Broad-spectrum antivirals US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Broad-spectrum antivirals. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Broad-spectrum antivirals US Medical PG Question 1: A 57-year-old man comes to the emergency department because he has been having problems seeing over the last week. He says that he has been seeing specks in his vision and his vision also becomes blurry when he tries to focus on objects. He says that he cannot recall anything that may have precipitated this; however, he has been homeless for several months. His CD4+ cell count is 27 cells/mL so he is started on a new medication. Notably, this drug has the following properties when mixed with various proteins:
Drug alone - drug remains unphosphorylated
Drug and HSV proteins - drug remains unphosphorylated
Drug and CMV proteins - drug remains unphosphorylated
Drug and human proteins - drug is phosphorylated
Which of the following drugs is most consistent with this set of findings?
- A. Cidofovir (Correct Answer)
- B. Oseltamivir
- C. Ganciclovir
- D. Acyclovir
- E. Foscarnet
Broad-spectrum antivirals Explanation: ***Cidofovir***
- The patient's presentation with **seeing specks and blurry vision** (floaters) along with a **CD4+ count of 27 cells/mL** strongly suggests **CMV retinitis**, a common opportunistic infection in advanced HIV/AIDS.
- **Cidofovir** is a nucleotide analog that **does NOT require viral kinases for activation** - it remains unphosphorylated when mixed with HSV or CMV proteins, as stated in the question.
- However, cidofovir **DOES require phosphorylation by host cellular kinases** (specifically cellular kinases, not viral kinases) to become the active triphosphate form. This matches the drug property showing it **becomes phosphorylated with human proteins**.
- This unique activation mechanism (host-dependent, viral-independent) distinguishes it from other antivirals and matches the experimental findings described.
*Foscarnet*
- **Foscarnet** is also used for CMV retinitis and **does NOT require ANY phosphorylation** - neither viral nor host enzymes.
- It acts as a **pyrophosphate analog** that directly inhibits viral DNA polymerase without requiring activation.
- The drug properties show phosphorylation occurs with human proteins, which is **inconsistent with foscarnet** that remains unphosphorylated under all conditions.
*Ganciclovir*
- **Ganciclovir** requires phosphorylation by **viral kinase UL97 in CMV** (or thymidine kinase in HSV) for initial activation, followed by host kinases.
- The drug properties state it remains unphosphorylated with CMV proteins, which is **inconsistent with ganciclovir's mechanism**.
*Acyclovir*
- **Acyclovir** is primarily used for **HSV and VZV infections**, not CMV retinitis in AIDS patients.
- It requires initial phosphorylation by **viral thymidine kinase** (HSV-TK), which contradicts the finding that it remains unphosphorylated with HSV proteins.
*Oseltamivir*
- **Oseltamivir** is a **neuraminidase inhibitor** used for **influenza treatment**.
- It has no role in CMV retinitis and does not act via phosphorylation-dependent DNA polymerase inhibition.
Broad-spectrum antivirals US Medical PG Question 2: A 60-year-old man comes to the physician’s office with jaundice. Liver ultrasound reveals a shrunken liver and biopsy reveals cirrhosis. Hepatitis serologies are below:
Anti-HAV: negative
HBsAg: negative
HBsAb: positive
HBeAg: negative
Anti-HBe: negative
Anti-HBc: negative
Anti-HCV: positive
The hepatitis C viral load is 1,000,000 copies/mL. The patient is started on an antiviral regimen including sofosbuvir. What is the mechanism of action of this drug?
