Class III antiarrhythmics (potassium channel blockers) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Class III antiarrhythmics (potassium channel blockers). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Class III antiarrhythmics (potassium channel blockers) US Medical PG Question 1: A 63-year-old man comes to the physician for a routine health maintenance examination. He feels well. He has a history of hypertension, atrial fibrillation, bipolar disorder, and osteoarthritis of the knees. Current medications include lisinopril, amiodarone, lamotrigine, and acetaminophen. He started amiodarone 6 months ago and switched from lithium to lamotrigine 4 months ago. The patient does not smoke. He drinks 1–4 beers per week. He does not use illicit drugs. Vital signs are within normal limits. Examination shows no abnormalities. Laboratory studies show:
Serum
Na+ 137 mEq/L
K+ 4.2 mEq/L
Cl- 105 mEq/L
HCO3- 24 mEq/L
Urea nitrogen 14 mg/dL
Creatinine 0.9 mg/dL
Alkaline phosphatase 82 U/L
Aspartate aminotransferase (AST) 110 U/L
Alanine aminotransferase (ALT) 115 U/L
Which of the following is the most appropriate next step in management?
- A. Discontinue amiodarone (Correct Answer)
- B. Discontinue acetaminophen
- C. Follow-up laboratory results in 3 months
- D. Follow-up laboratory results in 6 months
- E. Decrease alcohol consumption
Class III antiarrhythmics (potassium channel blockers) Explanation: ***Discontinue amiodarone***
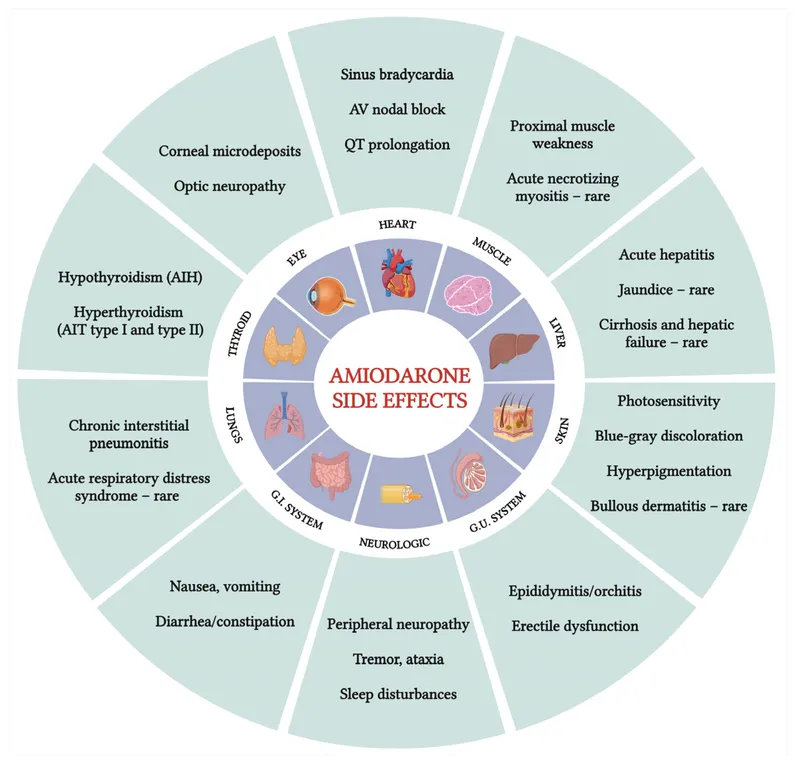
* The patient has elevated **AST** and **ALT** levels, suggestive of **drug-induced liver injury**. Amiodarone is a known cause of **hepatotoxicity**, which can occur even with normal baseline liver function.
* **Amiodarone-induced liver injury** can range from asymptomatic transaminase elevation to **fulminant hepatic failure**; therefore, discontinuing the drug is crucial to prevent further liver damage.
*Discontinue acetaminophen*
* Although **acetaminophen** can cause **hepatotoxicity** at high doses, the patient is likely taking it at therapeutic doses for osteoarthritis, as suggested by its use in routine care and the absence of overdose symptoms.
