Pulmonary hypertension therapies US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pulmonary hypertension therapies. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pulmonary hypertension therapies US Medical PG Question 1: A 70-year-old male presents to his primary care provider complaining of decreased sexual function. He reports that over the past several years, he has noted a gradual decline in his ability to sustain an erection. He used to wake up with erections but no longer does. His past medical history is notable for diabetes, hyperlipidemia, and a prior myocardial infarction. He takes metformin, glyburide, aspirin, and atorvastatin. He drinks 2-3 drinks per week and has a 25 pack-year smoking history. He has been happily married for 40 years. He retired from his job as a construction worker 5 years ago and has been enjoying retirement with his wife. His physician recommends starting a medication that is also used in the treatment of pulmonary hypertension. Which of the following is a downstream effect of this medication?
- A. Increase cGMP degradation
- B. Increase cAMP production
- C. Increase PDE5 activity
- D. Decrease nitric oxide production
- E. Decrease cGMP degradation (Correct Answer)
Pulmonary hypertension therapies Explanation: ***Decrease cGMP degradation***
- The medication described is likely a **phosphodiesterase-5 (PDE5) inhibitor** (e.g., sildenafil, tadalafil), used for erectile dysfunction and pulmonary hypertension.
- These drugs work by inhibiting the enzyme PDE5, which is responsible for the breakdown of **cyclic GMP (cGMP)**, thereby increasing cGMP levels.
*Increase cGMP degradation*
- This is the **opposite** of the medication's intended effect, as it would lead to reduced cGMP levels and worsen erectile dysfunction.
- An increase in cGMP degradation would diminish the **vasodilatory** effects necessary for erection.
*Increase cAMP production*
- This medication primarily affects the **cGMP pathway**, not directly boosting cyclic AMP (cAMP) production.
- While cAMP also plays a role in vasodilation, it's regulated by different enzymes and pathways, such as **adenylyl cyclase**.
*Increase PDE5 activity*
- This would lead to a more **rapid breakdown of cGMP**, counteracting the goal of the medication and exacerbating erectile dysfunction.
- The medication's mechanism is specifically designed to **inhibit PDE5 activity**.
*Decrease nitric oxide production*
- **Nitric oxide (NO)** production is a **precursor** to cGMP synthesis, as NO activates guanylate cyclase to produce cGMP.
- Decreasing NO production would **reduce cGMP levels**, which is contrary to the action of PDE5 inhibitors.
Pulmonary hypertension therapies US Medical PG Question 2: A 30-year-old woman presents complaining of shortness of breath, chest pain, and fatigue. The patient complains of dyspnea upon exertion, generalized fatigue, lethargy, and chest pain associated with strenuous activities. Her history is notable for an atrial septal defect at birth. Her temperature is 99.5°F (37.5°C), blood pressure is 147/98 mmHg, pulse is 90/min, respirations are 17/min, and oxygen saturation is 98% on room air. On exam, she has a wide, fixed splitting of S2. Which of the following medications most directly treats the underlying pathophysiology causing this patient's presentation?
- A. Epoprostenol
- B. Metoprolol
- C. Lisinopril
- D. Nifedipine
- E. Bosentan (Correct Answer)
Pulmonary hypertension therapies Explanation: ***Bosentan***
- Bosentan is an **endothelin receptor antagonist** that **vasodilates** the pulmonary vasculature, reducing **pulmonary hypertension**. This directly addresses the increased pulmonary artery pressures and subsequent right heart strain caused by long-standing left-to-right shunting from the **atrial septal defect (ASD)**.
- The patient's symptoms (dyspnea, chest pain, fatigue) and signs (elevated pulmonary artery pressure evidenced by a wide, fixed splitting of S2 and systemic hypertension) are consistent with **pulmonary arterial hypertension (PAH)**, likely due to an uncorrected or late-presentation ASD leading to Eisenmenger syndrome.
*Epoprostenol*
- Epoprostenol is a **prostacyclin analog** that causes **vasodilation** and inhibits platelet aggregation, used in severe pulmonary hypertension. While it treats PAH, it is typically reserved for more advanced or rapidly progressive cases, often administered intravenously.
