Peripheral vascular disease therapies US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Peripheral vascular disease therapies. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Peripheral vascular disease therapies US Medical PG Question 1: A 67-year-old man comes to the office due to pain in the lower part of his calves on his afternoon walk to get the mail. The pain is relieved by rest. It started slowly about 6 months ago and has become more painful over time. He has a history of hypertension, hyperlipidemia, diabetes mellitus, and a 20-pack-year smoking history. Medications include hydrochlorothiazide, atorvastatin, metformin, and a multivitamin that he takes daily. The patient quit smoking 2 years ago and only drinks socially. Today, his blood pressure is 145/90 mm Hg, pulse is 75/min, respiratory rate is 17/min, and temperature is 37.6°C (99.6°F). On physical exam, he appears mildly obese and healthy. His heart has a regular rate and rhythm, and his lungs are clear to auscultation bilaterally. Examination of the legs shows atrophic changes and diminished pedal pulses. A measure of his ankle brachial index (ABI) is 0.89. Which of the following is the most appropriate initial treatment?
- A. A recommendation to walk more
- B. Metoprolol
- C. A recommendation to perform pedal pumping exercises
- D. A referral to a supervised exercise program (Correct Answer)
- E. Enoxaparin
Peripheral vascular disease therapies Explanation: ***A referral to a supervised exercise program***
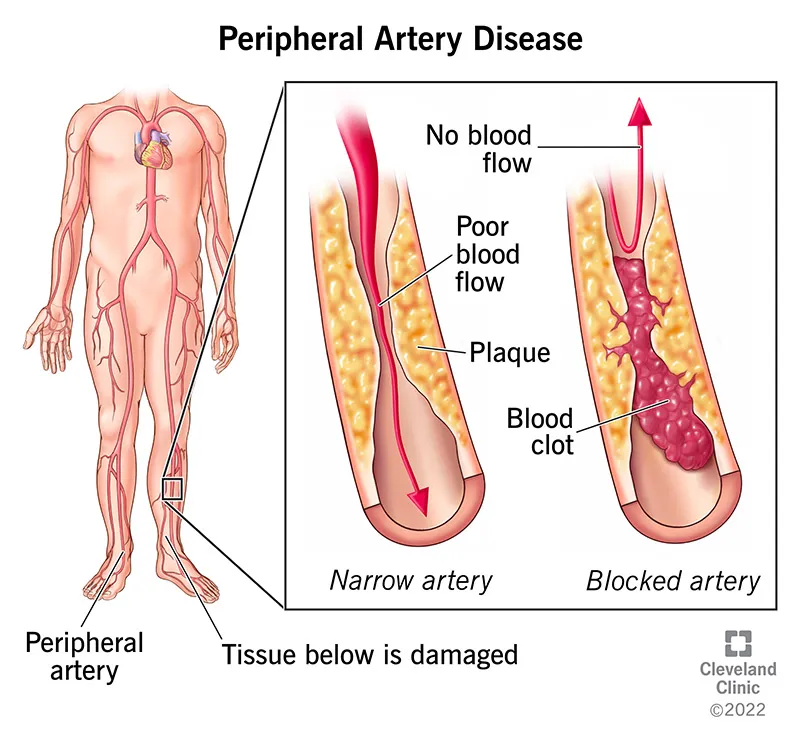
- The patient's symptoms (claudication, relief with rest), risk factors (**hypertension, hyperlipidemia, diabetes, smoking history**), physical exam findings (**atrophic changes, diminished pedal pulses**), and **ABI of 0.89** (indicating mild peripheral artery disease) all point to **peripheral arterial disease (PAD)**.
- A **supervised exercise program**, particularly walking, is the most effective initial non-pharmacological treatment for improving walking distance and quality of life in patients with claudication due to PAD.
*A recommendation to walk more*
- While walking is beneficial, simply recommending "walking more" without specific guidance or supervision is less effective than a structured program.
