Antiarrhythmic classification and mechanisms US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Antiarrhythmic classification and mechanisms. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Antiarrhythmic classification and mechanisms US Medical PG Question 1: A molecular biologist is studying the roles of different types of ion channels regulating cardiac excitation. He identifies a voltage-gated calcium channel in the sinoatrial node, which is also present throughout the myocardium. The channel is activated at ~ -40 mV of membrane potential, undergoes voltage-dependent inactivation, and is highly sensitive to nifedipine. Which of the following phases of the action potential in the sinoatrial node is primarily mediated by ion currents through the channel that the molecular biologist is studying?
- A. Phase 2
- B. Phase 3
- C. Phase 1
- D. Phase 4
- E. Phase 0 (Correct Answer)
Antiarrhythmic classification and mechanisms Explanation: ***Phase 0***
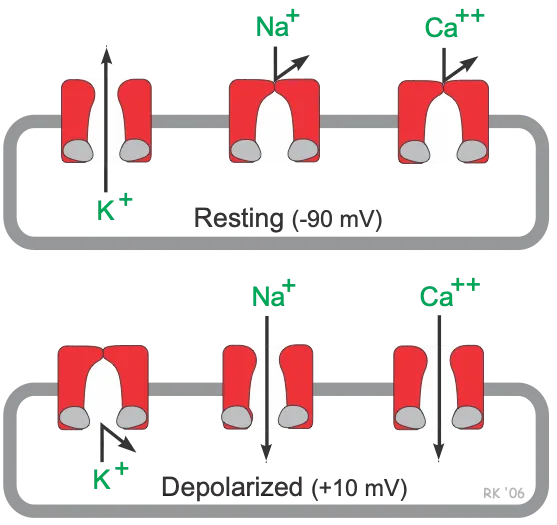
- The description of the channel (**activated at -40 mV**, **voltage-dependent inactivation**, sensitive to **nifedipine**) points to an **L-type calcium channel**.
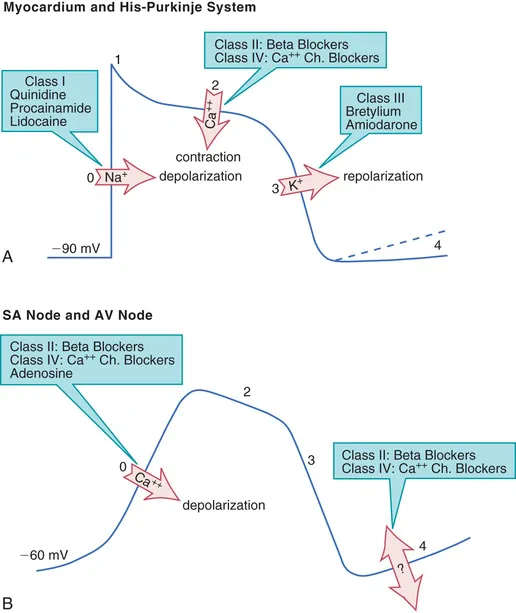
- In the **sinoatrial node**, **L-type calcium channels** are primarily responsible for the **Phase 0 depolarization** (upstroke) of the action potential.
*Phase 2*
- In **myocardial cells**, **Phase 2** (plateau phase) is primarily mediated by **L-type calcium channels**, but the question refers to the **sinoatrial node action potential**.
- **Sinoatrial node cells** typically lack a distinct **Phase 2** plateau, distinguishing them from ventricular myocytes.
*Phase 3*
- **Phase 3** (repolarization) in the **sinoatrial node** is primarily mediated by the **efflux of potassium ions** through various **potassium channels**.
- The described channel, being a **calcium channel**, would contribute to depolarization rather than repolarization.
*Phase 1*
- **Phase 1** (initial repolarization) is characteristic of **ventricular myocytes** and is mediated by a transient outward **potassium current (Ito)**.
- The **sinoatrial node** action potential typically lacks a distinct **Phase 1**, as it does not have this rapid initial repolarization.
*Phase 4*
- **Phase 4** (spontaneous depolarization) in the **sinoatrial node** is primarily driven by the "funny" current (**If**, carried by **HCN channels**) and a gradually increasing **calcium current** (mainly through **T-type calcium channels**), leading to the threshold for **Phase 0**.
- While L-type channels contribute to reaching the threshold, their primary role is the rapid depolarization of **Phase 0**.