- While it improves symptoms and survival in PAH, **endothelin receptor antagonists** like bosentan are often preferred as first-line oral therapy due to their specific mechanism targeting endothelin's role in PAH pathophysiology and easier administration.
*Metoprolol*
- Metoprolol is a **beta-blocker** used to treat hypertension, angina, and arrhythmias by reducing heart rate and contractility. It would not directly treat PAH.
- In patients with right heart failure secondary to PAH, beta-blockers can sometimes be detrimental by reducing cardiac output, though their use in specific PAH subsets is being investigated.
*Lisinopril*
- Lisinopril is an **ACE inhibitor** that reduces blood pressure by blocking the renin-angiotensin-aldosterone system. It is primarily used for systemic hypertension and heart failure but does not specifically target pulmonary vascular remodeling or vasodilation.
- While it might help with systemic hypertension, it offers no direct benefit for the primary pathophysiology of pulmonary arterial hypertension.
*Nifedipine*
- Nifedipine is a **calcium channel blocker** that causes systemic and, to some extent, pulmonary vasodilation, used for hypertension and angina. However, its use in PAH is typically reserved for a small subset of patients who are **vasoreactive** during acute vasodilator testing.
- For the majority of PAH patients, and especially those with structural heart defects leading to PAH, other vasodilators like endothelin receptor antagonists or prostacyclins are more effective and safer.
Pulmonary hypertension therapies US Medical PG Question 3: A 57-year-old male presents with a primary complaint of erectile dysfunction. After proper evaluation, the patient is started on daily administration of sildenafil. This medication directly causes accumulation of which of the following intracellular mediators?
- A. Ca2+
- B. AMP
- C. cGMP (Correct Answer)
- D. NO
- E. ANP
Pulmonary hypertension therapies Explanation: ***cGMP***
- Sildenafil is a **phosphodiesterase-5 (PDE5) inhibitor** which prevents the degradation of **cyclic guanosine monophosphate (cGMP)**.
- Accumulation of cGMP leads to **smooth muscle relaxation** and increased blood flow, which is crucial for achieving an erection.
*Ca2+*
- **Calcium ions (Ca2+)** are essential for muscle contraction, and a decrease in intracellular Ca2+ generally promotes relaxation, which is the opposite effect desired for PDE5 inhibitors.
- Sildenafil's mechanism does not directly increase intracellular Ca2+; rather, it indirectly promotes relaxation by a cGMP-mediated pathway that reduces Ca2+ sensitivity or levels.
*AMP*
- **Adenosine monophosphate (AMP)** is a product of ATP hydrolysis and is involved in cellular energy metabolism, but it is not directly accumulated by sildenafil.
- The pathway targeted by sildenafil involves guanylate cyclase and phosphodiesterase, not directly affecting AMP levels in this context.
*NO*
- **Nitric oxide (NO)** is a crucial signaling molecule that activates guanylate cyclase, leading to cGMP production. Sildenafil does not directly cause accumulation of NO; instead, it potentiates the effects of NO by preventing cGMP degradation.
- NO is the upstream mediator that triggers the cGMP pathway, and its presence is necessary for sildenafil to be effective.
*ANP*
- **Atrial natriuretic peptide (ANP)** is a hormone primarily involved in blood pressure regulation and fluid balance, often leading to natriuresis and vasodilation.
- While ANP also acts through a cGMP pathway, sildenafil specifically targets PDE5, which primarily breaks down cGMP generated in response to NO, not ANP.
Pulmonary hypertension therapies US Medical PG Question 4: A 72-year-old man with type 2 diabetes mellitus, hypertension, and systolic heart failure comes to the physician because of a 5-day history of progressively worsening shortness of breath at rest. Physical examination shows jugular venous distention, diffuse crackles over the lower lung fields, and bilateral lower extremity edema. As a part of treatment, he is given a derivative of a hormone that acts by altering guanylate cyclase activity. This drug has been found to reduce pulmonary capillary wedge pressure and causes systemic hypotension as an adverse effect. The drug is most likely a derivative of which of the following hormones?
- A. Prostacyclin
- B. Aldosterone
- C. Somatostatin
- D. Brain natriuretic peptide (Correct Answer)
- E. Angiotensin II
Pulmonary hypertension therapies Explanation: ***Brain natriuretic peptide***
- **Brain natriuretic peptide (BNP)** derivatives, like nesiritide, activate **guanylate cyclase**, leading to increased cGMP, vasodilation, and reduced preload/afterload, alleviating heart failure symptoms.
