Class I antiarrhythmics (sodium channel blockers) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Class I antiarrhythmics (sodium channel blockers). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Class I antiarrhythmics (sodium channel blockers) US Medical PG Question 1: A 64-year-old man presents to his physician for a scheduled follow-up visit. He has chronic left-sided heart failure with systolic dysfunction. His current regular medications include captopril and digoxin, which were started after his last episode of symptomatic heart failure approximately 3 months ago. His last episode of heart failure was accompanied by atrial fibrillation, which followed an alcohol binge over a weekend. Since then he stopped drinking. He reports that he has no current symptoms at rest and is able to perform regular physical exercise without limitation. On physical examination, mild bipedal edema is noted. The physician suggested to him that he should discontinue digoxin and continue captopril and scheduled him for the next follow-up visit. Which of the following statements best justifies the suggestion made by the physician?
- A. Long-term digoxin therapy produces significant survival benefits in patients with heart failure, but at the cost of increased heart failure-related admissions.
- B. Both captopril and digoxin are likely to improve the long-term survival of the patient with heart failure, but digoxin has more severe side effects.
- C. Captopril is likely to improve the long-term survival of the patient with heart failure, unlike digoxin.
- D. Digoxin does not benefit patients with left-sided heart failure in the absence of atrial fibrillation.
- E. Digoxin is useful to treat atrial fibrillation, but does not benefit patients with systolic dysfunction who are in sinus rhythm. (Correct Answer)
Class I antiarrhythmics (sodium channel blockers) Explanation: ***Digoxin is useful to treat atrial fibrillation, but does not benefit patients with systolic dysfunction who are in sinus rhythm.***
- The patient's **atrial fibrillation** was likely triggered by the alcohol binge and has since resolved, suggesting he is now in **sinus rhythm**.
- Digoxin's primary benefit in heart failure with **systolic dysfunction** (HFrEF) is to control ventricular rate in patients with **atrial fibrillation**, but it does not offer survival benefit in HFrEF patients who are in **sinus rhythm** and well-managed with other therapies.
*Long-term digoxin therapy produces significant survival benefits in patients with heart failure, but at the cost of increased heart failure-related admissions.*
- This statement is incorrect; digoxin has been shown to **reduce hospital admissions** for heart failure, but it does **not provide a significant survival benefit** in patients with HFrEF in sinus rhythm.
- The main benefit of digoxin in HFrEF is to improve symptoms and quality of life, alongside reducing hospitalizations, but not prolonging life.
*Both captopril and digoxin are likely to improve the long-term survival of the patient with heart failure, but digoxin has more severe side effects.*
- **Captopril (an ACE inhibitor)** does improve **long-term survival** in heart failure, but **digoxin does not** demonstrably improve survival.
- While digoxin can have side effects, its lack of survival benefit for HFrEF in sinus rhythm is the primary reason for discontinuation, not just side effect severity.
*Captopril is likely to improve the long-term survival of the patient with heart failure, unlike digoxin.*
- This statement is partially correct that **captopril improves survival**, but it does not fully explain the physician's decision to discontinue digoxin.
- The key missing piece is the patient's current **sinus rhythm** and the lack of benefit of digoxin in that specific context for HFrEF.
*Digoxin does not benefit patients with left-sided heart failure in the absence of atrial fibrillation.*
- This statement is nearly correct, but "left-sided heart failure" is broad. It is specifically in patients with **systolic dysfunction (HFrEF)** who are in **sinus rhythm** that digoxin lacks significant benefit beyond symptom control, and does not provide survival benefit.
Class I antiarrhythmics (sodium channel blockers) US Medical PG Question 2: An investigator is comparing the risk of adverse effects among various antiarrhythmic medications. One of the drugs being studied primarily acts by blocking the outward flow of K+ during myocyte repolarization. Further investigation shows that the use of this drug is associated with a lower rate of ventricular tachycardia, ventricular fibrillation, and torsades de pointes when compared to similar drugs. Which of the following drugs is most likely being studied?