Antiarrhythmic classification and mechanisms US Medical PG Question 2: A 54-year-old man comes to the emergency department because of episodic palpitations for the past 12 hours. He has no chest pain. He has coronary artery disease and type 2 diabetes mellitus. His current medications include aspirin, insulin, and atorvastatin. His pulse is 155/min and blood pressure is 116/77 mm Hg. Physical examination shows no abnormalities. An ECG shows monomorphic ventricular tachycardia. An amiodarone bolus and infusion is given, and the ventricular tachycardia converts to normal sinus rhythm. He is discharged home with oral amiodarone. Which of the following is the most likely adverse effect associated with long-term use of this medication?
- A. Angle-closure glaucoma
- B. Hepatic adenoma
- C. Shortened QT interval on ECG
- D. Progressive multifocal leukoencephalopathy
- E. Chronic interstitial pneumonitis (Correct Answer)
Antiarrhythmic classification and mechanisms Explanation: ***Chronic interstitial pneumonitis***
- **Amiodarone** is known to cause several dose-dependent adverse effects, including **pulmonary toxicity** in the form of **interstitial pneumonitis** or fibrosis.
- This adverse effect can manifest as progressive dyspnea, cough, and infiltrates on chest imaging, requiring careful monitoring during long-term use.
*Angle-closure glaucoma*
- While some medications can cause **angle-closure glaucoma**, it is **not a classic or common adverse effect of amiodarone**.
- **Topiramate** and **sulfonamides** are more commonly associated with acute angle-closure glaucoma.
*Hepatic adenoma*
- **Hepatic adenomas** are typically associated with **oral contraceptive use** and sometimes **anabolic steroid use**, not amiodarone.
- Amiodarone can cause **hepatic toxicity** (elevated transaminases, hepatitis), but not specifically hepatic adenoma.
*Shortened QT interval on ECG*
- **Amiodarone** is a Class III antiarrhythmic drug that **prolongs the QT interval** by blocking potassium channels, which is its mechanism of action for suppressing arrhythmias.
- Therefore, a shortened QT interval is the **opposite of what would be expected with amiodarone use**.
*Progressive multifocal leukoencephalopathy*
- **Progressive multifocal leukoencephalopathy (PML)** is a rare, severe opportunistic infection of the brain caused by the **JC virus**, typically seen in immunocompromised individuals.
- It is **not an adverse effect of amiodarone**; drugs like natalizumab or rituximab, which affect the immune system, are associated with PML.
Antiarrhythmic classification and mechanisms US Medical PG Question 3: A 53-year-old man with obesity and heart disease presents to your outpatient clinic with complaints of orthopnea, significant dyspnea on minimal exertion, nausea, vomiting, and diarrhea. He says that his old doctor gave him "some pills" that he takes in varying amounts every morning. Physical exam is significant for a severely displaced point of maximal impulse, bilateral rales in the lower lung fields, an S3 gallop, and hepatomegaly. You decide to perform an EKG (shown in figure A). Suddenly, his rhythm changes to ventricular tachycardia followed by ventricular fibrillation, and he syncopizes and expires despite resuscitative efforts. High levels of which medication are most likely responsible?
- A. Propranolol
- B. Amiodarone
- C. Lidocaine
- D. Verapamil
- E. Digoxin (Correct Answer)
Antiarrhythmic classification and mechanisms Explanation: ***Digoxin***
- The patient's presentation with **heart failure** symptoms (dyspnea, orthopnea, rales, S3 gallop, hepatomegaly) and erratic self-dosing of "some pills" strongly suggests **digoxin toxicity**.
- **Gastrointestinal symptoms** (nausea, vomiting, diarrhea) are common initial signs of digoxin toxicity, and the progression to **ventricular tachycardia** and **ventricular fibrillation** is consistent with severe digitalis-induced arrhythmia.
*Propranolol*
- This is a **beta-blocker** primarily used for hypertension, angina, and arrhythmias.
- While overdose can cause bradycardia, hypotension, and heart block, it typically does not lead to **ventricular tachycardia or fibrillation** as seen in this case.
*Amiodarone*
- This is a **Class III antiarrhythmic** medication with a long half-life, used for various tachyarrhythmias.
- Though it can cause many side effects, including proarrhythmia, it is less likely to present with the classic **GI symptoms** and rapid progression to fatal ventricular arrhythmias seen here, especially in the context of erratic self-dosing and underlying heart failure.
