Other antiarrhythmic agents US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Other antiarrhythmic agents. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
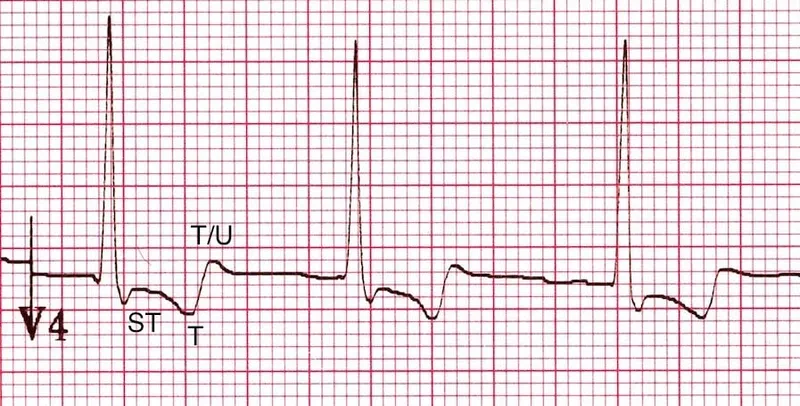
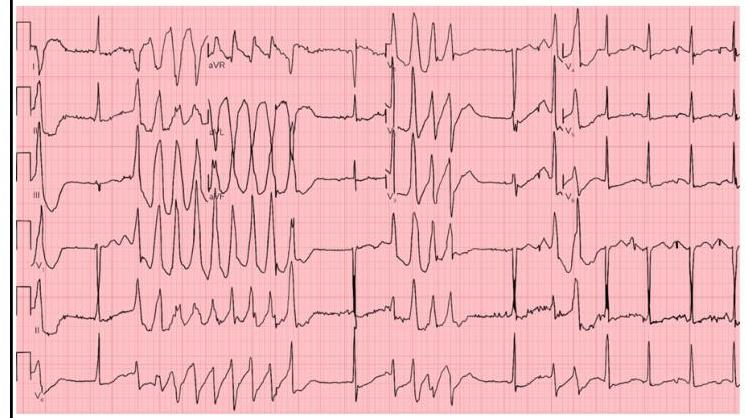
Other antiarrhythmic agents US Medical PG Question 1: A 53-year-old man with obesity and heart disease presents to your outpatient clinic with complaints of orthopnea, significant dyspnea on minimal exertion, nausea, vomiting, and diarrhea. He says that his old doctor gave him "some pills" that he takes in varying amounts every morning. Physical exam is significant for a severely displaced point of maximal impulse, bilateral rales in the lower lung fields, an S3 gallop, and hepatomegaly. You decide to perform an EKG (shown in figure A). Suddenly, his rhythm changes to ventricular tachycardia followed by ventricular fibrillation, and he syncopizes and expires despite resuscitative efforts. High levels of which medication are most likely responsible?
- A. Propranolol
- B. Amiodarone
- C. Lidocaine
- D. Verapamil
- E. Digoxin (Correct Answer)
Other antiarrhythmic agents Explanation: ***Digoxin***
- The patient's presentation with **heart failure** symptoms (dyspnea, orthopnea, rales, S3 gallop, hepatomegaly) and erratic self-dosing of "some pills" strongly suggests **digoxin toxicity**.
- **Gastrointestinal symptoms** (nausea, vomiting, diarrhea) are common initial signs of digoxin toxicity, and the progression to **ventricular tachycardia** and **ventricular fibrillation** is consistent with severe digitalis-induced arrhythmia.
*Propranolol*
- This is a **beta-blocker** primarily used for hypertension, angina, and arrhythmias.
- While overdose can cause bradycardia, hypotension, and heart block, it typically does not lead to **ventricular tachycardia or fibrillation** as seen in this case.
*Amiodarone*
- This is a **Class III antiarrhythmic** medication with a long half-life, used for various tachyarrhythmias.