* The chronic nature of amiodarone use (6 months) and its well-established risk of **liver injury** make it a more probable cause of the elevated transaminases than **therapeutic-dose acetaminophen**.
*Follow-up laboratory results in 3 months*
* The current **liver enzyme elevations** (AST 110 U/L, ALT 115 U/L) are significant and indicate acute liver injury. Waiting 3 months for follow-up without intervention significantly risks further liver damage.
* Prompt identification and removal of the offending agent are necessary to prevent potentially irreversible **hepatic injury**.
*Follow-up laboratory results in 6 months*
* Delaying follow-up for 6 months is an inappropriate and potentially harmful approach given the current enzyme elevations. There is an immediate need to identify and address the cause of **liver injury**.
* Such a delay could lead to progression of **liver damage**, especially if the causative agent (e.g., amiodarone) continues to be administered.
*Decrease alcohol consumption*
* While excessive alcohol consumption can cause **elevated liver enzymes**, the patient’s intake of 1–4 beers per week is considered light to moderate and is unlikely to be the sole cause of these significant elevations.
* The presence of a known **hepatotoxic medication** (amiodarone) alongside the elevated enzymes makes the drug a much more probable cause than the patient's modest alcohol intake.
Class III antiarrhythmics (potassium channel blockers) US Medical PG Question 2: A 70-year-old male immigrant from Asia is brought to the emergency room with complaints of palpitations and light-headedness for 1 hour. The patient was sitting in his chair watching television when he felt his heart racing and became dizzy. He was unable to stand up from his chair because of weakness and light-headedness. His past medical history is notable for mitral stenosis secondary to rheumatic fever as a child. On arrival to the emergency department, the patient's temperature is 99.7°F (37.6°C), blood pressure is 110/55 mmHg, pulse is 140/min, and respirations are 15/min. The patient appears comfortable but anxious. Electrocardiogram shows atrial fibrillation with rapid ventricular response. The patient is started on dofetilide. Which of the following would be expected in this patient’s cardiac action potential as a result of this drug?
- A. Decreased conduction velocity
- B. Increased QT interval (Correct Answer)
- C. Decreased calcium current
- D. Decreased slope of phase 0
- E. Decreased slope of phase 4
Class III antiarrhythmics (potassium channel blockers) Explanation: ***Increased QT interval***
- **Dofetilide** is a **Class III antiarrhythmic** drug that primarily blocks the delayed rectifier **potassium channels (Ik)** in cardiomyocytes.
- Blocking potassium efflux prolongs repolarization, which is reflected as a **prolonged action potential duration (APD)** and a lengthened **QT interval** on the electrocardiogram.
*Decreased conduction velocity*
- This effect is primarily associated with **Class I antiarrhythmic drugs** (e.g., flecainide, procainamide) which block **sodium channels**, thereby slowing the depolarization (Phase 0) and subsequent conduction velocity.
- **Dofetilide**, a Class III agent, does not directly impact sodium channels or significantly decrease conduction velocity.
*Decreased calcium current*
- A decreased calcium current (Phase 2) is characteristic of **Class IV antiarrhythmic drugs** (**calcium channel blockers** like verapamil and diltiazem).
- These drugs primarily act on nodal tissue to slow AV nodal conduction and heart rate, which is not the primary mechanism of action for **dofetilide**.
*Decreased slope of phase 0*
- The slope of **Phase 0 (depolarization)** is determined by the rapid influx of **sodium ions** into the cell.
- A decreased slope of Phase 0 would be expected with **Class I antiarrhythmic drugs** (sodium channel blockers), not with **dofetilide**, which targets potassium channels.
*Decreased slope of phase 4*
- The slope of **Phase 4 (spontaneous depolarization)** in pacemaker cells is primarily influenced by the "funny current" (If) and calcium currents.
- A decreased slope of Phase 4 is characteristic of **beta-blockers** (Class II antiarrhythmics) or **calcium channel blockers** that reduce the rate of spontaneous depolarization in nodal cells, thereby lowering heart rate. **Dofetilide** does not have this primary effect.