- A. Verapamil
- B. Procainamide
- C. Esmolol
- D. Amiodarone (Correct Answer)
- E. Sotalol
Class I antiarrhythmics (sodium channel blockers) Explanation: ***Amiodarone***
- Amiodarone is a **Class III antiarrhythmic drug** that primarily blocks **potassium channels**, thereby prolonging repolarization and the effective refractory period in cardiac myocytes.
- While it has properties of all four Vaughn-Williams classes, its dominant action as a potassium channel blocker makes it highly effective in preventing and treating various arrhythmias, including **ventricular tachycardia (VT)** and **ventricular fibrillation (VF)**, and it has a relatively lower risk of **torsades de pointes (TdP)** compared to other Class III drugs due to its broader ion channel effects.
*Verapamil*
- Verapamil is a **Class IV antiarrhythmic drug (non-dihydropyridine calcium channel blocker)** that primarily blocks **L-type calcium channels**, slowing conduction through the AV node.
- It is mainly used for **supraventricular tachycardias** and rate control in atrial fibrillation, not typically for ventricular arrhythmias like VT/VF.
*Procainamide*
- Procainamide is a **Class IA antiarrhythmic drug** that blocks **sodium channels** and also prolongs repolarization by blocking some potassium channels, but its primary effect is on sodium channels.
- Class IA drugs are known to **increase the QT interval** and carry a significant risk of **torsades de pointes**, making them less favorable for preventing VT/VF with adverse effect concerns.
*Esmolol*
- Esmolol is a **Class II antiarrhythmic drug (beta-blocker)** that primarily acts by **blocking beta-adrenergic receptors**, thereby reducing heart rate, contractility, and AV nodal conduction.
- While useful in some arrhythmias, its main mechanism is not potassium channel blockade, and it is not typically preferred for the direct prevention of VT/VF in situations with concerns about TdP.
*Sotalol*
- Sotalol is a **Class III antiarrhythmic drug** that primarily acts as a **potassium channel blocker**, prolonging the action potential duration and effective refractory period, and also has **beta-blocking properties**.
- While it blocks potassium channels, sotalol carries a **higher risk of torsades de pointes** compared to amiodarone, especially at higher doses and in patients with underlying heart conditions.
Class I antiarrhythmics (sodium channel blockers) US Medical PG Question 3: A 63-year-old man with a history of hypertension and atrial fibrillation is brought into the emergency room and found to have a ventricular tachyarrhythmia. Ibutilide is discontinued and the patient is switched to another drug that also prolongs the QT interval but is associated with a decreased risk of torsades de pointes. Which drug was most likely administered in this patient?
- A. Esmolol
- B. Digoxin
- C. Sotalol
- D. Amiodarone (Correct Answer)
- E. Quinidine
Class I antiarrhythmics (sodium channel blockers) Explanation: ***Amiodarone***
- **Amiodarone** prolongs the **QT interval** but has a lower risk of **torsades de pointes** compared to other **Class III antiarrhythmics** due to its mixed ion channel blocking properties and consistent action potential prolongation.
- It's a broad-spectrum **antiarrhythmic drug** effective for both **atrial** and **ventricular arrhythmias**, making it a good choice for someone with a history of **atrial fibrillation** presenting with **ventricular tachyarrhythmia**.
*Esmolol*
- **Esmolol** is a **beta-blocker** that does not prolong the **QT interval**; it is used to slow heart rate and can be used for rhythm control but not by **QT prolongation**.
- Its primary action is on **beta-1 receptors**, reducing **myocardial contractility** and **heart rate**, primarily used for acute control of **tachyarrhythmias** or **hypertensive emergencies**.
*Digoxin*
- **Digoxin** is a **cardiac glycoside** that does not prolong the **QT interval**; it primarily works by inhibiting the **Na+/K+-ATPase pump** and increasing **vagal tone**.
- It is used to control **ventricular rate** in **atrial fibrillation** and to manage **heart failure**, but it is not an **antiarrhythmic** in the sense of directly terminating **ventricular tachyarrhythmias** by affecting **QT prolongation**.
*Sotalol*
- **Sotalol** is a **beta-blocker** with **Class III antiarrhythmic properties** that prolongs the **QT interval** and has a significant **dose-related risk of torsades de pointes**, particularly at higher doses.