- Though it can cause many side effects, including proarrhythmia, it is less likely to present with the classic **GI symptoms** and rapid progression to fatal ventricular arrhythmias seen here, especially in the context of erratic self-dosing and underlying heart failure.
*Lidocaine*
- This is a **Class IB antiarrhythmic** primarily used for ventricular arrhythmias, especially post-myocardial infarction.
- Toxicity typically manifests as **neurological symptoms** (drowsiness, confusion, seizures) and sometimes hypotension or bradycardia, not the wide range of GI and lethal cardiac arrhythmias described.
*Verapamil*
- This is a **calcium channel blocker** used for hypertension, angina, and supraventricular tachycardias.
- Overdose primarily causes **bradycardia, hypotension, and atrioventricular block**, but it is generally not associated with the pronounced GI symptoms or directly triggering ventricular tachycardia/fibrillation like digoxin toxicity.
Other antiarrhythmic agents US Medical PG Question 2: An investigator is comparing the risk of adverse effects among various antiarrhythmic medications. One of the drugs being studied primarily acts by blocking the outward flow of K+ during myocyte repolarization. Further investigation shows that the use of this drug is associated with a lower rate of ventricular tachycardia, ventricular fibrillation, and torsades de pointes when compared to similar drugs. Which of the following drugs is most likely being studied?
- A. Verapamil
- B. Procainamide
- C. Esmolol
- D. Amiodarone (Correct Answer)
- E. Sotalol
Other antiarrhythmic agents Explanation: ***Amiodarone***
- Amiodarone is a **Class III antiarrhythmic drug** that primarily blocks **potassium channels**, thereby prolonging repolarization and the effective refractory period in cardiac myocytes.
- While it has properties of all four Vaughn-Williams classes, its dominant action as a potassium channel blocker makes it highly effective in preventing and treating various arrhythmias, including **ventricular tachycardia (VT)** and **ventricular fibrillation (VF)**, and it has a relatively lower risk of **torsades de pointes (TdP)** compared to other Class III drugs due to its broader ion channel effects.
*Verapamil*
- Verapamil is a **Class IV antiarrhythmic drug (non-dihydropyridine calcium channel blocker)** that primarily blocks **L-type calcium channels**, slowing conduction through the AV node.
- It is mainly used for **supraventricular tachycardias** and rate control in atrial fibrillation, not typically for ventricular arrhythmias like VT/VF.
*Procainamide*
- Procainamide is a **Class IA antiarrhythmic drug** that blocks **sodium channels** and also prolongs repolarization by blocking some potassium channels, but its primary effect is on sodium channels.
- Class IA drugs are known to **increase the QT interval** and carry a significant risk of **torsades de pointes**, making them less favorable for preventing VT/VF with adverse effect concerns.
*Esmolol*
- Esmolol is a **Class II antiarrhythmic drug (beta-blocker)** that primarily acts by **blocking beta-adrenergic receptors**, thereby reducing heart rate, contractility, and AV nodal conduction.
- While useful in some arrhythmias, its main mechanism is not potassium channel blockade, and it is not typically preferred for the direct prevention of VT/VF in situations with concerns about TdP.
*Sotalol*
- Sotalol is a **Class III antiarrhythmic drug** that primarily acts as a **potassium channel blocker**, prolonging the action potential duration and effective refractory period, and also has **beta-blocking properties**.
- While it blocks potassium channels, sotalol carries a **higher risk of torsades de pointes** compared to amiodarone, especially at higher doses and in patients with underlying heart conditions.
Other antiarrhythmic agents US Medical PG Question 3: A 63-year-old man with a history of hypertension and atrial fibrillation is brought into the emergency room and found to have a ventricular tachyarrhythmia. Ibutilide is discontinued and the patient is switched to another drug that also prolongs the QT interval but is associated with a decreased risk of torsades de pointes. Which drug was most likely administered in this patient?
