Respiratory syncytial virus therapies US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Respiratory syncytial virus therapies. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Respiratory syncytial virus therapies US Medical PG Question 1: A 10-year-old boy presents to the emergency department with his parents. The boy complains of fever, neck stiffness, and drowsiness for the last several days. His past medical history is noncontributory. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. There were no sick contacts at home or at school. The family did not travel out of the area recently. His heart rate is 100/min, respiratory rate is 22/min, blood pressure is 105/65 mm Hg, and temperature is 40.5ºC (104.9°F). On physical examination, he appears unwell and confused. His heart rate is elevated with a regular rhythm and his lungs are clear to auscultation bilaterally. During the examination, he experiences a right-sided focal seizure, which is controlled with lorazepam. A head CT reveals bilateral asymmetrical hypodensities of the temporal region. A lumbar puncture is performed and reveals the following:
WBC count 25/mm3
Cell predominance lymphocytes
Protein elevated
The patient is started on a medication to treat the underlying cause of his symptoms. What is the mechanism of action of this medication?
- A. Fusion inhibition
- B. Nucleoside reverse transcriptase inhibition
- C. Inhibition of DNA polymerase (Correct Answer)
- D. Binding with ergosterol in the cell membrane
- E. Cell wall synthesis inhibition
Respiratory syncytial virus therapies Explanation: ***Inhibition of DNA polymerase***
- The patient's symptoms (fever, neck stiffness, drowsiness, focal seizure, temporal lobe hypodensities) and CSF findings (lymphocytic pleocytosis, elevated protein) are highly suggestive of **herpes simplex encephalitis (HSE)**.
- The primary treatment for HSE is **acyclovir**, which works by inhibiting **viral DNA polymerase**.
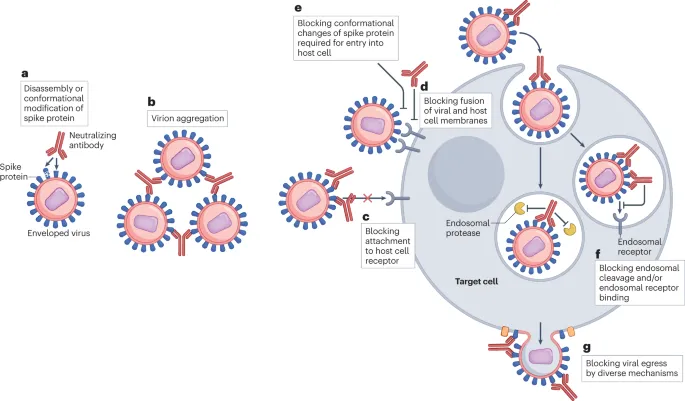
*Fusion inhibition*
- This mechanism is characteristic of **antiviral drugs used for HIV**, such as enfuvirtide, which block the entry of the virus into host cells by preventing fusion of the viral and cellular membranes.
- This mechanism is not relevant to the treatment of herpes simplex virus.
*Nucleoside reverse transcriptase inhibition*
- This mechanism is also primarily associated with **antiretroviral drugs for HIV** (e.g., zidovudine).
- These drugs inhibit the enzyme **reverse transcriptase**, which HIV uses to convert its RNA into DNA.
*Binding with ergosterol in the cell membrane*
- This is the mechanism of action for certain **antifungal medications**, such as **amphotericin B** and **nystatin**, which bind to ergosterol in fungal cell membranes, leading to cell lysis.
- This mechanism is not applicable to antiviral treatment for HSE.
*Cell wall synthesis inhibition*
- This mechanism describes the action of many **antibacterial agents** (e.g., penicillins, cephalosporins) that interfere with the formation of the bacterial cell wall.
- This is not relevant to viral infections like HSE.
