Hepatitis C direct-acting antivirals US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hepatitis C direct-acting antivirals. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hepatitis C direct-acting antivirals US Medical PG Question 1: You are seeing a patient in clinic who recently started treatment for active tuberculosis. The patient is currently being treated with rifampin, isoniazid, pyrazinamide, and ethambutol. The patient is not used to taking medicines and is very concerned about side effects. Specifically regarding the carbohydrate polymerization inhibiting medication, which of the following is a known side effect?
- A. Vision loss (Correct Answer)
- B. Paresthesias of the hands and feet
- C. Cutaneous flushing
- D. Arthralgias
- E. Elevated liver enzymes
Hepatitis C direct-acting antivirals Explanation: ***Vision loss***
- The "carbohydrate polymerization inhibiting medication" refers to **ethambutol**, which inhibits **arabinosyl transferase** (involved in mycobacterial cell wall arabinogalactan synthesis)
- **Ethambutol** causes **optic neuritis**, leading to **decreased visual acuity**, **red-green color blindness**, and potentially **irreversible vision loss**
- **Regular ophthalmologic monitoring** is essential during ethambutol therapy
*Paresthesias of the hands and feet*
- This describes **peripheral neuropathy** caused by **isoniazid**
- Isoniazid interferes with **pyridoxine (vitamin B6) metabolism**, leading to neurotoxicity
- Risk factors include malnutrition, diabetes, alcoholism, and pregnancy
- Prevented by **pyridoxine supplementation**
*Cutaneous flushing*
- Not a characteristic side effect of first-line anti-tuberculosis medications
- More commonly associated with niacin or certain allergic/vasodilatory reactions
*Arthralgias*
- Classic side effect of **pyrazinamide**, often affecting small joints
- Caused by **pyrazinamide-induced hyperuricemia** (inhibits renal uric acid excretion)
- May require dose adjustment or discontinuation if severe
*Elevated liver enzymes*
- **Hepatotoxicity** can occur with **rifampin**, **isoniazid**, and **pyrazinamide**
- Requires regular monitoring of liver function tests during TB treatment
- Most common serious adverse effect of combination TB therapy
Hepatitis C direct-acting antivirals US Medical PG Question 2: A 25-year-old sexually active male presents to an internal medicine physician for a routine health check up after having several unprotected sexual encounters. After appropriate testing the physician discusses with the patient that he is HIV+ and must be started on anti-retroviral treatment. Which of the following medications prescribed acts on the gp41 subunit of the HIV envelope glycoprotein?
- A. Zidovudine
- B. Saquinavir
- C. Enfuvirtide (Correct Answer)
- D. Amantadine
- E. Rimantadine
Hepatitis C direct-acting antivirals Explanation: ***Enfuvirtide***
- **Enfuvirtide** is a **fusion inhibitor** that binds specifically to the **gp41 subunit** of the HIV envelope glycoprotein.
- By binding to gp41, Enfuvirtide prevents the **fusion of the viral and host cell membranes**, thereby blocking viral entry and replication.
*Zidovudine*
- **Zidovudine** is a **nucleoside reverse transcriptase inhibitor (NRTI)**.
- It works by inhibiting the enzyme **reverse transcriptase**, which is responsible for converting viral RNA into DNA.
*Saquinavir*
- **Saquinavir** is a **protease inhibitor (PI)**.
- This drug works by inhibiting the **HIV protease enzyme**, which is crucial for cleaving viral polyproteins into functional proteins required for viral assembly and maturation.
*Amantadine*
- **Amantadine** is an **antiviral agent** primarily used to treat **influenza A**.
- It works by interfering with the **M2 proton channel** of the influenza A virus, thus inhibiting viral uncoating.
*Rimantadine*
- **Rimantadine** is another **antiviral agent** used for **influenza A treatment and prophylaxis**.
- Similar to amantadine, it targets the **M2 proton channel** of the influenza A virus, preventing the uncoating step necessary for viral replication.