*Lidocaine*
- This is a **Class IB antiarrhythmic** primarily used for ventricular arrhythmias, especially post-myocardial infarction.
- Toxicity typically manifests as **neurological symptoms** (drowsiness, confusion, seizures) and sometimes hypotension or bradycardia, not the wide range of GI and lethal cardiac arrhythmias described.
*Verapamil*
- This is a **calcium channel blocker** used for hypertension, angina, and supraventricular tachycardias.
- Overdose primarily causes **bradycardia, hypotension, and atrioventricular block**, but it is generally not associated with the pronounced GI symptoms or directly triggering ventricular tachycardia/fibrillation like digoxin toxicity.
Antiarrhythmic classification and mechanisms US Medical PG Question 4: An investigator is comparing the risk of adverse effects among various antiarrhythmic medications. One of the drugs being studied primarily acts by blocking the outward flow of K+ during myocyte repolarization. Further investigation shows that the use of this drug is associated with a lower rate of ventricular tachycardia, ventricular fibrillation, and torsades de pointes when compared to similar drugs. Which of the following drugs is most likely being studied?
- A. Verapamil
- B. Procainamide
- C. Esmolol
- D. Amiodarone (Correct Answer)
- E. Sotalol
Antiarrhythmic classification and mechanisms Explanation: ***Amiodarone***
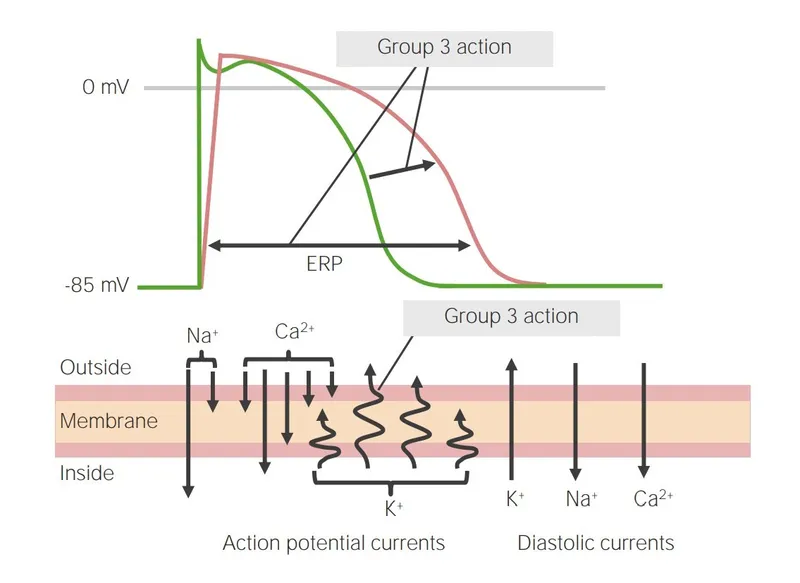
- Amiodarone is a **Class III antiarrhythmic drug** that primarily blocks **potassium channels**, thereby prolonging repolarization and the effective refractory period in cardiac myocytes.
- While it has properties of all four Vaughn-Williams classes, its dominant action as a potassium channel blocker makes it highly effective in preventing and treating various arrhythmias, including **ventricular tachycardia (VT)** and **ventricular fibrillation (VF)**, and it has a relatively lower risk of **torsades de pointes (TdP)** compared to other Class III drugs due to its broader ion channel effects.
*Verapamil*
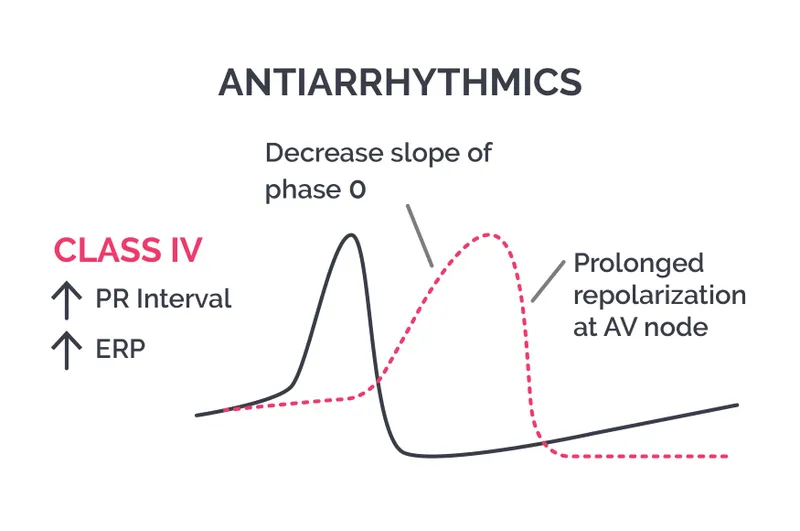
- Verapamil is a **Class IV antiarrhythmic drug (non-dihydropyridine calcium channel blocker)** that primarily blocks **L-type calcium channels**, slowing conduction through the AV node.
