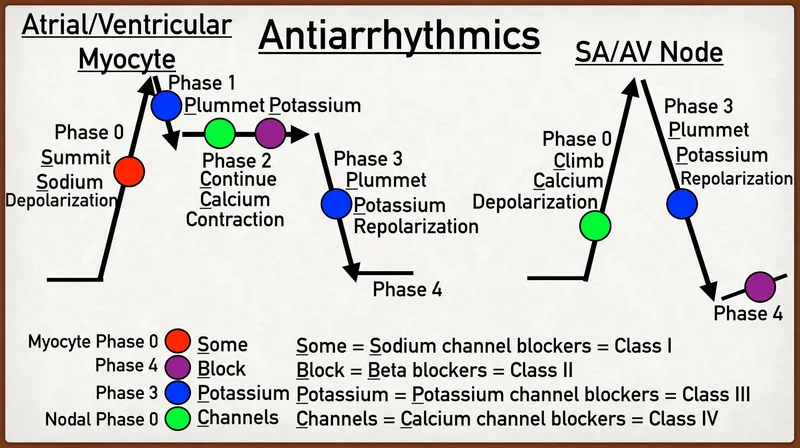
Class IV antiarrhythmics (calcium channel blockers) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Class IV antiarrhythmics (calcium channel blockers). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Class IV antiarrhythmics (calcium channel blockers) US Medical PG Question 1: A 72-year-old man comes to the emergency department because of blurry vision for the past 3 days. He has also had 4 episodes of right-sided headaches over the past month. He has no significant past medical history. His father died of coronary artery disease at the age of 62 years. His temperature is 37.2°C (99°F), pulse is 94/min, and blood pressure is 232/128 mm Hg. Fundoscopy shows right-sided optic disc blurring and retinal hemorrhages. A medication is given immediately. Five minutes later, his pulse is 75/min and blood pressure is 190/105 mm Hg. Which of the following drugs was most likely administered?
- A. Nicardipine
- B. Hydralazine
- C. Nitroprusside
- D. Fenoldopam
- E. Labetalol (Correct Answer)
Class IV antiarrhythmics (calcium channel blockers) Explanation: ***Labetalol***
- This patient presents with **malignant hypertension** given the severely elevated blood pressure (232/128 mm Hg) and signs of **end-organ damage** (blurry vision, optic disc blurring, retinal hemorrhages suggesting hypertensive retinopathy, and new-onset headaches).
- **Labetalol** is a mixed alpha- and beta-blocker commonly used in hypertensive emergencies because of its **rapid onset of action** and ability to effectively lower blood pressure without causing significant reflex tachycardia. The decrease in pulse rate from 94/min to 75/min after administration is consistent with its beta-blocking effects.
*Nicardipine*
- **Nicardipine** is a dihydropyridine calcium channel blocker that primarily causes **vasodilation**, making it effective in hypertensive emergencies.
- While it would lower blood pressure, it typically causes **reflex tachycardia** due to vasodilation, which is not observed in this patient (pulse decreased).
*Hydralazine*
- **Hydralazine** is a direct arterial vasodilator often used in hypertensive emergencies, but it typically causes a more pronounced **reflex tachycardia** than calcium channel blockers.
- Its onset of action can also be less predictable, and its use is generally avoided if there's evidence of **coronary artery disease** due to the risk of increased myocardial oxygen demand.
*Nitroprusside*
- **Nitroprusside** is a powerful balanced arterial and venous vasodilator, leading to a rapid and significant drop in blood pressure.
- It is known for causing **reflex tachycardia** and has a risk of **cyanide toxicity** with prolonged use, making its use in this scenario less ideal given the patient's existing elevated pulse.
*Fenoldopam*
- **Fenoldopam** is a dopamine-1 receptor agonist that causes vasodilation and improves renal blood flow, useful in hypertensive emergencies.
- Like other vasodilators, it can cause **reflex tachycardia** and may lead to increased intraocular pressure, which would be a concern in a patient with acute blurry vision.
Class IV antiarrhythmics (calcium channel blockers) US Medical PG Question 2: A 50-year-old man with a history of atrial fibrillation presents to his cardiologist’s office for a follow-up visit. He recently started treatment with an anti-arrhythmic drug to prevent future recurrences and reports that he has been feeling well and has no complaints. The physical examination shows that the arrhythmia appears to have resolved; however, there is now mild bradycardia. In addition, the electrocardiogram recording shows a slight prolongation of the PR and QT intervals. Which of the following drugs was most likely used to treat this patient?