- The patient's symptoms (shortness of breath, jugular venous distention, crackles, edema) are classic for **acute decompensated heart failure**, making a BNP derivative an appropriate treatment.
*Prostacyclin*
- **Prostacyclin** analogs (e.g., epoprostenol) are primarily used for **pulmonary hypertension** due to their potent vasodilatory effects in the pulmonary circulation.
- They activate **adenylyl cyclase** (increasing cAMP), not guanylate cyclase (which increases cGMP), representing a different mechanism of action.
*Aldosterone*
- **Aldosterone** is a mineralocorticoid that promotes **sodium and water retention** and potassium excretion, exacerbating heart failure symptoms.
- Its antagonists (e.g., spironolactone) are used in chronic heart failure but do not directly act via guanylate cyclase for acute symptom relief.
*Somatostatin*
- **Somatostatin** is a peptide hormone that **inhibits the secretion of various hormones**, including growth hormone, insulin, and glucagon.
- It is used in conditions like acromegaly or variceal bleeding and has no direct role in heart failure management via guanylate cyclase.
*Angiotensin II*
- **Angiotensin II** is a potent vasoconstrictor and a key component of the **renin-angiotensin-aldosterone system (RAAS)**, contributing to hypertension and heart failure progression.
- Drugs targeting angiotensin II (ACE inhibitors, ARBs) reduce its effects but do not act by directly altering guanylate cyclase activity; instead, they block its receptors or synthesis.
Pulmonary hypertension therapies US Medical PG Question 5: A 33-year-old woman comes to the physician because of a 6-month history of worsening shortness of breath and fatigue. Her paternal uncle had similar symptoms and died of respiratory failure at 45 years of age. The lungs are clear to auscultation. Pulmonary function testing shows an FVC of 84%, an FEV1/FVC ratio of 92%, and a normal diffusion capacity. An ECG shows a QRS axis greater than +90 degrees. Genetic analysis shows an inactivating mutation in the bone morphogenetic protein receptor type II (BMPR2) gene. Which of the following is the most likely cause of this patient's symptoms?
- A. Thickening of the interventricular septum
- B. Fibrosis of the pulmonary parenchyma
- C. Chronic intravascular hemolysis
- D. Elevated left atrial pressure
- E. Elevated pulmonary arterial pressure (Correct Answer)
Pulmonary hypertension therapies Explanation: ***Elevated pulmonary arterial pressure***
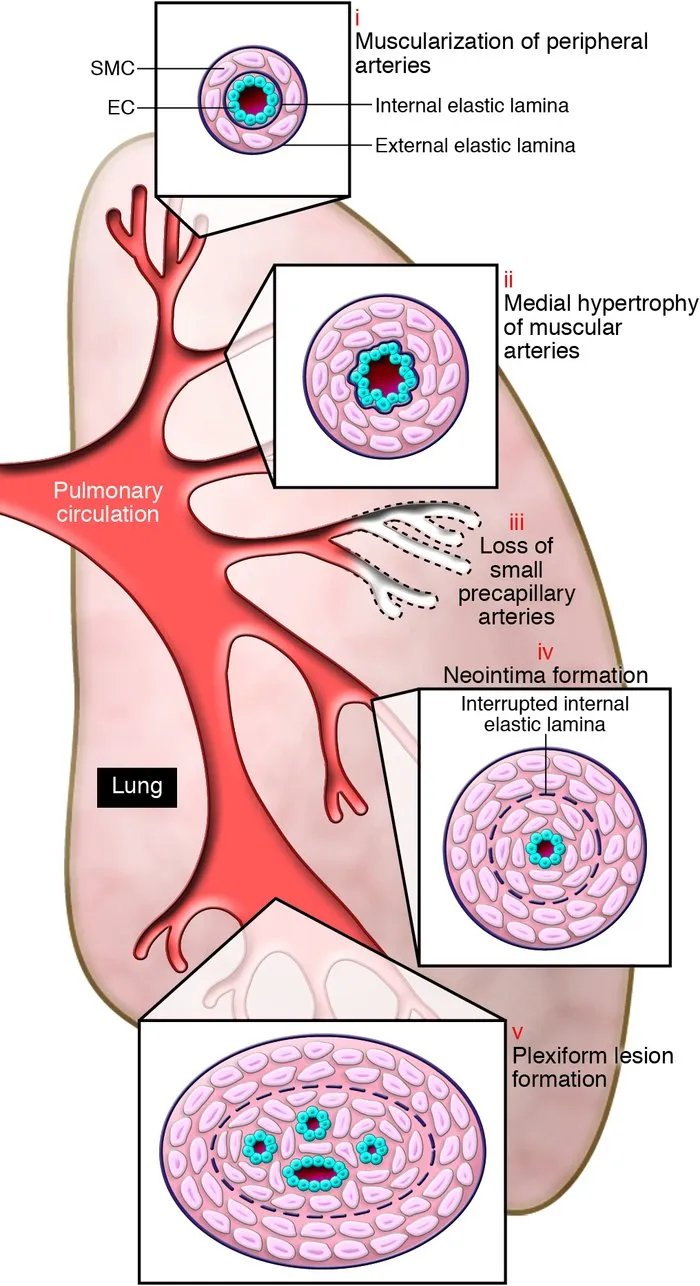
- The patient's symptoms (dyspnea, fatigue), family history of early respiratory failure, and the presence of an inactivating mutation in **BMPR2** are highly suggestive of **heritable pulmonary arterial hypertension (PAH)**.
- **PAH** is characterized by elevated pressures in the pulmonary arteries, leading to right ventricular strain, which is reflected by the **ECG finding of a QRS axis greater than +90 degrees** (right axis deviation).
