Phosphodiesterase inhibitors US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Phosphodiesterase inhibitors. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Phosphodiesterase inhibitors US Medical PG Question 1: A 66-year-old gentleman presents to a new primary care physician to establish care after a recent relocation. His past medical history is significant for gout, erectile dysfunction, osteoarthritis of bilateral knees, mitral stenosis, and diabetic peripheral neuropathy. He denies any past surgeries along with the use of any tobacco, alcohol, or illicit drugs. He has no known drug allergies and cannot remember the names of the medications he is taking for his medical problems. He states that he has recently been experiencing chest pain with strenuous activities. What part of the patient's medical history must be further probed before starting him on a nitrate for chest pain?
- A. Erectile dysfunction (Correct Answer)
- B. Diabetic peripheral neuropathy
- C. Gout
- D. Arthritis
- E. Mitral stenosis
Phosphodiesterase inhibitors Explanation: ***Erectile dysfunction***
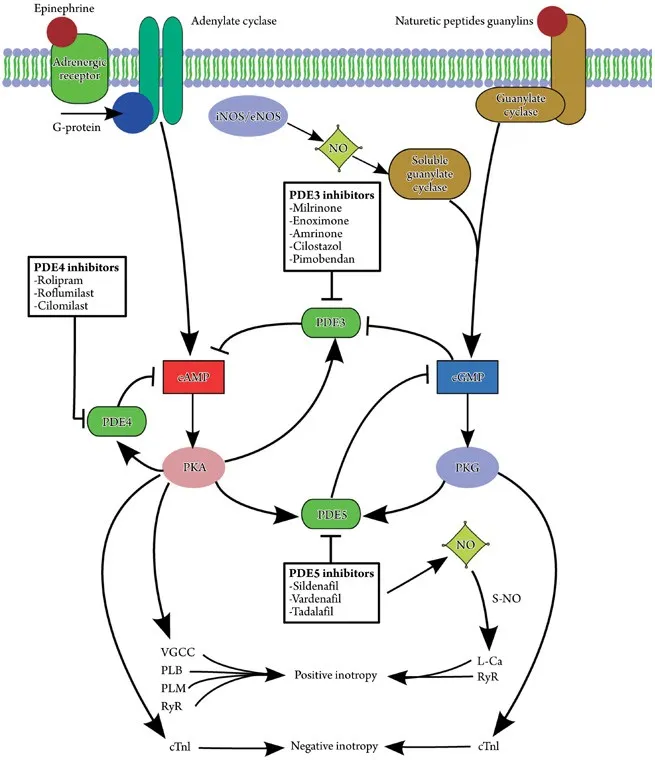
- Patients often take **phosphodiesterase-5 (PDE5) inhibitors** (e.g., sildenafil, tadalafil) for erectile dysfunction, which are absolutely contraindicated with nitrates.
- **Co-administration** can lead to a severe and potentially fatal drop in blood pressure due to enhanced vasodilation.
*Diabetic peripheral neuropathy*
- While important for overall health assessment, **diabetic peripheral neuropathy** does not directly contraindicate the use of nitrates for chest pain.
- It might influence medication choices if a patient has orthostatic hypotension, but not a direct contraindication.
*Gout*
- **Gout** is a joint condition and has no direct contraindication with nitrate use.
- Medications for gout, such as allopurinol or colchicine, do not interact adversely with nitrates.
*Arthritis*
- **Arthritis** (including osteoarthritis mentioned) is a musculoskeletal condition and does not contraindicate nitrate therapy.
- Pain management for arthritis does not typically involve drugs that interact dangerously with nitrates.
*Mitral stenosis*
- While **mitral stenosis** can affect cardiac function and hemodynamics, it is generally not an absolute contraindication to nitrate use.
- Nitrates can even be used cautiously in **mitral stenosis** to manage angina, though their use requires careful monitoring of preload.