- A. Metoprolol
- B. Sotalol (Correct Answer)
- C. Propranolol
- D. Verapamil
- E. Carvedilol
Class IV antiarrhythmics (calcium channel blockers) Explanation: ***Sotalol***
- **Sotalol** is a **beta-blocker** and a **Class III antiarrhythmic** drug, meaning it blocks potassium channels.
- This dual action explains the **bradycardia** (beta-blockade) and the **prolongation of the PR and QT intervals** (potassium channel blockade), which are characteristic side effects.
*Metoprolol*
- **Metoprolol** is a **selective beta-1 blocker** (Class II antiarrhythmic) that would cause **bradycardia** and **PR prolongation**, but it does not typically prolong the **QT interval**.
- It primarily affects the heart rate and AV nodal conduction without significant potassium channel blocking properties.
*Propranolol*
- **Propranolol** is a **non-selective beta-blocker** (Class II antiarrhythmic) that would cause **bradycardia** and **PR prolongation**.
- Similar to metoprolol, it does not typically prolong the **QT interval**.
*Verapamil*
- **Verapamil** is a **non-dihydropyridine calcium channel blocker** (Class IV antiarrhythmic) that causes **bradycardia** and **PR prolongation**.
- However, it does not prolong the **QT interval**; instead, it can sometimes shorten it.
*Carvedilol*
- **Carvedilol** is a **non-selective beta-blocker** with **alpha-1 blocking properties** (Class II antiarrhythmic), leading to **bradycardia** and **PR prolongation**.
- It does not have effects on potassium channels that would lead to **QT prolongation**.
Class IV antiarrhythmics (calcium channel blockers) US Medical PG Question 3: A 52-year-old man presents to the emergency department (ED) complaining of palpitations and lightheadedness for the last 30 minutes. He denies feeling pain or discomfort in his chest and is not short of breath. He does not have any known medical problems and does not take any medications regularly. He drinks 4–6 caffeinated drinks a day. The temperature is 36.8°C (98.2°F), the pulse rate is 150/min and slightly irregular, the blood pressure is 144/84 mm Hg, and the respiratory rate is 16/min. A focused examination of the cardiovascular and respiratory systems is unremarkable. An electrocardiogram is performed in the ED and the results are shown in the accompanying image. The ED physician prescribes a calcium channel blocking agent for his condition. Which of the following statements best describes the choice of verapamil over nifedipine in the treatment of this patient?
- A. Verapamil does not have non-specific anti-adrenergic effects, unlike nifedipine.
- B. Verapamil has fewer negative inotropic effects than nifedipine.
- C. Verapamil is more effective in decreasing blood pressure than nifedipine.
- D. Verapamil binds to the α2 subunit of the L-type calcium channel, while nifedipine binds to the α1 subunit of the L-type calcium channel.
- E. Verapamil slows atrioventricular conduction more effectively than nifedipine. (Correct Answer)
Class IV antiarrhythmics (calcium channel blockers) Explanation: ***Verapamil slows atrioventricular conduction more effectively than nifedipine.***
- Verapamil is a **non-dihydropyridine calcium channel blocker** that primarily acts on the **L-type calcium channels** in the heart, particularly in the AV node, slowing conduction and reducing heart rate. This is crucial for managing arrhythmias like the one suggested by the patient's symptoms (palpitations, lightheadedness, irregular pulse of 150/min), which is likely atrial fibrillation or flutter with rapid ventricular response.
- In contrast, nifedipine, a **dihydropyridine calcium channel blocker**, primarily acts on vascular smooth muscle to cause vasodilation, with little direct effect on cardiac conduction.
*Verapamil does not have non-specific anti-adrenergic effects, unlike nifedipine.*
- Neither verapamil nor nifedipine are known for significant anti-adrenergic effects; their primary mechanisms involve calcium channel blockade.
- Dihydropyridines like **nifedipine** can sometimes cause reflex tachycardia due to their vasodilation, which is an indirect adrenergic response, but not a direct anti-adrenergic effect.