- While it's effective for both **ventricular** and **supraventricular arrhythmias**, its risk of **TdP** is a major concern, making **amiodarone** a safer alternative when **TdP risk** is to be minimized.
*Quinidine*
- **Quinidine** is a **Class IA antiarrhythmic** that significantly prolongs the **QT interval** and is known for a high risk of causing **torsades de pointes**.
- It primarily blocks **fast sodium channels** and also **potassium channels**, contributing to its **proarrhythmic effects** and making it a less favored option when **TdP risk** needs to be decreased.
Class I antiarrhythmics (sodium channel blockers) US Medical PG Question 4: A 70-year-old man is brought to the emergency department unconscious after a fall. He appears pale and is pulseless. A 12-lead EKG reveals wide, monomorphic sawtooth-like QRS complexes. He undergoes synchronized cardioversion three times at increasing voltage with no effect. Epinephrine is administered with minimal effect. Which drug will minimize his risk of developing multifocal ventricular tachycardia?
- A. Amiodarone (Correct Answer)
- B. Ibutilide
- C. Sotalol
- D. Dofetilide
- E. Procainamide
Class I antiarrhythmics (sodium channel blockers) Explanation: ***Amiodarone***
- **Amiodarone** is a Class III antiarrhythmic, but it has properties of all four Vaughn-Williams classes, making it effective for a wide range of arrhythmias. It is often a first-line agent for both **ventricular tachycardia** and **ventricular fibrillation**.
- Its broad spectrum of action helps to stabilize the myocardial electrical activity and reduce the likelihood of developing additional, polymorphic ventricular arrhythmias like **multifocal ventricular tachycardia**.
*Ibutilide*
- **Ibutilide** is a Class III antiarrhythmic primarily used for the rapid conversion of **atrial fibrillation** and **atrial flutter** to sinus rhythm by selectively prolonging the action potential duration.
- While it prolongs repolarization, it is associated with a risk of **Torsades de Pointes**, a polymorphic ventricular tachycardia, and would not minimize the risk of multifocal ventricular tachycardia, but rather could induce it.
*Sotalol*
- **Sotalol** is a beta-blocker with Class III antiarrhythmic properties, used for both atrial and ventricular arrhythmias.
- Like ibutilide, it also carries a risk of inducing **Torsades de Pointes** due to its action potential prolonging effects, making it unsuitable for minimizing the risk of multifocal ventricular tachycardia in this context.
*Dofetilide*
- **Dofetilide** is a pure Class III antiarrhythmic agent specifically used for the maintenance of sinus rhythm in patients with **atrial fibrillation** or **atrial flutter**.
- It works by blocking the delayed rectifier potassium current, but similar to ibutilide and sotalol, it has a significant risk of **QT prolongation** and **Torsades de Pointes**, thus increasing the risk of polymorphic ventricular tachycardia.
*Procainamide*
- **Procainamide** is a Class IA antiarrhythmic drug that slows conduction and prolongs refractoriness in the atria, ventricles, and accessory pathways. It is used for both supraventricular and ventricular arrhythmias.
- While it can be effective for some ventricular arrhythmias, it is also associated with a risk of **prolonging the QT interval** and inducing **Torsades de Pointes**, especially in patients with structural heart disease or electrolyte imbalances, making it less ideal for minimizing the risk of multifocal ventricular tachycardia compared to amiodarone.
Class I antiarrhythmics (sodium channel blockers) US Medical PG Question 5: An 18-year-old boy is brought to the emergency department by his parents because he suddenly collapsed while playing football. His parents mention that he had complained of dizziness while playing before, but never fainted in the middle of a game. On physical examination, the blood pressure is 130/90 mm Hg, the respirations are 15/min, and the pulse is 110/min. The chest is clear, but a systolic ejection murmur is present. The remainder of the examination revealed no significant findings. An electrocardiogram is ordered, along with an echocardiogram. He is diagnosed with hypertrophic cardiomyopathy and the physician lists all the precautions he must follow. Which of the following drugs will be on the list of contraindicated substances?