- A. Esmolol
- B. Digoxin
- C. Sotalol
- D. Amiodarone (Correct Answer)
- E. Quinidine
Other antiarrhythmic agents Explanation: ***Amiodarone***
- **Amiodarone** prolongs the **QT interval** but has a lower risk of **torsades de pointes** compared to other **Class III antiarrhythmics** due to its mixed ion channel blocking properties and consistent action potential prolongation.
- It's a broad-spectrum **antiarrhythmic drug** effective for both **atrial** and **ventricular arrhythmias**, making it a good choice for someone with a history of **atrial fibrillation** presenting with **ventricular tachyarrhythmia**.
*Esmolol*
- **Esmolol** is a **beta-blocker** that does not prolong the **QT interval**; it is used to slow heart rate and can be used for rhythm control but not by **QT prolongation**.
- Its primary action is on **beta-1 receptors**, reducing **myocardial contractility** and **heart rate**, primarily used for acute control of **tachyarrhythmias** or **hypertensive emergencies**.
*Digoxin*
- **Digoxin** is a **cardiac glycoside** that does not prolong the **QT interval**; it primarily works by inhibiting the **Na+/K+-ATPase pump** and increasing **vagal tone**.
- It is used to control **ventricular rate** in **atrial fibrillation** and to manage **heart failure**, but it is not an **antiarrhythmic** in the sense of directly terminating **ventricular tachyarrhythmias** by affecting **QT prolongation**.
*Sotalol*
- **Sotalol** is a **beta-blocker** with **Class III antiarrhythmic properties** that prolongs the **QT interval** and has a significant **dose-related risk of torsades de pointes**, particularly at higher doses.
- While it's effective for both **ventricular** and **supraventricular arrhythmias**, its risk of **TdP** is a major concern, making **amiodarone** a safer alternative when **TdP risk** is to be minimized.
*Quinidine*
- **Quinidine** is a **Class IA antiarrhythmic** that significantly prolongs the **QT interval** and is known for a high risk of causing **torsades de pointes**.
- It primarily blocks **fast sodium channels** and also **potassium channels**, contributing to its **proarrhythmic effects** and making it a less favored option when **TdP risk** needs to be decreased.
Other antiarrhythmic agents US Medical PG Question 4: A 77-year-old woman with congestive heart failure is admitted to the hospital for evaluation prior to cardiac transplantation. During her stay at the hospital, the physician prescribes a drug to improve cardiac contractility. The drug works by selectively inhibiting an isoenzyme that is responsible for the degradation of cyclic adenosine monophosphate. Which of the following is the most likely adverse effect of this drug?
- A. Hyperkalemia
- B. QT interval prolongation
- C. Hyperglycemia
- D. Bronchospasm
- E. Hypotension (Correct Answer)
Other antiarrhythmic agents Explanation: ***Hypotension***
- The drug described is likely a **phosphodiesterase-3 inhibitor** (e.g., milrinone), which increases cyclic AMP in cardiac myocytes and vascular smooth muscle cells.
- Increased **cyclic AMP** in vascular smooth muscle leads to **vasodilation**, causing a drop in systemic vascular resistance and subsequently **hypotension**.
*Hyperkalemia*
- **Hyperkalemia** is not a characteristic adverse effect of phosphodiesterase inhibitors. It is associated with drugs like **ACE inhibitors**, **ARBs**, or **aldosterone antagonists**.
- These drugs primarily affect the **renin-angiotensin-aldosterone system** or potassium excretion.
*QT interval prolongation*
- While some **phosphodiesterase inhibitors** can cause **QT prolongation**, it is not the *most likely* adverse effect compared to hypotension, especially in a patient with heart failure.
- Furthermore, **QT prolongation** is a more prominent concern with drugs like **antiarrhythmics** (e.g., amiodarone, sotalol) or certain **antibiotics** (e.g., macrolides).
*Hyperglycemia*
- **Hyperglycemia** is typically associated with drugs that interfere with **insulin secretion** or **insulin sensitivity**, such as **corticosteroids** or some **atypical antipsychotics**.
- Phosphodiesterase inhibitors do not directly cause significant **glucose disturbances**.