*Verapamil has fewer negative inotropic effects than nifedipine.*
- Verapamil, by slowing calcium influx into cardiac myocytes, has more pronounced **negative inotropic effects** (decreases myocardial contractility) compared to nifedipine, which primarily affects peripheral vasculature.
- Nifedipine's effect on contractility is less profound clinically due to its selective action on smooth muscle cells and potential reflex sympathetic activation.
*Verapamil is more effective in decreasing blood pressure than nifedipine.*
- Nifedipine, a dihydropyridine, is generally more potent and preferred for its **vasodilatory effects** and greater efficacy in lowering blood pressure.
- While verapamil also lowers blood pressure, its primary utility in this context is its effect on cardiac rhythm and AV nodal conduction, not its blood pressure-lowering capabilities.
*Verapamil binds to the α2 subunit of the L-type calcium channel, while nifedipine binds to the α1 subunit of the L-type calcium channel.*
- Both verapamil and nifedipine primarily bind to the **α1 subunit** of the L-type calcium channel, though at different binding sites, leading to their distinct pharmacological effects.
- The α2 subunit is accessory and involved in channel trafficking and modulation, not the primary binding site for these drugs' therapeutic action.
Class IV antiarrhythmics (calcium channel blockers) US Medical PG Question 4: An 18-year-old boy is brought to the emergency department by his parents because he suddenly collapsed while playing football. His parents mention that he had complained of dizziness while playing before, but never fainted in the middle of a game. On physical examination, the blood pressure is 130/90 mm Hg, the respirations are 15/min, and the pulse is 110/min. The chest is clear, but a systolic ejection murmur is present. The remainder of the examination revealed no significant findings. An electrocardiogram is ordered, along with an echocardiogram. He is diagnosed with hypertrophic cardiomyopathy and the physician lists all the precautions he must follow. Which of the following drugs will be on the list of contraindicated substances?
- A. Βeta-blockers
- B. Dobutamine
- C. Nitrates (Correct Answer)
- D. Calcium channel blockers
- E. Potassium channel blockers
Class IV antiarrhythmics (calcium channel blockers) Explanation: ***Nitrates***
- **Nitrates** cause **vasodilation**, which decreases **preload** and worsens **left ventricular outflow tract obstruction (LVOTO)** in **hypertrophic cardiomyopathy (HCM)**, potentially leading to syncope or sudden death.
- Reduced preload exacerbates the dynamic obstruction, causing a critical drop in cardiac output.
- **Commonly encountered substances** patients must avoid include nitroglycerin, isosorbide, and **phosphodiesterase-5 inhibitors** (sildenafil, tadalafil) which potentiate nitrate effects.
- This is a critical counseling point for HCM patients in everyday life.
*Beta-blockers*
- **Beta-blockers** are **first-line treatment** for **hypertrophic cardiomyopathy (HCM)** as they reduce heart rate, improve diastolic filling, and decrease contractility, thereby reducing **LVOTO**.
- They alleviate symptoms and reduce the risk of sudden cardiac death in HCM.
*Dobutamine*
- **Dobutamine** is a **beta-1 adrenergic agonist** that increases contractility and heart rate, which would worsen **LVOTO** in HCM.
- While also contraindicated in HCM, dobutamine is only used in **controlled hospital settings** for stress testing or hemodynamic support, not a substance patients encounter in daily life.
- The question focuses on outpatient counseling about substances to avoid in everyday situations.
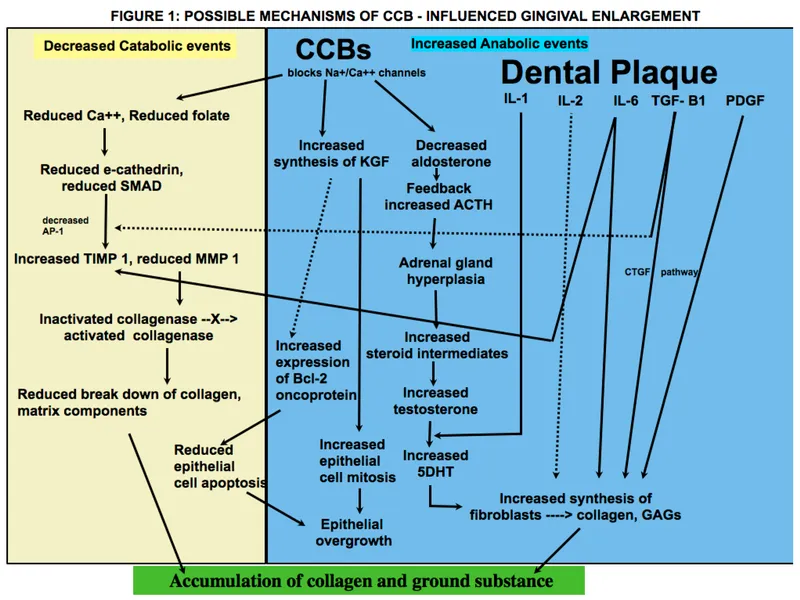
*Calcium channel blockers*
- **Non-dihydropyridine calcium channel blockers** (verapamil, diltiazem) are used in **HCM management**, particularly in patients who cannot tolerate beta-blockers.
