelines**, after failed defibrillation attempts, continue CPR, administer epinephrine, and give an antiarrhythmic agent (lidocaine 1-1.5 mg/kg when amiodarone cannot be used).
*Lidocaine and sotalol*
- **Lidocaine** is appropriate as an antiarrhythmic in refractory VF when amiodarone is contraindicated.
- However, this option omits **epinephrine (adrenaline)**, which is a critical vasopressor required during cardiac arrest per ACLS protocols.
- **Sotalol** is a beta-blocker with Class III antiarrhythmic properties, but it is not recommended for acute management of refractory VF in cardiac arrest.
*Adrenaline and verapamil*
- **Adrenaline** is indicated as the vasopressor for cardiac arrest.
- **Verapamil** is a calcium channel blocker used for supraventricular arrhythmias; it is **contraindicated in ventricular fibrillation** due to negative inotropic effects and peripheral vasodilation that can worsen hemodynamic collapse during cardiac arrest.
*Adrenaline and amiodarone*
- While **adrenaline** is indicated and **amiodarone** would typically be the preferred antiarrhythmic for refractory VF, this patient has a **documented allergy to amiodarone**, making it contraindicated.
- Lidocaine must be used as the alternative antiarrhythmic agent.
*Amiodarone and lidocaine*
- **Lidocaine** is appropriate in this scenario.
- However, **amiodarone is contraindicated** due to the patient's known allergy.
- This combination would be dangerous and violates basic principles of avoiding known allergens.
More Alpha-adrenergic antagonists US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.