*Bronchospasm*
- **Bronchospasm** is a common side effect of **beta-blockers** due to their antagonism of beta-2 adrenergic receptors in the airways.
- Phosphodiesterase inhibitors, by increasing **cyclic AMP**, would theoretically cause **bronchodilation**, not bronchospasm.
Other antiarrhythmic agents US Medical PG Question 5: A group of investigators have conducted a randomized clinical trial to evaluate the efficacy of adding a novel adenosine A1 receptor agonist to the standard anti-epileptic treatment in reducing the frequency of focal seizures. It was found that patients taking the combination regimen (n = 200) had a lower seizure frequency compared to patients taking the standard treatment alone (n = 200; p < 0.01). However, several participants taking the novel drug reported severe drowsiness. The investigators administered a survey to both the combination treatment group and standard treatment group to evaluate whether the drowsiness interfered with daily functioning using a yes or no questionnaire. Results are shown:
Interference with daily functioning Yes (number of patients) No (number of patients)
Combination treatment group 115 85
Standard treatment group 78 122
Which of the following statistical methods would be most appropriate for assessing the statistical significance of these results?
- A. Paired t-test
- B. Unpaired t-test
- C. Chi-square test (Correct Answer)
- D. Analysis of variance
- E. Multiple linear regression
Other antiarrhythmic agents Explanation: ***Chi-square test***
- The **chi-square test** is appropriate for comparing **categorical data** (yes/no responses) between two or more independent groups.
- The data presented (number of patients endorsing "yes" or "no" for interference with daily functioning in two different treatment groups) perfectly fits this scenario.
*Paired t-test*
- A **paired t-test** is used to compare means of two related (or dependent) samples, such as measurements taken on the same subjects before and after an intervention.
- This scenario involves two independent groups, not repeated measures on the same subjects.
*Unpaired t-test*
- An **unpaired t-test** (also known as an independent samples t-test) is used to compare the means of two independent groups for a **continuous outcome variable**.
- Here, the outcome variable ("interference with daily functioning") is categorical (yes/no), not continuous.
*Analysis of variance*
- **ANOVA** is used to compare the means of **three or more independent groups** for a **continuous outcome variable**.
- This study involves only two groups and a categorical outcome, making ANOVA unsuitable.
*Multiple linear regression*
- **Multiple linear regression** is used to model the relationship between a **continuous dependent variable** and two or more independent variables (either continuous or categorical).
- The outcome variable in this case is categorical, not continuous, making linear regression inappropriate.
Other antiarrhythmic agents US Medical PG Question 6: A 62-year-old man is brought to the emergency department because of a 4-hour history of abdominal pain, nausea, vomiting, and confusion. His wife reports that he had blurry vision on the way to the hospital. Two weeks ago, he lost his job and since then has been extremely worried about their financial situation and future. He has congestive heart failure and atrial fibrillation well controlled with combination medical therapy. His temperature is 36.5°C (97.7°F), pulse is 57/min and irregular, respirations are 14/min, and blood pressure is 118/63 mm Hg. The patient is oriented only to person. Serum studies show:
Na+ 138 mEq/L
Cl− 100 mEq/L
K+ 5.3 mEq/L
HCO3− 25 mEq/L
Blood urea nitrogen 14 mg/dL
Creatinine 0.9 mg/dL
An ECG shows premature ventricular beats. The drug most likely responsible for this patient's symptoms has which of the following mechanisms of action?
- A. Blockade of aldosterone receptors
- B. Blockade of beta-adrenergic receptors
- C. Inhibition of Na+/K+-ATPase (Correct Answer)
- D. Inhibition of Na+-K+-2Cl--cotransporters
- E. Inhibition of funny channels
Other antiarrhythmic agents Explanation: ***Inhibition of Na+/K+-ATPase***
- The patient's symptoms (confusion, blurry vision, nausea, vomiting, abdominal pain, arrhythmia, hyperkalemia) are classic for **digoxin toxicity**, which occurs due to the inhibition of the **Na+/K+-ATPase pump**.