- An unsupervised general walking recommendation may not optimize the **duration**, **intensity**, or **frequency** needed for therapeutic benefit in PAD.
*Metoprolol*
- **Beta-blockers** like metoprolol can worsen claudication symptoms by decreasing blood flow to the extremities, especially in patients with PAD.
- They are generally **contraindicated** or used with caution in PAD patients experiencing claudication.
*A recommendation to perform pedal pumping exercises*
- **Pedal pumping exercises** are primarily used to prevent **venous stasis** and **deep vein thrombosis**, typically post-surgery or during prolonged immobility.
- They do not address the underlying arterial insufficiency causing claudication and are not an effective treatment for PAD.
*Enoxaparin*
- **Enoxaparin** is a low molecular weight heparin, an **anticoagulant** used for conditions like deep vein thrombosis or acute coronary syndromes.
- It is not indicated for the chronic management of stable claudication in peripheral artery disease, where antiplatelet therapy is generally preferred if medication is needed.
Peripheral vascular disease therapies US Medical PG Question 2: A 62-year-old man presents to his primary care provider complaining of leg pain with exertion for the past 6 months. He notices that he has bilateral calf cramping with walking. He states that it is worse in his right calf than in his left, and it goes away when he stops walking. He has also noticed that his symptoms are progressing and that this pain is occurring sooner than before. His medical history is remarkable for type 2 diabetes mellitus and 30-pack-year smoking history. His ankle-brachial index (ABI) is found to be 0.80. Which of the following can be used as initial therapy for this patient's condition?
- A. Endovascular revascularization
- B. Arthroscopic resection
- C. Duloxetine
- D. Heparin
- E. Cilostazol (Correct Answer)
Peripheral vascular disease therapies Explanation: ***Cilostazol***
- This patient presents with symptoms highly suggestive of **peripheral artery disease (PAD)**, characterized by **intermittent claudication** (leg pain with exertion relieved by rest) and a **low ankle-brachial index (ABI)** of 0.80.
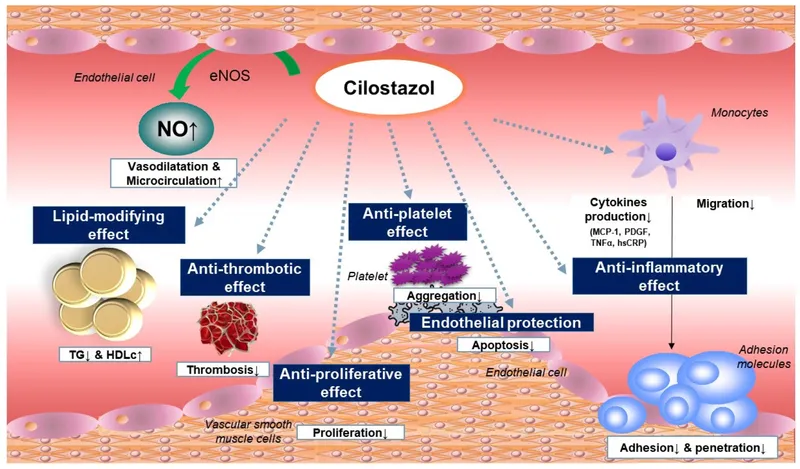
- **Cilostazol** is a phosphodiesterase inhibitor specifically approved for the symptomatic relief of **intermittent claudication** in patients with PAD, improving walking distance and quality of life.
*Endovascular revascularization*
- **Endovascular revascularization** (e.g., angioplasty, stenting) is typically reserved for patients with more severe symptoms, such as **rest pain**, **non-healing ulcers**, or **gangrene**, or for those who have failed appropriate medical therapy.
- Initial management of **intermittent claudication** usually begins with lifestyle modifications and pharmacotherapy, given the less severe presentation and the current guidelines.
*Arthroscopic resection*
- **Arthroscopic resection** is a surgical procedure primarily used for joint-related problems, such as removing damaged cartilage or bone spurs from a joint.
- It is not indicated for the treatment of **peripheral artery disease** or **intermittent claudication**, which is a vascular condition.