Respiratory syncytial virus therapies US Medical PG Question 2: A 2300-g (5-lb 1-oz) male newborn is delivered to a 29-year-old primigravid woman. The mother has HIV and received triple antiretroviral therapy during pregnancy. Her HIV viral load was 678 copies/mL 1 week prior to delivery. Labor was uncomplicated. Apgar scores are 7 and 8 at 1 and 5 minutes respectively. Physical examination of the newborn shows no abnormalities. Which of the following is the most appropriate next step in management of this infant?
- A. Administer lamivudine and nevirapine
- B. Administer zidovudine, lamivudine and nevirapine (Correct Answer)
- C. Administer nevirapine
- D. Administer zidovudine
- E. HIV antibody testing
Respiratory syncytial virus therapies Explanation: ***Administer zidovudine, lamivudine and nevirapine***
- The mother has a **viral load of 678 copies/mL**, which falls into the **intermediate-risk category** (50-999 copies/mL) for HIV transmission.
- Current guidelines recommend **combination antiretroviral prophylaxis** (zidovudine + lamivudine + nevirapine) for infants born to mothers with viral loads in this range, typically given for 2 weeks followed by zidovudine alone to complete 4-6 weeks.
- This enhanced regimen provides better protection than monotherapy when maternal viral suppression is suboptimal.
*Administer zidovudine*
- Zidovudine monotherapy is reserved for **low-risk infants** whose mothers have viral loads **<50 copies/mL** at delivery with documented adherence to ART during pregnancy.
- With a maternal viral load of 678 copies/mL, monotherapy alone is **insufficient** and would not meet current standard of care for HIV prophylaxis.
*Administer lamivudine and nevirapine*
- This regimen omits **zidovudine**, which remains the **backbone of neonatal HIV prophylaxis** and should always be included.
- Using only lamivudine and nevirapine without zidovudine is not consistent with established guidelines.
*Administer nevirapine*
- Nevirapine monotherapy is **not adequate** for HIV prophylaxis in developed countries with access to combination therapy.
- While nevirapine may be used as a single dose in resource-limited settings, it should be part of a multi-drug regimen when other agents are available.
*HIV antibody testing*
- HIV antibody testing in newborns will detect **maternal antibodies** that crossed the placenta and cannot determine the infant's true infection status at birth.
- While HIV diagnostic testing using **PCR or viral load assays** will be performed at 14-21 days, 1-2 months, and 4-6 months of age, **antiretroviral prophylaxis must be initiated immediately** after birth to prevent transmission.
Respiratory syncytial virus therapies US Medical PG Question 3: A 3-year-old girl is brought to the emergency department because of chest pain for 2 hours. Eight days ago, she was admitted to the hospital for treatment of low-grade fever, malaise, and sore throat. The hospitalization was complicated by pharyngitis with pseudomembrane formation and severe cervical lymphadenopathy briefly requiring intubation. She has not received any routine childhood vaccinations. Serum studies show elevated cardiac troponins. An ECG shows diffuse T wave inversions and prolonged PR interval. Which of the following preventative measures would most likely have prevented this patient's cardiac symptoms?
- A. Antibiotic that binds to penicillin-binding protein 3
- B. Salicylate that inhibits prostaglandin synthesis
- C. Electrolyte that reduces cardiomyocyte excitability
- D. Immunoglobulin that targets circulating proteins
- E. Denatured bacterial toxin that contains an intact receptor binding site (Correct Answer)
Respiratory syncytial virus therapies Explanation: ***Denatured bacterial toxin that contains an intact receptor binding site***
- This describes a **toxoid vaccine**, specifically the **diphtheria toxoid vaccine**. The patient's initial symptoms (low-grade fever, malaise, sore throat, pseudomembrane formation, lymphadenopathy, intubation) are classic for **diphtheria**, a disease caused by *Corynebacterium diphtheriae*.
- Diphtheria toxin can cause **myocarditis**, leading to elevated **cardiac troponins**, diffuse T wave inversions, and prolonged PR interval as seen in this patient. Vaccination with the diphtheria toxoid would have prevented the disease and its cardiac complications.