- A. Βeta-blockers
- B. Dobutamine
- C. Nitrates (Correct Answer)
- D. Calcium channel blockers
- E. Potassium channel blockers
Class I antiarrhythmics (sodium channel blockers) Explanation: ***Nitrates***
- **Nitrates** cause **vasodilation**, which decreases **preload** and worsens **left ventricular outflow tract obstruction (LVOTO)** in **hypertrophic cardiomyopathy (HCM)**, potentially leading to syncope or sudden death.
- Reduced preload exacerbates the dynamic obstruction, causing a critical drop in cardiac output.
- **Commonly encountered substances** patients must avoid include nitroglycerin, isosorbide, and **phosphodiesterase-5 inhibitors** (sildenafil, tadalafil) which potentiate nitrate effects.
- This is a critical counseling point for HCM patients in everyday life.
*Beta-blockers*
- **Beta-blockers** are **first-line treatment** for **hypertrophic cardiomyopathy (HCM)** as they reduce heart rate, improve diastolic filling, and decrease contractility, thereby reducing **LVOTO**.
- They alleviate symptoms and reduce the risk of sudden cardiac death in HCM.
*Dobutamine*
- **Dobutamine** is a **beta-1 adrenergic agonist** that increases contractility and heart rate, which would worsen **LVOTO** in HCM.
- While also contraindicated in HCM, dobutamine is only used in **controlled hospital settings** for stress testing or hemodynamic support, not a substance patients encounter in daily life.
- The question focuses on outpatient counseling about substances to avoid in everyday situations.
*Calcium channel blockers*
- **Non-dihydropyridine calcium channel blockers** (verapamil, diltiazem) are used in **HCM management**, particularly in patients who cannot tolerate beta-blockers.
- They improve **diastolic function** and reduce **LVOTO** by decreasing contractility and heart rate.
- **Caution:** Dihydropyridines (nifedipine, amlodipine) can worsen obstruction and should be avoided.
*Potassium channel blockers*
- **Antiarrhythmics** like **amiodarone** (potassium channel blocker) are used in **HCM** patients for atrial or ventricular arrhythmias.
- Not contraindicated; therapeutically indicated for rhythm management.
Class I antiarrhythmics (sodium channel blockers) US Medical PG Question 6: A 57-year-old woman with a history of diabetes and hypertension accidentally overdoses on antiarrhythmic medication. Upon arrival in the ER, she is administered a drug to counteract the effects of the overdose. Which of the following matches an antiarrhythmic with its correct treatment in overdose?
- A. Propafenone and glucose
- B. Sotalol and norepinephrine
- C. Encainide and epinephrine
- D. Quinidine and insulin
- E. Esmolol and glucagon (Correct Answer)
Class I antiarrhythmics (sodium channel blockers) Explanation: ***Esmolol and glucagon***
- **Esmolol** is a **beta-blocker**, and **glucagon** can be used in **beta-blocker overdose** to activate adenylate cyclase independently of beta-receptors, increasing intracellular cAMP and improving cardiac contractility and heart rate.
- This pair represents a correct antiarrhythmic drug (esmolol) with its appropriate antidote (glucagon) for overdose management.
*Propafenone and glucose*
- **Propafenone** is a **Class IC antiarrhythmic** that can cause **QRS widening**, but **glucose** is not a specific antidote for its overdose.
- Overdose management for propafenone typically involves sodium bicarbonate for QRS widening and supportive care.
*Sotalol and norepinephrine*
- **Sotalol** is a **beta-blocker** with **Class III antiarrhythmic** properties, and **norepinephrine** is a **vasopressor**.
- While norepinephrine might be used for **hypotension** in sotalol overdose, it is not the primary or specific antidote for reversing the beta-blocking effects; **glucagon** would be more appropriate for the cardiac effects.
*Encainide and epinephrine*
- **Encainide** is a **Class IC antiarrhythmic** drug, and its overdose treatment would generally focus on **sodium bicarbonate** for QRS widening and supportive measures.
- **Epinephrine** is a **vasopressor** and might be used for **hypotension** but is not a specific antidote for encainide overdose.