Hepatitis C direct-acting antivirals US Medical PG Question 3: A 49-year-old man presents to a new primary care provider complaining of fatigue and occasional fever over the last month. These symptoms are starting to affect his job and he would like treatment. The physician runs a standard metabolic panel that shows elevated AST and ALT. The patient is then tested for hepatitis viruses. He is hepatitis C positive. The patient and his doctor discuss treatment options and agree upon pegylated interferon and oral ribavirin. Which side-effect is most likely while taking the ribavirin?
- A. Hemolytic anemia (Correct Answer)
- B. Leukopenia
- C. Rash
- D. Drug-associated lupus
- E. Hyperthyroidism
Hepatitis C direct-acting antivirals Explanation: ***Hemolytic anemia***
- **Ribavirin** is a guanosine analog that causes **hemolytic anemia** by accumulating in red blood cells and disrupting their metabolism.
- This side effect is common and often dose-limiting, requiring close monitoring of hemoglobin levels.
*Leukopenia*
- **Leukopenia** (low white blood cell count) is a known side effect of **interferon therapy**, not primarily ribavirin.
- While patients on combination therapy may experience this, it's more directly attributable to the interferon component.
*Rash*
- **Rash** can occur with various medications, including combination hepatitis C therapy, but it is not a hallmark or most likely side effect specifically associated with **ribavirin**.
- It's generally less clinically significant than hemolytic anemia.
*Drug-associated lupus*
- **Drug-associated lupus** is a rare and severe reaction, sometimes linked to certain drugs like **hydralazine** or **procainamide**, but not typically associated with **ribavirin** or hepatitis C treatment.
- Its occurrence probability is much lower than hemolytic anemia.
*Hyperthyroidism*
- **Thyroid dysfunction**, including **hyperthyroidism** and hypothyroidism, is a known side effect of **interferon therapy**, due to its immunomodulatory effects.
- It is not a primary side effect of **ribavirin**.
Hepatitis C direct-acting antivirals US Medical PG Question 4: A 52-year-old woman comes to the physician because of abdominal discomfort, anorexia, and mild fatigue. She has systemic lupus erythematosus and takes hydroxychloroquine. She does not drink alcohol or use illicit drugs. Physical examination shows no abnormalities. Laboratory studies show:
Alanine aminotransferase 455 U/L
Aspartate aminotransferase 205 U/L
Hepatitis B surface antigen positive
Hepatitis B surface antibody negative
Hepatitis B envelope antigen positive
Hepatitis B core antigen IgG antibody positive
Which of the following is the most appropriate pharmacotherapy for this patient?
- A. Acyclovir
- B. Tenofovir (Correct Answer)
- C. Pegylated interferon-alpha
- D. Dolutegravir
- E. Sofosbuvir
Hepatitis C direct-acting antivirals Explanation: ***Tenofovir***
- This patient has **chronic active hepatitis B infection**, as indicated by **positive HBsAg**, **HBeAg**, and elevated liver enzymes. Antiviral therapy with **tenofovir** is highly effective and appropriate to suppress viral replication.
- The coexistence of **Systemic Lupus Erythematosus (SLE)** and **hydroxychloroquine** use increases the importance of managing HBV, as immunosuppression can lead to viral reactivation; tenofovir effectively targets the virus without significant interactions.
*Acyclovir*
- **Acyclovir** is an antiviral medication primarily used to treat infections caused by **herpes simplex virus (HSV)** and **varicella-zoster virus (VZV)**.
- It has **no efficacy** against hepatitis B virus (HBV) and therefore would not be appropriate for this patient's condition.
*Pegylated interferon-alpha*
- **Pegylated interferon-alpha** is an immunomodulatory agent used to treat chronic hepatitis B and C; however, it has a **less favorable side effect profile** and is often reserved for patients who cannot tolerate or respond to nucleoside/nucleotide analogs.
- The patient's underlying **SLE** could be **exacerbated by interferon**, making tenofovir a safer and more appropriate first-line choice given its better tolerability and potent antiviral effect.
*Dolutegravir*
- **Dolutegravir** is an **integrase inhibitor** used in the treatment of **HIV infection**.
- It has **no antiviral activity** against the hepatitis B virus and is therefore not indicated for this patient's condition.