*Duloxetine*
- **Duloxetine** is a serotonin-norepinephrine reuptake inhibitor (SNRI) primarily used for the treatment of **neuropathic pain**, depression, and generalized anxiety disorder.
- While the patient has diabetes (a risk factor for neuropathy), the symptom of **intermittent claudication associated with exertion** and a low ABI points away from neuropathic pain as the primary cause.
*Heparin*
- **Heparin** is an anticoagulant used to prevent blood clot formation, typically in acute settings like **deep vein thrombosis (DVT)**, **pulmonary embolism (PE)**, or acute limb ischemia.
- It is not indicated for the long-term management of stable **peripheral artery disease** with intermittent claudication, as it does not address the underlying atherosclerotic process.
Peripheral vascular disease therapies US Medical PG Question 3: A primary care physician who focuses on treating elderly patients is researching recommendations for secondary prevention. She is particularly interested in recommendations regarding aspirin, as she has several patients who ask her if they should take it. Of the following, which patient should be started on lifelong aspirin as monotherapy for secondary prevention of atherosclerotic cardiovascular disease?
- A. An 83-year-old female with a history of a hemorrhagic stroke 1 year ago without residual deficits
- B. A 75-year-old male who had a drug-eluting coronary stent placed 3 days ago
- C. A 67-year-old female who has diabetes mellitus and atrial fibrillation
- D. A 45-year-old female with no health problems
- E. A 63-year-old male with a history of a transient ischemic attack (Correct Answer)
Peripheral vascular disease therapies Explanation: **A 63-year-old male with a history of a transient ischemic attack**
- A patient with a history of **Transient Ischemic Attack (TIA)** has a high risk of subsequent stroke and should be on **lifelong aspirin monotherapy** for secondary prevention of **atherosclerotic cardiovascular disease (ASCVD)**.
- Aspirin helps prevent further thrombotic events by inhibiting platelet aggregation, making it a cornerstone for secondary prevention after TIA or ischemic stroke.
*An 83-year-old female with a history of a hemorrhagic stroke 1 year ago without residual deficits*
- Aspirin is generally **contraindicated** in patients with a history of **hemorrhagic stroke** due to the increased risk of recurrent bleeding.
- In such cases, the risks of aspirin therapy typically **outweigh the benefits** for cardiovascular prevention.
*A 75-year-old male who had a drug-eluting coronary stent placed 3 days ago*
- A patient with a recently placed **drug-eluting stent (DES)** requires **dual antiplatelet therapy (DAPT)**, typically aspirin plus a P2Y12 inhibitor, for a specific duration (e.g., 6-12 months), not aspirin monotherapy.
- Monotherapy with aspirin alone would be **insufficient** to prevent stent thrombosis in the immediate post-stenting period.
*A 67-year-old female who has diabetes mellitus and atrial fibrillation*
- This patient has two significant risk factors requiring specific management: **diabetes mellitus** for cardiovascular risk and **atrial fibrillation** for stroke risk.
- For atrial fibrillation, **anticoagulation with warfarin or a direct oral anticoagulant (DOAC)** is typically indicated, which makes aspirin monotherapy either unnecessary or potentially harmful if used alone.
*A 45-year-old female with no health problems*
- There is no indication for **aspirin primary prevention** in this patient, especially given the increased risk of bleeding without a clear cardiovascular benefit.
- Guidelines currently recommend against routine aspirin use for primary prevention in healthy individuals due to the **unfavorable risk-benefit ratio**.
Peripheral vascular disease therapies US Medical PG Question 4: A 58-year-old man comes to the physician because of a 3-month history of intermittent pain in his right calf that occurs after walking up more than 2 flights of stairs. He reports that the pain is associated with a tingling sensation and lasts for about 10 minutes. He is otherwise healthy. He has smoked 2 packs of cigarettes daily for 30 years and drinks 1 alcoholic beverage daily. He currently takes no medications. His pulse is 78/min, and blood pressure is 180/110 mm Hg. Physical examination shows yellow plaques below the lower eyelids bilaterally, loss of hair on the distal third of the right leg, and brittle toenails on the right foot. Femoral pulses are palpable bilaterally; right popliteal and pedal pulses are absent. Which of the following is the most appropriate management to prevent future morbidity and mortality of this patient's condition?