- They improve **diastolic function** and reduce **LVOTO** by decreasing contractility and heart rate.
- **Caution:** Dihydropyridines (nifedipine, amlodipine) can worsen obstruction and should be avoided.
*Potassium channel blockers*
- **Antiarrhythmics** like **amiodarone** (potassium channel blocker) are used in **HCM** patients for atrial or ventricular arrhythmias.
- Not contraindicated; therapeutically indicated for rhythm management.
Class IV antiarrhythmics (calcium channel blockers) US Medical PG Question 5: A 44-year-old woman presents with palpitations and lightheadedness. She says that symptoms onset 3 days ago and have not improved. She denies any similar episodes in this past. Her blood pressure is 140/90 mm Hg, heart rate is 150/min, respiratory rate is 16/min, and temperature is 36.6℃ (97.9℉). An ECG is performed and the results are shown in the picture. For cardioversion, it is decided to use an antiarrhythmic agent which has a use-dependent effect. Which of the following medications was most probably used?
- A. Diltiazem
- B. Verapamil
- C. Amiodarone
- D. Flecainide (Correct Answer)
- E. Propranolol
Class IV antiarrhythmics (calcium channel blockers) Explanation: ***Flecainide***
- Flecainide is a **Class IC antiarrhythmic drug** that exhibits **use-dependent (frequency-dependent) block** of sodium channels, meaning its blocking effect becomes more pronounced at faster heart rates.
- The ECG shows a **narrow complex tachycardia** with a regular rhythm at a rate of 150 bpm, consistent with **supraventricular tachycardia (SVT)**, likely **AVNRT (AV nodal reentrant tachycardia)**.
- Flecainide is effective for **cardioversion of SVT** and maintenance of sinus rhythm in patients without structural heart disease. Its use-dependent sodium channel blockade makes it particularly effective during tachyarrhythmias.
*Diltiazem*
- Diltiazem is a **non-dihydropyridine calcium channel blocker (Class IV antiarrhythmic)** primarily used for rate control in supraventricular tachycardias.
- It does not exhibit significant use-dependent sodium channel block like Class IC antiarrhythmics, and while effective for rate control, it is not the primary choice when use-dependent sodium channel blockade is specifically desired for cardioversion.
*Verapamil*
- Verapamil is a **non-dihydropyridine calcium channel blocker (Class IV antiarrhythmic)** used for rate control and termination of reentrant SVT.
- Like diltiazem, it works through **calcium channel blockade in the AV node**, not through use-dependent sodium channel block, making it less appropriate when this specific mechanism is sought.
*Amiodarone*
- Amiodarone is a **Class III antiarrhythmic drug** (primarily potassium channel blocker) with additional properties of Classes I, II, and IV, providing broad-spectrum action.
- While amiodarone does have some sodium channel blocking effects, its action is **not primarily characterized by use-dependent sodium channel block**. Its main mechanism involves prolonging the action potential duration through potassium channel blockade.
*Propranolol*
- Propranolol is a **non-selective beta-blocker (Class II antiarrhythmic)** that works by decreasing sympathetic activity to the heart, slowing heart rate and AV nodal conduction.
- Beta-blockers are primarily used for **rate control** and do not exhibit use-dependent sodium channel block, which is the key characteristic described in the question.