*Quinidine and insulin*
- **Quinidine** is a **Class IA antiarrhythmic** that primarily blocks **sodium channels** and can cause **QT prolongation** and **QRS widening**.
- **Insulin** is primarily used for **hyperglycemia** or in high-dose insulin therapy for certain drug overdoses (e.g., calcium channel blockers or beta-blockers), but it is not a direct antidote for quinidine overdose.
Class I antiarrhythmics (sodium channel blockers) US Medical PG Question 7: Match the following antiarrhythmic drugs with their mechanism of action:
| Mechanism of action | Drug |
| :-- | :-- |
| 1. Na+ channel blocker | A. Quinidine |
| 2. K+ channel blocker | B. Digoxin |
| 3. Na+K+ ATPase inhibitor | C. Esmolol |
| 4. Beta-blocker | D. Ibutilide |
- A. 1-D, 2-B, 3-A, 4-C
- B. 1-A, 2-D, 3-B, 4-C (Correct Answer)
- C. 1-A, 2-C, 3-D, 4-B
- D. 1-D, 2-C, 3-A, 4-B
Class I antiarrhythmics (sodium channel blockers) Explanation: ***1-A, 2-D, 3-B, 4-C***
- **Quinidine** is a Class IA antiarrhythmic drug that primarily blocks **sodium channels**, prolonging the action potential duration and refractoriness.
- **Ibutilide** is a Class III antiarrhythmic drug that blocks **potassium channels**, leading to delayed repolarization and increased effective refractory period.
- **Digoxin** inhibits the **Na+/K+ ATPase pump**, increasing intracellular calcium and affecting AV nodal conduction.
- **Esmolol** is a **beta-blocker** (Class II antiarrhythmic) that reduces heart rate and contractility by blocking β1-adrenergic receptors.
*1-A, 2-C, 3-D, 4-B*
- This option incorrectly matches **Esmolol** (a beta-blocker) with **K+ channel blocker** and **Ibutilide** (K+ channel blocker) with **Na+K+ ATPase inhibitor**.
- It also incorrectly matches **Digoxin** (Na+K+ ATPase inhibitor) with **beta-blocker**.
*1-D, 2-C, 3-A, 4-B*
- This option incorrectly matches **Ibutilide** (K+ channel blocker) with **Na+ channel blocker** and incorrectly matches **Quinidine** (Na+ channel blocker) with **Na+K+ ATPase inhibitor**.