Class III antiarrhythmics (potassium channel blockers) US Medical PG Question 3: A 53-year-old man with obesity and heart disease presents to your outpatient clinic with complaints of orthopnea, significant dyspnea on minimal exertion, nausea, vomiting, and diarrhea. He says that his old doctor gave him "some pills" that he takes in varying amounts every morning. Physical exam is significant for a severely displaced point of maximal impulse, bilateral rales in the lower lung fields, an S3 gallop, and hepatomegaly. You decide to perform an EKG (shown in figure A). Suddenly, his rhythm changes to ventricular tachycardia followed by ventricular fibrillation, and he syncopizes and expires despite resuscitative efforts. High levels of which medication are most likely responsible?
- A. Propranolol
- B. Amiodarone
- C. Lidocaine
- D. Verapamil
- E. Digoxin (Correct Answer)
Class III antiarrhythmics (potassium channel blockers) Explanation: ***Digoxin***
- The patient's presentation with **heart failure** symptoms (dyspnea, orthopnea, rales, S3 gallop, hepatomegaly) and erratic self-dosing of "some pills" strongly suggests **digoxin toxicity**.
- **Gastrointestinal symptoms** (nausea, vomiting, diarrhea) are common initial signs of digoxin toxicity, and the progression to **ventricular tachycardia** and **ventricular fibrillation** is consistent with severe digitalis-induced arrhythmia.
*Propranolol*
- This is a **beta-blocker** primarily used for hypertension, angina, and arrhythmias.
- While overdose can cause bradycardia, hypotension, and heart block, it typically does not lead to **ventricular tachycardia or fibrillation** as seen in this case.
*Amiodarone*
- This is a **Class III antiarrhythmic** medication with a long half-life, used for various tachyarrhythmias.
- Though it can cause many side effects, including proarrhythmia, it is less likely to present with the classic **GI symptoms** and rapid progression to fatal ventricular arrhythmias seen here, especially in the context of erratic self-dosing and underlying heart failure.
*Lidocaine*
- This is a **Class IB antiarrhythmic** primarily used for ventricular arrhythmias, especially post-myocardial infarction.
- Toxicity typically manifests as **neurological symptoms** (drowsiness, confusion, seizures) and sometimes hypotension or bradycardia, not the wide range of GI and lethal cardiac arrhythmias described.
*Verapamil*
- This is a **calcium channel blocker** used for hypertension, angina, and supraventricular tachycardias.
- Overdose primarily causes **bradycardia, hypotension, and atrioventricular block**, but it is generally not associated with the pronounced GI symptoms or directly triggering ventricular tachycardia/fibrillation like digoxin toxicity.
Class III antiarrhythmics (potassium channel blockers) US Medical PG Question 4: An investigator is comparing the risk of adverse effects among various antiarrhythmic medications. One of the drugs being studied primarily acts by blocking the outward flow of K+ during myocyte repolarization. Further investigation shows that the use of this drug is associated with a lower rate of ventricular tachycardia, ventricular fibrillation, and torsades de pointes when compared to similar drugs. Which of the following drugs is most likely being studied?
- A. Verapamil
- B. Procainamide
- C. Esmolol
- D. Amiodarone (Correct Answer)
- E. Sotalol
Class III antiarrhythmics (potassium channel blockers) Explanation: ***Amiodarone***
- Amiodarone is a **Class III antiarrhythmic drug** that primarily blocks **potassium channels**, thereby prolonging repolarization and the effective refractory period in cardiac myocytes.
- While it has properties of all four Vaughn-Williams classes, its dominant action as a potassium channel blocker makes it highly effective in preventing and treating various arrhythmias, including **ventricular tachycardia (VT)** and **ventricular fibrillation (VF)**, and it has a relatively lower risk of **torsades de pointes (TdP)** compared to other Class III drugs due to its broader ion channel effects.
*Verapamil*
- Verapamil is a **Class IV antiarrhythmic drug (non-dihydropyridine calcium channel blocker)** that primarily blocks **L-type calcium channels**, slowing conduction through the AV node.
- It is mainly used for **supraventricular tachycardias** and rate control in atrial fibrillation, not typically for ventricular arrhythmias like VT/VF.
*Procainamide*
- Procainamide is a **Class IA antiarrhythmic drug** that blocks **sodium channels** and also prolongs repolarization by blocking some potassium channels, but its primary effect is on sodium channels.