*Antibiotic that binds to penicillin-binding protein 3*
- This describes a **third-generation cephalosporin** (e.g., ceftazidime, ceftriaxone) or other beta-lactam antibiotics. While these antibiotics can treat bacterial infections, they are not typically the primary prevention for diphtheria.
- The focus of prevention for diphtheria is vaccination due to the profound systemic effects of the **diphtheria toxin**, which treatment with antibiotics alone cannot counteract once the toxin is circulating.
*Salicylate that inhibits prostaglandin synthesis*
- This describes **aspirin (acetylsalicylic acid)**, a non-steroidal anti-inflammatory drug (NSAID). Aspirin is used to manage pain, fever, and inflammation.
- While it could alleviate some symptoms, it does not prevent the underlying cardiac complications of diphtheria, which are caused by the direct toxic effects on the myocardium, not primarily by inflammation responsive to prostaglandin inhibition.
*Electrolyte that reduces cardiomyocyte excitability*
- This likely refers to **calcium** or **magnesium** administered to stabilize cardiac membranes in certain toxicities or arrhythmias. For example, calcium can be given for hyperkalemia or calcium channel blocker overdose.
- This would be a treatment for acute cardiac symptoms, not a preventative measure against the diphtheria toxin's effects on the heart.
*Immunoglobulin that targets circulating proteins*
- This refers to **diphtheria antitoxin (DAT)**, which consists of antibodies (immunoglobulins) that bind to and neutralize circulating diphtheria toxin.
- While DAT would be administered as a treatment for active diphtheria infection to mitigate toxin effects, it is not a prophylactic measure given at the time of previous admission to *prevent* the cardiac symptoms in the long term; vaccination is the preventative approach.
Respiratory syncytial virus therapies US Medical PG Question 4: A 6-month-old male presents for a routine visit to his pediatrician. Two months ago, the patient was seen for tachypnea and wheezing, and diagnosed with severe respiratory syncytial virus (RSV) bronchiolitis. After admission to the hospital and supportive care, the patient recovered and currently is not experiencing any trouble breathing. Regarding the possibility of future reactive airway disease, which of the following statements is most accurate?
- A. “There is no clear relationship between RSV and the development of asthma.”
- B. “Your child has a greater than 20% chance of developing asthma” (Correct Answer)
- C. “Your child’s risk of asthma is less than the general population.”
- D. “Your child has a less than 5% chance of developing asthma”
- E. “Your child’s risk of asthma is the same as the general population.”
Respiratory syncytial virus therapies Explanation: ***“Your child has a greater than 20% chance of developing asthma”***
- Severe **RSV bronchiolitis** in infancy is a significant risk factor for the development of **recurrent wheezing** and **childhood asthma**.
- Studies estimate that a substantial proportion, often greater than 20%, of infants with severe RSV bronchiolitis will go on to develop **asthma** later in childhood.
*“There is no clear relationship between RSV and the development of asthma.”*
- This statement is incorrect as there is a **well-established link** between severe RSV infection in early life and an increased risk of developing **asthma**.
- Numerous epidemiological and longitudinal studies have documented this association.
*“Your child’s risk of asthma is less than the general population.”*
- This is incorrect, as severe RSV infection **increases** the risk of asthma, not decreases it.
- Children with a history of severe RSV have a **higher incidence** of asthma compared to the general pediatric population.
*“Your child has a less than 5% chance of developing asthma”*
- This percentage is **too low** given the known association between severe RSV bronchiolitis and subsequent asthma.
- The actual risk is considerably higher, typically falling into the range of 20-50% for those with severe RSV.
*“Your child’s risk of asthma is the same as the general population.”*
- This statement is inaccurate because severe RSV infection in infancy is a recognized independent **risk factor** for **asthma development**.
- Therefore, the child's risk is elevated above that of the general population.