- It also incorrectly matches **Digoxin** (Na+K+ ATPase inhibitor) with **beta-blocker**.
*1-D, 2-B, 3-A, 4-C*
- This option incorrectly matches **Ibutilide** (K+ channel blocker) with **Na+ channel blocker** and **Digoxin** (Na+K+ ATPase inhibitor) with **K+ channel blocker**.
- It also incorrectly matches **Quinidine** (Na+ channel blocker) with **Na+K+ ATPase inhibitor**.
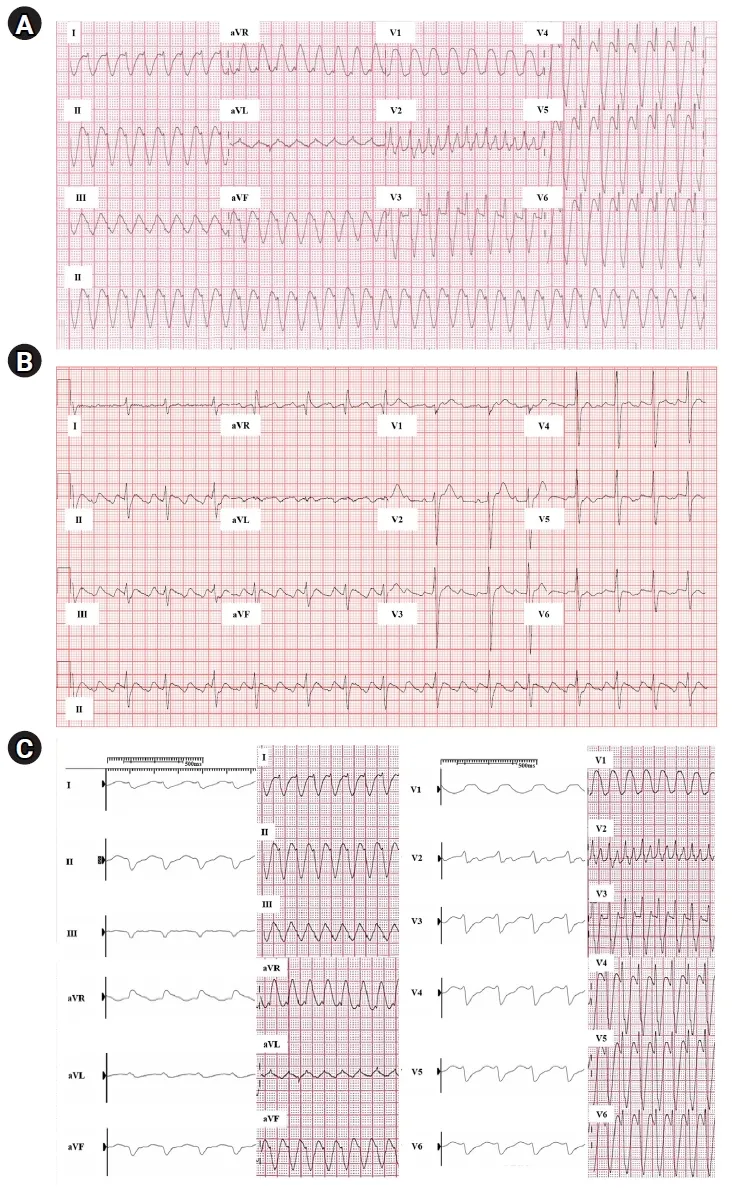
Class I antiarrhythmics (sodium channel blockers) US Medical PG Question 8: A 44-year-old woman presents with palpitations and lightheadedness. She says that symptoms onset 3 days ago and have not improved. She denies any similar episodes in this past. Her blood pressure is 140/90 mm Hg, heart rate is 150/min, respiratory rate is 16/min, and temperature is 36.6℃ (97.9℉). An ECG is performed and the results are shown in the picture. For cardioversion, it is decided to use an antiarrhythmic agent which has a use-dependent effect. Which of the following medications was most probably used?
- A. Diltiazem
- B. Verapamil
- C. Amiodarone
- D. Flecainide (Correct Answer)
- E. Propranolol
Class I antiarrhythmics (sodium channel blockers) Explanation: ***Flecainide***
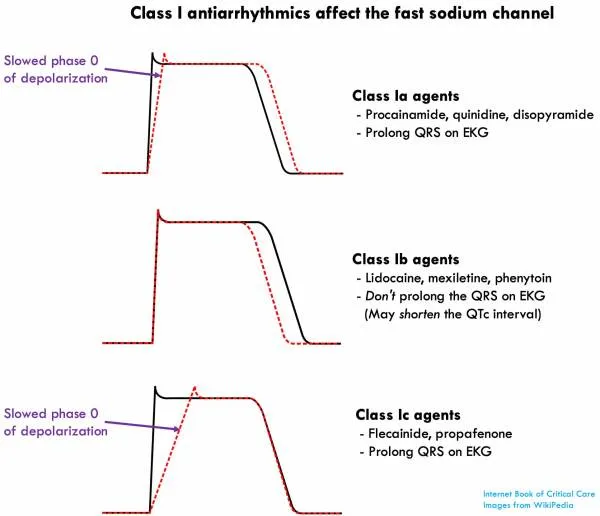
- Flecainide is a **Class IC antiarrhythmic drug** that exhibits **use-dependent (frequency-dependent) block** of sodium channels, meaning its blocking effect becomes more pronounced at faster heart rates.
- The ECG shows a **narrow complex tachycardia** with a regular rhythm at a rate of 150 bpm, consistent with **supraventricular tachycardia (SVT)**, likely **AVNRT (AV nodal reentrant tachycardia)**.
- Flecainide is effective for **cardioversion of SVT** and maintenance of sinus rhythm in patients without structural heart disease. Its use-dependent sodium channel blockade makes it particularly effective during tachyarrhythmias.