Phosphodiesterase inhibitors US Medical PG Question 2: A 70-year-old male presents to his primary care provider complaining of decreased sexual function. He reports that over the past several years, he has noted a gradual decline in his ability to sustain an erection. He used to wake up with erections but no longer does. His past medical history is notable for diabetes, hyperlipidemia, and a prior myocardial infarction. He takes metformin, glyburide, aspirin, and atorvastatin. He drinks 2-3 drinks per week and has a 25 pack-year smoking history. He has been happily married for 40 years. He retired from his job as a construction worker 5 years ago and has been enjoying retirement with his wife. His physician recommends starting a medication that is also used in the treatment of pulmonary hypertension. Which of the following is a downstream effect of this medication?
- A. Increase cGMP degradation
- B. Increase cAMP production
- C. Increase PDE5 activity
- D. Decrease nitric oxide production
- E. Decrease cGMP degradation (Correct Answer)
Phosphodiesterase inhibitors Explanation: ***Decrease cGMP degradation***
- The medication described is likely a **phosphodiesterase-5 (PDE5) inhibitor** (e.g., sildenafil, tadalafil), used for erectile dysfunction and pulmonary hypertension.
- These drugs work by inhibiting the enzyme PDE5, which is responsible for the breakdown of **cyclic GMP (cGMP)**, thereby increasing cGMP levels.
*Increase cGMP degradation*
- This is the **opposite** of the medication's intended effect, as it would lead to reduced cGMP levels and worsen erectile dysfunction.
- An increase in cGMP degradation would diminish the **vasodilatory** effects necessary for erection.
*Increase cAMP production*
- This medication primarily affects the **cGMP pathway**, not directly boosting cyclic AMP (cAMP) production.
- While cAMP also plays a role in vasodilation, it's regulated by different enzymes and pathways, such as **adenylyl cyclase**.
*Increase PDE5 activity*
- This would lead to a more **rapid breakdown of cGMP**, counteracting the goal of the medication and exacerbating erectile dysfunction.
- The medication's mechanism is specifically designed to **inhibit PDE5 activity**.
*Decrease nitric oxide production*
- **Nitric oxide (NO)** production is a **precursor** to cGMP synthesis, as NO activates guanylate cyclase to produce cGMP.
- Decreasing NO production would **reduce cGMP levels**, which is contrary to the action of PDE5 inhibitors.
Phosphodiesterase inhibitors US Medical PG Question 3: A 70-year-old man presents to an urgent care clinic with bilateral flank pain for the past 2 days. During the last week, he has been experiencing some difficulty with urination, which prevented him from leaving his home. Now, he has to go to the bathroom 4–5 times per hour and he wakes up multiple times during the night to urinate. He also complains of straining and difficulty initiating urination with a poor urinary stream. The temperature is 37.5°C (99.5°F), the blood pressure is 125/90 mm Hg, the pulse is 90/min, and the respiratory rate is 18/min. The physical examination showed bilateral flank tenderness and palpable kidneys bilaterally. A digital rectal exam revealed a smooth, severely enlarged prostate without nodules. A CT scan is obtained. He is prescribed a drug that will alleviate his symptoms by reducing the size of the prostate. Which of the following best describes the mechanism of action of this drug?
- A. 5-alpha reductase inhibitor (Correct Answer)
- B. Cholinergic agonist
- C. Anticholinergic
- D. Phosphodiesterase-5 inhibitors
- E. Alpha-1-adrenergic antagonists
Phosphodiesterase inhibitors Explanation: ***5-alpha reductase inhibitor***
- The patient's symptoms (difficulty urinating, frequent urination, straining, poor stream) and **enlarged prostate** on digital rectal exam are classic for **Benign Prostatic Hyperplasia (BPH)**. The question specifies a drug that *reduces prostate size*.
- **5-alpha reductase inhibitors** (e.g., finasteride, dutasteride) block the conversion of testosterone to **dihydrotestosterone (DHT)**, which is responsible for prostate growth. This leads to a reduction in prostate size over several months.
*Cholinergic agonist*
- **Cholinergic agonists** increase parasympathetic tone, leading to bladder contraction.
- While they might help with bladder emptying in hypotonic bladder, they would not reduce prostate size and could worsen symptoms if the obstruction is severe, potentially leading to increased bladder pressure or hydronephrosis.