- A. Clopidogrel therapy (Correct Answer)
- B. Percutaneous transluminal angioplasty
- C. Cilostazol therapy
- D. Graded exercise therapy
- E. Pentoxifylline therapy
Peripheral vascular disease therapies Explanation: ***Clopidogrel therapy***
- **Antiplatelet therapy** with clopidogrel (or aspirin) is crucial for **preventing future morbidity and mortality** in PAD patients by reducing the risk of **myocardial infarction**, stroke, and cardiovascular death.
- PAD is a manifestation of systemic atherosclerosis, and these patients have significantly elevated cardiovascular risk. Antiplatelet therapy addresses this systemic risk and is a cornerstone of medical management.
- Current guidelines (ACC/AHA) strongly recommend antiplatelet therapy for all patients with symptomatic PAD to reduce adverse cardiovascular events.
*Graded exercise therapy*
- **Graded exercise therapy** is highly effective for improving walking distance and reducing claudication symptoms by promoting collateral circulation and improving endothelial function.
- While exercise is essential for symptom management and quality of life, it is **not the primary intervention for preventing mortality** in PAD patients, which is what this question specifically asks about.
- Exercise should be recommended alongside antiplatelet therapy and risk factor modification.
*Pentoxifylline therapy*
- **Pentoxifylline** may improve red blood cell flexibility and microcirculation, but it has shown limited efficacy for symptom relief and **no proven benefit for reducing cardiovascular mortality**.
- Its use is generally reserved for patients who cannot tolerate other treatments.
*Percutaneous transluminal angioplasty*
- **Revascularization** (PTA or surgical bypass) is typically reserved for patients with severe, lifestyle-limiting claudication unresponsive to medical therapy, or for critical limb ischemia.
- This patient has intermittent claudication with moderate symptoms, making conservative medical management more appropriate initially.
- Revascularization improves symptoms but does not reduce mortality compared to medical therapy alone.
*Cilostazol therapy*
- **Cilostazol** is a phosphodiesterase-3 inhibitor that improves walking distance and claudication symptoms through vasodilation and antiplatelet effects.
- While effective for symptomatic relief, it does **not reduce cardiovascular mortality** and has a contraindication in heart failure patients.
- It is used as an adjunct for symptom management, not as primary prevention of morbidity and mortality.
Peripheral vascular disease therapies US Medical PG Question 5: A 26-year-old man comes to the physician because of a 1-week history of left-sided chest pain. The pain is worse when he takes deep breaths. Over the past 6 weeks, he had been training daily for an upcoming hockey tournament. He does not smoke cigarettes or drink alcohol but has used cocaine once. His temperature is 37.1°C (98.7°F), pulse is 75/min, and blood pressure is 128/85 mm Hg. Physical examination shows tenderness to palpation of the left chest. An x-ray of the chest is shown. Which of the following is the most appropriate initial pharmacotherapy?
- A. Heparin
- B. Nitroglycerin
- C. Alteplase
- D. Naproxen (Correct Answer)
- E. Alprazolam
Peripheral vascular disease therapies Explanation: ***Naproxen***
- This patient presents with symptoms highly suggestive of **costochondritis** or a **musculoskeletal chest wall pain**. Key features include **tenderness to palpation of the chest wall**, pain made worse by **deep breaths** (pleuritic nature), and a history of strenuous activity (hockey training).
- An X-ray of the chest appears normal, ruling out other serious causes of chest pain like pneumothorax or significant infiltrates. Given the musculoskeletal nature of the pain, a **nonsteroidal anti-inflammatory drug (NSAID)** like naproxen is the most appropriate initial treatment to reduce pain and inflammation.