- A. Inhibits reverse transcriptase
- B. Inhibits integrase
- C. Inhibits synthesis of DNA-dependent DNA polymerase
- D. Inhibits RNA-dependent RNA polymerase (Correct Answer)
- E. Inhibits hepatitis C protease
Broad-spectrum antivirals Explanation: ***Inhibits RNA-dependent RNA polymerase***
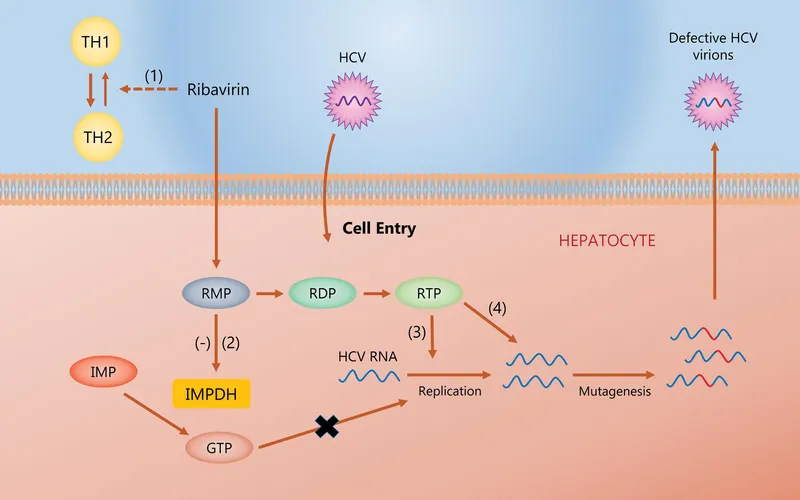
- Sofosbuvir is a **nucleotide analog** that targets the **HCV RNA-dependent RNA polymerase (NS5B)**, essential for viral replication.
- By inhibiting NS5B, it acts as a **chain terminator**, preventing the synthesis of new viral RNA strands.
*Inhibits reverse transcriptase*
- This mechanism is characteristic of drugs used to treat **HIV infection**, as reverse transcriptase is an enzyme found in retroviruses.
- Hepatitis C virus (HCV) is an **RNA virus** that replicates via an RNA intermediate, not DNA, and thus does not utilize reverse transcriptase.
*Inhibits integrase*
- Integrase inhibitors are a class of drugs primarily used in the treatment of **HIV infection**, preventing the viral DNA from integrating into the host genome.
- HCV replication does not involve an integration step into the host DNA, making this mechanism irrelevant for HCV treatment.
*Inhibits synthesis of DNA-dependent DNA polymerase*
- Inhibition of DNA-dependent DNA polymerase primarily targets organisms that replicate their DNA, such as **herpesviruses** or host cell processes.
- HCV is an RNA virus and does not synthesize or rely on a DNA-dependent DNA polymerase for its replication cycle.
*Inhibits hepatitis C protease*
- While **protease inhibitors (e.g., -previr drugs)** are an important class of anti-HCV drugs, sofosbuvir specifically targets the viral **RNA polymerase (NS5B)**.
- Protease inhibitors block the **NS3/4A protease**, which is responsible for cleaving the large HCV polyprotein into functional proteins.
Broad-spectrum antivirals US Medical PG Question 3: A 53-year-old woman comes to the physician in February because of a 1-day history of fever, chills, headache, and dry cough. She also reports malaise and generalized muscle aches. She works as a teacher at a local high school, where there was recently an outbreak of influenza. She has a history of intermittent asthma, for which she takes albuterol as needed. She declined the influenza vaccine offered in the fall because her sister told her that a friend developed a flulike illness after receiving the vaccine. She is worried about possibly becoming ill and cannot afford to miss work. Her temperature is 37.9°C (100.3°F), heart rate is 58/min, and her respirations are 12/min. Physical examination is unremarkable. Her hemoglobin concentration is 14.5 g/dL, leukocyte count is 9,400/mm3, and platelet count is 280,000/mm3. In addition to analgesia, which of the following is the most appropriate next step in management?
- A. Inactivated influenza vaccine
- B. Amantadine
- C. Live attenuated influenza vaccine
- D. Oseltamivir (Correct Answer)
- E. Supportive therapy only
Broad-spectrum antivirals Explanation: ***Oseltamivir***
- This patient presents with classic symptoms of **influenza** (fever, chills, headache, dry cough, malaise, myalgias) during an outbreak, making **antiviral therapy** like oseltamivir appropriate.
- She is at risk for complications due to her history of **asthma**, and early treatment (within 48 hours of symptom onset) can reduce illness severity and duration.