- Class IA drugs are known to **increase the QT interval** and carry a significant risk of **torsades de pointes**, making them less favorable for preventing VT/VF with adverse effect concerns.
*Esmolol*
- Esmolol is a **Class II antiarrhythmic drug (beta-blocker)** that primarily acts by **blocking beta-adrenergic receptors**, thereby reducing heart rate, contractility, and AV nodal conduction.
- While useful in some arrhythmias, its main mechanism is not potassium channel blockade, and it is not typically preferred for the direct prevention of VT/VF in situations with concerns about TdP.
*Sotalol*
- Sotalol is a **Class III antiarrhythmic drug** that primarily acts as a **potassium channel blocker**, prolonging the action potential duration and effective refractory period, and also has **beta-blocking properties**.
- While it blocks potassium channels, sotalol carries a **higher risk of torsades de pointes** compared to amiodarone, especially at higher doses and in patients with underlying heart conditions.
Class III antiarrhythmics (potassium channel blockers) US Medical PG Question 5: A 65-year-old woman comes to the physician because of a 3-month history of progressive shortness of breath and a dry cough. She has also noticed gradual development of facial discoloration. She has coronary artery disease, hypertension, and atrial fibrillation. She does not remember which medications she takes. Her temperature is 37°C (98.6°F), pulse is 90/min, respirations are 18/min, and blood pressure is 150/85 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 95%. Examination shows blue-gray discoloration of the face and both hands. Diffuse inspiratory crackles are heard. An x-ray of the chest shows reticular opacities around the lung periphery and particularly around the lung bases. The most likely cause of this patient's findings is an adverse effect to which of the following medications?
- A. Warfarin
- B. Metoprolol
- C. Procainamide
- D. Amiodarone (Correct Answer)
- E. Lisinopril
Class III antiarrhythmics (potassium channel blockers) Explanation: ***Amiodarone***
- The patient's **progressive shortness of breath**, **dry cough**, and **diffuse inspiratory crackles**, along with **reticular opacities** on chest X-ray, are classic signs of **amiodarone-induced pulmonary fibrosis**.
- The distinctive **blue-gray facial and hand discoloration** is also a well-known side effect of chronic amiodarone use, due to **iodine accumulation in the skin** (amiodarone contains high iodine content).
*Warfarin*
- Warfarin is an anticoagulant used for conditions like atrial fibrillation, but its primary adverse effects include **bleeding** and **skin necrosis**, not pulmonary symptoms or blue-gray discoloration.
- It does not cause interstitial lung disease or changes in skin pigmentation.
*Metoprolol*
- Metoprolol is a beta-blocker used for hypertension and coronary artery disease; common side effects include **bradycardia**, **fatigue**, and **bronchospasm** in susceptible individuals (asthmatics).
- It does not typically cause pulmonary fibrosis or skin discoloration.
*Procainamide*
- Procainamide is an antiarrhythmic, but it is typically used for acute arrhythmias and not long-term management like amiodarone. Its major side effect is a **lupus-like syndrome** and **agranulocytosis**.
- It is not associated with pulmonary fibrosis or skin discoloration as described.
*Lisinopril*
- Lisinopril is an ACE inhibitor used for hypertension and coronary artery disease; common side effects include a **dry cough** (due to bradykinin accumulation) and **angioedema**.
- However, it does not cause pulmonary fibrosis (reticular opacities) or blue-gray skin discoloration.
Class III antiarrhythmics (potassium channel blockers) US Medical PG Question 6: A 50-year-old man with a history of atrial fibrillation presents to his cardiologist’s office for a follow-up visit. He recently started treatment with an anti-arrhythmic drug to prevent future recurrences and reports that he has been feeling well and has no complaints. The physical examination shows that the arrhythmia appears to have resolved; however, there is now mild bradycardia. In addition, the electrocardiogram recording shows a slight prolongation of the PR and QT intervals. Which of the following drugs was most likely used to treat this patient?