Class IV antiarrhythmics (calcium channel blockers) US Medical PG Question 6: Match the following antiarrhythmic drugs with their mechanism of action:
| Mechanism of action | Drug |
| :-- | :-- |
| 1. Na+ channel blocker | A. Quinidine |
| 2. K+ channel blocker | B. Digoxin |
| 3. Na+K+ ATPase inhibitor | C. Esmolol |
| 4. Beta-blocker | D. Ibutilide |
- A. 1-D, 2-B, 3-A, 4-C
- B. 1-A, 2-D, 3-B, 4-C (Correct Answer)
- C. 1-A, 2-C, 3-D, 4-B
- D. 1-D, 2-C, 3-A, 4-B
Class IV antiarrhythmics (calcium channel blockers) Explanation: ***1-A, 2-D, 3-B, 4-C***
- **Quinidine** is a Class IA antiarrhythmic drug that primarily blocks **sodium channels**, prolonging the action potential duration and refractoriness.
- **Ibutilide** is a Class III antiarrhythmic drug that blocks **potassium channels**, leading to delayed repolarization and increased effective refractory period.
- **Digoxin** inhibits the **Na+/K+ ATPase pump**, increasing intracellular calcium and affecting AV nodal conduction.
- **Esmolol** is a **beta-blocker** (Class II antiarrhythmic) that reduces heart rate and contractility by blocking β1-adrenergic receptors.
*1-A, 2-C, 3-D, 4-B*
- This option incorrectly matches **Esmolol** (a beta-blocker) with **K+ channel blocker** and **Ibutilide** (K+ channel blocker) with **Na+K+ ATPase inhibitor**.
- It also incorrectly matches **Digoxin** (Na+K+ ATPase inhibitor) with **beta-blocker**.
*1-D, 2-C, 3-A, 4-B*
- This option incorrectly matches **Ibutilide** (K+ channel blocker) with **Na+ channel blocker** and incorrectly matches **Quinidine** (Na+ channel blocker) with **Na+K+ ATPase inhibitor**.
- It also incorrectly matches **Digoxin** (Na+K+ ATPase inhibitor) with **beta-blocker**.
*1-D, 2-B, 3-A, 4-C*
- This option incorrectly matches **Ibutilide** (K+ channel blocker) with **Na+ channel blocker** and **Digoxin** (Na+K+ ATPase inhibitor) with **K+ channel blocker**.
- It also incorrectly matches **Quinidine** (Na+ channel blocker) with **Na+K+ ATPase inhibitor**.
Class IV antiarrhythmics (calcium channel blockers) US Medical PG Question 7: A 22-year-old woman presents to the emergency department feeling lightheaded and states that her heart is racing. She does not have a history of any chronic medical conditions. She is a college sophomore and plays club volleyball. Although she feels stressed about her upcoming final exams next week, she limits her caffeine intake to 3 cups of coffee per day to get a good night sleep. She notes that her brother takes medication for some type of heart condition, but she does not know the name of it. Both her parents are alive and well. She denies recent illness, injuries, or use of cigarettes, alcohol, or recreational drugs. The pertinent negatives from the review of systems include an absence of fever, nausea, vomiting, sweating, fatigue, or change in bowel habits. The vital signs include: temperature 36.8°C (98.2°F), heart rate 125/min, respiratory rate 15/min, blood pressure 90/75 mm Hg, and oxygen saturation of 100% on room air. The laboratory results are within normal limits. The ECG is significant for a shortened PR interval and widened QRS. Which of the following medications should the patient avoid in this scenario?
- A. Amlodipine
- B. Procainamide
- C. Diltiazem
- D. Verapamil (Correct Answer)
- E. Metoprolol
Class IV antiarrhythmics (calcium channel blockers) Explanation: ***Verapamil***
- The ECG findings of a **shortened PR interval** and **widened QRS** are characteristic of **Wolff-Parkinson-White (WPW) syndrome**, an accessory pathway that can bypass the AV node.
- Verapamil is a **non-dihydropyridine calcium channel blocker** that blocks the AV node and can paradoxically increase conduction down the accessory pathway in WPW, potentially leading to **ventricular fibrillation** if an atrial tachyarrhythmia is present.
- **Verapamil is the most classically contraindicated medication in WPW syndrome** and is the prototype drug to avoid in this condition.
*Amlodipine*
- Amlodipine is a **dihydropyridine calcium channel blocker** primarily used for hypertension and angina.
- It has minimal effect on the AV node and does not carry the same risk as non-dihydropyridine calcium channel blockers in WPW syndrome.