- It is mainly used for **supraventricular tachycardias** and rate control in atrial fibrillation, not typically for ventricular arrhythmias like VT/VF.
*Procainamide*
- Procainamide is a **Class IA antiarrhythmic drug** that blocks **sodium channels** and also prolongs repolarization by blocking some potassium channels, but its primary effect is on sodium channels.
- Class IA drugs are known to **increase the QT interval** and carry a significant risk of **torsades de pointes**, making them less favorable for preventing VT/VF with adverse effect concerns.
*Esmolol*
- Esmolol is a **Class II antiarrhythmic drug (beta-blocker)** that primarily acts by **blocking beta-adrenergic receptors**, thereby reducing heart rate, contractility, and AV nodal conduction.
- While useful in some arrhythmias, its main mechanism is not potassium channel blockade, and it is not typically preferred for the direct prevention of VT/VF in situations with concerns about TdP.
*Sotalol*
- Sotalol is a **Class III antiarrhythmic drug** that primarily acts as a **potassium channel blocker**, prolonging the action potential duration and effective refractory period, and also has **beta-blocking properties**.
- While it blocks potassium channels, sotalol carries a **higher risk of torsades de pointes** compared to amiodarone, especially at higher doses and in patients with underlying heart conditions.
Antiarrhythmic classification and mechanisms US Medical PG Question 5: A 26-year-old healthy woman presents with lightheadedness, palpitations, and sweating, which started suddenly after she was frightened by her neighbor’s dog. The patient’s blood pressure is 135/80 mm Hg, the heart rate is 150/min, the respiratory rate is 15/min, and the temperature is 36.6℃ (97.9℉). Her ECG is shown in the exhibit. What is the preferred agent for pharmacologic management of this condition?
- A. Metoprolol
- B. Amiodarone
- C. Propafenone
- D. Adenosine (Correct Answer)
- E. Verapamil
Antiarrhythmic classification and mechanisms Explanation: ***Adenosine***
- The ECG shows a **narrow complex tachycardia** with a regular rhythm and no visible P waves, consistent with **paroxysmal supraventricular tachycardia (PSVT)**, likely AVNRT.
- **Adenosine** is the preferred agent for acute termination of stable PSVT due to its ability to transiently block the **AV node**.
*Metoprolol*
- **Beta-blockers** like metoprolol can be used for rate control or prevention of PSVT, but they are not the first-line agent for acute termination due to a slower onset of action compared to adenosine.
- While metoprolol can reduce heart rate, its efficacy in acutely converting PSVT to sinus rhythm is less predictable than adenosine's.
*Amiodarone*
- **Amiodarone** is primarily used for the treatment of **ventricular arrhythmias** and certain types of refractory supraventricular tachycardias, but it is not the first-line treatment for stable PSVT.
- Its use for PSVT is generally reserved for cases unresponsive to adenosine or other first-line agents, or in patients with structural heart disease, due to its significant side effect profile and slower onset.
*Propafenone*
- **Propafenone** is a Class Ic antiarrhythmic drug used for the maintenance of sinus rhythm in patients with atrial fibrillation or flutter, and for some supraventricular tachycardias.
- It is not typically the first-line agent for acute termination of stable PSVT due to its proarrhythmic potential and slower onset of action compared to adenosine.
*Verapamil*
- **Verapamil**, a non-dihydropyridine calcium channel blocker, is an alternative to adenosine for acute termination of PSVT, especially in patients where adenosine is contraindicated or ineffective.
- However, adenosine is generally preferred as the first-line agent for hemodynamically stable PSVT due to its very rapid onset and short duration of action.
Antiarrhythmic classification and mechanisms US Medical PG Question 6: A 63-year-old man with a history of hypertension and atrial fibrillation is brought into the emergency room and found to have a ventricular tachyarrhythmia. Ibutilide is discontinued and the patient is switched to another drug that also prolongs the QT interval but is associated with a decreased risk of torsades de pointes. Which drug was most likely administered in this patient?