*Heparin*
- Heparin is an **anticoagulant** used to treat or prevent blood clots, such as in **pulmonary embolism** or deep vein thrombosis.
- While chest pain can be a symptom of pulmonary embolism, the physical exam finding of **localized tenderness to palpation** is not characteristic of a pulmonary embolism, and the normal chest X-ray makes it less likely.
*Nitroglycerin*
- Nitroglycerin is primarily used to treat **angina pectoris** (chest pain due to reduced blood flow to the heart) by causing vasodilation and reducing cardiac workload.
- The patient's age (26), absence of typical cardiac risk factors (except for prior cocaine use, which can cause vasospasm but is not suggested by the clinical picture or exam), and the **pleuritic nature of the pain** with **chest wall tenderness** make angina unlikely.
*Alteplase*
- Alteplase is a **thrombolytic agent** used to dissolve existing blood clots, typically in conditions like **acute myocardial infarction**, **pulmonary embolism**, or **ischemic stroke**.
- There is no clinical or radiological evidence (normal chest X-ray) to suggest a life-threatening thrombotic event requiring thrombolysis in this patient.
*Alprazolam*
- Alprazolam is a **benzodiazepine** used to treat **anxiety and panic disorders**.
- While anxiety can sometimes manifest as chest pain, the clear physical finding of **localized chest wall tenderness** points to a physical cause, and thus, an anxiolytic is not the most appropriate initial pharmacotherapy.
Peripheral vascular disease therapies US Medical PG Question 6: A 43-year-old woman comes to the physician because of a 3-month history of a painless ulcer on the sole of her right foot. There is no history of trauma. She has been dressing the ulcer once daily at home with gauze. She has a 15-year history of poorly-controlled type 1 diabetes mellitus and hypertension. Current medications include insulin and lisinopril. Vital signs are within normal limits. Examination shows a 2 x 2-cm ulcer on the plantar aspect of the base of the great toe with whitish, loose tissue on the floor of the ulcer and a calloused margin. A blunt metal probe reaches the deep plantar space. Sensation to vibration and light touch is decreased over both feet. Pedal pulses are intact. An x-ray of the right foot shows no abnormalities. Which of the following is the most appropriate initial step in management?
- A. Surgical revascularization of the right foot
- B. Amputation of the right forefoot
- C. Total contact casting of right foot
- D. Intravenous antibiotic therapy
- E. Sharp surgical debridement of the ulcer (Correct Answer)
Peripheral vascular disease therapies Explanation: ***Sharp surgical debridement of the ulcer***
- The presence of a **painless ulcer**, decreased sensation (neuropathy), and a calloused margin with loose tissue indicates a **neuropathic ulcer** common in diabetic patients. **Sharp surgical debridement** is crucial to remove non-viable tissue and promote healing.
- The probe reaching the deep plantar space suggests a potential deep infection or osteomyelitis, which needs aggressive debridement to remove all infected and necrotic tissue. However, since the X-ray is normal, it is less likely to have osteomyelitis, but it needs to be ruled out by further investigations.
*Surgical revascularization of the right foot*
- This is primarily indicated for **ischemic ulcers** where blood supply is compromised.
- The patient has **intact pedal pulses**, meaning good distal blood flow, making revascularization unnecessary at this stage.
*Amputation of the right forefoot*
- Amputation is a measure of last resort for **severe, non-healing ulcers** with extensive infection or gangrene that fail to respond to conservative and surgical debridement.
- The current presentation does not warrant such an extreme intervention as a first step.
*Total contact casting of right foot*
- **Total contact casting** is used for **off-loading pressure** from a neuropathic ulcer to facilitate healing.
- While it's an important step in management, it should generally follow **debridement** to ensure a clean wound bed.
*Intravenous antibiotic therapy*
- This is indicated if there are definitive signs of **spreading infection** (e.g., cellulitis, fever, purulence).