- A. Metoprolol
- B. Sotalol (Correct Answer)
- C. Propranolol
- D. Verapamil
- E. Carvedilol
Class III antiarrhythmics (potassium channel blockers) Explanation: ***Sotalol***
- **Sotalol** is a **beta-blocker** and a **Class III antiarrhythmic** drug, meaning it blocks potassium channels.
- This dual action explains the **bradycardia** (beta-blockade) and the **prolongation of the PR and QT intervals** (potassium channel blockade), which are characteristic side effects.
*Metoprolol*
- **Metoprolol** is a **selective beta-1 blocker** (Class II antiarrhythmic) that would cause **bradycardia** and **PR prolongation**, but it does not typically prolong the **QT interval**.
- It primarily affects the heart rate and AV nodal conduction without significant potassium channel blocking properties.
*Propranolol*
- **Propranolol** is a **non-selective beta-blocker** (Class II antiarrhythmic) that would cause **bradycardia** and **PR prolongation**.
- Similar to metoprolol, it does not typically prolong the **QT interval**.
*Verapamil*
- **Verapamil** is a **non-dihydropyridine calcium channel blocker** (Class IV antiarrhythmic) that causes **bradycardia** and **PR prolongation**.
- However, it does not prolong the **QT interval**; instead, it can sometimes shorten it.
*Carvedilol*
- **Carvedilol** is a **non-selective beta-blocker** with **alpha-1 blocking properties** (Class II antiarrhythmic), leading to **bradycardia** and **PR prolongation**.
- It does not have effects on potassium channels that would lead to **QT prolongation**.
Class III antiarrhythmics (potassium channel blockers) US Medical PG Question 7: A 70-year-old man is brought to the emergency department unconscious after a fall. He appears pale and is pulseless. A 12-lead EKG reveals wide, monomorphic sawtooth-like QRS complexes. He undergoes synchronized cardioversion three times at increasing voltage with no effect. Epinephrine is administered with minimal effect. Which drug will minimize his risk of developing multifocal ventricular tachycardia?
- A. Amiodarone (Correct Answer)
- B. Ibutilide
- C. Sotalol
- D. Dofetilide
- E. Procainamide
Class III antiarrhythmics (potassium channel blockers) Explanation: ***Amiodarone***
- **Amiodarone** is a Class III antiarrhythmic, but it has properties of all four Vaughn-Williams classes, making it effective for a wide range of arrhythmias. It is often a first-line agent for both **ventricular tachycardia** and **ventricular fibrillation**.
- Its broad spectrum of action helps to stabilize the myocardial electrical activity and reduce the likelihood of developing additional, polymorphic ventricular arrhythmias like **multifocal ventricular tachycardia**.
*Ibutilide*
- **Ibutilide** is a Class III antiarrhythmic primarily used for the rapid conversion of **atrial fibrillation** and **atrial flutter** to sinus rhythm by selectively prolonging the action potential duration.
- While it prolongs repolarization, it is associated with a risk of **Torsades de Pointes**, a polymorphic ventricular tachycardia, and would not minimize the risk of multifocal ventricular tachycardia, but rather could induce it.
*Sotalol*
- **Sotalol** is a beta-blocker with Class III antiarrhythmic properties, used for both atrial and ventricular arrhythmias.
- Like ibutilide, it also carries a risk of inducing **Torsades de Pointes** due to its action potential prolonging effects, making it unsuitable for minimizing the risk of multifocal ventricular tachycardia in this context.
*Dofetilide*
- **Dofetilide** is a pure Class III antiarrhythmic agent specifically used for the maintenance of sinus rhythm in patients with **atrial fibrillation** or **atrial flutter**.
- It works by blocking the delayed rectifier potassium current, but similar to ibutilide and sotalol, it has a significant risk of **QT prolongation** and **Torsades de Pointes**, thus increasing the risk of polymorphic ventricular tachycardia.
*Procainamide*
- **Procainamide** is a Class IA antiarrhythmic drug that slows conduction and prolongs refractoriness in the atria, ventricles, and accessory pathways. It is used for both supraventricular and ventricular arrhythmias.
- While it can be effective for some ventricular arrhythmias, it is also associated with a risk of **prolonging the QT interval** and inducing **Torsades de Pointes**, especially in patients with structural heart disease or electrolyte imbalances, making it less ideal for minimizing the risk of multifocal ventricular tachycardia compared to amiodarone.