*Sofosbuvir*
- **Sofosbuvir** is a direct-acting antiviral agent primarily used to treat **chronic hepatitis C virus (HCV) infection**.
- It is **not effective** against hepatitis B virus (HBV) and would not be the correct treatment for this patient.
Hepatitis C direct-acting antivirals US Medical PG Question 5: A 26-year-old nurse presents 12 hours after she accidentally stuck herself with a blood-contaminated needle. She reported the accident appropriately and now seeks post-exposure prophylaxis. She does not have any complaints at the moment of presentation. Her vital signs include: blood pressure 125/80 mm Hg, heart rate 71/min, respiratory rate 15/min, and temperature 36.5℃ (97.7℉). Physical examination is unremarkable. The nurse has prescribed a post-exposure prophylaxis regimen which includes tenofovir, emtricitabine, and raltegravir. How will tenofovir change the maximum reaction rate (Vm) and Michaelis constant (Km) of the viral reverse transcriptase?
- A. Vm will decrease, Km will increase
- B. Vm and Km will both decrease
- C. Vm will stay the same, Km will increase
- D. Vm and Km will both increase
- E. Vm will decrease, Km will stay the same (Correct Answer)
Hepatitis C direct-acting antivirals Explanation: ***Vm will decrease, Km will stay the same***
- **Tenofovir** is a **nucleotide reverse transcriptase inhibitor (NtRTI)** that acts as a **competitive substrate analog**. Once phosphorylated to **tenofovir diphosphate**, it competes with natural deoxyadenosine triphosphate (dATP) for incorporation into the viral DNA chain.
- Upon incorporation, tenofovir acts as a **chain terminator** because it lacks a 3'-hydroxyl group necessary for further DNA elongation. This **irreversibly inactivates** the enzyme-DNA complex, effectively reducing the **maximum reaction rate (Vm)** by decreasing the amount of functional enzyme available.
- Since tenofovir competes with natural nucleotides but doesn't affect the enzyme's affinity for its natural substrates, the **Michaelis constant (Km) remains unchanged**. The inhibition pattern shows characteristics of competitive inhibition with irreversible chain termination.
*Vm will decrease, Km will increase*
- This pattern is characteristic of a **mixed inhibitor**, where the inhibitor can bind to both the free enzyme and the enzyme-substrate complex, reducing Vm while also decreasing substrate affinity (increasing Km).
- While tenofovir does reduce Vm through chain termination, it does not significantly alter the enzyme's affinity for natural nucleotide substrates. Tenofovir diphosphate **competes directly** with dATP rather than binding to an allosteric site, so Km remains unchanged rather than increasing.
*Vm and Km will both decrease*
- This effect is typical of an **uncompetitive inhibitor**, which binds only to the **enzyme-substrate complex**. Uncompetitive inhibitors decrease both Vm and Km, implying increased apparent substrate affinity.
- Tenofovir does not function as an uncompetitive inhibitor. As a **nucleotide analog**, it competes for the active site and gets incorporated into DNA, causing chain termination. This mechanism does not involve preferential binding to the enzyme-substrate complex that would decrease Km.
*Vm will stay the same, Km will increase*
- This describes **pure reversible competitive inhibition**, where the inhibitor competes with substrate for the active site but can be overcome by increasing substrate concentration, leaving Vm unchanged.
- While tenofovir diphosphate does **compete with natural nucleotides**, it acts as a **suicide substrate** that causes irreversible chain termination once incorporated. This **permanently inactivates** the enzyme-DNA complex, reducing the pool of functional enzyme and thus decreasing Vm, distinguishing it from simple reversible competitive inhibition.
*Vm and Km will both increase*
- An increase in both Vm and Km is not a standard pattern for enzyme inhibition and would suggest **reduced substrate affinity** with paradoxically increased catalytic capacity, which is inconsistent with any inhibitory mechanism.
- This scenario contradicts the **intended therapeutic effect** of tenofovir, which is to inhibit HIV reverse transcriptase activity and prevent viral replication, not to enhance enzyme function.