Respiratory syncytial virus therapies US Medical PG Question 5: A research consortium is studying a new vaccine for respiratory syncytial virus (RSV) in premature infants compared to the current standard of care. 1000 infants were randomized to either the new vaccine group or the standard of care group. In total, 520 receive the new vaccine and 480 receive the standard of care. Of those who receive the new vaccine, 13 contract RSV. Of those who received the standard of care, 30 contract RSV. Which of the following is the absolute risk reduction of this new vaccine?
- A. 4.3%
- B. 3.75% (Correct Answer)
- C. 6.25%
- D. 1.7%
- E. 2.5%
Respiratory syncytial virus therapies Explanation: ***3.75%***
- **Absolute Risk Reduction (ARR)** is calculated as the difference between the event rate in the control group (CER) and the event rate in the experimental group (EER).
- Here, the event rate in the standard of care (control) group is (30/480) * 100% = 6.25%, and in the new vaccine (experimental) group is (13/520) * 100% = 2.5%. Therefore, ARR = 6.25% - 2.5% = **3.75%**.
*4.3%*
- This value might be obtained from an incorrect calculation or misinterpreting the numbers for the **risk reduction**.
- It does not represent the direct difference in risk between the two groups.
*6.25%*
- This value represents the event rate in the **standard of care (control) group** (30/480).
- It is the control event rate (CER), not the absolute risk reduction.
*1.7%*
- This value is not derived from the correct formula for **absolute risk reduction**.
- It may arise from an incomplete or incorrect calculation of the risk difference.
*2.5%*
- This value represents the event rate in the **new vaccine (experimental) group** (13/520).
- This is the experimental event rate (EER), not the absolute risk reduction.
Respiratory syncytial virus therapies US Medical PG Question 6: A 33-year-old woman presents to her local clinic in rural eastern India complaining of neck pain and fever. She reports a 4 day history of severe neck pain, neck stiffness, mild diarrhea, and fever. She has not taken her temperature. She works as a laborer and frequently carries heavy weights on her back. She is prescribed a medication and told to come back if her symptoms do not improve. Her symptoms resolve after a couple days. Six months later, she gives birth to a newborn male at 34 weeks gestation. His temperature is 97.8°F (36.6°C), blood pressure is 90/55 mmHg, pulse is 110/min, and respirations are 24/min. On examination, the baby is irritable with a weak cry. Ashen gray cyanosis is noted diffusely. What is the mechanism of action of the drug responsible for this child's presentation?
- A. DNA-dependent RNA polymerase inhibitor
- B. Dihydropteroate synthase inhibitor
- C. DNA gyrase inhibitor
- D. 30S ribosomal subunit inhibitor
- E. 50S ribosomal subunit inhibitor (Correct Answer)
Respiratory syncytial virus therapies Explanation: ***50S ribosomal subunit inhibitor***
- The mother's symptoms (neck pain, stiffness, fever, mild diarrhea) and rapid improvement suggest a bacterial infection treated with an antibiotic. Given the newborn's presentation of **gray baby syndrome** (ashen gray cyanosis, irritability, weak cry, hypothermia, hypotension), the likely causative drug is **chloramphenicol**.
- **Chloramphenicol** inhibits bacterial protein synthesis by binding to the **50S ribosomal subunit**, which can cause idiosyncratic toxicity in neonates due to underdeveloped glucuronidation enzymes needed for its metabolism.
*DNA-dependent RNA polymerase inhibitor*
- This mechanism describes drugs like **rifampin**, which is primarily used for **tuberculosis** and does not cause gray baby syndrome.
- Rifampin's side effects include **red-orange discoloration** of bodily fluids and **hepatotoxicity**, which are distinct from the described neonatal symptoms.
*Dihydropteroate synthase inhibitor*
- This mechanism is characteristic of **sulfonamides** (e.g., sulfamethoxazole), which inhibit folic acid synthesis in bacteria.
