Acetylcholine receptors and function US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Acetylcholine receptors and function. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Acetylcholine receptors and function US Medical PG Question 1: Which receptor type mediates the slow phase of synaptic transmission in autonomic ganglia?
- A. Muscarinic (M3)
- B. Muscarinic (M2)
- C. Muscarinic (M1) (Correct Answer)
- D. Nicotinic (N2)
Acetylcholine receptors and function Explanation: ***Muscarinic (M1)***
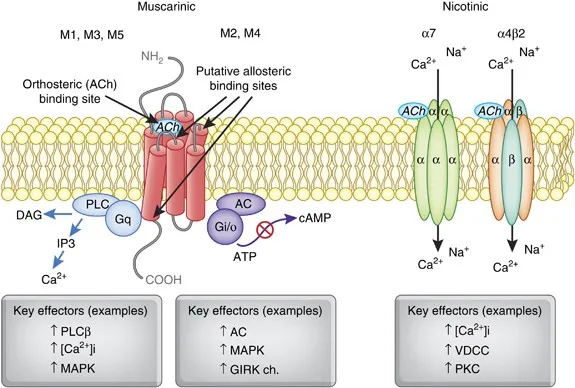
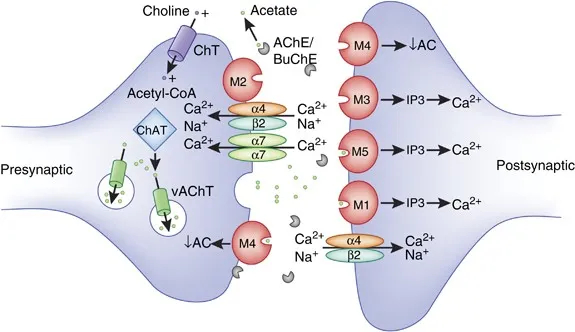
- **M1 receptors** are **Gq-protein coupled receptors** that activate phospholipase C, leading to increased intracellular calcium and diacylglycerol, which mediates the slow excitatory postsynaptic potential in autonomic ganglia.
- This activation results in a **slow depolarization** that prolongs the excitability of ganglionic neurons after the initial fast synaptic transmission.
*Muscarinic (M3)*
- **M3 receptors** are primarily found on **smooth muscle**, glands, and endothelium, mediating contraction, secretion, and vasodilation, respectively.
- While also **Gq-protein coupled**, their role in autonomic ganglia is not the main mediator of the slow phase of synaptic transmission.
*Muscarinic (M2)*
- **M2 receptors** are **Gi-protein coupled receptors** mainly found in the heart, mediating decreased heart rate and contractility.
- In autonomic ganglia, M2 receptors could have a modulatory role, but they are not responsible for the slow excitatory phase of synaptic transmission.
*Nicotinic (N2)*
- **Nicotinic N2 receptors** (also known as **NN or neuronal nicotinic receptors**) mediate the **fast excitatory postsynaptic potential** (EPSP) in autonomic ganglia by opening ion channels.
- This leads to rapid depolarization and action potential generation, which is distinct from the **slower, prolonged phase** of transmission.
Acetylcholine receptors and function US Medical PG Question 2: A 32-year-old farmer is brought to the emergency department by his wife. The patient was reportedly anxious, sweaty, and complaining of a headache and chest tightness before losing consciousness on route to the hospital. Which of the following is mechanistically responsible for this patient's symptoms?
- A. Reversible inhibition of acetylcholinesterase
- B. Competitive inhibition of acetylcholine at post-junctional effector sites
- C. Binding of acetylcholine agonists to post-junctional receptors
- D. Irreversible inhibition of acetylcholinesterase (Correct Answer)
- E. Inhibition of presynaptic exocytosis of acetylcholine vesicles
Acetylcholine receptors and function Explanation: ***Irreversible inhibition of acetylcholinesterase***
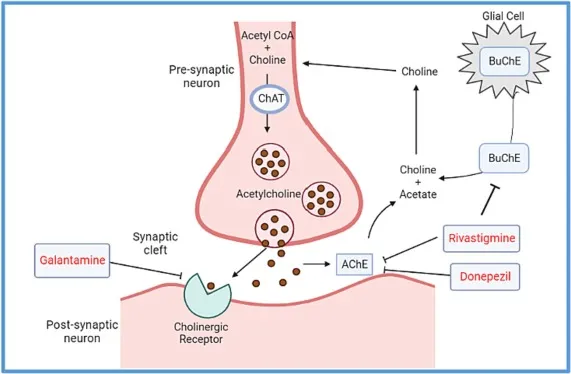
- The farmer's symptoms (anxiety, sweating, headache, chest tightness, loss of consciousness) are characteristic of **organophosphate poisoning**, which causes a cholinergic crisis due to accumulation of acetylcholine.