*Inactivated influenza vaccine*
- An **inactivated influenza vaccine** is a **preventive measure** and is not effective as a treatment once symptoms have already begun.
- Vaccination in the past fall would have been appropriate, but it will not help resolve her current acute illness.
*Amantadine*
- **Amantadine** is an older antiviral agent active only against **influenza A**, and its use is limited due to widespread **resistance**.
- It is generally not recommended for routine influenza treatment due to its narrow spectrum and resistance profile.
*Live attenuated influenza vaccine*
- The **live attenuated influenza vaccine (LAIV)** is a **preventive measure** indicated for healthy individuals aged 2-49 years and is contraindicated in individuals with **asthma**.
- Like the inactivated vaccine, it is not used for treating active influenza infection.
*Supportive therapy only*
- While supportive care (analgesia, hydration) is important, relying solely on it is not the most appropriate step given the patient's **risk factors** (asthma) and the availability of effective antiviral treatment.
- Early antiviral therapy can reduce serious complications in at-risk individuals.
Broad-spectrum antivirals US Medical PG Question 4: A 66-year-old woman with chronic obstructive pulmonary disease is brought to the emergency department because of fever, body aches, malaise, and a dry cough. She has smoked one pack of cigarettes daily for 30 years but quit smoking 1 year ago. She lives with her daughter and her granddaughter, who attends daycare. Her temperature is 38.1°C (101°F). Physical examination shows bilateral conjunctivitis, rhinorrhea, and erythematous tonsils without exudates. Further testing confirms infection with an enveloped orthomyxovirus. Administration of a drug with which of the following mechanisms of action is most appropriate?
- A. Inhibition of protease
- B. Inhibition of neuraminidase (Correct Answer)
- C. Inhibition of proton translocation
- D. Inhibition of nucleoside reverse transcriptase
- E. Inhibition of DNA polymerase
Broad-spectrum antivirals Explanation: ***Inhibition of neuraminidase***
- The patient's symptoms (fever, body aches, malaise, dry cough, conjunctivitis, rhinorrhea, erythematous tonsils), exposure history (daycare contact), and diagnosis of an **enveloped orthomyxovirus** strongly indicate **influenza**.
- **Neuraminidase inhibitors** (e.g., oseltamivir, zanamivir) prevent viral release from infected cells by cleaving sialic acid residues, effectively halting the spread of the virus.
*Inhibition of protease*
- **Protease inhibitors** are primarily used to treat **HIV infection**, preventing the cleavage of viral polyproteins into functional enzymes.
- This mechanism is not relevant for influenza virus, which utilizes different replication enzymes and strategies.
*Inhibition of proton translocation*
- **M2 inhibitors** (amantadine, rimantadine) act by blocking the viral M2 ion channel, which is essential for **viral uncoating** within the host cell.
- However, due to widespread resistance, especially among influenza A strains, these drugs are generally not recommended for routine use.
*Inhibition of nucleoside reverse transcriptase*
- **Nucleoside reverse transcriptase inhibitors (NRTIs)** are a class of antiretroviral drugs used to treat **HIV infection** by inhibiting the reverse transcription of viral RNA into DNA.
- This mechanism is specific to retroviruses and has no role in the treatment of orthomyxovirus infections like influenza.
*Inhibition of DNA polymerase*
- **DNA polymerase inhibitors** (e.g., acyclovir, ganciclovir) are used to treat **herpesvirus infections** by interfering with viral DNA replication.
- Influenza is an RNA virus and does not rely on DNA polymerase for its replication cycle.
Broad-spectrum antivirals US Medical PG Question 5: A 49-year-old woman presents to her primary care doctor in late December with malaise. She reports worsening fatigue, myalgias, headache, and malaise that started 1 day ago. She works as a lunch lady at an elementary school. Her past medical history is notable for a distal radius fracture after a fall 2 years ago, but she is otherwise healthy and takes no medications. She does not smoke or drink alcohol. She is married and has 3 adult children who are healthy. Her temperature is 102.9°F (39.4°C), blood pressure is 101/61 mmHg, pulse is 112/min, and respirations are 21/min. On exam, she appears lethargic and uncomfortable but is able to answer questions appropriately. Breath sounds are normal bilaterally. She is started on intravenous fluids and a pharmacologic agent for treatment. Which of the following is the most likely mechanism of action of the drug being used to treat this patient?