Hepatitis C direct-acting antivirals US Medical PG Question 6: A 52-year-old man presents to his physician after his routine screening revealed that he has elevated liver enzymes. He complains of occasional headaches during the past year, but otherwise feels well. The patient reports that he was involved in a serious car accident in the 1980s. He does not smoke or drink alcohol. He has no history of illicit intravenous drug use. He does not currently take any medications and has no known allergies. His father had a history of alcoholism and died of liver cancer. The patient appears thin. His temperature is 37.8°C (100°F), pulse is 100/min, and blood pressure is 110/70 mm Hg. The physical examination reveals no abnormalities. The laboratory test results show the following:
Complete blood count
Hemoglobin 14 g/dL
Leukocyte count 10,000/mm3
Platelet count 146,000/mm3
Comprehensive metabolic profile
Glucose 150 mg/dL
Albumin 3.2 g/dL
Total bilirubin 1.5 mg/dL
Alkaline phosphatase 75 IU/L
AST 95 IU/L
ALT 73 IU/L
Other lab tests
HIV negative
Hepatitis B surface antigen negative
Hepatitis C antibody positive
HCV RNA positive
HCV genotype 1
A liver biopsy is performed and shows mononuclear infiltrates localized to portal tracts that reveal periportal hepatocyte necrosis. Which of the following is the most appropriate next step in management?
- A. Peginterferon alpha therapy
- B. Interferon and ribavirin therapy
- C. Sofosbuvir and ledipasvir therapy (Correct Answer)
- D. Tenofovir and entecavir therapy
- E. Tenofovir and velpatasvir therapy
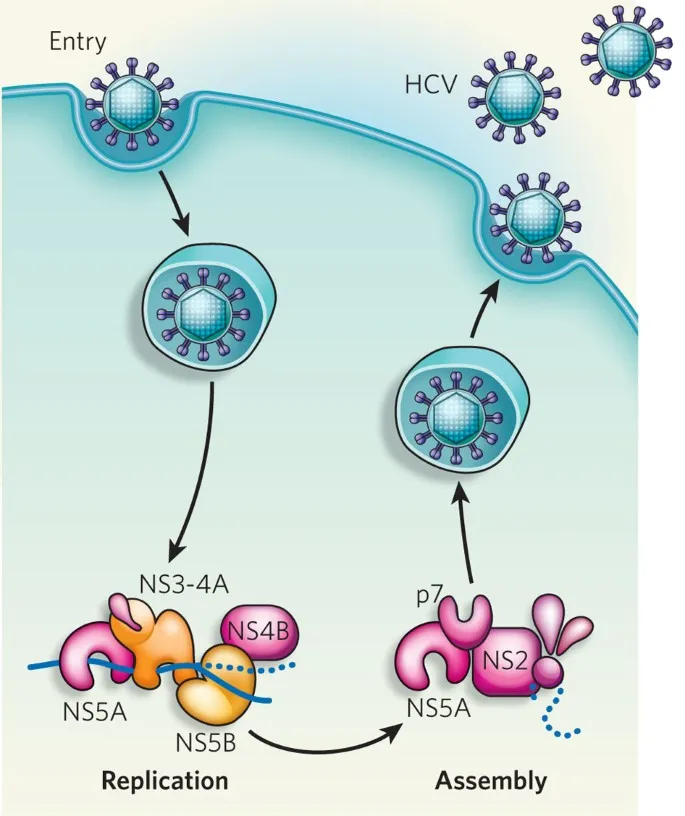
Hepatitis C direct-acting antivirals Explanation: ***Sofosbuvir and ledipasvir therapy***
- This patient has chronic **Hepatitis C (HCV) infection** (HCV antibody positive, HCV RNA positive). **Sofosbuvir/ledipasvir** is an effective **direct-acting antiviral (DAA)** regimen for **genotype 1 HCV**, which is indicated for treatment-naïve patients without cirrhosis.
- The liver biopsy findings of **mononuclear infiltrates** and **periportal necrosis** confirm active hepatitis and the need for antiviral treatment to prevent progression to cirrhosis.