- Organophosphates are common in **pesticides** and act by irreversibly inhibiting **acetylcholinesterase**, leading to prolonged stimulation of cholinergic receptors.
*Reversible inhibition of acetylcholinesterase*
- Reversible acetylcholinesterase inhibitors, such as **physostigmine** or **neostigmine**, typically have a shorter duration of action and might cause similar symptoms but are less likely to lead to such severe, acute presentations in an accidental exposure scenario for a farmer.
- These agents are often used therapeutically and would not typically cause prolonged loss of consciousness in this context unless in very high intentional doses.
*Competitive inhibition of acetylcholine at post-junctional effector sites*
- This mechanism describes the action of **anticholinergic drugs** (e.g., atropine), which would block acetylcholine's effects and cause symptoms like dry mouth, dilated pupils, and tachycardia, opposite to what is observed here.
- Such agents would alleviate, not cause, the cholinergic symptoms seen in this patient.
*Binding of acetylcholine agonists to post-junctional receptors*
- While direct agonists (e.g., pilocarpine, methacholine) would mimic acetylcholine and cause cholinergic symptoms, organophosphate poisoning operates by preventing acetylcholine breakdown, rather than directly binding as an exogenous agonist.
- The context of a farmer and sudden, severe symptoms points more strongly to pesticide exposure and acetylcholinesterase inhibition.
*Inhibition of presynaptic exocytosis of acetylcholine vesicles*
- This mechanism is characteristic of **botulinum toxin**, which blocks the release of acetylcholine from presynaptic terminals, leading to muscle paralysis and weakness.
- The patient's symptoms are those of cholinergic excess, not cholinergic blockade or deficiency at the neuromuscular junction.
Acetylcholine receptors and function US Medical PG Question 3: A scientist is trying to design a drug to modulate cellular metabolism in the treatment of obesity. Specifically, he is interested in understanding how fats are processed in adipocytes in response to different energy states. His target is a protein within these cells that catalyzes catabolism of an energy source. The products of this reaction are subsequently used in gluconeogenesis or β-oxidation. Which of the following is true of the most likely protein that is being studied by this scientist?
- A. It is stimulated by epinephrine (Correct Answer)
- B. It is inhibited by glucagon
- C. It is inhibited by acetylcholine
- D. It is inhibited by cortisol
- E. It is stimulated by insulin
Acetylcholine receptors and function Explanation: ***It is stimulated by epinephrine***
- The protein described is likely **hormone-sensitive lipase (HSL)**, which catabolizes **triglycerides** in adipocytes to **glycerol** and **fatty acids**.
- **Epinephrine** (and norepinephrine) stimulates HSL activity via a **cAMP-dependent protein kinase A (PKA)** pathway, leading to increased fatty acid release for energy.
*It is inhibited by glucagon*
- **Glucagon primarily acts on the liver** to promote gluconeogenesis and glycogenolysis, but it does **not directly inhibit HSL** in adipocytes.
- While glucagon has a lipolytic effect, it doesn't inhibit the enzyme that releases fatty acids.
*It is inhibited by acetylcholine*
- **Acetylcholine** is a neurotransmitter involved in the **parasympathetic nervous system**, which generally promotes energy storage.
- It does **not directly inhibit HSL**; its effects on lipid metabolism are indirect and typically involve other pathways.
*It is inhibited by cortisol*
- **Cortisol**, a glucocorticoid, generally **promotes lipolysis** (breakdown of fats) in certain contexts, particularly during stress to provide energy substrates.
- Therefore, it would **not inhibit HSL**; rather, it often enhances its activity or provides a permissive effect for other lipolytic hormones.
*It is stimulated by insulin*
- **Insulin** is an **anabolic hormone** that promotes energy storage, including **lipogenesis** (fat synthesis) and inhibits lipolysis.
- Insulin **inhibits HSL activity** by activating phosphodiesterase, which reduces cAMP levels, thus deactivating PKA and preventing HSL phosphorylation.