- A. Neuraminidase inhibitor (Correct Answer)
- B. Reverse transcriptase inhibitor
- C. RNA-dependent polymerase inhibitor
- D. DNA polymerase inhibitor
- E. Protease inhibitor
Broad-spectrum antivirals Explanation: ***Neuraminidase inhibitor***
- The patient's symptoms (malaise, fatigue, myalgias, headache, fever) with rapid onset in **late December**, especially given her exposure to children in an elementary school, are highly suggestive of **influenza**.
- **Neuraminidase inhibitors** (e.g., oseltamivir, zanamivir) are the primary antiviral treatment for influenza, preventing the release of new viral particles from infected cells.
*Reverse transcriptase inhibitor*
- **Reverse transcriptase inhibitors** are primarily used in the treatment of **HIV infection**, which typically presents with a different constellation of symptoms and has a chronic rather than acute course.
- This class of drugs targets the enzyme **reverse transcriptase**, which is not central to the influenza virus replication cycle.
*RNA-dependent polymerase inhibitor*
- While **baloxavir marboxil** (an RNA polymerase inhibitor) is FDA-approved for influenza treatment, **neuraminidase inhibitors** remain the most commonly used first-line agents.
- In this clinical scenario without specific contraindications to neuraminidase inhibitors, oseltamivir or zanamivir would be the most likely agents prescribed.
*DNA polymerase inhibitor*
- **DNA polymerase inhibitors** are primarily used to treat **DNA viral infections** such as herpes viruses (e.g., acyclovir for HSV/VZV) or cytomegalovirus (e.g., ganciclovir).
- Influenza is an **RNA virus** and therefore does not have a DNA polymerase for replication.
*Protease inhibitor*
- **Protease inhibitors** are a class of antiviral drugs predominantly used in the treatment of **HIV** and **Hepatitis C virus** infections.
- Influenza viruses do not have a protease target that is typically inhibited by these drugs for therapeutic purposes.
Broad-spectrum antivirals US Medical PG Question 6: An HIV-positive patient with a CD4+ count of 45 is receiving recommended first-line treatment for a case of cytomegalovirus retinitis. Coadministration with which of the following agents would be most likely to precipitate a deficiency of neutrophils in this patient?
- A. Ritonavir
- B. Raltegravir
- C. Foscarnet
- D. Efavirenz
- E. Zidovudine (Correct Answer)
Broad-spectrum antivirals Explanation: ***Zidovudine***
- **Zidovudine (AZT)** is a nucleoside reverse transcriptase inhibitor (NRTI) that is well-known for causing **myelosuppression**, particularly **neutropenia** and **anemia**.
- In an HIV-positive patient with a low **CD4+ count** and concurrent treatment for **CMV retinitis** (which often involves drugs like ganciclovir that can also cause myelosuppression), adding zidovudine significantly increases the risk of severe neutropenia.
*Ritonavir*
- **Ritonavir** is a protease inhibitor primarily known for its role as a **pharmacokinetic booster** in HIV therapy, enhancing the levels of other antiretrovirals.
- While it can cause gastrointestinal side effects and hepatotoxicity, **myelosuppression** and specifically neutropenia are not its primary or common adverse effects.
*Raltegravir*
- **Raltegravir** is an integrase strand transfer inhibitor (INSTI) generally well-tolerated with a favorable side effect profile.
- Common side effects include headache, nausea, and fatigue, but it is **not typically associated with significant myelosuppression** or neutropenia.
*Foscarnet*
- **Foscarnet** is an antiviral agent used for treating CMV retinitis, particularly in cases of ganciclovir resistance.