*Procainamide*
- **Procainamide is a Class Ia antiarrhythmic** that can be used to treat tachyarrhythmias related to WPW syndrome, as it prolongs the refractory period of the accessory pathway.
- It would be a potential **treatment option**, not a medication to avoid, especially for antidromic atrioventricular reentrant tachycardia (AVRT) in WPW.
*Diltiazem*
- Similar to verapamil, diltiazem is a **non-dihydropyridine calcium channel blocker** that blocks the AV node.
- While it carries similar risks to verapamil in WPW syndrome, **verapamil is more classically emphasized** as the prototypical contraindicated medication in medical education and board examinations.
*Metoprolol*
- Metoprolol is a **beta-blocker** that slows conduction through the AV node.
- While beta-blockers are also generally **avoided in WPW syndrome with atrial fibrillation**, **AV nodal blocking calcium channel blockers (especially verapamil) are considered the primary contraindication** due to more pronounced effects on accessory pathway conduction.
Class IV antiarrhythmics (calcium channel blockers) US Medical PG Question 8: An investigator is studying the effects of drugs on the cardiac action potential. Cardiomyocytes are infused with a pharmacological agent and incubated for 5 minutes, after which the action potential is registered on a graph in real time for 2 minutes. Following infusion of the pharmacological agent, the action potential demonstrates a decreased slope of phase 0 depolarization and reduced peak amplitude compared to baseline. These results are most likely caused by an agent that inhibits which of the following?
- A. Opening of voltage-gated sodium channels (Correct Answer)
- B. Opening of voltage-gated potassium channels
- C. Closure of voltage-gated potassium channels
- D. Closure of voltage-gated sodium channels
- E. Opening of voltage-gated calcium channels
Class IV antiarrhythmics (calcium channel blockers) Explanation: ***Opening of voltage-gated sodium channels***
- The **upstroke (phase 0)** of the cardiac action potential, characterized by rapid depolarization, is primarily mediated by the fast influx of **sodium ions** through voltage-gated sodium channels.
- Inhibition of these channels would lead to a slower rate of depolarization, resulting in a **decreased slope** of phase 0 and a **reduced peak amplitude** of the action potential, as seen in the black line.
*Opening of voltage-gated potassium channels*
- The opening of voltage-gated potassium channels primarily contributes to **repolarization (phase 3)**, leading to an outward flow of potassium ions and a decrease in membrane potential.
- Inhibition of these channels would prolong repolarization and the **action potential duration**, which is not depicted as the primary change in the graph.
*Closure of voltage-gated potassium channels*
- An agent causing the closure of voltage-gated potassium channels would lead to a **slower efflux of potassium**, thus **prolonging repolarization** and the action potential duration.
- The graph shows a primary effect on depolarization (phase 0), not on the duration of repolarization.
*Closure of voltage-gated sodium channels*
- **Closure** of voltage-gated sodium channels is a normal part of the action potential cycle, contributing to the inactivation of sodium channels during the plateau phase.
- An agent that *promotes* closure would not cause the observed **slowed depolarization**, as the issue is with the initial opening or function of these channels.
*Opening of voltage-gated calcium channels*
- The opening of voltage-gated calcium channels primarily contributes to the **plateau phase (phase 2)** of the cardiac action potential, allowing a sustained influx of calcium ions.
- Inhibition of these channels would primarily affect the plateau phase duration, potentially **shortening it**, rather than significantly altering the initial upstroke.
Class IV antiarrhythmics (calcium channel blockers) US Medical PG Question 9: A previously healthy 52-year-old woman comes to the physician because of a 3-month history of chest pain on exertion. She takes no medications. Cardiopulmonary examination shows no abnormalities. Cardiac stress ECG shows inducible ST-segment depressions in the precordial leads that coincide with the patient's report of chest pain and resolve upon cessation of exercise. Pharmacotherapy with verapamil is initiated. This drug is most likely to have which of the following sets of effects?
$$$ End-diastolic volume (EDV) %%% Blood pressure (BP) %%% Contractility %%% Heart rate (HR) $$$
- A. No change no change no change no change
- B. ↓ ↓ no change ↑
- C. ↓ ↓ ↓ ↑
- D. ↓ ↓ ↓ no change
- E. ↑ ↓ ↓ ↓ (Correct Answer)
Class IV antiarrhythmics (calcium channel blockers) Explanation: ***↑ ↓ ↓ ↓***
- **Verapamil**, a **non-dihydropyridine calcium channel blocker**, reduces **cardiac contractility**, leading to decreased **heart rate** and **blood pressure**, while increasing **end-diastolic volume**.