*Anticholinergic*
- **Anticholinergic drugs** relax the bladder detrusor muscle, reducing bladder overactivity and symptoms of urgency and frequency.
- They do not address the underlying prostatic hypertrophy or reduce prostate size and could exacerbate urinary retention in a patient with significant prostatic obstruction.
*Phosphodiesterase-5 inhibitors*
- **Phosphodiesterase-5 (PDE5) inhibitors** (e.g., sildenafil, tadalafil) are primarily used for erectile dysfunction, and tadalafil can also improve BPH symptoms by relaxing smooth muscle in the bladder neck and prostate.
- However, they do not **reduce the size of the prostate**; their mechanism of action is related to smooth muscle relaxation, not inhibition of prostate growth.
*Alpha-1-adrenergic antagonists*
- **Alpha-1-adrenergic antagonists** (e.g., tamsulosin, doxazosin) relax the smooth muscle in the prostate and bladder neck, improving urinary flow by reducing dynamic obstruction.
- While effective for BPH symptoms, they do not **reduce the size of the prostate**; they only alleviate symptoms by relaxing the existing tissue.
Phosphodiesterase inhibitors US Medical PG Question 4: A 52-year-old man with a history of hypertension and hyperlipidemia comes to the physician because of a 10-month history of substernal chest pain on exertion that is relieved with rest. His pulse is 82/min and blood pressure is 145/82 mm Hg. He is prescribed a drug that acts by forming free radical nitric oxide. The patient is most likely to experience which of the following adverse effects as a result of this drug?
- A. Pulsating headaches (Correct Answer)
- B. Erectile dysfunction
- C. Hypertensive urgency
- D. Lower extremity edema
- E. Nonproductive cough
Phosphodiesterase inhibitors Explanation: ***Pulsating headaches***
- The drug described is likely **nitroglycerin** or another **nitrate**, which acts by releasing **nitric oxide (NO)** to cause **vasodilation**.
- **Vasodilation** in the cerebral vasculature is a common side effect of nitrates and can lead to **pulsating headaches**.
*Erectile dysfunction*
- **Erectile dysfunction** is not a direct adverse effect of nitrates; in fact, nitrates can be used to treat it, though their use with PDE5 inhibitors is contraindicated.
- This condition is more commonly associated with the underlying cardiovascular disease rather than the medication used to treat angina.
*Hypertensive urgency*
- **Nitrates** cause **vasodilation** and typically **lower blood pressure**, making **hypotension** (not hypertension) a potential side effect.
- **Hypertensive urgency** would indicate a sudden, severe elevation in blood pressure, which is antithetical to the drug's mechanism of action.
*Lower extremity edema*
- **Lower extremity edema** is generally not a direct side effect of nitrates; it is more commonly associated with conditions like **heart failure**, certain **calcium channel blockers**, or **venous insufficiency**.
- While vasodilation can sometimes lead to fluid shifts, edema is not a prominent or expected adverse effect of this class of drugs.
*Nonproductive cough*
- A **nonproductive cough** is a common side effect of **ACE inhibitors** (e.g., lisinopril), which act on the **renin-angiotensin-aldosterone system**.
- This symptom is not associated with **nitrates** because their mechanism of action is primarily through nitric oxide-mediated vasodilation, unrelated to the respiratory irritation seen with ACE inhibitors.
Phosphodiesterase inhibitors US Medical PG Question 5: A 65-year-old male with a history of CHF presents to the emergency room with shortness of breath, lower leg edema, and fatigue. He is diagnosed with acute decompensated congestive heart failure, was admitted to the CCU, and treated with a medication that targets beta-1 adrenergic receptors preferentially over beta-2 adrenergic receptors. The prescribing physician explained that this medication would only be used temporarily as its efficacy decreases within 2-3 days due to receptor downregulation. Which of the following was prescribed?
- A. Epinephrine
- B. Norepinephrine
- C. Milrinone
- D. Isoproterenol
- E. Dobutamine (Correct Answer)
Phosphodiesterase inhibitors Explanation: ***Dobutamine***
- **Dobutamine** is a beta-1 adrenergic agonist preferentially acting on beta-1 receptors in the heart, increasing contractility and heart rate during acute decompensated heart failure.