Class III antiarrhythmics (potassium channel blockers) US Medical PG Question 8: An 18-year-old boy is brought to the emergency department by his parents because he suddenly collapsed while playing football. His parents mention that he had complained of dizziness while playing before, but never fainted in the middle of a game. On physical examination, the blood pressure is 130/90 mm Hg, the respirations are 15/min, and the pulse is 110/min. The chest is clear, but a systolic ejection murmur is present. The remainder of the examination revealed no significant findings. An electrocardiogram is ordered, along with an echocardiogram. He is diagnosed with hypertrophic cardiomyopathy and the physician lists all the precautions he must follow. Which of the following drugs will be on the list of contraindicated substances?
- A. Βeta-blockers
- B. Dobutamine
- C. Nitrates (Correct Answer)
- D. Calcium channel blockers
- E. Potassium channel blockers
Class III antiarrhythmics (potassium channel blockers) Explanation: ***Nitrates***
- **Nitrates** cause **vasodilation**, which decreases **preload** and worsens **left ventricular outflow tract obstruction (LVOTO)** in **hypertrophic cardiomyopathy (HCM)**, potentially leading to syncope or sudden death.
- Reduced preload exacerbates the dynamic obstruction, causing a critical drop in cardiac output.
- **Commonly encountered substances** patients must avoid include nitroglycerin, isosorbide, and **phosphodiesterase-5 inhibitors** (sildenafil, tadalafil) which potentiate nitrate effects.
- This is a critical counseling point for HCM patients in everyday life.
*Beta-blockers*
- **Beta-blockers** are **first-line treatment** for **hypertrophic cardiomyopathy (HCM)** as they reduce heart rate, improve diastolic filling, and decrease contractility, thereby reducing **LVOTO**.
- They alleviate symptoms and reduce the risk of sudden cardiac death in HCM.
*Dobutamine*
- **Dobutamine** is a **beta-1 adrenergic agonist** that increases contractility and heart rate, which would worsen **LVOTO** in HCM.
- While also contraindicated in HCM, dobutamine is only used in **controlled hospital settings** for stress testing or hemodynamic support, not a substance patients encounter in daily life.
- The question focuses on outpatient counseling about substances to avoid in everyday situations.
*Calcium channel blockers*
- **Non-dihydropyridine calcium channel blockers** (verapamil, diltiazem) are used in **HCM management**, particularly in patients who cannot tolerate beta-blockers.
- They improve **diastolic function** and reduce **LVOTO** by decreasing contractility and heart rate.
- **Caution:** Dihydropyridines (nifedipine, amlodipine) can worsen obstruction and should be avoided.
*Potassium channel blockers*
- **Antiarrhythmics** like **amiodarone** (potassium channel blocker) are used in **HCM** patients for atrial or ventricular arrhythmias.
- Not contraindicated; therapeutically indicated for rhythm management.
Class III antiarrhythmics (potassium channel blockers) US Medical PG Question 9: Match the following antiarrhythmic drugs with their mechanism of action:
| Mechanism of action | Drug |
| :-- | :-- |
| 1. Na+ channel blocker | A. Quinidine |
| 2. K+ channel blocker | B. Digoxin |
| 3. Na+K+ ATPase inhibitor | C. Esmolol |
| 4. Beta-blocker | D. Ibutilide |
- A. 1-D, 2-B, 3-A, 4-C
- B. 1-A, 2-D, 3-B, 4-C (Correct Answer)
- C. 1-A, 2-C, 3-D, 4-B
- D. 1-D, 2-C, 3-A, 4-B
Class III antiarrhythmics (potassium channel blockers) Explanation: ***1-A, 2-D, 3-B, 4-C***
- **Quinidine** is a Class IA antiarrhythmic drug that primarily blocks **sodium channels**, prolonging the action potential duration and refractoriness.
- **Ibutilide** is a Class III antiarrhythmic drug that blocks **potassium channels**, leading to delayed repolarization and increased effective refractory period.
- **Digoxin** inhibits the **Na+/K+ ATPase pump**, increasing intracellular calcium and affecting AV nodal conduction.