- Its therapeutic effect in **exertional angina** is primarily due to reduced myocardial oxygen demand, achieved by decreasing **heart rate**, **contractility** (both leading to reduced work of heart), and **afterload** (due to vasodilation which decreases blood pressure).
*No change no change no change no change*
- This option is incorrect because verapamil has significant **pharmacological effects** on the cardiovascular system.
- Verapamil is prescribed to treat the patient's symptoms, implying a need for **hemodynamic changes**, not stasis.
*↓ ↓ no change ↑*
- Verapamil typically **decreases heart rate** due to its action on the sinoatrial (SA) node, making an increase unlikely.
- While it decreases **blood pressure** and **contractility**, the absence of an effect on heart rate and an increase in heart rate are inconsistent with verapamil's known pharmacology.
*↓ ↓ ↓ ↑*
- This option incorrectly suggests an **increase in heart rate**, whereas verapamil is known to cause a dose-dependent **decrease in heart rate**.
- The other parameters (decreased EDV, BP, contractility) are also not fully aligned with verapamil's effects; EDV tends to increase due to better filling time and reduced contractility.
*↓ ↓ ↓ no change*
- This option suggests a **decrease in EDV**, which is generally incorrect; verapamil tends to allow for **increased ventricular filling** due to a reduced heart rate and prolonged diastole.
- The absence of a change in heart rate is also incorrect, as verapamil is a known **negative chronotropic agent**.
Class IV antiarrhythmics (calcium channel blockers) US Medical PG Question 10: A 72-year-old man with congestive heart failure is brought to the emergency department because of chest pain, shortness of breath, dizziness, and palpitations for 30 minutes. An ECG shows a wide complex tachycardia with a P-wave rate of 105/min, an R-wave rate of 130/min, and no apparent relation between the two. Intravenous pharmacotherapy is initiated with a drug that prolongs the QRS and QT intervals. The patient was most likely treated with which of the following drugs?
- A. Carvedilol
- B. Verapamil
- C. Flecainide
- D. Quinidine (Correct Answer)
- E. Sotalol
Class IV antiarrhythmics (calcium channel blockers) Explanation: **Quinidine**
- Quinidine is a **Class IA antiarrhythmic** that blocks fast sodium channels, prolonging both the **QRS complex** (due to slowed conduction) and the **QT interval** (due to prolonged repolarization).
- The ECG findings of **wide-complex tachycardia** and **AV dissociation** (P-wave rate different from R-wave rate without apparent relation) are consistent with ventricular tachycardia, which Class IA drugs can treat.
*Carvedilol*
- Carvedilol is a **beta-blocker** (Class II antiarrhythmic) that primarily slows heart rate and AV nodal conduction, generally **shortening the QT interval** or having no effect, and would not widen the QRS complex.
- Beta-blockers are typically contraindicated in **decompensated heart failure** and **wide-complex tachycardia** due to their negative inotropic effects and risk of worsening decompensation.
*Verapamil*
- Verapamil is a **non-dihydropyridine calcium channel blocker** (Class IV antiarrhythmic) that mainly slows AV nodal conduction. It would not cause QRS widening and can shorten the QT interval.
- Verapamil is generally contraindicated in **wide-complex tachycardias** of unknown origin as it can precipitate cardiovascular collapse if the arrhythmia is ventricular.
*Flecainide*
- Flecainide is a **Class IC antiarrhythmic** that primarily blocks fast sodium channels, causing significant **QRS widening** but has **minimal effect on the QT interval**, which is contrary to the case description.
- Class IC agents are also generally avoided in patients with **structural heart disease** like congestive heart failure due to increased mortality risk.
*Sotalol*
- Sotalol is a **Class III antiarrhythmic** (beta-blocker with potassium channel blockade) that primarily prolongs the **QT interval** by blocking potassium channels. While it prolongs the QT, it does **not significantly widen the QRS complex**.
- Its beta-blocking effects could exacerbate **decompensated heart failure** in this patient, similar to carvedilol.
More Class IV antiarrhythmics (calcium channel blockers) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.