*Peginterferon alpha therapy*
- **Peginterferon alpha** was historically used for HCV, but its use has largely been replaced by **DAAs** due to significant side effects and lower efficacy.
- This therapy is associated with numerous adverse effects, including **flu-like symptoms**, **depression**, and **bone marrow suppression**.
*Interferon and ribavirin therapy*
- This combination was a standard treatment for HCV before the advent of DAAs, but it is associated with a high burden of **side effects** like **hemolytic anemia** (from ribavirin) and **flu-like symptoms** (from interferon).
- Given the availability of highly effective and well-tolerated DAAs, this regimen is no longer considered first-line for chronic HCV.
*Tenofovir and entecavir therapy*
- **Tenofovir** and **entecavir** are antiviral medications primarily used for the treatment of **chronic Hepatitis B (HBV) infection**.
- This patient's **Hepatitis B surface antigen is negative**, ruling out chronic HBV infection as the primary issue requiring these specific drugs.
*Tenofovir and velpatasvir therapy*
- While **velpatasvir** is a DAA used for HCV, its combination with **tenofovir** is not a standard HCV treatment for genotype 1.
- **Tenofovir** is primarily an anti-HBV drug; for HCV, velpatasvir is typically combined with **sofosbuvir** (as in Epclusa) for pan-genotypic coverage.
Hepatitis C direct-acting antivirals US Medical PG Question 7: A 45-year-old man presents for follow-up to monitor his chronic hepatitis C treatment. The patient was infected with hepatitis C genotype 1, one year ago. He has been managed on a combination of pegylated interferon-alpha and ribavirin, but a sustained viral response has not been achieved. Past medical history is significant for non-alcoholic fatty liver disease for the last 5 years. Which of the following, if added to the patient’s current treatment regimen, would most likely benefit this patient?
- A. Emtricitabine
- B. Entecavir
- C. Simeprevir (Correct Answer)
- D. Tenofovir
- E. Telbivudine
Hepatitis C direct-acting antivirals Explanation: ***Simeprevir***
- Simeprevir is a **first-generation direct-acting antiviral (DAA)**, specifically a **protease inhibitor (NS3/4A inhibitor)**, highly effective against **HCV genotype 1**.
- Adding simeprevir to a regimen of **pegylated interferon-alpha and ribavirin** significantly increases the likelihood of achieving a **sustained virologic response** for patients who previously failed interferon-based therapy.
- **Note:** While this triple therapy approach was standard practice historically, current guidelines (as of 2024-2025) favor **interferon-free DAA combination regimens** (such as sofosbuvir/ledipasvir or glecaprevir/pibrentasvir) as first-line treatment for HCV genotype 1. However, among the options provided, simeprevir remains the only appropriate HCV-specific antiviral agent.
*Emtricitabine*
- This is a **nucleoside reverse transcriptase inhibitor (NRTI)** primarily used in the treatment of **HIV infection** and sometimes for hepatitis B.
- It has **no significant role** in the treatment of **hepatitis C viral infection**.
*Entecavir*
- Entecavir is an **antiviral agent** specifically used for the treatment of **chronic hepatitis B virus (HBV)** infection.
- It has **no established efficacy** against the **hepatitis C virus (HCV)**.
*Tenofovir*
- Tenofovir is a **nucleotide reverse transcriptase inhibitor** primarily used for treating **HIV infection** and **chronic hepatitis B virus (HBV)** infection.
- It is **not effective** against **hepatitis C virus (HCV)**.
*Telbivudine*
- Telbivudine is an **oral antiviral agent** indicated specifically for the treatment of **chronic hepatitis B virus (HBV)** infection.
- It does **not have antiviral activity** against the **hepatitis C virus (HCV)**.