Acetylcholine receptors and function US Medical PG Question 4: A drug research team has synthesized a novel oral drug that acts as an agonist at multiple adrenergic receptors. When administered in animals, it has been shown to produce urinary retention at therapeutic doses with the absence of other manifestations of adrenergic stimulation. The researchers are interested in understanding signal transduction and molecular mechanisms behind the action of the novel drug. Which of the following receptors would most likely transduce signals across the plasma membrane following the administration of this novel drug?
- A. GoPCRs (Go protein-coupled receptors)
- B. GsPCRs (Gs protein-coupled receptors)
- C. GqPCRs (Gq protein-coupled receptors) (Correct Answer)
- D. GtPCRs (Gt protein-coupled receptors)
- E. GiPCRs (Gi protein-coupled receptors)
Acetylcholine receptors and function Explanation: ***GqPCRs (Gq protein-coupled receptors)***
- **Urinary retention** is primarily mediated by the activation of **alpha-1 adrenergic receptors** in the bladder neck and prostate, which are classically Gq-protein coupled receptors.
- Activation of **GqPCRs** leads to the activation of **phospholipase C**, increased **IP3 (inositol trisphosphate)** and **DAG (diacylglycerol)**, and subsequently, a rise in intracellular **calcium**, causing smooth muscle contraction.
*GoPCRs (Go protein-coupled receptors)*
- While Go proteins are a subtype of Gi/Go family, their direct primary role in mediating **urinary retention** via **adrenergic agonism** is not as well-established as Gq.
- Go signaling often involves modulation of **ion channels** and can be involved in neuronal signaling, not directly causing smooth muscle contraction in the bladder.
*GsPCRs (Gs protein-coupled receptors)*
- **GsPCRs** (e.g., beta-adrenergic receptors) activate **adenylate cyclase**, leading to increased **cAMP** levels, which typically causes smooth muscle relaxation.
- This effect would promote **urinary relaxation** and flow, not retention, and hence is contrary to the observed drug effect.
*GtPCRs (Gt protein-coupled receptors)*
- **GtPCRs** (transducin) are primarily involved in the **phototransduction** cascade in the retina, mediating vision.
- They have no known central role in mediating adrenergic effects on the **urinary tract smooth muscle**.
*GiPCRs (Gi protein-coupled receptors)*
- **GiPCRs** (e.g., alpha-2 adrenergic receptors) inhibit **adenylate cyclase**, leading to decreased **cAMP** levels, which generally causes smooth muscle contraction in some tissues, but also presynaptic inhibition.
- While Gi activation can lead to contraction in some contexts, the primary mechanism of **urinary retention** via bladder neck contraction is through alpha-1 receptors linked to Gq.
Acetylcholine receptors and function US Medical PG Question 5: A 45-year-old unconscious man is brought to the emergency department by a friend who witnessed him collapse. They were working in a greenhouse spraying the vegetables when the man started to complain of blurred vision and nausea. On the way to the hospital, the man lost consciousness and lost bladder continence. The patient’s vital signs are as follows: blood pressure 95/60 mm Hg; heart rate 59/min; respiratory rate 22/min; and temperature 36.0℃ (96.8℉). On examination, he is unconscious with a GCS score of 7. His pupils are contracted and react poorly to light. Lung auscultation reveals diffuse wheezing. Cardiac auscultation is significant for bradycardia. Abdominal auscultation reveals increased bowel sounds. A cardiac monitor shows bradycardia with grade 2 AV-block. Which of the following leads to the cardiac manifestations seen in this patient?
- A. Activation of M1-cholinergic receptors
- B. Activation of β2-adrenergic receptors
- C. Activation of M2-cholinergic receptors (Correct Answer)
- D. Inhibition of β1-adrenergic receptors
- E. Inhibition of M2-cholinergic receptors
Acetylcholine receptors and function Explanation: ***Activation of M2-cholinergic receptors***
- The patient's symptoms (blurred vision, nausea, unconsciousness, incontinence, miosis, wheezing, bradycardia, increased bowel sounds) are classic for **organophosphate poisoning**, which involves excessive activation of the **parasympathetic nervous system**.
- **M2 receptors** are primarily located in the heart and, when activated by acetylcholine, lead to slowed heart rate (bradycardia) and decreased conduction (AV block), characteristic of the cardiac manifestations observed.
*Activation of M1-cholinergic receptors*
- **M1 receptors** are primarily found in neural tissue and glands, contributing to increased GI motility and glandular secretions but not directly to cardiac slowing.
- Their activation does not directly cause the observed **bradycardia** and **AV block**.