- Inhibition of this pump leads to increased intracellular calcium, enhancing cardiac contractility but also causing hyperexcitability and arrhythmias like **premature ventricular beats**.
*Blockade of aldosterone receptors*
- This mechanism is characteristic of **aldosterone antagonists** (e.g., spironolactone, eplerenone) which are often used in heart failure.
- While they can cause hyperkalemia, they typically do not cause the constellation of neurological (confusion, blurry vision) and gastrointestinal symptoms seen in this patient.
*Blockade of beta-adrenergic receptors*
- This is the mechanism of **beta-blockers** (e.g., carvedilol, metoprolol), also commonly used in heart failure and atrial fibrillation.
- Symptoms of beta-blocker overdose usually include bradycardia, hypotension, and bronchospasm, but not the prominent GI or blurry vision symptoms seen here.
*Inhibition of Na+-K+-2Cl--cotransporters*
- This mechanism belongs to **loop diuretics** (e.g., furosemide), often used in congestive heart failure.
- Loop diuretics primarily cause electrolyte imbalances such as hypokalemia and hypomagnesemia, and volume depletion, which does not match the patient's presentation of hyperkalemia and specific digoxin toxicity symptoms.
*Inhibition of funny channels*
- This is the mechanism of action of **ivabradine**, a selective inhibitor of the I_f current in the sinoatrial node, used to reduce heart rate in heart failure.
- While it can cause bradycardia, it is not associated with the severe GI distress, neurological symptoms, or hyperkalemia observed in this patient.
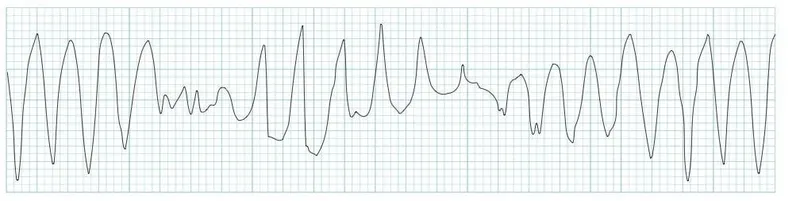
Other antiarrhythmic agents US Medical PG Question 7: A 44-year-old woman presents with palpitations and lightheadedness. She says that symptoms onset 3 days ago and have not improved. She denies any similar episodes in this past. Her blood pressure is 140/90 mm Hg, heart rate is 150/min, respiratory rate is 16/min, and temperature is 36.6℃ (97.9℉). An ECG is performed and the results are shown in the picture. For cardioversion, it is decided to use an antiarrhythmic agent which has a use-dependent effect. Which of the following medications was most probably used?
- A. Diltiazem
- B. Verapamil
- C. Amiodarone
- D. Flecainide (Correct Answer)
- E. Propranolol
Other antiarrhythmic agents Explanation: ***Flecainide***
- Flecainide is a **Class IC antiarrhythmic drug** that exhibits **use-dependent (frequency-dependent) block** of sodium channels, meaning its blocking effect becomes more pronounced at faster heart rates.
- The ECG shows a **narrow complex tachycardia** with a regular rhythm at a rate of 150 bpm, consistent with **supraventricular tachycardia (SVT)**, likely **AVNRT (AV nodal reentrant tachycardia)**.
- Flecainide is effective for **cardioversion of SVT** and maintenance of sinus rhythm in patients without structural heart disease. Its use-dependent sodium channel blockade makes it particularly effective during tachyarrhythmias.
*Diltiazem*
- Diltiazem is a **non-dihydropyridine calcium channel blocker (Class IV antiarrhythmic)** primarily used for rate control in supraventricular tachycardias.
- It does not exhibit significant use-dependent sodium channel block like Class IC antiarrhythmics, and while effective for rate control, it is not the primary choice when use-dependent sodium channel blockade is specifically desired for cardioversion.
*Verapamil*
- Verapamil is a **non-dihydropyridine calcium channel blocker (Class IV antiarrhythmic)** used for rate control and termination of reentrant SVT.