- While debridement helps prevent infection by removing necrotic tissue, there is no mention of systemic signs of infection or severe local infection requiring immediate IV antibiotics.
Peripheral vascular disease therapies US Medical PG Question 7: A 67-year-old man presents with pain in both legs. He says the pain is intermittent in nature and has been present for approximately 6 months. The pain increases with walking, especially downhill, and prolonged standing. It is relieved by lying down and leaning forward. Past medical history is significant for type 2 diabetes mellitus, hypercholesterolemia, and osteoarthritis. The patient reports a 56-pack-year history but denies any alcohol or recreational drug use. His vital signs include: blood pressure 142/88 mm Hg, pulse 88/min, respiratory rate 14/min, temperature 37°C (98.6°F). On physical examination, the patient is alert and oriented. Muscle strength is 5/5 in his upper and lower extremities bilaterally. Babinski and Romberg tests are negative. Pulses measure 2+ in upper and lower extremities bilaterally. Which of the following is the next best step in the management of this patient?
- A. MRI of the spine (Correct Answer)
- B. CT angiography of the lower extremities
- C. Ankle-brachial index
- D. Cilostazol
- E. Epidural corticosteroid injection
Peripheral vascular disease therapies Explanation: ***MRI of the spine***
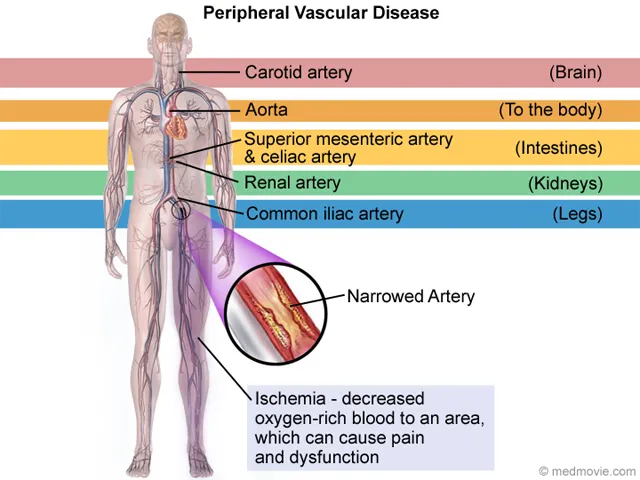
- The patient's symptoms of **intermittent leg pain worsened by walking (especially downhill) and prolonged standing**, and **relieved by lying down and leaning forward**, are highly classic for **neurogenic claudication** due to **lumbar spinal stenosis**.
- An **MRI of the spine** is the *gold standard* for diagnosing spinal stenosis, clearly visualizing nerve root compression and the degree of canal narrowing.
*CT angiography of the lower extremities*
- This imaging is used to assess **peripheral artery disease** (PAD) but the patient's symptoms are inconsistent with vascular claudication.
- **Vascular claudication** typically improves with rest, not with specific postures like leaning forward.
*Ankle-brachial index*
- The **ankle-brachial index (ABI)** is a non-invasive test to screen for **peripheral artery disease (PAD)**.
- While the patient has risk factors for PAD (diabetes, hypercholesterolemia, smoking), his symptoms are classic for neurogenic claudication, and his **2+ pulses** in the lower extremities make PAD less likely.
*Cilostazol*
- **Cilostazol** is a phosphodiesterase inhibitor used to treat symptoms of **intermittent claudication** caused by **peripheral artery disease (PAD)**.
- Since the patient's symptoms are more consistent with neurogenic claudication rather than vascular claudication, cilostazol would not be the appropriate initial step.
*Epidural corticosteroid injection*
- An **epidural corticosteroid injection** is a treatment option for symptomatic spinal stenosis but is not the *initial diagnostic step*.
- Diagnosis with an **MRI** is necessary before considering targeted therapeutic interventions like injections.