- Its efficacy reduces over time due to **receptor downregulation**, making it effective for only short-term use, typically less than 72 hours.
*Epinephrine*
- **Epinephrine** is a non-selective adrenergic agonist acting on both alpha and beta receptors, causing vasoconstriction and bronchodilation in addition to cardiac stimulation.
- It is typically used in emergency situations like **cardiac arrest** and **anaphylaxis**, not primarily for acute CHF exacerbation in this manner.
*Norepinephrine*
- **Norepinephrine** primarily acts on alpha-1 adrenergic receptors, causing significant vasoconstriction, and has some beta-1 agonistic effects.
- It is mainly used as a **vasopressor** in septic shock or severe hypotension to increase systemic vascular resistance, rather than directly improving cardiac output in decompensated CHF.
*Milrinone*
- **Milrinone** is a phosphodiesterase-3 inhibitor, increasing intracellular cAMP levels and leading to positive inotropy and vasodilation.
- While used in acute heart failure, its mechanism is distinct from adrenergic agonists, and its efficacy is not limited by a rapid receptor downregulation mechanism as described.
*Isoproterenol*
- **Isoproterenol** is a non-selective beta-adrenergic agonist, stimulating both beta-1 and beta-2 receptors, leading to increased heart rate and contractility, as well as bronchodilation and vasodilation.
- Due to its strong chronotropic effects and potential for severe arrhythmias and hypotension, it is rarely used in CHF and is primarily reserved for conditions like **bradycardia** or **torsades de pointes**.
Phosphodiesterase inhibitors US Medical PG Question 6: The drug cilostazol is known for its ability to relax vascular smooth muscle and therefore cause vasodilation through its inhibition of phosphodiesterase 3. Given this mechanism of action, what other effect would be expected?
- A. Antiarrhythmic action
- B. Negative chronotropy
- C. Angioedema
- D. Increased left ventricular end-diastolic volume
- E. Positive inotropy (Correct Answer)
Phosphodiesterase inhibitors Explanation: ***Positive inotropy***
- **Cilostazol** inhibits **phosphodiesterase 3 (PDE3)**, leading to an increase in **cAMP** levels within cardiac myocytes.
- Increased **cAMP** in the heart results in enhanced calcium influx and release, which strengthens myocardial contraction, leading to **positive inotropy**.
*Antiarrhythmic action*
- While some drugs affecting **cAMP** can have antiarrhythmic effects, **PDE3 inhibitors** like cilostazol can sometimes **increase heart rate** and potentially cause or worsen arrhythmias due to increased conduction and excitability.
- Their primary mechanism of action for cardiac effects is **inotropy**, not rhythm stabilization.
*Negative chronotropy*
- **Negative chronotropy** refers to a decrease in heart rate, which is typically seen with drugs that reduce **cAMP** or directly inhibit the **sinoatrial node**.
- As a **PDE3 inhibitor**, cilostazol leads to increased **cAMP**, which usually causes a modest increase in heart rate (**positive chronotropy**), not a decrease.
*Angioedema*
- **Angioedema** is a side effect often associated with **ACE inhibitors** or certain allergic reactions, mediated by bradykinin or histamine release.
- It is not a known or expected effect of **cilostazol** based on its mechanism of **PDE3 inhibition** and cAMP modulation.
*Increased left ventricular end-diastolic volume*
- **Cilostazol** causes **vasodilation**, which **reduces peripheral vascular resistance** and thus **afterload**.
- This reduction in afterload, combined with its **positive inotropic** effects, tends to improve cardiac output and can actually lead to a **decrease** in **left ventricular end-diastolic volume** due to more efficient ejection, rather than an increase.
Phosphodiesterase inhibitors US Medical PG Question 7: A 52-year-old man is seen by his endocrinologist for routine followup of his type 2 diabetes. Although he has previously been on a number of medication regimens, his A1C has remained significantly elevated. In order to try to better control his glucose level, the endocrinologist prescribes a new medication. He explains that this new medication works by blocking the ability of his kidneys to reabsorb glucose and therefore causes glucose wasting in the urine. Which of the following medications has this mechanism of action?