Hepatitis C direct-acting antivirals US Medical PG Question 8: A 27-year-old man is brought to the emergency department by his friends in a confused state. He was doing fine 5 days ago when he started to complain of fever and flu-like symptoms. His fever was low-grade and associated with a headache. For the past 2 days, he has become increasingly irritable, confused, and was getting angry at trivial things. Past medical history is unremarkable. He is a college student and is physically active. He smokes cigarettes occasionally. He drinks alcohol socially. He is sexually active with his girlfriend and they use condoms inconsistently. Physical examination reveals: blood pressure 120/80 mm Hg, heart rate 108/min, respiratory rate 10/min, and temperature 37.4°C (99.4°F). He is confused and disoriented. Pupils are 3 mm in diameter and respond to light sluggishly. He is moving all his limbs spontaneously. His neck is supple. MRI of the brain is shown in the picture. Cerebrospinal fluid (CSF) reveals an opening pressure of 16 cm of H20, a total leukocyte count of 112/mm3 with 85% lymphocytes, the protein of 42 mg/dL, and glucose of 58 mg/dL. What is the best treatment for this condition?
- A. Intravenous immunoglobulin
- B. High-dose steroids
- C. Rituximab
- D. Acyclovir (Correct Answer)
- E. Ceftriaxone
Hepatitis C direct-acting antivirals Explanation: ***Acyclovir***
- The patient's presentation with **fever**, **flu-like symptoms** followed by **irritability**, **confusion**, and **MRI findings** suggestive of temporal lobe involvement, along with **lymphocytic pleocytosis** in CSF, is highly indicative of **herpes simplex encephalitis (HSE)**.
- **Acyclovir** is the treatment of choice for HSE, as it is an antiviral drug effective against the **herpes simplex virus (HSV)**. Prompt administration significantly improves outcomes.
*Intravenous immunoglobulin*
- **Intravenous immunoglobulin (IVIG)** is generally used for certain **immunodeficiencies** or **autoimmune conditions**, not for acute viral encephalitis like HSE.
- There is no evidence to support the use of IVIG as a primary treatment for HSV encephalitis.
*High-dose steroids*
- While steroids can reduce cerebral edema and inflammation, their routine use in **viral encephalitis** like HSE is **controversial** and not a first-line treatment.
- Steroids might be considered in specific cases of severe cerebral edema, but not as the primary antiviral therapy.
*Rituximab*
- **Rituximab** is a **monoclonal antibody** targeting **CD20-positive B cells**, primarily used in certain **lymphomas** and **autoimmune diseases** like **rheumatoid arthritis** or **multiple sclerosis**.
- It has no role in the treatment of acute viral encephalitis.
*Ceftriaxone*
- **Ceftriaxone** is a broad-spectrum **antibiotic** used to treat **bacterial meningitis** or other bacterial infections.
- It is ineffective against viral infections such as HSV encephalitis.
Hepatitis C direct-acting antivirals US Medical PG Question 9: A 62-year-old man presents to his geriatrician due to waking several times during the night and also rising too early in the morning. He says this has worsened over the past 7 months. In the morning, he feels unrefreshed and tired. His medical history is positive for hypertension and benign prostatic hyperplasia. He has never been a smoker. He denies drinking alcohol or caffeine prior to bedtime. Vital signs reveal a temperature of 36.6°C (97.8°F), blood pressure of 130/80 mm Hg, and heart rate of 77/min. Physical examination is unremarkable. After discussing good sleep hygiene with the patient, which of the following is the best next step in the management of this patient’s condition?