- Its major dose-limiting toxicities include **nephrotoxicity** and **electrolyte disturbances** (e.g., hypocalcemia, hypomagnesemia), not primarily neutropenia.
*Efavirenz*
- **Efavirenz** is a non-nucleoside reverse transcriptase inhibitor (NNRTI) associated with central nervous system side effects such as dizziness, insomnia, and vivid dreams.
- While skin rash and hepatotoxicity can occur, **bone marrow suppression** leading to neutropenia is not a characteristic or frequent adverse effect of efavirenz.
Broad-spectrum antivirals US Medical PG Question 7: A 27-year-old man is brought to the emergency department by his friends in a confused state. He was doing fine 5 days ago when he started to complain of fever and flu-like symptoms. His fever was low-grade and associated with a headache. For the past 2 days, he has become increasingly irritable, confused, and was getting angry at trivial things. Past medical history is unremarkable. He is a college student and is physically active. He smokes cigarettes occasionally. He drinks alcohol socially. He is sexually active with his girlfriend and they use condoms inconsistently. Physical examination reveals: blood pressure 120/80 mm Hg, heart rate 108/min, respiratory rate 10/min, and temperature 37.4°C (99.4°F). He is confused and disoriented. Pupils are 3 mm in diameter and respond to light sluggishly. He is moving all his limbs spontaneously. His neck is supple. MRI of the brain is shown in the picture. Cerebrospinal fluid (CSF) reveals an opening pressure of 16 cm of H20, a total leukocyte count of 112/mm3 with 85% lymphocytes, the protein of 42 mg/dL, and glucose of 58 mg/dL. What is the best treatment for this condition?
- A. Intravenous immunoglobulin
- B. High-dose steroids
- C. Rituximab
- D. Acyclovir (Correct Answer)
- E. Ceftriaxone
Broad-spectrum antivirals Explanation: ***Acyclovir***
- The patient's presentation with **fever**, **flu-like symptoms** followed by **irritability**, **confusion**, and **MRI findings** suggestive of temporal lobe involvement, along with **lymphocytic pleocytosis** in CSF, is highly indicative of **herpes simplex encephalitis (HSE)**.
- **Acyclovir** is the treatment of choice for HSE, as it is an antiviral drug effective against the **herpes simplex virus (HSV)**. Prompt administration significantly improves outcomes.
*Intravenous immunoglobulin*
- **Intravenous immunoglobulin (IVIG)** is generally used for certain **immunodeficiencies** or **autoimmune conditions**, not for acute viral encephalitis like HSE.
- There is no evidence to support the use of IVIG as a primary treatment for HSV encephalitis.
*High-dose steroids*
- While steroids can reduce cerebral edema and inflammation, their routine use in **viral encephalitis** like HSE is **controversial** and not a first-line treatment.
- Steroids might be considered in specific cases of severe cerebral edema, but not as the primary antiviral therapy.
*Rituximab*
- **Rituximab** is a **monoclonal antibody** targeting **CD20-positive B cells**, primarily used in certain **lymphomas** and **autoimmune diseases** like **rheumatoid arthritis** or **multiple sclerosis**.
- It has no role in the treatment of acute viral encephalitis.
*Ceftriaxone*
- **Ceftriaxone** is a broad-spectrum **antibiotic** used to treat **bacterial meningitis** or other bacterial infections.
- It is ineffective against viral infections such as HSV encephalitis.
Broad-spectrum antivirals US Medical PG Question 8: A 6-month-old infant boy is brought to the clinic for a check-up by a couple who recently adopted him from foster care. The biological mother was from a rehabilitation facility and was found incompetent to care for the child, hence he was handed over to foster care. No other information is available regarding his prenatal or birth history. On examination, his weight is found to be below the 3rd percentile. Physical appearance is remarkable for midfacial hypoplasia with a flattened nasal bridge, smooth philtrum, and thin lips. Auscultation reveals a grade 3/6 holosystolic murmur at the left lower sternal border. Developmental delay is noted as well. Which of the following teratogens is most likely to be associated with the infant's presentation?