Peripheral vascular disease therapies US Medical PG Question 8: A 38-year-old woman with a history of Crohn’s disease presents with a 3-week history of weight gain. The patient also presents with a 1-month history of abdominal pain, cramping, and bloody diarrhea consistent with worsening of her inflammatory bowel disease. Past medical history is significant for Crohn’s disease diagnosed 2 years ago for which she currently takes an oral medication daily and intermittently receives intravenous medication she cannot recall the name of. Her temperature is 37.0°C (98.6°F), blood pressure is 120/90 mm Hg, pulse is 68/min, respiratory rate is 14/min, and oxygen saturation is 99% on room air. Physical examination reveals significant truncal weight gain. The patient has excessive facial hair in addition to purplish striae on her abdomen. Which of the following laboratory findings would most likely be found in this patient?
- A. Hyperglycemia (Correct Answer)
- B. Hypoglycemia
- C. Metabolic acidosis
- D. Hyperkalemia
- E. Hypokalemia
Peripheral vascular disease therapies Explanation: ***Hyperglycemia***
- The patient exhibits **Cushing's syndrome** due to chronic corticosteroid use for Crohn's disease, with classic features including truncal obesity, hirsutism, and purplish striae.
- **Hyperglycemia is the most common and expected metabolic abnormality** with chronic glucocorticoid therapy, occurring in 30-40% of patients.
- Glucocorticoids cause hyperglycemia by **increasing gluconeogenesis**, **promoting glycogenolysis**, and **inducing insulin resistance** in peripheral tissues.
- This is a direct and prominent effect of glucocorticoid excess, making it the most likely laboratory finding in this clinical scenario.
*Hypokalemia*
- While possible with high-dose corticosteroids, hypokalemia is **less common** with modern synthetic glucocorticoids (prednisone, methylprednisolone) which have minimal mineralocorticoid activity.
- Hypokalemia primarily occurs with corticosteroids having significant mineralocorticoid effects (hydrocortisone, cortisone) or at very high doses.
- Compared to hyperglycemia, this is not the "most likely" finding in typical glucocorticoid therapy.
*Hypoglycemia*
- Glucocorticoids cause **hyperglycemia**, not hypoglycemia, due to their counter-regulatory effects on glucose metabolism.
- This is the opposite of what occurs with steroid excess.
*Metabolic acidosis*
- **Metabolic alkalosis**, not acidosis, can occur with Cushing's syndrome due to mineralocorticoid effects promoting hydrogen ion excretion.
- The hypokalemia that may develop is typically accompanied by alkalosis, not acidosis.
*Hyperkalemia*
- Glucocorticoids promote **potassium excretion** through mineralocorticoid receptor activation, making hyperkalemia unlikely.
- This would contradict the known effects of corticosteroid excess.
Peripheral vascular disease therapies US Medical PG Question 9: A 60-year-old patient is at his physician’s office for a routine health maintenance exam. The patient has a past medical history of osteoarthritis in his right knee and GERD that is well-controlled with over the counter medication. On a fasting lipid profile, he is found to have high cholesterol. The patient is started on daily atorvastatin to reduce his risk of cardiovascular disease. What is the major apolipoprotein found on the lipoprotein most directly affected by his statin medication?
- A. Apolipoprotein C-II
- B. Apolipoprotein B-100 (Correct Answer)
- C. Apolipoprotein A-I
- D. Apolipoprotein B-48
- E. Apolipoprotein E
Peripheral vascular disease therapies Explanation: ***Apolipoprotein B-100***
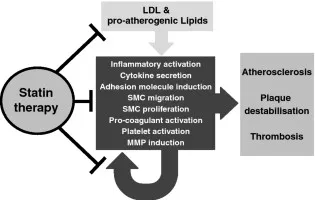
- Statins primarily reduce **LDL-C** levels by inhibiting **HMG-CoA reductase**, leading to increased LDL receptor expression and clearance of LDL particles from the blood.
- **Apolipoprotein B-100** is the main apolipoprotein found on **LDL** and is crucial for its binding to the LDL receptor.