- The **normal diffusion capacity** helps distinguish PAH from parenchymal lung diseases, and the **FEV1/FVC ratio of 92%** (elevated) with relatively preserved FVC is consistent with the restrictive physiology sometimes seen in PAH.
*Thickening of the interventricular septum*
- While septal thickening can occur in some cardiac conditions, it is not the primary cause of symptoms in the context of heritable PAH, nor is it directly indicated by the given pulmonary function tests or ECG.
- **Hypertrophic cardiomyopathy** can cause septal thickening, but it typically presents with different cardiac pathologies and is not associated with BMPR2 mutations.
*Fibrosis of the pulmonary parenchyma*
- This would cause a **restrictive lung disease** with a **reduced FVC** and **reduced diffusion capacity** due to impaired gas exchange across thickened alveolar-capillary membranes.
- The patient's **normal diffusion capacity** specifically rules out significant pulmonary fibrosis or other interstitial lung diseases.
*Chronic intravascular hemolysis*
- This condition would typically present with **anemia**, **jaundice**, **elevated LDH**, and possibly **splenomegaly**, none of which are mentioned.
- It is not associated with the BMPR2 genetic mutation or the specific PFT and ECG findings in this case.
*Elevated left atrial pressure*
- Elevated left atrial pressure (e.g., due to **left-sided heart failure** or mitral stenosis) can cause pulmonary congestion and dyspnea, but would typically lead to **pulmonary edema** with crackles on auscultation and **reduced diffusion capacity** due to fluid in the alveoli.
- The patient's clear lung auscultation and normal diffusion capacity make elevated left atrial pressure unlikely.
Pulmonary hypertension therapies US Medical PG Question 6: A 69-year-old woman comes to the clinic for an annual well exam. She reports no significant changes to her health except for an arm fracture 3 weeks ago while she was lifting some heavy bags. Her diabetes is well controlled with metformin. She reports some vaginal dryness that she manages with adequate lubrication. She denies any weight changes, fevers, chills, palpitations, nausea/vomiting, incontinence, or bowel changes. A dual-energy X-ray absorptiometry (DEXA) scan was done and demonstrated a T-score of -2.7. She was subsequently prescribed a selective estrogen receptor modulator, in addition to vitamin and weight-bearing exercises, for the management of her symptoms. What is the mechanism of action of the prescribed medication?
- A. Estrogen antagonist in cervix and agonist in bone
- B. Estrogen agonist in bone and breast
- C. Estrogen antagonist in breast and agonist in bone (Correct Answer)
- D. Partial estrogen agonist in endometrium and bone
- E. Partial estrogen agonist in bone and antagonist in cervix
Pulmonary hypertension therapies Explanation: ***Estrogen antagonist in breast and agonist in bone***
- Selective estrogen receptor modulators (SERMs) like **raloxifene** act as **estrogen agonists in bone**, helping to prevent osteoporosis by increasing bone mineral density.