- A. Canagliflozin (Correct Answer)
- B. Acarbose
- C. Metformin
- D. Glyburide
- E. Exenatide
Phosphodiesterase inhibitors Explanation: ***Canagliflozin***
- **Canagliflozin** is an **SGLT2 inhibitor** that works by blocking the reabsorption of glucose in the renal tubules, leading to glucose excretion in the urine.
- This mechanism of action directly matches the description provided: "blocking the ability of his kidneys to reabsorb glucose and therefore causes glucose wasting in the urine."
*Acarbose*
- **Acarbose** is an **alpha-glucosidase inhibitor** that delays the digestion and absorption of carbohydrates in the small intestine.
- Its primary action is in the gastrointestinal tract, not by directly affecting renal glucose reabsorption.
*Metformin*
- **Metformin** is a **biguanide** that primarily works by decreasing hepatic glucose production and improving insulin sensitivity.
- It does not directly affect the kidney's ability to reabsorb glucose.
*Glyburide*
- **Glyburide** is a **sulfonylurea** that stimulates insulin secretion from pancreatic beta cells.
- Its mechanism involves increasing insulin release, independent of renal glucose handling.
*Exenatide*
- **Exenatide** is a **GLP-1 receptor agonist** that enhances glucose-dependent insulin secretion, suppresses glucagon secretion, slows gastric emptying, and promotes satiety.
- Its actions are mainly related to insulin and glucagon regulation, not direct renal glucose filtration.
Phosphodiesterase inhibitors US Medical PG Question 8: A researcher is studying how arachidonic acid metabolites mediate the inflammatory response in rats. She has developed multiple enzyme inhibitors that specifically target individual proteins in the arachidonic acid pathway. She injects these inhibitors in rats who have been exposed to common bacterial pathogens and analyzes their downstream effects. In one of her experiments, she injects a leukotriene B4 inhibitor into a rat and observes an abnormal cell response. Which of the following interleukins would most closely restore the function of one of the missing products?
- A. Interleukin 2
- B. Interleukin 4
- C. Interleukin 1
- D. Interleukin 5
- E. Interleukin 8 (Correct Answer)
Phosphodiesterase inhibitors Explanation: ***Interleukin 8***
- **Leukotriene B4 (LTB4)** is a potent **chemoattractant** and activator of neutrophils.
- **Interleukin 8 (IL-8)**, also known as **CXCL8**, is a primary **chemoattractant** for neutrophils, functionally mimicking the role of LTB4 in recruiting these inflammatory cells to the site of infection.
*Interleukin 2*
- **IL-2** is primarily involved in the **growth, proliferation, and differentiation of T cells**, as well as the activation of B cells and natural killer cells.
- It does not have a significant role in **neutrophil chemotaxis**, which is the main function of LTB4.
*Interleukin 4*
- **IL-4** is crucial for **B cell activation** and class switching to IgE, and it's a key cytokine in the **Th2 immune response**.
- Its functions are related to **allergic reactions** and **parasitic infections**, not neutrophil recruitment.
*Interleukin 1*
- **IL-1** is a pro-inflammatory cytokine that mediates a wide range of immune responses, including **fever** and the activation of other immune cells.
- While it contributes to inflammation, it does not directly act as a **chemoattractant for neutrophils** in the same manner as LTB4 or IL-8.
*Interleukin 5*
- **IL-5** is primarily involved in the **growth and differentiation of eosinophils** and B cell IgA production.
- It plays a significant role in **allergic reactions** and defense against parasites, not neutrophil chemotaxis.
Phosphodiesterase inhibitors US Medical PG Question 9: A 66-year-old male with a history of deep venous thrombosis is admitted to the hospital with shortness of breath and pleuritic chest pain. He is treated with an anticoagulant, but he develops significant hematochezia. His BP is now 105/60 and HR is 117; both were within normal limits on admission. The effects of the anticoagulant are virtually completely reversed with the administration of protamine. Which of the following was the anticoagulant most likely administered to this patient?