- **Esmolol** is a **beta-blocker** (Class II antiarrhythmic) that reduces heart rate and contractility by blocking β1-adrenergic receptors.
*1-A, 2-C, 3-D, 4-B*
- This option incorrectly matches **Esmolol** (a beta-blocker) with **K+ channel blocker** and **Ibutilide** (K+ channel blocker) with **Na+K+ ATPase inhibitor**.
- It also incorrectly matches **Digoxin** (Na+K+ ATPase inhibitor) with **beta-blocker**.
*1-D, 2-C, 3-A, 4-B*
- This option incorrectly matches **Ibutilide** (K+ channel blocker) with **Na+ channel blocker** and incorrectly matches **Quinidine** (Na+ channel blocker) with **Na+K+ ATPase inhibitor**.
- It also incorrectly matches **Digoxin** (Na+K+ ATPase inhibitor) with **beta-blocker**.
*1-D, 2-B, 3-A, 4-C*
- This option incorrectly matches **Ibutilide** (K+ channel blocker) with **Na+ channel blocker** and **Digoxin** (Na+K+ ATPase inhibitor) with **K+ channel blocker**.
- It also incorrectly matches **Quinidine** (Na+ channel blocker) with **Na+K+ ATPase inhibitor**.
Class III antiarrhythmics (potassium channel blockers) US Medical PG Question 10: A 44-year-old woman presents with palpitations and lightheadedness. She says that symptoms onset 3 days ago and have not improved. She denies any similar episodes in this past. Her blood pressure is 140/90 mm Hg, heart rate is 150/min, respiratory rate is 16/min, and temperature is 36.6℃ (97.9℉). An ECG is performed and the results are shown in the picture. For cardioversion, it is decided to use an antiarrhythmic agent which has a use-dependent effect. Which of the following medications was most probably used?
- A. Diltiazem
- B. Verapamil
- C. Amiodarone
- D. Flecainide (Correct Answer)
- E. Propranolol
Class III antiarrhythmics (potassium channel blockers) Explanation: ***Flecainide***
- Flecainide is a **Class IC antiarrhythmic drug** that exhibits **use-dependent (frequency-dependent) block** of sodium channels, meaning its blocking effect becomes more pronounced at faster heart rates.
- The ECG shows a **narrow complex tachycardia** with a regular rhythm at a rate of 150 bpm, consistent with **supraventricular tachycardia (SVT)**, likely **AVNRT (AV nodal reentrant tachycardia)**.
- Flecainide is effective for **cardioversion of SVT** and maintenance of sinus rhythm in patients without structural heart disease. Its use-dependent sodium channel blockade makes it particularly effective during tachyarrhythmias.
*Diltiazem*
- Diltiazem is a **non-dihydropyridine calcium channel blocker (Class IV antiarrhythmic)** primarily used for rate control in supraventricular tachycardias.
- It does not exhibit significant use-dependent sodium channel block like Class IC antiarrhythmics, and while effective for rate control, it is not the primary choice when use-dependent sodium channel blockade is specifically desired for cardioversion.
*Verapamil*
- Verapamil is a **non-dihydropyridine calcium channel blocker (Class IV antiarrhythmic)** used for rate control and termination of reentrant SVT.
- Like diltiazem, it works through **calcium channel blockade in the AV node**, not through use-dependent sodium channel block, making it less appropriate when this specific mechanism is sought.
*Amiodarone*
- Amiodarone is a **Class III antiarrhythmic drug** (primarily potassium channel blocker) with additional properties of Classes I, II, and IV, providing broad-spectrum action.
- While amiodarone does have some sodium channel blocking effects, its action is **not primarily characterized by use-dependent sodium channel block**. Its main mechanism involves prolonging the action potential duration through potassium channel blockade.
*Propranolol*
- Propranolol is a **non-selective beta-blocker (Class II antiarrhythmic)** that works by decreasing sympathetic activity to the heart, slowing heart rate and AV nodal conduction.
- Beta-blockers are primarily used for **rate control** and do not exhibit use-dependent sodium channel block, which is the key characteristic described in the question.
More Class III antiarrhythmics (potassium channel blockers) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.