- A. Lithium
- B. Tobacco
- C. Phenytoin
- D. Alcohol (Correct Answer)
- E. Cocaine
Broad-spectrum antivirals Explanation: ***Alcohol***
- The combination of **facial dysmorphology** (midfacial hypoplasia, flattened nasal bridge, smooth philtrum, thin lips), **growth restriction** (weight below 3rd percentile), **cardiac defect** (holosystolic murmur), and **developmental delay** is highly characteristic of **Fetal Alcohol Syndrome (FAS)**.
- The biological mother's history of being in a **rehabilitation facility** suggests a potential history of substance abuse, making maternal alcohol consumption during pregnancy a strong possibility.
*Lithium*
- Maternal lithium use is associated with **Ebstein's anomaly**, a specific congenital heart defect, but typically does not cause the widespread facial dysmorphism and growth restriction seen in this infant.
- While it can cause cardiac defects, the overall constellation of findings points away from lithium as the primary teratogen.
*Tobacco*
- Maternal tobacco use is primarily associated with **low birth weight**, premature birth, and an increased risk of specific birth defects like **cleft lip and palate**.
- It does not typically cause the characteristic facial features, significant cardiac anomalies, or widespread developmental delay observed in this case.
*Phenytoin*
- Phenytoin, an anticonvulsant, can cause **fetal hydantoin syndrome**, characterized by specific facial features (e.g., hypertelorism, short nose, cleft lip/palate), **digital hypoplasia**, and intellectual disability.
- While it can cause some overlapping features like growth deficiency and developmental delay, the specific craniofacial features described for this infant are more typical of FAS.
*Cocaine*
- Cocaine exposure during pregnancy is associated with a range of problems including **preterm birth**, **placental abruption**, and **genitourinary defects**.
- Its teratogenic effects often involve vascular disruption leading to limb defects or cerebral infarctions, rather than the characteristic facial dysmorphology and cardiac defects described in this infant.
Broad-spectrum antivirals US Medical PG Question 9: A 26-year-old G1P0 woman is brought to the emergency room by her spouse for persistently erratic behavior. Her spouse reports that she has been sleeping > 1 hour a night, and it sometimes seems like she’s talking to herself. She has maxed out their credit cards on baby clothes. The patient’s spouse reports this has been going on for over a month. Since first seeing a physician, she has been prescribed multiple first and second generation antipsychotics, but the patient’s spouse reports that her behavior has failed to improve. Upon examination, the patient is speaking rapidly and occasionally gets up to pace the room. She reports she is doing “amazing,” and that she is “so excited for the baby to get here because I’m going to be the best mom.” She denies illicit drug use, audiovisual hallucinations, or suicidal ideation. The attending psychiatrist prescribes a class of medication the patient has not yet tried to treat the patient’s psychiatric condition. In terms of this new medication, which of the following is the patient’s newborn most likely at increased risk for?
- A. Ototoxicity
- B. Attention deficit hyperactivity disorder
- C. Right ventricular atrialization (Correct Answer)
- D. Renal defects
- E. Caudal regression syndrome
Broad-spectrum antivirals Explanation: ***Right ventricular atrialization***
- The patient's presentation of persistent **erratic behavior**, **reduced sleep**, rapid speech, and increased spending, enduring for over a month, is highly suggestive of a **manic episode** in the context of **bipolar I disorder**. Since antipsychotics have been ineffective, the next step is often **lithium**.
- **Lithium** exposure during the first trimester of pregnancy is associated with an increased risk of **Ebstein's anomaly**, a congenital heart defect characterized by **right ventricular atrialization** (displacement of the tricuspid valve leaflets into the right ventricle), leading to tricuspid regurgitation and right heart failure.
*Ototoxicity*
- **Ototoxicity** in newborns is typically associated with exposure to medications such as **aminoglycoside antibiotics** (e.g., gentamicin) or certain diuretics (e.g., furosemide) during pregnancy.
- Lithium is not known to cause ototoxicity as a primary birth defect.
*Attention deficit hyperactivity disorder*
- While various prenatal exposures can influence neurodevelopment, there is currently **no strong evidence** linking in-utero lithium exposure specifically to an increased risk of **ADHD** in offspring.