- A. Esmolol
- B. Digoxin
- C. Sotalol
- D. Amiodarone (Correct Answer)
- E. Quinidine
Antiarrhythmic classification and mechanisms Explanation: ***Amiodarone***
- **Amiodarone** prolongs the **QT interval** but has a lower risk of **torsades de pointes** compared to other **Class III antiarrhythmics** due to its mixed ion channel blocking properties and consistent action potential prolongation.
- It's a broad-spectrum **antiarrhythmic drug** effective for both **atrial** and **ventricular arrhythmias**, making it a good choice for someone with a history of **atrial fibrillation** presenting with **ventricular tachyarrhythmia**.
*Esmolol*
- **Esmolol** is a **beta-blocker** that does not prolong the **QT interval**; it is used to slow heart rate and can be used for rhythm control but not by **QT prolongation**.
- Its primary action is on **beta-1 receptors**, reducing **myocardial contractility** and **heart rate**, primarily used for acute control of **tachyarrhythmias** or **hypertensive emergencies**.
*Digoxin*
- **Digoxin** is a **cardiac glycoside** that does not prolong the **QT interval**; it primarily works by inhibiting the **Na+/K+-ATPase pump** and increasing **vagal tone**.
- It is used to control **ventricular rate** in **atrial fibrillation** and to manage **heart failure**, but it is not an **antiarrhythmic** in the sense of directly terminating **ventricular tachyarrhythmias** by affecting **QT prolongation**.
*Sotalol*
- **Sotalol** is a **beta-blocker** with **Class III antiarrhythmic properties** that prolongs the **QT interval** and has a significant **dose-related risk of torsades de pointes**, particularly at higher doses.
- While it's effective for both **ventricular** and **supraventricular arrhythmias**, its risk of **TdP** is a major concern, making **amiodarone** a safer alternative when **TdP risk** is to be minimized.
*Quinidine*
- **Quinidine** is a **Class IA antiarrhythmic** that significantly prolongs the **QT interval** and is known for a high risk of causing **torsades de pointes**.
- It primarily blocks **fast sodium channels** and also **potassium channels**, contributing to its **proarrhythmic effects** and making it a less favored option when **TdP risk** needs to be decreased.
Antiarrhythmic classification and mechanisms US Medical PG Question 7: A 52-year-old man presents to the emergency department (ED) complaining of palpitations and lightheadedness for the last 30 minutes. He denies feeling pain or discomfort in his chest and is not short of breath. He does not have any known medical problems and does not take any medications regularly. He drinks 4–6 caffeinated drinks a day. The temperature is 36.8°C (98.2°F), the pulse rate is 150/min and slightly irregular, the blood pressure is 144/84 mm Hg, and the respiratory rate is 16/min. A focused examination of the cardiovascular and respiratory systems is unremarkable. An electrocardiogram is performed in the ED and the results are shown in the accompanying image. The ED physician prescribes a calcium channel blocking agent for his condition. Which of the following statements best describes the choice of verapamil over nifedipine in the treatment of this patient?
- A. Verapamil does not have non-specific anti-adrenergic effects, unlike nifedipine.
- B. Verapamil has fewer negative inotropic effects than nifedipine.
- C. Verapamil is more effective in decreasing blood pressure than nifedipine.
- D. Verapamil binds to the α2 subunit of the L-type calcium channel, while nifedipine binds to the α1 subunit of the L-type calcium channel.
- E. Verapamil slows atrioventricular conduction more effectively than nifedipine. (Correct Answer)
Antiarrhythmic classification and mechanisms Explanation: ***Verapamil slows atrioventricular conduction more effectively than nifedipine.***
- Verapamil is a **non-dihydropyridine calcium channel blocker** that primarily acts on the **L-type calcium channels** in the heart, particularly in the AV node, slowing conduction and reducing heart rate. This is crucial for managing arrhythmias like the one suggested by the patient's symptoms (palpitations, lightheadedness, irregular pulse of 150/min), which is likely atrial fibrillation or flutter with rapid ventricular response.
- In contrast, nifedipine, a **dihydropyridine calcium channel blocker**, primarily acts on vascular smooth muscle to cause vasodilation, with little direct effect on cardiac conduction.