- Sulfonamides are associated with **kernicterus** in neonates (due to displacement of bilirubin from albumin), not gray baby syndrome.
*DNA gyrase inhibitor*
- This describes **fluoroquinolones** (e.g., ciprofloxacin), which block bacterial DNA replication and transcription.
- Fluoroquinolones are generally **contraindicated in pregnancy and children** due to concerns about cartilage damage, but they do not cause gray baby syndrome.
*30S ribosomal subunit inhibitor*
- This mechanism is used by **tetracyclines** and **aminoglycosides**.
- **Tetracyclines** can cause **tooth discoloration** and **bone growth inhibition** in children, while **aminoglycosides** are associated with **ototoxicity** and **nephrotoxicity**; neither causes gray baby syndrome.
Respiratory syncytial virus therapies US Medical PG Question 7: A parent presents to her pediatrician requesting information about immunizations for her newborn. The pediatrician explains about basic principles of immunization, types of vaccines, possible adverse effects, and the immunization schedule. Regarding how immunizations work, the pediatrician explains that there are mainly 2 types of vaccines. The first type of vaccine provides stronger and more lasting immunity as it induces both cellular and humoral immune responses. The second type of vaccine produces mainly a humoral response only, and its overall efficacy is less as compared to the first type. Which of the following vaccines belongs to the first type of vaccine that the pediatrician is talking about?
- A. Hepatitis A vaccine
- B. Polio vaccine (Salk)
- C. Yellow fever vaccine (Correct Answer)
- D. Rabies vaccine
- E. Hepatitis B vaccine
Respiratory syncytial virus therapies Explanation: ***Yellow fever vaccine***
- The Yellow fever vaccine is a **live-attenuated vaccine**, which mimics natural infection and effectively stimulates both **cellular and humoral immune responses**, leading to strong and long-lasting immunity.
- Live-attenuated vaccines contain a weakened form of the pathogen, allowing for replication within the host and robust immune system activation.
*Hepatitis A vaccine*
- The Hepatitis A vaccine is an **inactivated vaccine**, which primarily induces a **humoral (antibody-mediated) immune response**.
- Inactivated vaccines generally do not stimulate a strong cellular immune response and often require booster doses to maintain protective immunity.
*Polio vaccine (Salk)*
- The Salk polio vaccine is an **inactivated polio vaccine (IPV)**, meaning it contains killed viral particles.
- As an inactivated vaccine, it mainly elicits a **humoral immune response** producing circulating antibodies but less mucosal or cellular immunity.
*Rabies vaccine*
- The Rabies vaccine is an **inactivated vaccine** given after exposure or for pre-exposure prophylaxis.
- It primarily induces a **humoral antibody response** rather than a strong cellular immune response.
*Hepatitis B vaccine*
- The Hepatitis B vaccine is a **recombinant vaccine**, containing only a portion of the viral antigen (HBsAg).
- This type of vaccine primarily stimulates a **humoral immune response** leading to antibody production, which is effective but does not typically induce a strong cellular response like live vaccines.
Respiratory syncytial virus therapies US Medical PG Question 8: A 25-year-old man presents with jaw discomfort and the inability to open his mouth fully for about 3 days. About a week ago, he says he cut himself while preparing a chicken dinner but did not seek medical assistance. Five days after the original injury, he started noticing jaw discomfort and an inability to open his mouth completely. He has no history of a serious illness or allergies and takes no medications. The patient says he had received his primary tetanus series in childhood, and that his last booster was more than 10 years ago. His blood pressure is 125/70 mm Hg and temperature is 36.9℃ (98.5°F). On physical examination, the patient is unable to open his jaw wider than 2.5 cm. Head and neck examinations are otherwise unremarkable. There is a 5 cm linear shallow laceration with some granulation tissue on the right index finger without necrosis, erythema, or pus. After wound care and initiation of metronidazole, which of the following is the next best step in the management of this patient?