- A. Enoxaparin
- B. Dabigatran
- C. Bivalirudin
- D. Warfarin
- E. Heparin (Correct Answer)
Phosphodiesterase inhibitors Explanation: ***Heparin***
- **Protamine sulfate** is the specific and virtually complete antidote for **unfractionated heparin (UFH)** and, to a lesser extent, low molecular weight heparins (LMWH).
- The patient's presentation with **shortness of breath** and **pleuritic chest pain** suggests a **pulmonary embolism (PE)**, a common indication for heparin.
*Enoxaparin*
- Enoxaparin is a **low molecular weight heparin (LMWH)**. While protamine can partially reverse LMWH effects, it is **not complete** (only 60-75% reversal) compared to UFH.
- LMWHs have a **longer half-life** and less predictable reversal with protamine than UFH.
*Dabigatran*
- Dabigatran is a **direct thrombin inhibitor** and its antidote is **idarucizumab**, not protamine.
- This drug is not reversible by protamine.
*Bivalirudin*
- Bivalirudin is a **direct thrombin inhibitor** used mainly during percutaneous coronary intervention and its effects are **not reversible with protamine**.
- Its short half-life often makes reversal agents unnecessary, but there is no specific antidote listed.
*Warfarin*
- Warfarin is a **vitamin K antagonist** and its effects are reversed by **vitamin K**, fresh frozen plasma (FFP), or prothrombin complex concentrates (PCCs), not protamine.
- Warfarin also has a **delayed onset of action**, making it less suitable for acute treatment of a suspected PE.
Phosphodiesterase inhibitors US Medical PG Question 10: A 59-year-old woman comes to the clinic complaining of an intermittent, gnawing epigastric pain for the past 2 months. The pain is exacerbated with food and has been getting progressively worse. The patient denies any weight changes, nausea, vomiting, cough, or dyspepsia. Medical history is significant for chronic back pain for which she takes ibuprofen. Her father passed at the age of 55 due to pancreatic cancer. Labs were unremarkable except for a mild decrease in hemoglobin. What medication is most appropriate to be switched to from the current medication at this time?
- A. Naproxen
- B. Ranitidine
- C. Aspirin
- D. Acetaminophen
- E. Omeprazole (Correct Answer)
Phosphodiesterase inhibitors Explanation: ***Omeprazole***
- The patient's symptoms of **gnawing epigastric pain** exacerbated by food, along with a history of chronic ibuprofen use and mild anemia, strongly suggest a **peptic ulcer**.
- **Omeprazole**, a proton pump inhibitor (PPI), is the most effective medication for healing ulcers and preventing their recurrence by reducing gastric acid production.
*Naproxen*
- **Naproxen** is a non-steroidal anti-inflammatory drug (NSAID), similar to ibuprofen, and would likely worsen the patient's symptoms by further inhibiting prostaglandin synthesis necessary for gastric mucosal protection.
- Continuing an NSAID without gastroprotection would increase the risk of ulcer complications, such as bleeding.
*Ranitidine*
- **Ranitidine** is an H2-receptor antagonist, which reduces stomach acid, but it is generally less potent than PPIs like omeprazole for treating and healing ulcers, especially in cases of NSAID-induced gastropathy.
- Its efficacy for advanced or severe peptic ulcer disease is inferior to that of PPIs.
- Note: Ranitidine was withdrawn from the US market in 2020 due to NDMA contamination; alternative H2 blockers include famotidine.
*Aspirin*
- **Aspirin** is an NSAID with significant antiplatelet effects and is well-known to cause and exacerbate peptic ulcers and gastrointestinal bleeding.
- Switching to aspirin would be contraindicated in the presence of strong evidence suggesting active peptic ulcer disease.
*Acetaminophen*
- **Acetaminophen** (paracetamol) is an analgesic that does not have significant anti-inflammatory properties and is not associated with gastric irritation or ulcer formation.
- While it could be used for pain relief, it does not address the underlying issue of peptic ulcer disease or provide gastroprotection, making it an inadequate switch for effective management.
More Phosphodiesterase inhibitors US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.