- A. Cognitive behavioral therapy for insomnia (CBT-I) (Correct Answer)
- B. Melatonin supplementation
- C. Referral to sleep medicine specialist
- D. Polysomnography
- E. Zolpidem
Hepatitis C direct-acting antivirals Explanation: ***Cognitive behavioral therapy for insomnia (CBT-I)***
- CBT-I is the **first-line treatment** for chronic insomnia according to the American Academy of Sleep Medicine and American College of Physicians guidelines
- After addressing sleep hygiene (already done), CBT-I is the recommended next step before considering pharmacotherapy
- CBT-I has **durable benefits** without the risks of medications, particularly important in elderly patients
- Components include sleep restriction, stimulus control, cognitive restructuring, and relaxation techniques
- In elderly patients, CBT-I avoids medication-related risks such as **falls, cognitive impairment, and dependence**
*Zolpidem*
- While hypnotics like zolpidem may provide short-term symptom relief, they are **not first-line therapy** for chronic insomnia
- The American Geriatrics Society **Beers Criteria** lists benzodiazepines and Z-drugs (including zolpidem) as potentially inappropriate medications in older adults due to increased risk of **falls, fractures, cognitive impairment, and delirium**
- Hypnotics should be reserved for situations where CBT-I is unavailable, ineffective, or when used as a short-term adjunct while implementing behavioral therapy
- If used, they should be prescribed at the **lowest effective dose for the shortest duration**
*Melatonin supplementation*
- Melatonin is most helpful for **circadian rhythm disorders** (e.g., delayed sleep phase syndrome) or **jet lag**
- Limited evidence supports its effectiveness for chronic insomnia with sleep maintenance problems (frequent awakenings and early morning awakening) in elderly patients
- May have a role in patients with documented melatonin deficiency or specific circadian disorders
*Referral to sleep medicine specialist*
- Appropriate if initial interventions (sleep hygiene, CBT-I, limited pharmacotherapy trial) fail
- Indicated when suspecting **primary sleep disorders** such as obstructive sleep apnea, restless legs syndrome, or periodic limb movement disorder
- Not the immediate next step for straightforward chronic insomnia presentation after sleep hygiene counseling
*Polysomnography*
- Polysomnography (sleep study) is indicated when there is clinical suspicion of **sleep-disordered breathing** (sleep apnea), **narcolepsy**, **REM sleep behavior disorder**, or **periodic limb movement disorder**
- This patient's presentation (sleep maintenance insomnia with frequent awakenings and early morning awakening) is most consistent with **primary insomnia**, not a parasomnia or sleep-disordered breathing
- Red flags for sleep apnea (witnessed apneas, loud snoring, gasping, excessive daytime sleepiness, obesity) are absent
- Polysomnography is **not routinely indicated** for the diagnosis of chronic insomnia
Hepatitis C direct-acting antivirals US Medical PG Question 10: A 67-year-old woman presents to the infectious disease clinic after her PPD was found to be positive. A subsequent chest radiography shows a cavity in the apex of the right upper lobe, along with significant hilar adenopathy. The patient is diagnosed with tuberculosis and is started on the standard four-drug treatment regimen. Four weeks later, she returns for her first follow-up appointment in panic because her eyes have taken on an orange/red hue. Which of the following describes the mechanism of action of the drug most likely responsible for this side effect?
- A. Inhibition of RNA polymerase (Correct Answer)
- B. Inhibition of squalene epoxidase
- C. Inhibition of arabinosyltransferase
- D. Inhibition of mycolic acid synthesis
- E. Inhibition of topoisomerase
Hepatitis C direct-acting antivirals Explanation: ***Inhibition of RNA polymerase***
- The drug most likely responsible for the **orange/red discoloration of tears, sweat, saliva, and urine is rifampin**.
- **Rifampin exerts its bactericidal effect by inhibiting bacterial DNA-dependent RNA polymerase**, thereby blocking RNA synthesis.
*Inhibition of squalene epoxidase*
- This mechanism of action is characteristic of **terbinafine**, an antifungal drug.
- **Terbinafine is used to treat fungal infections** like dermatophytosis and onychomycosis, not tuberculosis.
*Inhibition of arabinosyltransferase*
- This is the **mechanism of action for ethambutol**, another first-line drug for tuberculosis.
- While ethambutol is part of the standard regimen, its primary side effect is **optic neuritis**, not orange discoloration of bodily fluids.
*Inhibition of mycolic acid synthesis*
- This mechanism is primarily associated with **isoniazid (INH)**, a key drug in tuberculosis treatment.
- **Isoniazid's main toxicities include hepatotoxicity and peripheral neuropathy**, not the red-orange discoloration.
*Inhibition of topoisomerase*
- This mechanism is characteristic of **fluoroquinolone antibiotics**, such as ciprofloxacin and levofloxacin.
- While fluoroquinolones can be used in some tuberculosis regimens, they are typically **second-line agents** and do not cause the orange/red bodily fluid discoloration.
More Hepatitis C direct-acting antivirals US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.