*Activation of β2-adrenergic receptors*
- **β2-adrenergic receptors** are part of the sympathetic nervous system and are present in the smooth muscle of the bronchioles and blood vessels.
- Their activation typically causes **bronchodilation** and **vasodilation**, which would counteract the patient's wheezing and hypotension, and are not involved in bradycardia.
*Inhibition of β1-adrenergic receptors*
- **β1-adrenergic receptors** are found in the heart and their inhibition would lead to bradycardia, but organophosphate poisoning causes **cholinergic excess**, not adrenergic inhibition.
- This mechanism would not explain the other widespread **parasympathetic activation** symptoms like miosis, wheezing, and increased GI motility.
*Inhibition of M2-cholinergic receptors*
- **Inhibition of M2-cholinergic receptors** would lead to an increase in heart rate and improved AV conduction, rather than the severe **bradycardia** and **AV block** observed.
- This mechanism is characteristic of **anticholinergic toxidrome**, which presents with opposing symptoms.
Acetylcholine receptors and function US Medical PG Question 6: A 72-year-old man with coronary artery disease comes to the physician because of intermittent episodes of substernal chest pain and shortness of breath. The episodes occur only when walking up stairs and resolves after resting for a few minutes. He is a delivery man and is concerned because the chest pain has impacted his ability to work. His pulse is 98/min and blood pressure is 132/77 mm Hg. Physical examination is unremarkable. An ECG shows no abnormalities. A drug that blocks which of the following receptors is most likely to prevent future episodes of chest pain from occurring?
- A. Angiotensin II receptors
- B. M2 muscarinic receptors
- C. Aldosterone receptors
- D. Beta-1 adrenergic receptors (Correct Answer)
- E. Alpha-2 adrenergic receptors
Acetylcholine receptors and function Explanation: ***Beta-1 adrenergic receptors***
- The patient's symptoms are classic for **stable angina**, triggered by exertion and relieved by rest, which indicates myocardial oxygen demand exceeding supply. Blocking **beta-1 adrenergic receptors** with a beta-blocker **reduces heart rate** and **contractility**, thereby decreasing myocardial oxygen consumption.
- Beta-blockers are a cornerstone in the treatment of stable angina to prevent future episodes of chest pain by **reducing cardiac workload**.
*Angiotensin II receptors*
- Blocking **Angiotensin II receptors** (e.g., with ARBs) is primarily used for **hypertension**, **heart failure**, and **renal protection**, not as a first-line treatment for acute angina prevention by reducing myocardial oxygen demand.
- While beneficial for overall cardiovascular risk reduction, ARBs do not directly lower heart rate or contractility to the same extent as beta-blockers for immediate angina symptom control.
*M2 muscarinic receptors*
- Blocking **M2 muscarinic receptors** would primarily **increase heart rate** and contractility by inhibiting parasympathetic tone, which would worsen, not prevent, angina by increasing myocardial oxygen demand.
- This is the opposite effect desired for angina management.
*Aldosterone receptors*
- Aldosterone receptor blockade (e.g., with spironolactone) is mainly used in **heart failure** and **hypertension** to reduce fluid retention and remodeling, but it does not directly impact myocardial oxygen demand or supply to prevent exertional angina.
- It does not have a direct anti-anginal effect on heart rate or contractility.
*Alpha-2 adrenergic receptors*
- Alpha-2 adrenergic receptor agonists (e.g., clonidine) are centrally acting sympatholytics that **decrease sympathetic outflow**, leading to vasodilation and reduced heart rate and blood pressure. However, they are not first-line agents for stable angina due to potential side effects and less direct impact on myocardial oxygen demand compared to beta-blockers.
- Their primary role is in **hypertension management**, and sudden discontinuation can lead to **rebound hypertension**.
Acetylcholine receptors and function US Medical PG Question 7: A 48-year-old man is unable to pass urine after undergoing open abdominal surgery. His physical examination and imaging findings suggest that the cause of his urinary retention is non-obstructive and is most probably due to urinary bladder atony. He is prescribed a new selective muscarinic (M3) receptor agonist, which improves his symptoms. Which of the following is most likely involved in the mechanism of action of this new drug?
- A. Activation of phospholipase C (Correct Answer)
- B. Inhibition of guanylyl cyclase
- C. Inhibition of adenylyl cyclase
- D. Increased transmembrane K+ conductance
- E. Increased transmembrane Na+ conductance
Acetylcholine receptors and function Explanation: ***Activation of phospholipase C***
- **M3 receptors** are Gq protein-coupled receptors, and their activation leads to the stimulation of **phospholipase C**.