- They also act as **estrogen antagonists in breast tissue**, which can reduce the risk of breast cancer in high-risk postmenopausal women.
- This is the mechanism of the medication prescribed for this patient's osteoporosis (T-score -2.7).
*Estrogen antagonist in cervix and agonist in bone*
- While SERMs are **agonists in bone**, they do not typically have significant antagonistic effects on the cervix, which is not a primary target for their therapeutic action or side effect profile.
- The primary antagonism is observed in breast tissue, not the cervix.
*Estrogen agonist in bone and breast*
- This describes the action of **estrogen replacement therapy (ERT)**, which increases breast cancer risk, whereas SERMs are designed to avoid this by being antagonists in breast tissue.
- The goal of SERMs is to achieve the beneficial bone effects of estrogen without the undesirable estrogenic effects on breast tissue.
*Partial estrogen agonist in endometrium and bone*
- Some SERMs, particularly **tamoxifen**, can act as a **partial estrogen agonist in the endometrium**, which can increase the risk of endometrial hyperplasia or cancer.
- However, raloxifene (a common SERM for osteoporosis) is typically **neutral or minimally agonistic** on the endometrium, and the primary description here is for its breast and bone effects.
*Partial estrogen agonist in bone and antagonist in cervix*
- SERMs are indeed **agonists in bone**, but their antagonistic action is primarily in the breast, not the cervix.
- The cervix is not a key target for either agonist or antagonist effects in the context of SERM therapeutic use for osteoporosis and breast cancer risk reduction.
Pulmonary hypertension therapies US Medical PG Question 7: A 45-year-old woman with history of systemic sclerosis presents with new onset dyspnea, which is worsened with moderate exertion. She also complains of chest pain. An ECG was obtained, and showed right-axis deviation. Chest x-ray showed right ventricle hypertrophy. Given the patient's history and presentation, right heart catheterization was performed, which confirmed the suspected diagnosis of pulmonary artery hypertension. It is decided to start the patient on bosentan. Which of the following describes the method of action of bosentan?
- A. Endothelin receptor antagonist (Correct Answer)
- B. Endothelin receptor agonist
- C. Anticoagulant
- D. Phosphodiesterase type 5 inhibitor
- E. Calcium channel blocker
Pulmonary hypertension therapies Explanation: ***Endothelin receptor antagonist***
- **Bosentan** is a **dual endothelin receptor antagonist** that blocks both ETA and ETB receptors.
- By blocking these receptors, bosentan prevents the **vasoconstrictive** and **proliferative effects of endothelin-1**, a potent vasoconstrictor implicated in pulmonary hypertension.
*Endothelin receptor agonist*
- An **endothelin receptor agonist** would activate endothelin receptors, leading to **increased vasoconstriction** and worsening pulmonary hypertension.
- This mechanism would **exacerbate** the patient's condition rather than alleviate it.
*Anticoagulant*
- **Anticoagulants** prevent **blood clot formation** and are used in some cases of pulmonary hypertension to reduce the risk of thrombosis.
- However, they do not directly address the primary **vasoconstriction** and **vascular remodeling** found in pulmonary artery hypertension.
*Phosphodiesterase type 5 inhibitor*
- **Phosphodiesterase type 5 (PDE5) inhibitors** like sildenafil and tadalafil increase cyclic GMP levels, leading to **vasodilation** in the pulmonary vasculature.
- While used in pulmonary hypertension, this is a **different mechanism of action** from bosentan.
*Calcium channel blocker*
- **Calcium channel blockers** are used in a small subset of pulmonary hypertension patients who are **vasoreactive** on acute vasodilator testing.
- They primarily act by reducing calcium influx into vascular smooth muscle cells, leading to **vasodilation**, which is not the mechanism of bosentan.