*Verapamil does not have non-specific anti-adrenergic effects, unlike nifedipine.*
- Neither verapamil nor nifedipine are known for significant anti-adrenergic effects; their primary mechanisms involve calcium channel blockade.
- Dihydropyridines like **nifedipine** can sometimes cause reflex tachycardia due to their vasodilation, which is an indirect adrenergic response, but not a direct anti-adrenergic effect.
*Verapamil has fewer negative inotropic effects than nifedipine.*
- Verapamil, by slowing calcium influx into cardiac myocytes, has more pronounced **negative inotropic effects** (decreases myocardial contractility) compared to nifedipine, which primarily affects peripheral vasculature.
- Nifedipine's effect on contractility is less profound clinically due to its selective action on smooth muscle cells and potential reflex sympathetic activation.
*Verapamil is more effective in decreasing blood pressure than nifedipine.*
- Nifedipine, a dihydropyridine, is generally more potent and preferred for its **vasodilatory effects** and greater efficacy in lowering blood pressure.
- While verapamil also lowers blood pressure, its primary utility in this context is its effect on cardiac rhythm and AV nodal conduction, not its blood pressure-lowering capabilities.
*Verapamil binds to the α2 subunit of the L-type calcium channel, while nifedipine binds to the α1 subunit of the L-type calcium channel.*
- Both verapamil and nifedipine primarily bind to the **α1 subunit** of the L-type calcium channel, though at different binding sites, leading to their distinct pharmacological effects.
- The α2 subunit is accessory and involved in channel trafficking and modulation, not the primary binding site for these drugs' therapeutic action.
Antiarrhythmic classification and mechanisms US Medical PG Question 8: Match the following antiarrhythmic drugs with their mechanism of action:
| Mechanism of action | Drug |
| :-- | :-- |
| 1. Na+ channel blocker | A. Quinidine |
| 2. K+ channel blocker | B. Digoxin |
| 3. Na+K+ ATPase inhibitor | C. Esmolol |
| 4. Beta-blocker | D. Ibutilide |
- A. 1-D, 2-B, 3-A, 4-C
- B. 1-A, 2-D, 3-B, 4-C (Correct Answer)
- C. 1-A, 2-C, 3-D, 4-B
- D. 1-D, 2-C, 3-A, 4-B
Antiarrhythmic classification and mechanisms Explanation: ***1-A, 2-D, 3-B, 4-C***
- **Quinidine** is a Class IA antiarrhythmic drug that primarily blocks **sodium channels**, prolonging the action potential duration and refractoriness.
- **Ibutilide** is a Class III antiarrhythmic drug that blocks **potassium channels**, leading to delayed repolarization and increased effective refractory period.
- **Digoxin** inhibits the **Na+/K+ ATPase pump**, increasing intracellular calcium and affecting AV nodal conduction.
- **Esmolol** is a **beta-blocker** (Class II antiarrhythmic) that reduces heart rate and contractility by blocking β1-adrenergic receptors.
*1-A, 2-C, 3-D, 4-B*
- This option incorrectly matches **Esmolol** (a beta-blocker) with **K+ channel blocker** and **Ibutilide** (K+ channel blocker) with **Na+K+ ATPase inhibitor**.
- It also incorrectly matches **Digoxin** (Na+K+ ATPase inhibitor) with **beta-blocker**.
*1-D, 2-C, 3-A, 4-B*
- This option incorrectly matches **Ibutilide** (K+ channel blocker) with **Na+ channel blocker** and incorrectly matches **Quinidine** (Na+ channel blocker) with **Na+K+ ATPase inhibitor**.
- It also incorrectly matches **Digoxin** (Na+K+ ATPase inhibitor) with **beta-blocker**.
*1-D, 2-B, 3-A, 4-C*
- This option incorrectly matches **Ibutilide** (K+ channel blocker) with **Na+ channel blocker** and **Digoxin** (Na+K+ ATPase inhibitor) with **K+ channel blocker**.
- It also incorrectly matches **Quinidine** (Na+ channel blocker) with **Na+K+ ATPase inhibitor**.
Antiarrhythmic classification and mechanisms US Medical PG Question 9: An investigator is studying a drug that acts on the thyroid hormone pathway. Levels of serum free T3 and T4 in healthy participants are measured before and after administration of the drug. After administration, there is a decrease in the average serum free T3 level, while the average serum free T4 level is increased compared to initial serum studies. Inhibition of which of the following is the most likely mechanism of action of this drug?