- **Phospholipase C** hydrolyzes **phosphatidylinositol 4,5-bisphosphate (PIP2)** into **inositol trisphosphate (IP3)** and **diacylglycerol (DAG)**, which ultimately increases intracellular Ca2+ and causes smooth muscle contraction in the bladder.
*Inhibition of guanylyl cyclase*
- **Guanylyl cyclase** is typically modulated by other pathways, such as **nitric oxide (NO)**, leading to cGMP production and smooth muscle relaxation.
- Its inhibition would not be the primary mechanism for a muscarinic M3 agonist aiming to contract the bladder.
*Inhibition of adenylyl cyclase*
- **Adenylyl cyclase** is typically inhibited by Gi-coupled receptors (e.g., M2 receptors) leading to a decrease in cAMP and muscle relaxation, which is the opposite effect desired in bladder atony.
- M3 receptors, which are Gq-coupled, do not directly inhibit adenylyl cyclase.
*Increased transmembrane K+ conductance*
- **Increased K+ conductance** typically leads to hyperpolarization and relaxation of smooth muscle, which would worsen bladder atony rather than improve it.
- This mechanism is not associated with direct M3 receptor activation.
*Increased transmembrane Na+ conductance*
- While Na+ channels play a role in neuronal excitability, a direct effect on **transmembrane Na+ conductance** is not the primary mechanism of action for M3 receptor agonists in causing bladder smooth muscle contraction.
- Smooth muscle contraction primarily involves **calcium influx and release**.
Acetylcholine receptors and function US Medical PG Question 8: A 28-year-old female presents to her primary care doctor complaining of new onset blurry vision. She first noticed her vision getting blurry toward the end of the day several days ago. Since then, she reports that her vision has been fine when she wakes up but gets worse throughout the day. She has also noticed that her eyelids have started to droop before she goes to bed. On exam, she has bilateral ptosis that is worse on the right. Administering edrophonium to this patient leads to an immediate improvement in her symptoms. Which of the following is most likely true about this patient’s condition?
- A. It is caused by a type III hypersensitivity reaction
- B. It is associated with a neoplasm of lung neuroendocrine cells
- C. It is caused by antibodies directed against presynaptic P/Q calcium channels
- D. An increasing response will be seen on repeated nerve stimulation
- E. It is associated with a benign proliferation of epithelial cells of the thymus (Correct Answer)
Acetylcholine receptors and function Explanation: ***It is associated with a benign proliferation of epithelial cells of the thymus***
- The patient's symptoms of progressive weakness throughout the day, ptosis, and improvement with edrophonium (an acetylcholinesterase inhibitor) are highly suggestive of **myasthenia gravis**.
- Approximately 75% of patients with myasthenia gravis have **thymic abnormalities**, with about 65% having **thymic hyperplasia** (a benign proliferation of epithelial cells) and 10% having a **thymoma**.
*It is caused by a type III hypersensitivity reaction*
- **Type III hypersensitivity reactions** involve immune complex deposition, as seen in diseases like Systemic Lupus Erythematosus or post-streptococcal glomerulonephritis.
- Myasthenia gravis is a **Type II hypersensitivity reaction**, where antibodies directly target specific cell surface antigens, in this case, acetylcholine receptors at the neuromuscular junction.
*It is associated with a neoplasm of lung neuroendocrine cells*
- A neoplasm of **lung neuroendocrine cells**, specifically **small cell lung carcinoma**, is associated with **Lambert-Eaton Myasthenic Syndrome (LEMS)**.
- LEMS presents with proximal muscle weakness that *improves* with activity, unlike the fatiguable weakness seen in myasthenia gravis.
*It is caused by antibodies directed against presynaptic P/Q calcium channels*
- Antibodies directed against **presynaptic P/Q calcium channels** are characteristic of **Lambert-Eaton Myasthenic Syndrome (LEMS)**.
- In LEMS, these antibodies reduce the release of acetylcholine into the synaptic cleft, leading to muscle weakness.
*An increasing response will be seen on repeated nerve stimulation*
- An **increasing (incremental) response** on repeated nerve stimulation is a characteristic finding in **Lambert-Eaton Myasthenic Syndrome (LEMS)**.
- In myasthenia gravis, repeated nerve stimulation typically shows a **decreasing (decremental) response** due to the depletion of functionally available acetylcholine receptors.