Pulmonary hypertension therapies US Medical PG Question 8: A 58-year-old man presents for a follow-up appointment. He recently was found to have a history of stage 2 chronic kidney disease secondary to benign prostatic hyperplasia leading to urinary tract obstruction. He has no other medical conditions. His father died at age 86 from a stroke, and his mother lives in an assisted living facility. He smokes a pack of cigarettes a day and occasionally drinks alcohol. His vital signs include: blood pressure 130/75 mm Hg, pulse 75/min, respiratory rate 17/min, and temperature 36.5°C (97.7°F). His physical examination is unremarkable. A 24-hour urine specimen reveals the following findings:
Specific gravity 1,050
pH 5.6
Nitrites (-)
Glucose (-)
Proteins 250 mg/24hrs
Which of the following should be prescribed to this patient to decrease his cardiovascular risk?
- A. Enalapril (Correct Answer)
- B. Ezetimibe
- C. Amlodipine
- D. Carvedilol
- E. Aspirin
Pulmonary hypertension therapies Explanation: ***Enalapril***
- **Enalapril**, an ACE inhibitor, is indicated for patients with **chronic kidney disease** and **proteinuria** to reduce cardiovascular risk and slow kidney disease progression.
- The patient has stage 2 CKD and **250 mg/24hrs of protein in urine**, which, when coupled with hypertension, makes ACE inhibitors the preferred choice to mitigate cardiovascular risk.
*Ezetimibe*
- **Ezetimibe** is a **cholesterol absorption inhibitor** used to lower LDL-C, but there is no information in the vignette to suggest hyperlipidemia.
- It is an inappropriate choice without evidence of dyslipidemia or a strong indication for lipid-lowering therapy.
*Amlodipine*
- **Amlodipine** is a **calcium channel blocker** used to treat hypertension but does not provide specific renal-protective benefits in patients with proteinuria.
- It would be a consideration for blood pressure control if an ACE inhibitor were contraindicated or insufficient.
*Carvedilol*
- **Carvedilol** is a **beta-blocker** used for hypertension, heart failure, and post-MI, but there is no indication for its use here.
- It is not the first-line agent for cardiovascular risk reduction in patients with chronic kidney disease and proteinuria without other specific cardiac indications.
*Aspirin*
- **Aspirin** is used for primary or secondary prevention of cardiovascular events due to its **antiplatelet effects**. However, in the absence of established cardiovascular disease, its use for primary prevention in CKD patients needs careful consideration of bleeding risk.
- While patients with CKD are at higher cardiovascular risk, an ACE inhibitor addresses both the hypertension and proteinuria, which directly contribute to cardiovascular and kidney disease progression in this patient.
Pulmonary hypertension therapies US Medical PG Question 9: A 72-year-old man presents to his primary care provider to discuss the frequency with which he wakes up at night to urinate. He avoids drinking liquids at night, but the symptoms have progressively worsened. The medical history is significant for hypertension and hyperlipidemia. He takes lisinopril, atorvastatin, and a multivitamin every day. Today, the vital signs include: blood pressure 120/80 mm Hg, heart rate 90/min, respiratory rate 17/min, and temperature 37.0°C (98.6°F). On physical examination, he appears tired. The heart has a regular rate and rhythm and the lungs are clear to auscultation bilaterally. A bedside bladder ultrasound reveals a full bladder. A digital rectal exam reveals an enlarged and symmetric prostate free of nodules, that is consistent with benign prostatic enlargement. He also has a history of symptomatic hypotension with several episodes of syncope in the past. The patient declines a prostate biopsy that would provide a definitive diagnosis and requests less invasive treatment. Which of the following is recommended to treat this patient’s enlarged prostate?
- A. Tadalafil
- B. Finasteride (Correct Answer)
- C. Tamsulosin
- D. Prazosin
- E. Leuprolide
Pulmonary hypertension therapies Explanation: ***Finasteride***
- This patient's symptoms of **nocturia** and an **enlarged, symmetric prostate** on DRE are classic for **benign prostatic hyperplasia (BPH)**. Finasteride is a **5-alpha reductase inhibitor** that reduces prostate volume by blocking the conversion of testosterone to dihydrotestosterone.
- Given the patient's history of **symptomatic hypotension** and preference for less invasive treatment, finasteride is a suitable choice as it has a lower risk of exacerbating hypotension compared to alpha-blockers.
*Tadalafil*
- While tadalafil is approved for BPH with erectile dysfunction, its primary mechanism involves **vasodilation**, which could worsen the patient's existing **symptomatic hypotension**.