- A. Thyroid-stimulating hormone
- B. Follicular iodotyrosine deiodinase
- C. Follicular thyroid peroxidase
- D. Peripheral 5'-deiodinase (Correct Answer)
- E. Follicular thyroid proteases
Antiarrhythmic classification and mechanisms Explanation: ***Peripheral 5'-deiodinase***
- Inhibition of **peripheral 5'-deiodinase** would decrease the conversion of **T4 to T3** in the periphery, resulting in lower **free T3** and higher **free T4** levels.
- This enzyme is crucial for activating T4 into the more potent T3, and its blockade explains the observed changes in hormone levels.
*Thyroid-stimulating hormone*
- Inhibition of **TSH** would lead to a decrease in the production and release of both **T3 and T4** from the thyroid gland.
- This contradicts the observed increase in **free T4** levels.
*Follicular iodotyrosine deiodinase*
- This enzyme is involved in recycling iodine from **monoiodotyrosine (MIT)** and **diiodotyrosine (DIT)** within the thyroid follicular cells, which is important for efficient thyroid hormone synthesis.
- Its inhibition would primarily affect iodine availability and synthesis, not directly lead to increased T4 and decreased T3 in the periphery.
*Follicular thyroid peroxidase*
- **Thyroid peroxidase (TPO)** is critical for the **iodination of tyrosine residues** on thyroglobulin and the **coupling of MIT and DIT** to form T3 and T4.
- Inhibition of TPO would decrease the synthesis of both **T3 and T4**, contrary to the observed increase in **free T4**.
*Follicular thyroid proteases*
- **Thyroid proteases** cleave thyroglobulin to release mature **T3 and T4** into the bloodstream.
- Inhibition of these proteases would lead to a decrease in the release of both **T3 and T4**, which does not align with the observed increase in **free T4**.
Antiarrhythmic classification and mechanisms US Medical PG Question 10: A 72-year-old man with congestive heart failure is brought to the emergency department because of chest pain, shortness of breath, dizziness, and palpitations for 30 minutes. An ECG shows a wide complex tachycardia with a P-wave rate of 105/min, an R-wave rate of 130/min, and no apparent relation between the two. Intravenous pharmacotherapy is initiated with a drug that prolongs the QRS and QT intervals. The patient was most likely treated with which of the following drugs?
- A. Carvedilol
- B. Verapamil
- C. Flecainide
- D. Quinidine (Correct Answer)
- E. Sotalol
Antiarrhythmic classification and mechanisms Explanation: **Quinidine**
- Quinidine is a **Class IA antiarrhythmic** that blocks fast sodium channels, prolonging both the **QRS complex** (due to slowed conduction) and the **QT interval** (due to prolonged repolarization).
- The ECG findings of **wide-complex tachycardia** and **AV dissociation** (P-wave rate different from R-wave rate without apparent relation) are consistent with ventricular tachycardia, which Class IA drugs can treat.
*Carvedilol*
- Carvedilol is a **beta-blocker** (Class II antiarrhythmic) that primarily slows heart rate and AV nodal conduction, generally **shortening the QT interval** or having no effect, and would not widen the QRS complex.
- Beta-blockers are typically contraindicated in **decompensated heart failure** and **wide-complex tachycardia** due to their negative inotropic effects and risk of worsening decompensation.
*Verapamil*
- Verapamil is a **non-dihydropyridine calcium channel blocker** (Class IV antiarrhythmic) that mainly slows AV nodal conduction. It would not cause QRS widening and can shorten the QT interval.
- Verapamil is generally contraindicated in **wide-complex tachycardias** of unknown origin as it can precipitate cardiovascular collapse if the arrhythmia is ventricular.
*Flecainide*
- Flecainide is a **Class IC antiarrhythmic** that primarily blocks fast sodium channels, causing significant **QRS widening** but has **minimal effect on the QT interval**, which is contrary to the case description.
- Class IC agents are also generally avoided in patients with **structural heart disease** like congestive heart failure due to increased mortality risk.
*Sotalol*
- Sotalol is a **Class III antiarrhythmic** (beta-blocker with potassium channel blockade) that primarily prolongs the **QT interval** by blocking potassium channels. While it prolongs the QT, it does **not significantly widen the QRS complex**.
- Its beta-blocking effects could exacerbate **decompensated heart failure** in this patient, similar to carvedilol.
More Antiarrhythmic classification and mechanisms US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.