- Like diltiazem, it works through **calcium channel blockade in the AV node**, not through use-dependent sodium channel block, making it less appropriate when this specific mechanism is sought.
*Amiodarone*
- Amiodarone is a **Class III antiarrhythmic drug** (primarily potassium channel blocker) with additional properties of Classes I, II, and IV, providing broad-spectrum action.
- While amiodarone does have some sodium channel blocking effects, its action is **not primarily characterized by use-dependent sodium channel block**. Its main mechanism involves prolonging the action potential duration through potassium channel blockade.
*Propranolol*
- Propranolol is a **non-selective beta-blocker (Class II antiarrhythmic)** that works by decreasing sympathetic activity to the heart, slowing heart rate and AV nodal conduction.
- Beta-blockers are primarily used for **rate control** and do not exhibit use-dependent sodium channel block, which is the key characteristic described in the question.
Other antiarrhythmic agents US Medical PG Question 8: A 78-year-old male comes to the physician’s office for a routine check-up. He complains of increased lower extremity swelling, inability to climb the one flight of stairs in his home, and waking up in the middle of the night 2-3 times gasping for breath. He has had to increase the number of pillows on which he sleeps at night. These symptoms started 9 months ago and have been progressing. The doctor starts him on a medication regimen, one of which changes his Starling curve from A to B as shown in the Figure. Which of the following medications is most consistent with this mechanism of action?
- A. Aspirin
- B. Furosemide
- C. Digoxin (Correct Answer)
- D. Metoprolol
- E. Hydrochlorothiazide
Other antiarrhythmic agents Explanation: ***Digoxin***
- The patient's symptoms (lower extremity swelling, dyspnea on exertion, paroxysmal nocturnal dyspnea) are highly suggestive of **congestive heart failure (CHF)**.
- The Starling curve shifts from **A to B** with the medication, indicating an increase in stroke volume for a given left ventricular end-diastolic pressure, which is characteristic of an **inotropic effect**.
- **Digoxin** is a positive inotropic agent that increases cardiac contractility by inhibiting Na⁺/K⁺-ATPase, leading to increased intracellular calcium.
*Aspirin*
- Aspirin is an antiplatelet agent used for cardiovascular disease prevention, but it does not directly alter the Starling curve in the manner shown by improving cardiac contractility.
- It would not improve the symptoms of heart failure by increasing stroke volume.
*Furosemide*
- Furosemide is a loop diuretic that reduces preload (LV end-diastolic pressure) but does not directly improve cardiac contractility.
- On the Starling curve, a diuretic would shift the operating point to the left, not upward as shown from A to B.
*Metoprolol*
- Metoprolol is a beta-blocker that reduces heart rate and myocardial oxygen demand and can improve mortality in CHF, but it is a **negative inotrope**, reducing contractility acutely.
- It would not cause an immediate upward shift in the Starling curve representing increased stroke volume.
*Hydrochlorothiazide*
- Hydrochlorothiazide is a thiazide diuretic that reduces preload by increasing sodium and water excretion, similar to furosemide but less potent.
- It would cause a leftward shift on the Starling curve, not an upward shift indicating improved contractility.
Other antiarrhythmic agents US Medical PG Question 9: A 51-year-old woman with a history of paroxysmal atrial fibrillation comes to the physician for a follow-up visit. She feels well and wants to discuss pausing her only current medication, flecainide. Her pulse is 75/min and regular, blood pressure is 125/75 mm Hg. Physical examination shows no abnormalities. An ECG shows a PR interval of 180 ms, QRS time of 120 ms, and corrected QT interval of 440 ms. Which of the following ECG changes is most likely to be seen on cardiac stress testing in this patient?
- A. Decreased maximal heart rate
- B. Prolonged QRS complex (Correct Answer)
- C. Shortened PR interval
- D. False-positive ST-segment depression
- E. Prolonged QTc interval
Other antiarrhythmic agents Explanation: ***Prolonged QRS complex***
- **Flecainide** is a class Ic antiarrhythmic that **blocks fast sodium channels** in myocardial cells, slowing conduction in the atria, ventricles, and His-Purkinje system.