*Diltiazem*
- Diltiazem is a **non-dihydropyridine calcium channel blocker (Class IV antiarrhythmic)** primarily used for rate control in supraventricular tachycardias.
- It does not exhibit significant use-dependent sodium channel block like Class IC antiarrhythmics, and while effective for rate control, it is not the primary choice when use-dependent sodium channel blockade is specifically desired for cardioversion.
*Verapamil*
- Verapamil is a **non-dihydropyridine calcium channel blocker (Class IV antiarrhythmic)** used for rate control and termination of reentrant SVT.
- Like diltiazem, it works through **calcium channel blockade in the AV node**, not through use-dependent sodium channel block, making it less appropriate when this specific mechanism is sought.
*Amiodarone*
- Amiodarone is a **Class III antiarrhythmic drug** (primarily potassium channel blocker) with additional properties of Classes I, II, and IV, providing broad-spectrum action.
- While amiodarone does have some sodium channel blocking effects, its action is **not primarily characterized by use-dependent sodium channel block**. Its main mechanism involves prolonging the action potential duration through potassium channel blockade.
*Propranolol*
- Propranolol is a **non-selective beta-blocker (Class II antiarrhythmic)** that works by decreasing sympathetic activity to the heart, slowing heart rate and AV nodal conduction.
- Beta-blockers are primarily used for **rate control** and do not exhibit use-dependent sodium channel block, which is the key characteristic described in the question.
Class I antiarrhythmics (sodium channel blockers) US Medical PG Question 9: An investigator is studying the effects of drugs on the cardiac action potential. Cardiomyocytes are infused with a pharmacological agent and incubated for 5 minutes, after which the action potential is registered on a graph in real time for 2 minutes. Following infusion of the pharmacological agent, the action potential demonstrates a decreased slope of phase 0 depolarization and reduced peak amplitude compared to baseline. These results are most likely caused by an agent that inhibits which of the following?
- A. Opening of voltage-gated sodium channels (Correct Answer)
- B. Opening of voltage-gated potassium channels
- C. Closure of voltage-gated potassium channels
- D. Closure of voltage-gated sodium channels
- E. Opening of voltage-gated calcium channels
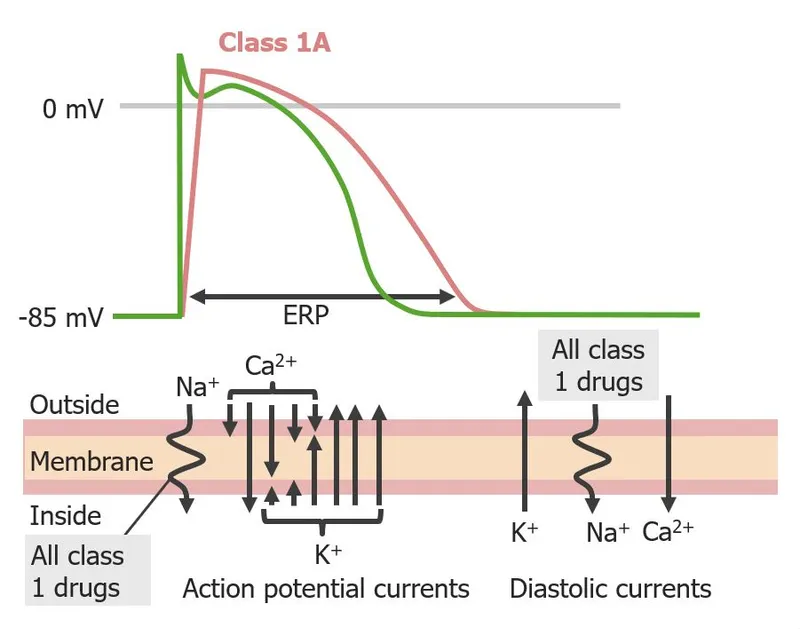
Class I antiarrhythmics (sodium channel blockers) Explanation: ***Opening of voltage-gated sodium channels***
- The **upstroke (phase 0)** of the cardiac action potential, characterized by rapid depolarization, is primarily mediated by the fast influx of **sodium ions** through voltage-gated sodium channels.