- A. DTaP
- B. Td
- C. Tetanus immunoglobulin (TIG) (Correct Answer)
- D. No further treatment is required
- E. Tdap
Respiratory syncytial virus therapies Explanation: ***Tetanus immunoglobulin (TIG)***
- This patient presents with symptoms highly suggestive of **tetanus**, including **trismus** (lockjaw) and a recent puncture wound. TIG provides **passive immunity** with pre-formed antibodies that can neutralize circulating tetanus toxin, which is crucial for immediate treatment.
- Given that his last tetanus booster was more than 10 years ago and he is symptomatic, immediate TIG is necessary to combat the toxin already produced by *Clostridium tetani*.
- **Note**: A tetanus toxoid vaccine (Td or Tdap) should also be administered at a different site to provide active immunity, but TIG is the **priority** intervention for neutralizing existing toxin in a symptomatic patient.
*DTaP*
- **DTaP (diphtheria, tetanus, acellular pertussis)** is administered to **children younger than 7 years old**. This patient is 25 years old.
- While it provides **active immunity**, its effect is not immediate and would not address the acute, life-threatening toxin effects already present in a symptomatic patient.
*Td*
- **Td (tetanus and diphtheria)** is a booster vaccine providing **active immunity** suitable for adults.
- Like DTaP, it confers active immunity, which takes time to develop and would not provide immediate protection against the existing tetanus toxin in a symptomatic patient. However, Td should be administered alongside TIG at a different site as part of complete management.
*No further treatment is required*
- This patient is clearly symptomatic with **trismus** after a puncture wound and an outdated tetanus vaccination, indicating an active **tetanus infection**.
- Without immediate intervention, tetanus can lead to severe muscle spasms, respiratory failure, and death, so further treatment is urgently required.
*Tdap*
- **Tdap (tetanus, diphtheria, acellular pertussis)** is an adult-formulation booster vaccine, primarily given to adolescents and adults, especially during pregnancy or when in contact with infants.
- It provides **active immunity**, which is not effective in neutralizing the immediate effects of existing tetanus toxin in a symptomatic patient. However, Tdap should be administered alongside TIG at a different site as part of complete management.
Respiratory syncytial virus therapies US Medical PG Question 9: A 6-month-old infant boy is brought to the clinic for a check-up by a couple who recently adopted him from foster care. The biological mother was from a rehabilitation facility and was found incompetent to care for the child, hence he was handed over to foster care. No other information is available regarding his prenatal or birth history. On examination, his weight is found to be below the 3rd percentile. Physical appearance is remarkable for midfacial hypoplasia with a flattened nasal bridge, smooth philtrum, and thin lips. Auscultation reveals a grade 3/6 holosystolic murmur at the left lower sternal border. Developmental delay is noted as well. Which of the following teratogens is most likely to be associated with the infant's presentation?
- A. Lithium
- B. Tobacco
- C. Phenytoin
- D. Alcohol (Correct Answer)
- E. Cocaine
Respiratory syncytial virus therapies Explanation: ***Alcohol***
- The combination of **facial dysmorphology** (midfacial hypoplasia, flattened nasal bridge, smooth philtrum, thin lips), **growth restriction** (weight below 3rd percentile), **cardiac defect** (holosystolic murmur), and **developmental delay** is highly characteristic of **Fetal Alcohol Syndrome (FAS)**.
- The biological mother's history of being in a **rehabilitation facility** suggests a potential history of substance abuse, making maternal alcohol consumption during pregnancy a strong possibility.
*Lithium*
- Maternal lithium use is associated with **Ebstein's anomaly**, a specific congenital heart defect, but typically does not cause the widespread facial dysmorphism and growth restriction seen in this infant.
- While it can cause cardiac defects, the overall constellation of findings points away from lithium as the primary teratogen.
*Tobacco*
- Maternal tobacco use is primarily associated with **low birth weight**, premature birth, and an increased risk of specific birth defects like **cleft lip and palate**.