*Apolipoprotein C-II*
- This apolipoprotein activates **lipoprotein lipase**, which is involved in the hydrolysis of triglycerides in **chylomicrons** and **VLDL**, not directly targeted by statins.
- While statins can indirectly affect VLDL, ApoC-II is not the major apolipoprotein of the lipoprotein most directly affected by statins.
*Apolipoprotein A-I*
- **Apolipoprotein A-I** is the primary apolipoprotein found on **HDL**, which is involved in **reverse cholesterol transport**.
- While statins can have a modest effect on increasing HDL, their primary action is on reducing LDL.
*Apolipoprotein B-48*
- **Apolipoprotein B-48** is found exclusively on **chylomicrons**, which are responsible for the transport of exogenous dietary fats from the intestines.
- Chylomicrons are not the primary target of statin therapy, which focuses on endogenous cholesterol metabolism.
*Apolipoprotein E*
- **Apolipoprotein E** is found on chylomicrons, VLDL, and HDL and plays a role in receptor binding for their clearance from circulation.
- While important for lipoprotein metabolism, it is not the *major* apolipoprotein of the lipoprotein most *directly* affected by statins (LDL).
Peripheral vascular disease therapies US Medical PG Question 10: A 21-year-old woman comes to the physician because of a 4-day history of abdominal cramps and bloody diarrhea 5 times per day. Her symptoms began after she ate an egg sandwich from a restaurant. Her vital signs are within normal limits. Physical examination shows diffuse abdominal tenderness. Stool culture shows gram-negative rods that produce hydrogen sulfide and do not ferment lactose. Which of the following effects is most likely to occur if she receives antibiotic therapy?
- A. Orange discoloration of bodily fluids
- B. Pruritic maculopapular rash on the extensor surface
- C. Self-limiting systemic inflammatory response
- D. Prolonged fecal excretion of the pathogen (Correct Answer)
- E. Thrombocytopenia and hemolytic anemia
Peripheral vascular disease therapies Explanation: ***Prolonged fecal excretion of the pathogen***
- The patient's symptoms (abdominal cramps, bloody diarrhea after eating an egg sandwich) and stool culture results (gram-negative rods, hydrogen sulfide producers, non-lactose fermenting) are highly suggestive of **Salmonella enterica** infection.
- Antibiotic treatment for non-typhoidal Salmonella gastroenteritis typically **prolongs fecal excretion** and does not shorten the illness, reserving antibiotics for severe cases or immunocompromised individuals.
*Orange discoloration of bodily fluids*
- **Orange discoloration of bodily fluids** (urine, sweat, tears) is a known side effect of **rifampin**, an antibiotic primarily used for tuberculosis and some bacterial meningitides.
- Rifampin is not indicated nor commonly used for Salmonella gastroenteritis.
*Pruritic maculopapular rash on the extensor surface*
- A **pruritic maculopapular rash on the extensor surfaces** is a common presentation of drug reactions, often associated with **penicillins** or **cephalosporins**, especially in viral infections (e.g., amoxicillin rash in mononucleosis).
- This is a general antibiotic side effect and not specifically linked to the outcome of treating Salmonella.
*Self-limiting systemic inflammatory response*
- A self-limiting systemic inflammatory response could be a general reaction to an active infection or a drug, but it's not the most likely or specific outcome of **antibiotic therapy in Salmonella gastroenteritis**.
- Worsening of symptoms can occur in some cases due to toxemia from bacterial lysis (e.g., Jarisch-Herxheimer reaction), but "self-limiting systemic inflammatory response" is too generic for this specific scenario.
*Thrombocytopenia and hemolytic anemia*
- **Thrombocytopenia and hemolytic anemia** in the setting of diarrheal illness strongly suggest **hemolytic uremic syndrome (HUS)**, which is typically associated with **Shiga toxin-producing E. coli** (STEC), particularly E. coli O157:H7.
- While Salmonella can cause severe disease, HUS is not a typical complication of its treatment, and antibiotics are often avoided in STEC infections due to increased risk of HUS.
More Peripheral vascular disease therapies US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.