- Inhibition of these channels would lead to a slower rate of depolarization, resulting in a **decreased slope** of phase 0 and a **reduced peak amplitude** of the action potential, as seen in the black line.
*Opening of voltage-gated potassium channels*
- The opening of voltage-gated potassium channels primarily contributes to **repolarization (phase 3)**, leading to an outward flow of potassium ions and a decrease in membrane potential.
- Inhibition of these channels would prolong repolarization and the **action potential duration**, which is not depicted as the primary change in the graph.
*Closure of voltage-gated potassium channels*
- An agent causing the closure of voltage-gated potassium channels would lead to a **slower efflux of potassium**, thus **prolonging repolarization** and the action potential duration.
- The graph shows a primary effect on depolarization (phase 0), not on the duration of repolarization.
*Closure of voltage-gated sodium channels*
- **Closure** of voltage-gated sodium channels is a normal part of the action potential cycle, contributing to the inactivation of sodium channels during the plateau phase.
- An agent that *promotes* closure would not cause the observed **slowed depolarization**, as the issue is with the initial opening or function of these channels.
*Opening of voltage-gated calcium channels*
- The opening of voltage-gated calcium channels primarily contributes to the **plateau phase (phase 2)** of the cardiac action potential, allowing a sustained influx of calcium ions.
- Inhibition of these channels would primarily affect the plateau phase duration, potentially **shortening it**, rather than significantly altering the initial upstroke.
Class I antiarrhythmics (sodium channel blockers) US Medical PG Question 10: A 24-year-old man is brought to the emergency department because of violent jerky movements of his arms and legs that began 30 minutes ago. His father reports that the patient has a history of epilepsy. He is not responsive. Physical examination shows alternating tonic jerks and clonic episodes. There is blood in the mouth. Administration of intravenous lorazepam is begun. In addition, treatment with a second drug is started that alters the flow of sodium ions across neuronal membranes. The second agent administered was most likely which of the following drugs?
- A. Lamotrigine
- B. Phenobarbital
- C. Topiramate
- D. Carbamazepine
- E. Fosphenytoin (Correct Answer)
Class I antiarrhythmics (sodium channel blockers) Explanation: ***Fosphenytoin***
- This patient is experiencing **status epilepticus** as evidenced by prolonged tonic-clonic seizures. **Lorazepam** is the first-line short-acting benzodiazepine for acute seizure termination, but a second, longer-acting antiepileptic drug is needed for maintenance.
- **Fosphenytoin** is a prodrug of **phenytoin** that can be administered intravenously; **phenytoin** works by blocking **voltage-sensitive sodium channels**, thereby altering the flow of sodium ions and stabilizing neuronal membranes.
*Lamotrigine*
- While **lamotrigine** does block voltage-gated sodium channels, it is primarily used for **partial seizures** and **generalized tonic-clonic seizures** as a maintenance therapy, not typically as an acute treatment for status epilepticus.
- It requires **slow titration** due to the risk of severe skin reactions (e.g., Stevens-Johnson syndrome), making it unsuitable for immediate use in status epilepticus.
*Phenobarbital*
- **Phenobarbital** is an antiepileptic drug that enhances **GABAergic neurotransmission**, leading to neuronal hyperpolarization and reduced excitability. It is a very effective and older anticonvulsant.
- Although it can be used for status epilepticus, it acts primarily on GABA receptors, not directly on **sodium ion channels** as described in the question.
*Topiramate*
- **Topiramate** has multiple mechanisms of action, including blocking voltage-gated sodium channels and enhancing GABA activity, but it is typically used as a **maintenance therapy** for various seizure types.
- It is not a first-line agent for acute management of **status epilepticus** and its primary mechanism mentioned isn't restricted to sodium channel modulation as explicitly as phenytoin.
*Carbamazepine*
- **Carbamazepine** is a sodium channel blocker, similar to phenytoin, and is effective for **partial** and **tonic-clonic seizures**.
- However, it is primarily an **oral medication** and its slow absorption makes it inappropriate for acute intravenous treatment of status epilepticus.
More Class I antiarrhythmics (sodium channel blockers) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.