- It does not typically cause the characteristic facial features, significant cardiac anomalies, or widespread developmental delay observed in this case.
*Phenytoin*
- Phenytoin, an anticonvulsant, can cause **fetal hydantoin syndrome**, characterized by specific facial features (e.g., hypertelorism, short nose, cleft lip/palate), **digital hypoplasia**, and intellectual disability.
- While it can cause some overlapping features like growth deficiency and developmental delay, the specific craniofacial features described for this infant are more typical of FAS.
*Cocaine*
- Cocaine exposure during pregnancy is associated with a range of problems including **preterm birth**, **placental abruption**, and **genitourinary defects**.
- Its teratogenic effects often involve vascular disruption leading to limb defects or cerebral infarctions, rather than the characteristic facial dysmorphology and cardiac defects described in this infant.
Respiratory syncytial virus therapies US Medical PG Question 10: A 26-year-old G1P0 woman is brought to the emergency room by her spouse for persistently erratic behavior. Her spouse reports that she has been sleeping > 1 hour a night, and it sometimes seems like she’s talking to herself. She has maxed out their credit cards on baby clothes. The patient’s spouse reports this has been going on for over a month. Since first seeing a physician, she has been prescribed multiple first and second generation antipsychotics, but the patient’s spouse reports that her behavior has failed to improve. Upon examination, the patient is speaking rapidly and occasionally gets up to pace the room. She reports she is doing “amazing,” and that she is “so excited for the baby to get here because I’m going to be the best mom.” She denies illicit drug use, audiovisual hallucinations, or suicidal ideation. The attending psychiatrist prescribes a class of medication the patient has not yet tried to treat the patient’s psychiatric condition. In terms of this new medication, which of the following is the patient’s newborn most likely at increased risk for?
- A. Ototoxicity
- B. Attention deficit hyperactivity disorder
- C. Right ventricular atrialization (Correct Answer)
- D. Renal defects
- E. Caudal regression syndrome
Respiratory syncytial virus therapies Explanation: ***Right ventricular atrialization***
- The patient's presentation of persistent **erratic behavior**, **reduced sleep**, rapid speech, and increased spending, enduring for over a month, is highly suggestive of a **manic episode** in the context of **bipolar I disorder**. Since antipsychotics have been ineffective, the next step is often **lithium**.
- **Lithium** exposure during the first trimester of pregnancy is associated with an increased risk of **Ebstein's anomaly**, a congenital heart defect characterized by **right ventricular atrialization** (displacement of the tricuspid valve leaflets into the right ventricle), leading to tricuspid regurgitation and right heart failure.
*Ototoxicity*
- **Ototoxicity** in newborns is typically associated with exposure to medications such as **aminoglycoside antibiotics** (e.g., gentamicin) or certain diuretics (e.g., furosemide) during pregnancy.
- Lithium is not known to cause ototoxicity as a primary birth defect.
*Attention deficit hyperactivity disorder*
- While various prenatal exposures can influence neurodevelopment, there is currently **no strong evidence** linking in-utero lithium exposure specifically to an increased risk of **ADHD** in offspring.
- ADHD is a complex neurodevelopmental disorder with multifactorial origins, including genetic and environmental factors.
*Renal defects*
- While lithium is primarily excreted by the kidneys and can cause **renal dysfunction** in adults (e.g., nephrogenic diabetes insipidus), it is not a prominent teratogen known to cause specific **structural renal defects** in newborns when exposed during pregnancy.
- Renal anomalies are more commonly associated with other medications or genetic syndromes.
*Caudal regression syndrome*
- **Caudal regression syndrome** is a severe congenital anomaly affecting the development of the lower spine and limbs. It is strongly associated with **poorly controlled maternal diabetes**.
- There is no established link between in-utero lithium exposure and caudal regression syndrome.
More Respiratory syncytial virus therapies US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.