- It does not directly reduce prostate size, which is a key component of long-term BPH management, especially in a patient with a significantly enlarged prostate.
*Tamsulosin*
- Tamsulosin is an **alpha-1 adrenergic blocker** that relaxes smooth muscle in the prostate and bladder neck, improving urine flow. However, it can cause **hypotension** and **syncope**, which would be contraindicated in this patient with a history of symptomatic hypotension.
- While effective for BPH symptoms, the risk of worsening his cardiovascular stability makes it a less favorable option given his medical history.
*Prazosin*
- Prazosin is another **alpha-1 adrenergic blocker** that can be used for BPH. However, it has a significant risk of **first-dose hypotension** and orthostatic hypotension, which would be highly problematic for this patient with a history of symptomatic hypotension and syncope.
- Due to its potent hypotensive effects, prazosin is generally not preferred for BPH, especially in older patients or those with cardiovascular instability.
*Leuprolide*
- Leuprolide is a **GnRH agonist** primarily used in the treatment of **prostate cancer** to reduce testosterone levels. It would effectively reduce prostate size but is an aggressive treatment with significant side effects (e.g., hot flashes, decreased libido, bone density loss) not typically used for benign prostatic hyperplasia.
- It is not indicated for the management of BPH and would be considered overtreatment for this patient's condition, especially given his desire for less aggressive management.
Pulmonary hypertension therapies US Medical PG Question 10: A 26-year-old man comes to the physician because of a 1-week history of left-sided chest pain. The pain is worse when he takes deep breaths. Over the past 6 weeks, he had been training daily for an upcoming hockey tournament. He does not smoke cigarettes or drink alcohol but has used cocaine once. His temperature is 37.1°C (98.7°F), pulse is 75/min, and blood pressure is 128/85 mm Hg. Physical examination shows tenderness to palpation of the left chest. An x-ray of the chest is shown. Which of the following is the most appropriate initial pharmacotherapy?
- A. Heparin
- B. Nitroglycerin
- C. Alteplase
- D. Naproxen (Correct Answer)
- E. Alprazolam
Pulmonary hypertension therapies Explanation: ***Naproxen***
- This patient presents with symptoms highly suggestive of **costochondritis** or a **musculoskeletal chest wall pain**. Key features include **tenderness to palpation of the chest wall**, pain made worse by **deep breaths** (pleuritic nature), and a history of strenuous activity (hockey training).
- An X-ray of the chest appears normal, ruling out other serious causes of chest pain like pneumothorax or significant infiltrates. Given the musculoskeletal nature of the pain, a **nonsteroidal anti-inflammatory drug (NSAID)** like naproxen is the most appropriate initial treatment to reduce pain and inflammation.
*Heparin*
- Heparin is an **anticoagulant** used to treat or prevent blood clots, such as in **pulmonary embolism** or deep vein thrombosis.
- While chest pain can be a symptom of pulmonary embolism, the physical exam finding of **localized tenderness to palpation** is not characteristic of a pulmonary embolism, and the normal chest X-ray makes it less likely.
*Nitroglycerin*
- Nitroglycerin is primarily used to treat **angina pectoris** (chest pain due to reduced blood flow to the heart) by causing vasodilation and reducing cardiac workload.
- The patient's age (26), absence of typical cardiac risk factors (except for prior cocaine use, which can cause vasospasm but is not suggested by the clinical picture or exam), and the **pleuritic nature of the pain** with **chest wall tenderness** make angina unlikely.
*Alteplase*
- Alteplase is a **thrombolytic agent** used to dissolve existing blood clots, typically in conditions like **acute myocardial infarction**, **pulmonary embolism**, or **ischemic stroke**.
- There is no clinical or radiological evidence (normal chest X-ray) to suggest a life-threatening thrombotic event requiring thrombolysis in this patient.
*Alprazolam*
- Alprazolam is a **benzodiazepine** used to treat **anxiety and panic disorders**.
- While anxiety can sometimes manifest as chest pain, the clear physical finding of **localized chest wall tenderness** points to a physical cause, and thus, an anxiolytic is not the most appropriate initial pharmacotherapy.
More Pulmonary hypertension therapies US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.