- Its effects are **use-dependent**, meaning the drug binds more effectively to channels that are frequently activated (i.e., at higher heart rates), leading to a **further widening of the QRS complex** during exercise.
*Decreased maximal heart rate*
- While some class II antiarrhythmics (beta-blockers) can decrease maximal heart rate, **flecainide** primarily affects cardiac conduction and does not significantly impact heart rate response to stress.
- The ECG does not suggest sinus node dysfunction that would limit heart rate increase with activity.
*Shortened PR interval*
- Flecainide typically **prolongs the PR interval** by slowing conduction through the atrioventricular (AV) node.
- Exercise would likely exacerbate this effect rather than shorten the PR interval.
*False-positive ST-segment depression*
- While wide QRS complexes (as may occur with flecainide-induced conduction slowing) can cause abnormal ST-segment morphology, the **most prominent and characteristic effect** of flecainide during stress testing is **progressive QRS widening** due to use-dependent sodium channel blockade.
- False-positive ST changes are a nonspecific finding and not the hallmark ECG change expected with flecainide during exercise.
*Prolonged QTc interval*
- Flecainide is generally known to **not significantly prolong the QT interval**; in some cases, it may even shorten it due to its effect on action potential duration.
- Other antiarrhythmics like Class III agents (e.g., amiodarone, sotalol) are more commonly associated with QTc prolongation.
Other antiarrhythmic agents US Medical PG Question 10: An 8-year-old boy is brought to the emergency department by his parents because of vomiting, abdominal pain, and blurry vision for the past hour. The parents report that the boy developed these symptoms after he accidentally ingested 2 tablets of his grandfather’s heart failure medication. On physical examination, the child is drowsy, and his pulse is 120/min and irregular. Digoxin toxicity is suspected. A blood sample is immediately sent for analysis and shows a serum digoxin level of 4 ng/mL (therapeutic range: 0.8–2 ng/mL). Which of the following electrolyte abnormalities is most likely to be present in the boy?
- A. Hypermagnesemia
- B. Hypokalemia
- C. Hypercalcemia
- D. Hyperkalemia (Correct Answer)
- E. Hypocalcemia
Other antiarrhythmic agents Explanation: ***Hyperkalemia***
- **Digoxin** inhibits the **Na+/K+-ATPase pump**, leading to an increase in intracellular sodium and a decrease in intracellular potassium.
- The decreased function of the Na+/K+-ATPase pump results in reduced cellular uptake of potassium, causing **elevated extracellular potassium** levels.
*Hypermagnesemia*
- **Magnesium** is not directly affected by digoxin toxicity in a way that would lead to hypermagnesemia; in fact, hypomagnesemia can exacerbate digoxin toxicity.
- High magnesium levels are typically associated with renal failure or excessive intake of magnesium-containing antacids or laxatives.
*Hypokalemia*
- While hypokalemia can **predispose to digoxin toxicity** (by increasing digoxin binding to the Na+/K+-ATPase pump), acute digoxin overdose, as described here, often leads to **hyperkalemia** due to the direct inhibition of the pump's ability to drive potassium into cells.
- The classic association of hypokalemia with digoxin refers more to its role as a risk factor for toxicity, especially with diuretic use, rather than a direct consequence of acute overdose.
*Hypercalcemia*
- **Calcium** levels are not directly altered to hypercalcemia by digoxin toxicity.
- Digoxin's mechanism involves increasing intracellular calcium by promoting calcium influx and inhibiting its efflux via the Na+/Ca2+ exchanger, but this typically does not manifest as measurable serum hypercalcemia.
*Hypocalcemia*
- Digoxin toxicity does not directly cause hypocalcemia.
- Digoxin actually leads to **increased intracellular calcium**, which is responsible for its positive inotropic effect, but this change is primarily intracellular and does not result in systemic hypocalcemia.
More Other antiarrhythmic agents US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.