Acetylcholine receptors and function US Medical PG Question 9: A researcher is studying receptors that respond to epinephrine in the body and discovers a particular subset that is expressed in presynaptic adrenergic nerve terminals. She discovers that upon activation, these receptors will lead to decreased sympathetic nervous system activity. She then studies the intracellular second messenger changes that occur when this receptor is activated. She records these changes and begins searching for analogous receptor pathways. Which of the following receptors would cause the most similar set of intracellular second messenger changes?
- A. Muscarinic cholinoreceptors in the gastrointestinal tract
- B. Growth hormone receptors in the musculoskeletal system
- C. Vasopressin receptors in the kidney
- D. Dopamine receptors in the brain (Correct Answer)
- E. Aldosterone receptors in the kidney
Acetylcholine receptors and function Explanation: ***Dopamine receptors in the brain***
- The described presynaptic receptors for epinephrine that decrease sympathetic activity are **alpha-2 adrenergic receptors**, which are **G inhibitory protein (Gi)-coupled receptors**.
- Gi-coupled receptors **inhibit adenylyl cyclase**, leading to a **decrease in intracellular cAMP**, a signaling pathway shared by **D2 dopamine receptors**.
*Muscarinic cholinoreceptors in the gastrointestinal tract*
- Most muscarinic receptors (M1 and M3) in the GI tract are **Gq-coupled**, leading to an **increase in phospholipase C (PLC) activity**, ultimately increasing intracellular **IP3 and DAG** and promoting smooth muscle contraction.
- This mechanism is distinct from the **Gi-mediated inhibition of cAMP** described for the presynaptic adrenergic receptor.
*Growth hormone receptors in the musculoskeletal system*
- Growth hormone receptors are **tyrosine kinase-associated receptors** (specifically, they are linked to **JAK/STAT pathways**), not G protein-coupled receptors.
- Their intracellular signaling involves **protein phosphorylation cascades**, which are fundamentally different from second messenger changes involving cAMP.
*Vasopressin receptors in the kidney*
- Vasopressin (ADH) acts on **V2 receptors** in the kidney, which are **G stimulatory protein (Gs)-coupled receptors**.
- Activation of V2 receptors leads to an **increase in adenylyl cyclase activity** and thus an **increase in intracellular cAMP**, the opposite effect of the described Gi-coupled receptor.
*Aldosterone receptors in the kidney*
- Aldosterone receptors are **intracellular steroid hormone receptors** that directly bind to DNA and regulate gene transcription.
- They do not engage in rapid intracellular second messenger changes like G protein-coupled receptors, but rather alter **protein synthesis** over hours to days.
Acetylcholine receptors and function US Medical PG Question 10: Which of the following statements is correct regarding the given graph?
- A. Drug 1 represents agonist and drug 2 represents inverse agonist
- B. Drug 3 represents agonist and drug 4 represents inverse agonist
- C. Drug 2 represents partial agonist and drug 3 represents inverse agonist
- D. Drug 1 represents agonist and drug 4 represents inverse agonist (Correct Answer)
Acetylcholine receptors and function Explanation: ***Drug 1 represents agonist and drug 4 represent inverse agonist***
- **Drug 1** demonstrates maximal efficacy, producing a **supraphysiologic response** above the baseline (100%), characteristic of an **agonist**.
- **Drug 4** produces a response **below the baseline** (100%), indicating inhibition of constitutive receptor activity, which is the definition of an **inverse agonist**.
*Drug 1 represents agonist and drug 2 represents inverse agonist*
- While **Drug 1** is correctly identified as an **agonist** due to its maximal effect above baseline, **Drug 2** is a **partial agonist**, as it produces a submaximal effect above baseline but does not reach the full agonist's efficacy.
- **Drug 2** does not reduce the baseline response, so it cannot be an inverse agonist.
*Drug 3 represents agonist and drug 4 represents inverse agonist*
- **Drug 3** maintains the **baseline response** (at 100%) regardless of concentration, indicating it is a **neutral antagonist** or has no effect, not an agonist.
- **Drug 4** is correctly identified as an **inverse agonist** because it reduces the baseline receptor activity.
*Drug 2 represents partial agonist and drug 3 represents inverse agonist*
- **Drug 2** is correctly identified as a **partial agonist** as it produces an effect above baseline but less than a full agonist.
- **Drug 3** is incorrect; it shows no change from baseline (100%), reflecting a **neutral antagonist** or inactive substance, not an inverse agonist which would decrease the baseline response.
More Acetylcholine receptors and function US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.