- ADHD is a complex neurodevelopmental disorder with multifactorial origins, including genetic and environmental factors.
*Renal defects*
- While lithium is primarily excreted by the kidneys and can cause **renal dysfunction** in adults (e.g., nephrogenic diabetes insipidus), it is not a prominent teratogen known to cause specific **structural renal defects** in newborns when exposed during pregnancy.
- Renal anomalies are more commonly associated with other medications or genetic syndromes.
*Caudal regression syndrome*
- **Caudal regression syndrome** is a severe congenital anomaly affecting the development of the lower spine and limbs. It is strongly associated with **poorly controlled maternal diabetes**.
- There is no established link between in-utero lithium exposure and caudal regression syndrome.
Broad-spectrum antivirals US Medical PG Question 10: An 8-year-old boy is brought to the emergency department by his parents because of sudden onset of abdominal pain beginning an hour ago. The parents report that their son has also had an episode of dark urine earlier that morning. Three days ago, he was diagnosed with a urinary tract infection and was treated with trimethoprim-sulfamethoxazole. He emigrated from Liberia to the US with his family 3 years ago. There is no personal history of serious illness. His immunizations are up-to-date. Vital signs are within normal limits. Examination shows diffuse abdominal tenderness and scleral icterus. The spleen is palpated 1–2 cm below the left costal margin. Laboratory studies show:
Hemoglobin 10 g/dL
Mean corpuscular volume 90 μm3
Reticulocyte count 3%
Serum
Bilirubin
Total 3 mg/dL
Direct 0.5 mg/dL
Haptoglobin 20 mg/dL (N=41–165 mg/dL)
Lactate dehydrogenase 160 U/L
Urine
Blood 3+
Protein 1+
RBC 2–3/hpf
WBC 2–3/hpf
Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Production of hemoglobin S
- B. Deficient glucose-6-phosphate dehydrogenase (Correct Answer)
- C. Lead poisoning
- D. Cold agglutinins
- E. Defective RBC membrane proteins
Broad-spectrum antivirals Explanation: ***Deficient glucose-6-phosphate dehydrogenase***
- The patient's presentation with **hemolytic anemia** (low hemoglobin, elevated reticulocytes, low haptoglobin, elevated LDH, elevated indirect bilirubin) following **trimethoprim-sulfamethoxazole** administration, along with dark urine (hemoglobinuria), is highly suggestive of G6PD deficiency.
- G6PD deficiency is common in individuals of African descent (patient emigrated from Liberia) and certain medications like sulfa drugs can trigger **oxidative stress** leading to hemolysis in affected individuals.
*Production of hemoglobin S*
- While **sickle cell anemia** (due to hemoglobin S) can cause hemolytic anemia and abdominal pain (**vaso-occlusive crisis**), the sudden onset linked to a specific medication and the absence of a prior history of serious illness make G6PD deficiency more likely.
- Sickle cell disease typically presents with recurrent painful crises, dactylitis in infancy, and chronic hemolytic anemia, which are not described here.
*Lead poisoning*
- **Lead poisoning** can cause abdominal pain and anemia, but it typically presents with a **microcytic hypochromic anemia** and **basophilic stippling** on peripheral smear.
- It does not directly cause an acute hemolytic crisis triggered by trimethoprim-sulfamethoxazole.
*Cold agglutinins*
- **Cold agglutinin disease** involves hemolytic anemia triggered by cold exposure, and the antibodies react optimally at cold temperatures.
- The patient's symptoms are acute and triggered by a medication known to induce oxidative stress, which is not characteristic of cold agglutinin disease.
*Defective RBC membrane proteins*
- **Hereditary spherocytosis** (a defect in RBC membrane proteins like spectrin or ankyrin) causes chronic hemolytic anemia and splenomegaly.
- While it can manifest with jaundice, it typically does not cause an acute, drug-induced hemolytic crisis with hemoglobinuria as seen here.
More Broad-spectrum antivirals US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.